Abstract
Purpose
The objective of this study was to determine the safe penetration depth of the FasT-Fix meniscal suture repair system during all-inside repair of the posterior part of the lateral meniscus.
Methods
Thirty-one knees from 17 embalmed and formalin-fixed cadavers (11 women, 6 men) were used. In each case, the circumference of the cadaver knee was measured before dissection. After dissection, 41 Fast-Fix meniscal repair devices were used in different predetermined penetration depths ranging from 8 to 16 mm. In this study, non-involvement of the popliteal neurovascular bundle, common peroneal nerve or the inferior lateral genicular vessels by either needle penetration or affixment by the suture bar anchors was considered to be a safe trial.
Results
Out of the 41 FasT-Fix devices used in this study, only one device bent during introduction and was excluded from the study. For the remaining 40 trials, 27 of them were considered safe, while 13 trials were considered unsafe. The ratio of the average penetration depth to the average circumference of the cadaver knee was found to be >0.05 for the unsafe penetrations, and this was statistically significant P < 0.05. Additionally, for the first point, which is more central, there was a trend for the straight needles through the direct lateral approach to be less safe, and this was found to be statistically significant P < 0.05.
Conclusions
Correlating the needle-penetration depth to the measured circumference of the cadaver knee may be an important clinical predictor of safety whereby a ratio of less than 0.05 might be useful as a guide to determine the safe penetration depth of the FasT-Fix suture repair needle during repair of the posterior horn lateral meniscus. Also, it is better to avoid using straight needles through the direct lateral approach during repair of the more central portion of the posterior horn lateral meniscus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several methods are currently available for meniscal repair. The Inside-out meniscal repair remains the gold standard for meniscal fixation due to the greater ultimate strength provided by conventional vertical meniscal suturing [7, 24, 27]. However, this procedure is associated with increased surgical time, due to the need for an additional posterior incision. It has been also associated with a potentially increased risk of neurovascular complications. All-inside fixation has been a focal point for advances in arthroscopy, due in part to its ease of insertion and the decreased surgical time required for repair [7, 24]. The newest generation of meniscal repair devices is designed to incorporate the best features of the all-inside techniques with the superior biomechanical properties of the inside-out technique [1, 3–5, 16, 17, 24, 26, 27, 34].
One of these devices is the FasT-Fix meniscal repair suture system (the FasT-Fix; Smith and Nephew, Endoscopy Division, Andover, MA), which is a second generation fixator device and is actually a modification of a previously introduced device, the T Fix [1, 6, 8, 16, 17]. This device is particularly interesting because of its low profile, double-point fixation, and the arthroscopic technique used for its application comprising the use of self-locking sliding knot technology that eliminates the need to tie intra-articular sutures. This affords a fast and simple method of attaining all-inside meniscal repair [1, 8, 16]. Moreover, clinical as well as biomechanical studies have demonstrated the clinical utility and the excellent biomechanical properties of this device that are comparable to the vertical mattress suture, meanwhile better than other all-inside meniscal repair systems [2, 5, 8, 10, 15, 16, 19, 23, 25, 28, 34].
Despite the proven safety of this device relative to the inside-out techniques [17, 18, 21], there is still risk of injury to neurovascular structures as well as to capsuloligamentous structures [13]. This is particularly true in the management of the posterior part of the lateral meniscus. These structures theoretically might be injured by the needle tip or affixed by the suture anchor bar of the device [9, 12, 19].
Therefore, this study was developed to evaluate the safest method of using the FasT-Fix suture meniscal repair system, particularly in regards to the posterior part of the lateral meniscus, due to the more frequent association of tears of this part of the meniscus with anterior cruciate ligament injury and its close proximity to vital neurovascular structures on the posterior aspect of the knee [9, 19, 20, 22].
In this study, it is hypothesized that the ratio of the preset needle-penetration depth to the measured circumference of the operated knee might have an implication on the safety of the device. The study also assesses the effect of varying both the needle angle (whether straight or curved) and the repair approach (whether medial or lateral) on the safety of the FasT-Fix all-inside meniscal repair system when used for repair of a peripherally located tear in the posterior horn of the lateral meniscus.
