Abstract
Tensile strength is the most often reported parameter in biomechanical investigations of meniscal repair techniques. However, the magnitude of the tensile forces that actually occur on repaired lesions is not clear. The purpose of this study was to investigate if tensile forces occur on repaired lateral meniscal lesions, which could exceed the failure strength of common repair techniques. In human knees (n = 6), vertical-longitudinal lesions 25 mm in length were created in the posterior horn of the lateral meniscus at a distance of 3 mm from the meniscosynovial junction and the popliteal hiatus. A braided steel wire, resembling a vertical suture, was inserted into the meniscal tissue and fitted with a force transducer. The knees were mounted in an apparatus, which simulated weight bearing and non-weight bearing conditions. Repeated measurements were conducted with both internal and external rotation at flexion angles of 0°, 30°, 60°, 90° and 120°. Weight loading alone caused no tension on the suture. Combined flexion and rotation generated mean forces between 0.5 and 4.1 N. No significant effect of the flexion angle or direction of rotation was found. If a minimum strength of 10 N was assumed for the common meniscal repair techniques, the tensile forces were well below this limit under all circumstances (P < 0.001). These data indicate that, within the range of motion investigated, no significant tensile forces occur on longitudinal lateral lesions. Forces other than tension and biological factors are of greater importance for the healing. Therefore, the assessment of repair techniques should not be based on alone the ability to resist high distraction forces.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Current knowledge suggests that meniscal repair is preferred to meniscectomy if feasible [1]. A multitude of suture techniques and implants to facilitate easy repair were developed in recent years. The strength of fixation is the most often reported parameter in biomechanical studies comparing repair techniques [2, 3, 6]. Intuitively, a higher strength would be associated with better results. However, it has not been established that the strength of fixation is indeed a predictor of clinical success. Barbed rigid implants or implants of the screw type fail at loads that are substantially less than those reported for suture repair [4]. Nevertheless, intermediate term results indicate that the clinical success rates are not different between the techniques [19]. Thus, the question arises, which significance should be attributed to the strength of fixation.
Findings suggest that the tensile forces that occur postoperatively are not large enough to cause meniscal tears or failure of a repair. A positive pressure was found in lateral meniscal tears throughout the range of motion in a human in vitro study, which indicates that no distraction of the tear occurs [13]. However, no tibio-femoral compression was applied in this investigation, which may affect the results. A study on distraction forces in medial meniscal lesions reported forces of less than 5 N with flexion angles of up to 120° [5]. Results from the medial compartment cannot be extrapolated to the lateral side because of differences in the anatomy and kinematics [10, 12]. Direct measurements of the tension acting on sutures in lateral menisci have not been reported in literature so far.
The purpose of the study was to directly measure tensile forces, which are generated on lateral meniscal sutures in a human model and to assess whether or not they exceed the failure strength of contemporary repair techniques. Our hypothesis was that the tensile forces acting on sutures in lateral longitudinal lesions of the meniscus are in a range that is below the failure strength of common repair techniques.
Materials and methods
Human knees from donors at a mean age of 43 years were obtained for the tests (median age 35 years, range 28–68 years). The knees had been frozen immediately after harvest and were thawed at room temperature 24 h prior to the experiments. Overlying skin and muscle tissues were removed while taking care not to damage the knee ligaments. The proximal fibula and the tibio-fibular joint were left intact to retain lateral stability.
A protocol similar to that used by Becker et al. [5] in a study on medial meniscal lesions was used. To gain access to the lateral meniscus, the lateral collateral ligament was detached with its bony insertion from the femur using an oscillating saw with a semi-circular blade (Aesculap; Tuttlingen, Germany). The capsule ventral to the ligament was longitudinally dissected. This approach allowed for a sufficient exposure of the meniscus to do the necessary manipulations. It was shown that an osteotomy and reattachment of the medial femoral epicondyle does not alter the menisco-femoral contact mechanics [11].
Using a scalpel, a full-thickness, vertical-longitudinal lesion with a length of 25 mm was created in the posterior part of the meniscus at a distance of 3 mm from the menisco-synovial junction and the popliteal hiatus.
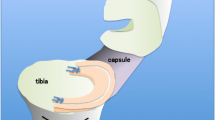
Then, a highly flexible, braided steel wire (diameter 0.35 mm, nominal breaking load 68 N) was inserted into the meniscal tissue, resembling a vertical suture. In the outer segment, both branches of the wire were led through a small steel tube (diameter 0.9 mm), the length of which was adjusted to meet the thickness of the meniscal segment (Fig. 1). The inner diameter of the tube was appropriately sized to let the wire just pass through, thereby eliminating friction of the wire in the outer segment. Finally, the bony insertion of the collateral ligament was anatomically re-attached, using a 6.5 mm cancellous screw with a spiked washer. The capsule was closed with strong sutures.
