Abstract
Purpose
The purpose of this study was to propose an objective description of femoral tunnel position expressed as time of the intercondylar clock in ACL reconstruction using a simple radiograph for the sake of objective discussion and technical improvement. The reproducibility of the method was evaluated in double-bundle (DB) reconstructions.
Methods
The first series of 54 knees in 54 patients who underwent primary “isometric” DB ACL reconstructions from 1995 to 2002 were randomly picked up. The second series of 48 knees in 48 patients with primary “anatomic” DB ACL reconstructions during 2007 were assessed as a recent femoral tunnel position with the same method. All DB reconstructions of ACL with the anteromedial (AM) and posterolateral (PL) bundles were performed with an arthroscopically assisted trans-tibial technique. The o’clock description of femoral tunnel placement was expressed using a weight-bearing posterior–anterior view at 45° of flexion (45° W/B PA view) of the knee. Assessment was undertaken with radiographs 1 year postoperatively.
Results
The o’clock descriptions of femoral tunnel placement resulted in noon 40 min (standard deviation (SD): 10 min) for the AM bundle and one o’clock 40 min (SD: 20 min) for the PL bundle on average in the “isometric” reconstruction. In the “anatomic” reconstruction, the time descriptions of femoral tunnel placement were one o’clock 20 min (SD: 10 min) for the AM bundle and two o’clock 20 min (SD: 20 min) for the PL bundle on average. With the intra-examiner reproducibility assessment in the “anatomic” reconstruction, the differences between first and second assessments averaged 10 min (SD: 7 min) for femoral tunnel placement of the AM bundle and 12 min (SD: 9 min) of the PL bundle. Regarding the inter-examiner reproducibility, the differences between two examiners averaged 9 min (SD: 6 min) for femoral tunnel placement of the AM bundle and 14 min (SD: 9 min) of the PL bundle.
Conclusion
This simple radiographic assessment is reproducible and reliable for clinical use, and useful for the evaluation of ACL reconstructive procedures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Any ligament surgeon will agree that accurate placement of the femoral and tibial tunnels is very important to achieve good outcome of anterior cruciate ligament (ACL) reconstruction. Anatomic placement of the tunnels has been emphasized as an important factor to achieve better stability and to restore normal kinematics in ACL-reconstructed knees, especially in double-bundle (DB) reconstructions [22, 26].
For the description of tibial tunnel placement, Howell et al. radiographically described tibial tunnel placement in the sagittal plane of the knee and documented that pathologic roof impingement was prevented when the entire width of the tibial tunnel was posterior to the slope of the intercondylar roof [7, 8]. However, based on the recent anatomical observations, the concept of roof impingement itself has been changed. Petersen et al. described that the normal ACL accepts “physiologic” roof impingement at the tibial attachment [19]. In the coronal plain, Muneta et al. reported that the medial intercondylar spine could be the radiographic marker for the tibial drill hole position [15].
For the description of femoral tunnel placement, the quadrant method has been found practical in sagittal plain [3, 4, 25]. In coronal plain, intercondylar o’clock description has been frequently used during arthroscopic procedures by many surgeons and documented in many textbooks [1, 11, 13, 14, 18]. However, this description of femoral tunnel placement in the coronal plain is arthroscopically determined based mainly on the subjective impression of surgeons. Although the placement of the femoral tunnel is important, the o’clock description of femoral tunnel placement in the coronal plain has not been well defined in the past literature. Some definitive descriptions of the time in the intercondylar clock would be useful for surgeons to better discuss and understand the femoral tunnel placement in each other’s ACL reconstructions.
In this study, we propose a new objective o’clock description of femoral tunnel placement with a simple radiograph in “isometric” DB hamstring ACL reconstructions [16]. Then, the recent femoral tunnel placement of “anatomic” DB ACL reconstruction [17, 23] was prospectively assessed using the proposed intercondylar o’clock description. The hypothesis of the current study is that the o’clock description is useful and reproducible, and applicable for both the “isometric” and the “anatomic” DB ACL reconstructions.