Materials and methods
Thirty-one knees from 17 cadavers (11 Females, 6 Males) were used from the Gross Anatomy Department at our university. They were embalmed and fixed with formalin, ethanol, isopropanol, phenol, and glycerin.
The mean age of the subjects at the time of death was 84.3 years (range from 46 to 94 years). A total of 41 trials of the FasT-Fix meniscal repair system were carried out. One device was bent after deployment of the first suture bar anchor, so a total of 40 devices were validly used in the study.
The surgical procedures were all done by the same surgeon, with the knee in the standard 90° flexion position. The FasT-Fix meniscal repair system (Smith and Nephew Endoscopy, Andover, MA) was used. The repair system comprises a FasT-Fix AB suture bar that is made up of a 5-mm poly L-lactic acid (PLLA) bioabsorbable polymer suture bar, pre-tied with 0 non-absorbable USP braided polyester sutures. Two types of FasT-Fix needles were used: the straight 0° and the curved 22°. The white trimmable depth-penetration limiter was set at different penetration depths 8, 10, 12, 14, and 16 mm. The insertion technique of the FasT-Fix devices was keeping with the manufacturer`s recommendations [16, 17, 21, 25].
The overall circumference of the tested knee was measured preoperatively at the joint level in centimeters (cm) using a measuring tape. In order to find out its relation to the needle-penetration depth, this measurement was converted to millimeters (mm) to allow a uniform ratio of the needle-penetration depth to the knee circumference.
All the measurements were done by two surgeons. The inter-observer reliability was then assessed. The two individuals who performed the inter-observer reliability tests were the same individuals who invented and agreed on the measurement technique together. All observer-dependent steps in the analysis were repeated, including the preoperative measurement of the circumference of the knee, establishment of points 1, and 2 located 5, and 10 mm, respectively, from the root of the lateral meniscus, as well as the distance between the needle tips to the vital neurovascular structures.
A medial parapatellar arthrotomy was performed. As the knee is usually stiff in extension, the following sequential release was tried.
-
First, release the quadriceps tendon two inches above the patella.
-
Then, medial release of the medial collateral ligament, the pes anserinus insertion, and medial joint capsule.
-
Next, release of the ACL (anterior cruciate ligament) and the PCL (posterior cruciate ligament).
-
Finally, partial release of the iliotibial band two inches above the joint line level.
The aim was to obtain a range of movement of at least 0–90°, and to be able to put the knee in a position simulating that used during arthroscopic meniscal repair.
Two arbitrary proposed points of needle penetration, Points 1 and 2 both in the posterior part of the lateral meniscus, were chosen on the midsubstance of the posterior horn of the lateral meniscus at 5 and 10 mm, respectively, from the root of the meniscus. These points are usually used to repair a peripherally located tear in the corresponding portion of the posterior horn lateral meniscus [1, 16, 20, 22].
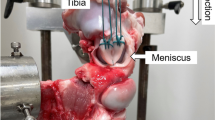
Both points 1 and 2 were randomly approached through either the lateral side or the medial side using either a straight needle or curved needle. Randomization was designed so that an equal number of trials was performed using each of the five tested penetration depths (Fig. 1). Gross dissection of the posterior aspect of the knee was carried out at the same time, to identify the anatomical structure pierced by the needle tip before release of the first implant, as well as before release of the second suture bar anchor. This was done through a midline skin incision with cutting and reflection of the lateral head of the gastrocnemius and plantaris muscles to expose the posterolateral corner structures (Fig. 2) [12, 29, 32].
Showing gross dissection of the posterolateral aspect of the knee, CPN (Common Peroneal Nerve) marked by a yellow star, The Inferior lateral genicular vessels (ILGVs) on the back of the lateral meniscus (pointed to by a long red arrow), and the lateral head of gastrocinemeus (LHGC) reflected (Green arrow head). The FasT-Fix needle is in situ (Short black arrow). The needle tip is not seen, indicating safe penetration
For needle tips penetrating beyond the posterior capsule, the distance between the needle tip and the popliteal neurovascular bundle, the inferior lateral genicular vessels and the common peroneal nerve was measured in millimeters in a horizontal plane parallel to the knee joint, using a flexible metal ruler. Finally, the anatomical structure affixed by the suture bar anchors was observed.