The meniscus with the force transducer in place. A steel wire (a) is anchored in the inner segment (b) of the meniscus. The wire is led through a small tube (c) in the outer segment (d) to eliminate friction. A small-sized force sensor (e) is borne on the back of the meniscus. Distraction forces are transferred to the sensor via the wire. Strain gauges (f)
The steel wire left the meniscus dorsally. At this site, the capsule was longitudinally dissected down to the back of the meniscus, while taking care not to damage the structural integrity of the dorsal ligamentous structures. A custom-made, miniature load sensor was placed directly on the meniscus periphery (Fig. 1). The base of the sensor, which faced the meniscal periphery dorsally, was shaped to fit between the tibial and femoral condyle. Then, the steel wire was rigidly connected to the transducer, thereby transferring tensile forces to the sensor (Fig. 1). A screw allowed adjusting the pretension of the wire. This small-sized force transducer was based on a lightweight, circular aluminum frame, instrumented with four active strain gauges, which were wired as a full bridge.
A dedicated apparatus was constructed to load the knees in a manner similar to in vivo conditions. First, the femur and the tibia were potted into steel cylinders using acrylic cement (Biomet; Warsaw, IN, USA). Both ends were fitted with an extension to gain a length of 45 cm on each side. This length was chosen to account for the average length of the lower leg and femur, respectively [17].
The tibial part was mounted to a steady base in a way that it could rotate freely about its long axis and be flexed from 0° to 90° in a sagittal direction at the height of the ankle joint (Fig. 3).
Loading apparatus. The proximal femur is loaded with 300 N (a) or left unloaded. The length of the “extensor system” (b) determines the flexion angle (c). The tibia can be rotated along its long axis (d). Note that the input load is amplified due to the lever effect of the femur and the resultant tibio-femoral contact forces reach a multiple of the input depending on the flexion angle
The quadriceps tendon was grasped with a cryo-clamp [14]. Controlled evaporation of CO2 was used to cool the clamp down and to keep the tendon frozen and securely fixed within the clamp. This clamp was connected proximally to the femoral part of the construction. The distance between the clamp and the proximal attachment site was adjustable, which allowed controlling the length of the extensor system and the flexion angle, as realized in vivo by the quadriceps muscle. The length adjustment was done manually and did not allow for dynamic changes. Instead, distinct angles were tested successively.
At a distance of 45 cm from the knee joint, which represents approximately the distance of the hip from the knee [17], the femoral part of the construction was loaded with up to 300 N. This load was chosen as an estimate of the weight that acts on the hip of an average person with a bi-pedal stance (70 kg divided by two, less the weight of the leg itself).
It must be emphasized that this load represents not the tibio-femoral contact forces. The tibio-femoral forces equal the input load only in the case of zero degrees of flexion, when the weight is centered upon the knee. With increasing flexion, the net forces in the knee reach a multiple of the input load of 300 N due to the lever effect. This approach allows a near-physiological loading of the knee with realistic tibio-femoral forces [7, 18].
A handle with an integrated torque sensor was mounted on the tibial side and used to manually rotate the tibia internally and externally. The flexion–rotation was thus realized with a static flexion component and dynamic torsion. A torque slightly higher than 5 N was chosen to approximate a magnitude that occurs with activities of daily living. This value is based on estimations, which are derived from studies by Komistek et al. and Shoemaker et al. [10, 15].
In order to avoid a tilting moment, a supporting frame was constructed to keep the loading mass centered upon the distal bearing. The signals from the force and torque transducer were sampled at a frequency of 100 Hz using a multi-channel A/D converter/amplifier (Spider8, HBM; Darmstadt, Germany) and logged to a file.
After setting up the sensor and data acquisition system, five different angles of flexion (0°, 30°, 60°, 90° and 120°), two states of loading (0 and 300 N) and two directions of rotation (internally/externally) were investigated in successive sets, giving a total of 20 distinct combinations. Every measurement was repeated 10 times for each knee.
The measurement setup was validated on explanted menisci (n = 6) in a pilot investigation. These specimens were prepared with an artificial tear and the sensor and wire were installed as described above. A slight pretension was applied. The peripheral part of the meniscus was fixed and the central part was then incrementally loaded with gauged weights in the region of the tear. It was found that the setup allowed measuring the true load across the tear with a mean deviation better than 2% (Fig. 2).
Statistical methods
For further analysis, data were converted to a Microsoft Excel (Microsoft; Redmond, WA, USA)-compatible format. A Visual Basic script was used to detect the load cycles and to identify the distraction forces corresponding to a torque of 5 N. The software package SPSS v11.0 (SPSS Inc.; Chicago, IL, USA) was used for statistical analysis.