Materials and methods
First radiography sets from 54 knees in 54 patients who underwent a primary “isometric” DB ACL reconstruction from 1995 to 2002 in Tokyo Medical and Dental University Hospital were retrospectively picked up with a randomized fashion and included in this study. The knee joint radiographs including a weight-bearing posterior–anterior view at 45° of flexion (45° W/B PA view) advocated by Rosenberg et al. [20] were routinely taken at 3 months and every 1 year after ACL reconstruction in our hospital from 1995 to present. For inclusion and exclusion criteria, knees with a clearly identifiable femoral and tibial tunnel placement radiographs were included in this study. Knees in which it was difficult to identify either tibial or femoral tunnel placement or radiographic evidence of degenerative arthritis were excluded. The subjects of the first series included 28 men and 26 women, and the median age of the patients was 23 years (range, 15–44 years).
As the second part of the study, radiography sets from 52 knees in 52 patients who underwent a primary “anatomic” DB ACL reconstruction in 2007 in the same hospital were prospectively and consecutively picked up using the proposed intercondylar o’clock description. The subjects of the second series included 23 men and 29 women, and the median age of the patients was 21 years (range, 14–53 years).
The DB ACL reconstruction was performed with an arthroscopically assisted trans-tibial technique using a 4-strand semitendinosus tendon. The AM bundle was positioned aimed at around noon 30 min, and the PL bundle at around one o’clock 30 min with reference to the posterior intercondylar notch. The tunnel position was determined according to the concept of “isometric” reconstruction [16]. O’clock determination during surgery was arthroscopically done at about 70° knee flexion. The operative concept of our DB ACL reconstruction has been changed to “anatomic” reconstruction from 2002 to consider more about the normal ACL anatomy in our hospital [17, 23]. The AM bundle was positioned at around one o’clock 30 min and the PL bundle at around 3 o’clock with reference to the posterior intercondylar notch during 2007 period.
O’clock description of femoral tunnel placement
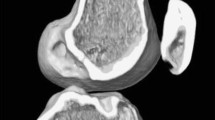
A radiographic objective o’clock description of the femoral tunnel position had been developed as follows. A weight-bearing posterior–anterior view at 45° of flexion (45° W/B PA view) of the knee was taken according to Rosenberg’s report [20] (Fig. 1). The radiographs of the contralateral knees were routinely taken with a 45° W/B PA view at the same time simultaneously, and the contralateral, asymptomatic knee could be evaluated as a control. From this simple radiograph, the o’clock description of the femoral tunnel placement was expressed and defined as intercondylar clock time. The clock was drawn between the two lines as follows. One line connected the distal edges of the medial and lateral femoral condyles. The other was parallel to the previous line through the top of the posterior intercondylar notch (Fig. 2). The center of the femoral tunnel was marked as the cross-point of the intercondylar clock and the femoral tunnel extension of the 4.5-mm tunnel outside the joint to the lateral cortex. The line connecting the center of the clock and the cross-point above was expressed as time shown on the clock.
O’clock description of the femoral tunnel placement in the intercondylar clock was defined on the weight-bearing posterior–anterior view at 45° of flexion of the knee. The clock was drawn between the two lines. One line connected the distal edges of the medial and lateral femoral condyles. The other was parallel to the previous line through the top of the posterior intercondylar notch. After the center of the femoral tunnel opening was marked, the line connecting the center of the clock and the cross-point between the clock and the extension of the femoral tunnel to the joint was described as time shown on the clock
When the tunnel widening is found or two tunnels are overlapped, two options will be considered to determine the tunnel position. One is to point out the center of the tunnel opening to the joint by an examiner’s impression, and the other is to select the point of extension of the mid-line of femoral drill hole to the lateral femoral cortex. In this study, o’clock description for each AM and PL bundle was respectively made using the latter method. The latter method is thought to be more accurate and reproducible. However, the real tunnel position changed by tunnel widening at the o’clock of measurements is not well taken into consideration. All the knees were assumed to be left knees, and the time was described as one o’clock 30 min or two o’clock 40 min, for example, by converting each angle for each AM and PL bundle.