Safety criteria
In this study, violation of the vital neurovascular structures namely the popliteal neurovascular bundle, the common peroneal nerve or the inferior lateral genicular vessels, by needle tip penetration before deployment of the first or second suture bar anchors was considered to be unsafe. Also, involvement of either of these structures in the suture bar anchor was considered to be unsafe.
Statistical analysis
Statistical analysis was done using the Mann–whitney test, for non-parametric values and categorical variables. P values of less than 0.05 were considered statistically significant. Also, one-way analysis of variants and the subsequent Chi-square test were used. The intraclass correlation coefficient and the standard error of measurement were used for assessment of the inter-observer reliability of the measurements.
Results
Out of the 41 Fast-Fix devices used in this study, 40 trials were successful with deployment of the two suture bar anchors and intra-articular knot tightening at the planned points of lateral meniscal penetration, 5 and 10 mm from the root of the posterior horn lateral meniscus representing points 1 and 2, respectively.
Of these 40 trials, 27 were considered safe without penetration or affixment of the vital neurovascular structures in the posterior and posterolateral aspects of the knee, namely the popliteal neurovascular bundle, the inferior lateral genicular vessels, and the common peroneal nerve, by either the needle tip or the suture bar anchors, respectively. On the other hand, 13 trials were considered unsafe. In seven cases, there was violation of the popliteal neurovascular bundle, while in four cases there was penetration of the common peroneal nerve, and in two cases there was penetration of the inferior lateral genicular vessels.
For the safe penetrations, the average distance from the popliteal neurovascular bundle was 15.2 and 8.3 mm from the common peroneal nerve and 2.1 mm from the inferior lateral genicular vessels. None of these structures was involved in the suture bar anchors. According to inter-observer variation, the measurement technique showed high reliability.
For both the safe (Fig. 3) and unsafe penetrations (Figs. 4 and 5) the ratio of the average needle-penetration depth to the average cadaver knee circumference was calculated. It was found that for unsafe penetration this ratio was more than 0.05, while for the safe penetration this ratio was less than 0.05, and this difference was found to be statistically significant P < 0.05 (Fig. 6).
For the first point, which is more central, there was a statistically significant relation between the use of straight needles through the direct lateral approach and unsafety P < 0.05. While for the second point, there was no statistically significant correlation between the safety and either the needle type (straight or curved), or the approach used (medial or lateral) (Figs. 7 and 8).
Showing the relation between the approach used for repair of the posterior horn of the lateral meniscal and the safety of the FasT-Fix meniscal repair system. The upper graph shows a higher percentage of unsafe trials for the first point, which is more central, when the lateral approach is used. M Medial, L Lateral
Showing the relation between the needle angle and the safety of the FasT-Fix meniscal repair system. The upper graph shows a higher percentage of unsafe trials for the first point, which is more central, when straight needles are used for repair of the posterior horn of the lateral meniscus. St straight, Cu curved
Discussion
The most important finding of this study is that there is a relation between the measured circumference of the knee and the FasT-Fix needle-penetration depth. Consequently, the former could be used as a preoperative, easily measured patient-specific clinical parameter to guide the safe use of the FasT-Fix meniscal repair system. Also, the use of straight needles through the lateral approach for repair of the more centrally located tears in the posterior horn of the lateral meniscus should be prohibited as it potentially carries more risk to the vital neurovascular structures in the posterior aspect of the knee.
There are several devices currently available for all-inside meniscal repair. One of these devices, the FasT-Fix (Smith and Nephew, Endoscopic Division, Andover, MA), is attractive, because it combines the advantages of traditional inside-out meniscal repair with an all-inside technique. Moreover, there are many studies proving their biomechanical efficiency in comparison to other meniscal repair devices [1, 8, 10, 14, 16, 17, 19, 25, 28, 33].
Despite the proven clinical safety of these devices [18, 21], there are some studies in the literature proving the existence of a significant risk to the nearby neurovascular structures during all-inside repair of the posterior horn of the lateral meniscus [11, 13]. In a recent investigation, the authors found that under certain circumstances, the application cannula of a FasT-Fix device came within 3 mm of the popliteal artery, whereas the RapidLoc (DePuy Mitek, Raynham, MA), with its shorter cannula, remained at a greater distance from that vessel [13].