Due to the high forces generated in the extensor mechanism, a premature failure occurred in four knees. In these cases, only an incomplete set of data could be acquired, leaving six knees for the statistical analysis.
In order to assess the clinical significance of the tensile forces measured, it was a major goal of the study to relate those forces to the strength of common repair techniques. Although a trend toward suture-based all inside systems is observable, which reach failure loads in a range of conventional sutures, devices with a low pullout strength such as screws or barbed pins are still in use. Tensile failure loads as low as 9.5 N were reported in human knees for those implants [4]. Therefore, tensile forces of 10 N are considered the lower limit of a clinical significance in this investigation. A t test was conducted against this hypothetical boundary of 10 N using the pooled data from all knees. Further, a repeated measures ANOVA (factors: flexion angle, weight, direction of tibial rotation) was run on the data. Significance was assumed at P ≤ 0.05.
Results
Weight loading alone had no significant effect on the tension generated in the suture. Additional torsion of the tibia was accompanied by a corresponding increase of the measured tensile force. Figure 4 shows a representative example of the raw data as gained from the torque and tensile force sensors. As mentioned in “Materials and methods”, the tensile force that corresponded to a tibial torque of 5 Nm was used. A trend was noted that internal rotation of the tibia, a situation in which the femur translates posteriorly and displaces the meniscus, increased the resultant tension in the suture compared to external tibial rotation. Depending on the flexion angle, the resultant suture tension reached 3.0–4.1 N with weight loading and 1.5–2.7 N without weight loading in internal rotation. In external rotation, tensile forces between 0.5–3.5 N and 0.6–1.5 N were measured for the same conditions. However, the differences did not reach statistical significance.
The ANOVA did not demonstrate a significant effect of the flexion angle on the resultant tension in the suture. Visual examination of the data did not reveal a conclusive pattern in terms of a potential effect of flexion.
Table 1 gives means and standard deviations of the measured tension in internal and external rotation with and without weight loading, respectively. The average tensile forces acting on the suture did not exceed 4.1 N under all conditions. Comparing the pooled data from all measurements against the assumed level of clinical relevance (10 N), it was found that the mean tensile forces acting on the suture were highly significantly less than this value (P < 0.001, 99% confidence interval of mean difference: −8.29 ≤ M d ≤ −7.24).
Discussion
The most important finding of the study was that within the range of motion and loads investigated here, no clinically significant tensile forces acting on the sutures could be found. Ancillary tests did prove that the setup allowed measuring artificially applied tensile forces on vertical sutures accurately. The results are in line with investigations that addressed the same problem using different approaches:
Only a minor gapping was found in porcine medial menisci under axial load and tibial torsion, which indicates that no significant tension would be generated [8]. In human knees, a positive pressure was found throughout the range of motion in both, medial and lateral menisci that, again, indirectly suggests that no distraction of the tear and hence no substantial tension on sutures occur [13]. Studies addressing tensile forces in medial meniscal lesions reported forces less than 10 N [5].
Hence, neither our own results nor the current literature provide evidence that relevant tensile forces occur on meniscal sutures or implants under postoperative conditions. This has implications for clinical practice as well as for research:
A particularly high failure strength in the axis of insertion should not be the principal criterion on which the choice of the repair technique is based. Biomechanical studies do not imply that a high failure load is necessary. Clinical studies could not prove a correlation of the outcome to the failure strength of the repair technique used. Safety, ease of use and potential for secondary morbidity are probably equally important.
It was shown in an in vitro study that tibio-femoral compression in conjunction with forceful flexion and torsion of the knee can cause vertical-longitudinal lesions [16]. The knees were twisted maximally in this study, while we used only a moderate torque. It seems reasonable to assume that either a particular forceful twisting and flexion is necessary or that special circumstances are essential to produce a distraction of the meniscal fragments. Moderate, controlled motion of the knee, as practiced postoperatively, is not likely to cause substantial distraction forces. Our data suggest that weight bearing alone is not critical to repaired lesions in terms of mechanical effects. This is supported by structure–function considerations, which imply that weight load induces radial forces in the meniscus, rather reducing a vertical-longitudinal tear [9]. Both, tibial rotation as well as flexion of the knee, are accompanied by a coupled motion of the meniscus. The shape of the contacting surfaces changes, depending on the degree of flexion or direction of tibial rotation. Therefore, the meniscus experiences a deformation, which gives rise to shear forces within the tissue. On repaired longitudinal tears, this will cause tension on the repair material. Most likely, the tensile forces measured in our study are explained by those shear motions between the meniscal fragments and are not necessarily caused by a distraction of the tear margins.