Reproducibility and repeatability of o’clock description of the method
The o’clock description of the AM bundle and the PL bundle was performed by three examiners who were not involved in every surgery. Two were orthopedic fellows and the other was an orthopedic resident. In 20 knees out of 48 subjects, o’clock measurement of the AM and PL bundles was performed twice by a fellow examiner, and the intra-examiner reproducibility was assessed. Dependent upon 20 knees out of 48 subjects of the second series, the inter-examiner reproducibility was assessed by two examiners. In fifteen knees out of 54 subjects of the first series, the radiographs were taken twice, at 1 year and again at 2 years postoperatively, and the repeatability between the two radiographs at the different times was assessed. The difference in the o’clock was described as an absolute value of angle to each tunnel and then converted to o’clock description. The reproducibility and repeatability of the measurements were described by minutes of the differences. Using the second series of the radiographs, the usability of the method was also evaluated. The number of the radiograph, which was unable for the examiner to express the o’clock description because of poor image quality, was counted.
Statistical analysis
Statistical analysis regarding the reproducibility and repeatability between AM and PL bundles was carried out using the unpaired t test with a significance established at P < 0.05. The StatView for Windows (version 5.0) was used for the statistical evaluation (SAS Institute Inc., Cary, NC, USA).
Results
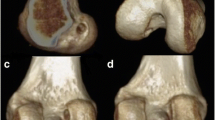
O’clock description of femoral tunnel placement
The o’clock descriptions of femoral tunnel placement of the “isometric” reconstruction resulted in noon 40 min (SD: 10 min) for the AM bundle and o’clock 40 min (SD: 20 min) for the PL bundle on average. In the second series of the radiographic evaluation, the o’clock descriptions of femoral tunnel placement of the “anatomic” reconstruction resulted in one o’clock 20 min (SD: 10 min) for the AM bundle and two o’clock 20 min (SD: 20 min) for the PL bundle (Fig. 3).
A magnified image of Fig. 2. The o’clock description of femoral tunnel placement was 1:10 for AM bundle and 2:30 for PL bundle in this case
Reproducibility and repeatability of the description and usability of the method
The evaluation results using the “anatomic” reconstruction were summarized in the Table 1. The inter-examiner reproducibility of the o’clock description for the PL bundle was inferior. For the assessment of the repeatability between the two radiographs at the different times, 48 radiographs out of 52 (92%) were found to be sufficiently clear for the time description.
Discussion
The most important finding of the present study was that o’clock description of femoral tunnel based on a 45° W/B PA view in DB ACL reconstruction advocated by the current study is easy and reproducible both in “isometric” and in “anatomic” reconstructions. The hypothesis of the current study was elucidated although there are several problems and limitations for clinical use as below.
In respect to the description of femoral tunnel placement in the coronal plane, the use of o’clock description has been frequently applied [1, 11, 13, 14, 18]. However, the definition of the femoral tunnel time has not been well described. Howell et al. described the femoral tunnel placement as “an imaginary clock” [9]. Petersen and Zantop [19] have already described the center of the femoral attachment of both AM bundle and PL bundle of the normal ACL using a 45° W/B PA view. The center of the femoral AM bundle was described at the 10:30 position, while the femoral PL center was at the 9:30 position. However, the intercondylar clock was not a clock, but a semicircle in the study. The arthroscopic o’clock position reference has been reported by Giron et al. [5]. The definition of the clock is not well described. From the drawing, they seemed to set the clock in the posterior intercondylar notch. In their clock definition, the accurate description is not possible because the natural femoral attachment of the PL bundle expands shallower and out of the clock in the lower direction in flexion position.
As the o’clock is described by a 45° W/B PA view, the absolute time is inevitably different from the time description made arthroscopically. The value tends to be earlier, time near to noon, than the arthroscopically determined time. In the “isometric” reconstruction, the difference between the average radiographic value and the aiming time arthroscopically was well correlated with aimed o’clock both for the AM and PL bundles, while the difference was 10 min for the AM bundle and 40 min for the PL bundle in the “anatomic” reconstruction. However, the real accuracy of the current o’clock description cannot be evaluated because the arthroscopic placement itself has not been well evaluated or controlled. Regarding the central position of AM and PL bundles, Colombet et al. reported the natural ACL anatomy and radiographic description using the methods followed Amis and Jakob on the tibia and the grid prepared by Bernard et al. on the femur [4]. Steckel and Fu et al. evaluated the femoral insertion of the AM and PL bundles of the normal ACL by a radiographic method at different knee flexion angles [21]. However, both results of the normal morphology of AM and PL bundles were not directly imagined to describe arthroscopic o’clock position.