In previous studies devised to discuss the technical aspects related to the use of the FasT-Fix device, the authors recommended the use of the depth-penetration limiter and pre-measurement of the desired depth followed by trimming of the depth-limitation device to no greater than 15 mm, in order to avoid potential problems related to excessive penetration depth [13, 16, 21, 25, 30]. However, it was reported that over-penetration still occurred in several instances even after experience was gained [16, 25].
On the other hand, in the study performed by Miller et al. [25], they reported that in 3 cases when the device was inserted to the full 22 mm depth, it actually penetrated superficial structures, including the skin, but when the optional trimmable depth-penetration limiter was cut to a length of 15 mm and used, this superficial penetration was avoided. These authors recommended not using a straight needle of more than 10 mm for the posterior horn of the lateral meniscus and advised avoidance of the device in the extreme posterior regions of the menisci, particularly in the lateral meniscus where the neurovascular structures are most at risk, and urged consistent use the depth-penetration limiter [13, 25].
The importance of using the preset depth-penetration limiter to avoid excessive needle penetration is well recognized [13, 18, 21, 25]. However, in order to better specify a safe penetration depth, this study was implemented. The ratio between the penetration depth and the circumference of the pre-surgery knee was measured for both the safe and unsafe trials. Also, the relationship between the needle angles (whether straight or curved), the approach (whether medial or lateral) and safety was assessed.
In this study, it was shown that the ratio of the preset depth penetration to the knee circumference at the joint level is more important than the absolute value, due to the marked individual variation in knee size. This finding is in keeping with those of other authors who have reported that in spite of using the preset depth-penetration limiter; it was consistently shown that an inappropriate depth of penetration was achieved, especially in smaller knees [13, 25].
On the other hand, for the first point, there was a trend for the straight needles, and the lateral approach to be more unsafe, and this was found to be statistically significant. This could be explained by the fact that the lateral approach to the posterior horn of the lateral meniscus using straight needles affords a direct access to the central neurovascular structures and puts these structures under a higher risk of injury.
It is worth mentioning that one device bent during insertion. This may be due to the relatively increased hardness of the cadaveric meniscal tissue.
The major limitation of this study is that it was performed on formaldehyde-preserved cadaveric knees. Formaldehyde preservation can lead to tissue contracture, thus to some extent impeding penetration [11]. However, formalin preservation of the cadavers did not significantly affect this study, as a sequential, stepwise release of the cadaveric knees was performed so that a reasonable range of motion from 0° to 90° could be obtained to mimic the clinical situation of arthroscopic lateral meniscal repair. Moreover, the mildly increased stiffness of the meniscal tissue did not hinder the conduction of the experiment, as only one FasT-Fix needle bent out of the 41 devices used.
The reported clinical safety of the FasT-Fix meniscal repair devices as opposed to this cadaveric study could be attributed to the fact that the study was performed on formaldehyde-preserved knees [16, 18, 21, 31]. Another explanation may be due to the fact that in this study, we used a wider range of penetration depths including 14 and 16 mm outside the range commonly used in clinical practice for repair of a tear in the posterior horn lateral meniscus. This was in a trial to find a correlation between the penetration depth and the circumference of the operated knee. Also the involvement of the inferior lateral genicular vessels was considered to be unsafe although involvement of these vessels during clinical meniscal repair might not lead to catastrophic clinical consequences and might not be discovered in the early postoperative period.
Regarding the clinical relevance, the findings of this study suggest that peripheral tears in the posterior horn of the lateral meniscus can be repaired safely using the FasT-Fix all-inside meniscal repair device provided that the trimmable depth-penetration limiter is used and is preset to a length so that its ratio to the knee circumference is less than 0.05. For example, if the operated knee circumference is 280 mm, the depth stop should be set at less than 14 mm, e.g., 12 mm. However, excessive reduction of the penetration depth to gain more safety should be prohibited, as this might prevent deployment of the suture bar anchors, which is essential for successful meniscal repair. Furthermore, according to this study, the use of curved needles through the medial approach may be preferable, especially for the first point that is more central.