In biomechanical research, the value of the tensile failure load as the prime parameter to compare meniscal repair techniques must be questioned. The significance of shear forces has been insufficiently addressed in biomechanical studies of the knee meniscus. Probably, shear forces play a role in the development of vertical-longitudinal lesions. However, so far it has not been established, under which circumstances shear forces are generated. It seems worthwhile to shift the focus of future studies toward shear forces instead of tensile forces.
The presented study has several limitations. First, the flexion component was only static and limited to a maximum of 120°. Specifically, deep flexion might increase the stress at the meniscus. The effective sample size in this study was small, which limits possible inferences. It would be of particular interest if shear stress is generated within the meniscus under the applied conditions. This, however, has not been specifically addressed in this study and deserves attention in future experiments. Further, tears larger than investigated in the presented study could be less stable and give rise to higher tensile forces then found in our experiments.
Nevertheless, the data indicate that rehabilitation protocols with moderate range of motion exercises and weight bearing would not jeopardize the stability of repaired longitudinal lesions of the lateral meniscus.
Conclusions
Under the conditions investigated in the present study, the tensile forces acting on sutures in lateral longitudinal lesions are significantly lower than the failure strength of common repair techniques. Tibio-femoral compression alone does not cause tension across the tear.
References
Alford JW, Lewis P, Kang RW, Cole BJ (2005) Rapid progression of chondral disease in the lateral compartment of the knee following meniscectomy. Arthroscopy 21:1505–1509
Aşík M, Sener N (2002) Failure strength of repair devices versus meniscus suturing techniques. Knee Surg Sports Traumatol Arthrosc 10:25–29
Barber FA, Herbert MA (2000) Meniscal repair devices. Arthroscopy 16:613–618
Becker R, Schröder M, Stärke C, Urbach D, Nebelung W (2001) Biomechanical investigations of different meniscal repair implants in comparison with horizontal sutures on human meniscus. Arthroscopy 17:439–444
Becker R, Brettschneider O, Gröbel K, von Versen R, Stärke C (2006) Distraction forces on repaired bucket-handle lesions in the medial meniscus. Am J Sports Med 34:1941–1947
Chang HC, Nyland J, Caborn DNM, Burden R (2005) Biomechanical evaluation of meniscal repair systems: a comparison of the Meniscal Viper Repair System, the vertical mattress FasT-Fix Device, and vertical mattress ethibond sutures. Am J Sports Med 33:1846–1852
Dahlkvist NJ, Mayo P, Seedhom BB (1982) Forces during squatting and rising from a deep squat. Eng Med 11:69–76
Dürselen L, Hebisch A, Claes LE, Bauer G (2003) Gapping phenomenon of longitudinal meniscal tears. Clin Biomech (Bristol, Avon) 18:505–510
Fithian DC, Kelly MA, Mow VC (1990) Material properties and structure–function relationships in the menisci. Clin Orthop Relat Res 252:19–31
Komistek RD, Dennis DA, Mahfouz M (2003) In vivo fluoroscopic analysis of the normal human knee. Clin Orthop Relat Res 410:69–81
Martens TA, Hull ML, Howell SM (1997) An in vitro osteotomy method to expose the medial compartment of the human knee. J Biomech Eng 119:379–385
McDermott ID, Sharifi F, Bull AMJ, Gupte CM, Thomas RW, Amis AA (2004) An anatomical study of meniscal allograft sizing. Knee Surg Sports Traumatol Arthrosc 12:130–135
Richards DP, Barber FA, Herbert MA (2008) Meniscal tear biomechanics: loads across meniscal tears in human cadaveric knees. Orthopedics 31:347–350
Riemersa DJ, Schamhardt HC (1982) The cryo-jaw, a clamp designed for in vitro rheology studies of horse digital flexor tendons. J Biomech 15:619–620
Shoemaker SC, Markolf KL (1982) In vivo rotatory knee stability: ligamentous and muscular contributions. J Bone Joint Surg Am 64:208–216
Stewart JP, Erskine CA (1979) An experimental analysis of injuries to the menisci of the knee joint. Int Orthop 3:9–12
Strecker W, Keppler P, Gebhard F, Kinzl L (1997) Length and torsion of the lower limb. J Bone Joint Surg Br 79:1019–1023
Thambyah A, Pereira BP, Wyss U (2005) Estimation of bone-on-bone contact forces in the tibiofemoral joint during walking. Knee 12:383–388
Spindler KP, McCarty EC, Warren TA, Devin C, Connor JT Prospective comparison of arthroscopic medial meniscal repair technique: inside-out suture versus entirely arthroscopic arrows. Am J Sports Med 31:929–934
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Staerke, C., Brettschneider, O., Gröbel, KH. et al. Tensile forces on sutures in the human lateral knee meniscus. Knee Surg Sports Traumatol Arthrosc 17, 1354–1359 (2009). https://doi.org/10.1007/s00167-009-0875-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-009-0875-0