With thinking about how accurate to describe the tunnel position by the current method, the outlets to the joint of the two tunnels were found overlapped in the majority of the radiographs at 1 year postoperatively. Therefore, to use the extension line of the mid-line of the femoral tunnel outside the joint to the lateral femoral cortex is thought to be practical and reproducible for the current radiographic method. The o’clock description using the current method is accepted in 10-min increment based on the intra- and inter-reproducibility, and repeatability evaluation. Even in cases with interference screw fixation, the lateral tunnel position and the screw position will help describing the tunnel position correctly. Original tunnel position is easily describable with reference to the drill hole position outside the joint to lateral femoral cortex. Also, the same description can be applied in the cases with bone tunnel enlargement or with obscure tunnel margin by low bone density. However, the center of enlarged bone tunnel or overlapped bone tunnels will be hard to describe accurately with the plain radiography.
The advantages of this assessment are that this radiograph can be taken easily and included as routine radiographs without a CT or MRI. On the other hand, in the sense of accurate description fit to intraoperative determination, an intercondylar tunnel view of the knee at 70° flexion [24] or CT evaluation [2, 6, 10, 12] can be better used for the assessment of femoral tunnel. With the use of CT images, any flexion angle can be applied to determine the femoral tunnel position, but repeated evaluation with CT images will be less desirable in respect to radiation exposure, cost, and time consumption. Another limitation of the study is that there is no standard for accurate description methods of tunnel placement. The standard methods should be discussed to create in the future. There may be large individual differences in each center of AM and PL portions in normal knees. Or, there may be a good correlation of the posterior intercondylar notch shape and each normal ACL anatomy. Those detailed investigations will be a future study.
As the clinical relevance, this description of the femoral tunnel can be of great value when the surgical procedures and the results are analyzed retrospectively or the effect of femoral tunnel change is intended to be evaluated using routine radiographs. It will be applicable for every surgeon to discuss tunnel placement in ACL reconstruction as a standard method.
Conclusion
O’clock description of femoral tunnel position on the posterior intercondylar clock using the 45° W/B PA view is simple, practical, and reproducible both in the “isometric” and in the “anatomic” double-bundle ACL reconstructions. The assessment will be useful for describing tunnel position in ACL reconstructions in conjunction with clinical results.
References
Aglietti P, Giron F (2001) Anterior cruciate ligament reconstruction for chronic injuries. In: Insall JN, Scott WN (eds) Surgery of the knee, 3rd edn. Churchill and Livingstone, Philadelphia, pp 717–787
Basdekis G, Christel P, Anne F (2009) Validation of the position of the femoral tunnels in anatomic double-bundle ACL reconstruction with 3-D CT scan. Knee Surg Sports Traumatol Arthrosc 17:1089–1094
Bernard M, Hertel P, Hornung H, Cierpinski T (1997) Femoral insertion of the ACL. Radiographic quadrant method. Am J Knee Surg 10:14–21
Colombet P, Robinson J, Christel P, Franceschi JP, Djian P, Bellier G, Sbihi A (2006) Morphology of anterior cruciate ligament attachments for anatomic reconstruction: a cadaveric dissection and radiographic study. Arthroscopy 22:984–992
Giron F, Cuomo P, Aglietti P, Bull AM, Amis AA (2005) Femoral attachment of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 14:250–256
Hoser C, Tecklenburg K, Kuenzel KH, Fink C (2005) Postoperative evaluation of femoral tunnel position in ACL reconstruction: plain radiography versus computer tomography. Knee Surg Sports Traumatol Arthrosc 13:256–262
Howell SM, Clark JA, Farley TE (1991) A rationale for predicting anterior cruciate graft impingement by the intercondylar roof. A magnetic resonance imaging study. Am J Sports Med 19:276–282