Despite the fact that penetration of the capsuloligamentous structures is considered safe in this study, in terms of non-penetration of the vital neurovascular structures, future clinical studies will be necessary to exclude the possibility of any associated adverse clinical effects.
Conclusions
Correlation of the needle-penetration depth to the measured circumference of the cadaver knee might be an important clinical predictor of safety when using the Fast-Fix meniscal suture device for repair of the posterior part of the lateral meniscus. The ratio of less than 0.05 of the preset penetration depth of the needle to be used to the circumference of the patient`s knee might be useful as a guide for determining the safe penetration depth of the FasT-Fix Suture repair system. Also, it is better to avoid using straight needles through the direct lateral approach during repair of the more central portion of the posterior horn lateral meniscus.
References
Ahn JH, Lee YS, Chang JY, Chang MJ, Eun SS, Kim SM (2009) Arthroscopic all inside repair of the lateral meniscus root tear. Knee 16:77–80
Aros BC, Pedroza A, Vasileff WK, Litsky AS, Flanigan DC (2010) Mechanical comparison of meniscal repair devices with mattress suture devices in vitro. Knee Surg Sports Traumatol Arthrosc 18:1594–1598
Baratz ME, Fu FH, Mengato R (1986) Meniscal tears; the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee: a preliminary report. Am J Sports Med 14:270–275
Barber FA, Herbert MA (2000) Meniscal repair devices. Arthroscopy 16:613–618
Barber FA, Herbert MA, Richards DP (2004) Load to failure testing of new meniscal repair devices. Arthroscopy 20:45–50
Barrett GR, Treacy S, Ruff C (1997) Preliminary results of the T-fix endoscopic meniscus repair technique in an anterior cruciate ligament reconstruction population. Arthroscopy 13:218–223
Barrett GR, Richardson K, Ruff CG, Jones A (1997) The effect of suture type on meniscus repair. A clinical analysis. Am J Knee Surg 10:2–9
Borden P, Nyland J, Caborn DN, Pienkowski D (2003) Biomechanical comparison of the FasT-Fix meniscal repair suture system with vertical mattress sutures and meniscus arrows. Am J Sports Med 31:374–378
Brody JM, Lin HM, Hulstyn MJ, Tung GA (2006) Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology 239:805–810
Chang HC, Nyland J, Caborn DN, Burden R (2005) Biomechanical evaluation of meniscal repair systems: a comparison of the meniscal viper repair system, the vertical mattress FasT-Fix device, and vertical mattress ethibond sutures. Am J Sports Med 33:1846–1852
Chen NC, Martin SD, Gill TJ (2007) Risk to the lateral geniculate artery during arthroscopic lateral meniscal suture passage. Arthroscopy 23:642–646
Coen MJ, Caborn DN, Urban W, Nyland J, Johnson DL (1999) An anatomic evaluation of T-Fix suture device placement for arthroscopic all-inside meniscal repair. Arthroscopy 15:275–280
Cohen SB, Boyd L, Miller MD (2007) Vascular risk associated with meniscal repair using Rapidloc versus FasT-Fix: comparison of two all-inside meniscal devices. J Knee Surg 20:235–240
Espejo-Baena A, Figueroa-Mata A, Serrano-Fernández J, de la Torre-Solís F (2008) All-inside suture technique using anterior portals in posterior horn tears of lateral meniscus. Arthroscopy 24:369.e1-4
Gunes T, Bostan B, Erdem M, Asci M, Sen C, Kelestemur MH (2009) Biomechanical evaluation of arthroscopic all-inside meniscus repairs. Knee Surg Sports Traumatol Arthrosc 17:1347–1353
Haas AL, Schepsis AA, Hornstein J, Edgar CM (2005) Meniscal repair using the FasT-Fix all-inside meniscal repair device. Arthroscopy 21:167–175
Hospodar SJ, Schmitz MR, Golish SR, Ruder CR, Miller MD (2009) FasT-Fix versus inside-out suture meniscal repair in the goat model. Am J Sports Med 37:330–333
Kalliakmanis A, Zourntos S, Bousgas D, Nikolaou P (2008) Comparison of arthroscopic meniscal repair results using 3 different meniscal repair devices in anterior cruciate ligament reconstruction patients. Arthroscopy 24:810–816
Kocabey Y, Chang HC, Brand JC Jr, Nawab A, Nyland J, Caborn DN (2006) A biomechanical comparison of the FasT-Fix meniscal repair suture system and the Rapid Loc device in cadaver meniscus. Arthroscopy 22:406–413
Koenig JH, Ranawat AS, Umans HR, DiFelice GS (2009) Meniscal root tears: diagnosis and treatment; concise review with video illustration. Arthroscopy 25:1025–1032
Kotsovolos ES, Hantes ME, Mastrokalos DS, Lorbach O, Paessler HH (2006) Results of all-inside meniscal repair with the FasT-Fix meniscal repair system. Arthroscopy 22:3–9
Lee JH, Hwang BY, Lim YJ, Kim KH, Song JH (2009) Radial tears in the roots of the posterior horns of both the medial and lateral menisci combined with anterior cruciate ligament tear: a case report. Knee Surg Sports Traumatol Arthrosc 17:1340–1343
Lozano J, Ma CB, Cannon WD (2007) All-inside meniscus repair. Clin Orthop Relat Res 455:134–141
McCarty EC, Marx RG, DeHaven KE (2002) Meniscus repair: considerations in treatment and update of clinical results. Clin Orthop Relat Res 402:122–134
Miller MD, Kline AJ, Gonzales J, Beach WR (2002) Pitfalls associated with FasT-Fix meniscal repair; technical note. Arthroscopy 18:939–943
Morgan CD (1991) The “all-inside” meniscus repair. Arthroscopy 7:120–125
Noyes FR, Barber-Westin SD (2010) Repair of complex and avascular meniscal tears and meniscal transplantation. J Bone Joint Surg Am 92:1012–1029
Nyland J, Chang H, Kocabey Y, Nawab A, Brand J, Caborn DN (2008) A cyclic testing comparison of FasT-Fix and RapidLoc devices in human cadaveric meniscus. Arch Orthop Trauma Surg 128:489–494
Raheem O, Philpott J, Ryan W, O’Brien M (2007) Anatomical variations in the anatomy of the posterolateral corner of the knee. Knee Surg Sports Traumatol Arthrosc 15:895–900
Roos EM, Ostenberg A, Roos H, Ekdahl C, Lohmander LS (2001) Long-term outcome of meniscectomy: symptoms function, and performance tests in patients with or without radiographic osteoarthritis compared to matched controls. Osteoarthritis Cartilage 9:316–332
Stärke C, Kopf S, Petersen W, Becker R (2009) Meniscal repair. Arthroscopy 25:1033–1044
Seebacher JR, Inglis AE, Marshall JL, Warren RF (1982) The structure of the posterolateral aspect of the knee. J Bone Joint Surg Am 64:536–541
Staerke C, Brettschneider O, Gröbel KH, Becker R (2009) Tensile forces on sutures in the human lateral knee meniscus. Knee Surg Sports Traumatol Arthrosc 17:1354–1359
Zantop T, Eggers AK, Weimann A (2004) Initial fixation strength of flexible all-inside meniscus suture anchors in comparison to conventional suture technique and rigid anchors: biomechanical evaluation of new meniscus refixation systems. Am J Sports Med 32:863–869
Acknowledgments
This research was supported by Smith and Nephew Company by providing the Fast-Fix devices necessary to conduct this cadaveric study. The authors would like to thank Professor Hirohiko Aoyama PhD from The Anatomy and Developmental Biology Department, Graduate School of Biomedical Sciences, Hiroshima University, for allowing to perform this cadaveric study in his department and providing all of the possible facilities to conduct such study. The authors also would like to thank Professor Junko Tanaka PhD from the Department of Epidemiology and Infectious disease control, Graduate School of Biomedical Sciences Hiroshima University for performing the statistical analysis of this study.
Conflict of interest
The authors report no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abouheif, M.M., Shibuya, H., Niimoto, T. et al. Determination of the safe penetration depth during all-inside meniscal repair of the posterior part of the lateral meniscus using the FasT-Fix suture repair system. Knee Surg Sports Traumatol Arthrosc 19, 1868–1875 (2011). https://doi.org/10.1007/s00167-011-1489-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1489-x