Howell SM, Taylor MA (1993) Failure of reconstruction of the anterior cruciate ligament due to impingement by the intercondylar roof. J Bone Joint Surg 75A:1044–1055
Howell SM, Gittins ME, Gottlieb JE (2001) The relationship between the angle of the tibial tunnel in the coronal plane and loss of flexion and anterior laxity after anterior cruciate ligament reconstruction. Am J Sports Med 29:567–574
Inoue M, Tokuyasu S, Kuwahara S, Yasojima N, Kasahara Y, Kondo E, Onodera S, Yasuda K (2009) Tunnel location in transparent 3-dimensional CT in anatomic double-bundle anterior cruciate ligament reconstruction with the trans-tibial tunnel technique. Knee Surg Sports Traumatol Arthrosc [Epub ahead of print]
Johnson D (2001) Anterior cruciate ligament reconstruction with semitendinosus. In: Insall JN, Scott WN (eds) Surgery of the knee, 3rd edn. Churchill and Livingstone, Philadelphia, pp 693–710
Lorenz S, Elser F, Mitterer M, Obst T, Imhoff AB (2009) Radiographic evaluation of the insertion sites of the 2 functional bundles of the anterior cruciate ligament using 3-dimensional computed tomography. Am Sports Med 37:2368–2376
Manifold SG, Cushner FD, Scott WN (2001) Anterior cruciate ligament reconstruction with bone-patellar- tendon-bone autograft: indications, technique, complications, and management. In: Insall JN, Scott WN (eds) Surgery of the knee, 3rd edn. Churchill and Livingstone, Philadelphia, pp 665–680
Mologne TS, Friedman MJ (2001) Arthroscopic Anterior cruciate reconstruction with Hamstring tendons: indications, surgical technique, complications, and their treatment. In: Insall JN, Scott WN (eds) Surgery of the knee, 3rd edn. Churchill and Livingstone, Philadelphia, pp 681–692
Muneta T, Yamamoto H, Ishibashi T (1995) The effects of tibial tunnel placement and roofplasty on reconstructed anterior cruciate ligament knees. Arthroscopy 11:57–62
Muneta T, Sekiya I, Yagishita K (1999) Two-bundle reconstruction of the anterior cruciate ligament using semitendinosus tendon with endobuttons: operative technique and preliminary results. Arthroscopy 15:618–624
Muneta T, Koga H, Mochizuki T, Ju YJ, Nimura A, Yagishita K, Sekiya I (2007) A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy 23:618–628
Nogalski MP, Bach BR Jr (1994) Acute anterior cruciate ligament injuries. In: Fu FH, Harner CD, Vince KG (eds) Knee surgery. Williams and Wilkins, Baltimore, pp 679–730
Petersen W, Zantop T (2007) Anatomy of the anterior cruciate ligament with regard to its two bundles. Clin Orthop Relat Res 454:35–47
Rosenberg TD, Paulos LE, Parker RD (1988) The forty-five-degree posteroanterior flexion weight-bearing radiograph of the knee. J Bone Joint Surg 70A:1479–1482
Steckel H, Musahl V, Fu FH (2010) The femoral insertion of the anteromedial and posterolateral bundles of the anterior cruciate ligament: a radiographic evaluation. Knee Surg Sports Traumatol Arthrosc 18:52–55
Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL (2002) Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med 30:660–666
Yasuda K, Kondo E, Ichiyama H, Kitamura N, Tanabe Y, Tohyama H, Minami A (2004) Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon graft. Arthroscopy 20:1015–1025
Yoo JH, Yi SR, Son BK (2008) The prone kneeling view of the intercondylar notch for radiographic assessment of the femoral tunnel position in anterior cruciate ligament reconstruction. Arthroscopy 24:465–471
Zantop T, Wellmann M, Fu FH, Petersen W (2008) Tunnel positioning of anteromedial and posterolateral bundles in anatomic anterior cruciate ligament reconstruction: anatomic and radiographic findings. Am J Sports Med 36:65–72
Zantop T, Diermann N, Schumacher T, Schanz S, Fu FH, Petersen W (2008) Anatomical and nonanatomical double-bundle anterior cruciate ligament reconstruction: importance of femoral tunnel location on knee kinematics. Am J Sports Med 36:678–685
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamazaki, J., Muneta, T., Koga, H. et al. Radiographic description of femoral tunnel placement expressed as intercondylar clock time in double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 19, 418–423 (2011). https://doi.org/10.1007/s00167-010-1243-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-010-1243-9