Abstract
We reviewed thirty patients with degenerative posterior root tear of the medial meniscus to investigate clinical results of non-operative treatment retrospectively. There were 3 men and 27 women at a median age of 59 years old (range, 51–65). The median follow-up period was 36 months (range, 24–51). Non-operative treatments included non-steroidal anti-inflammatory drugs daily for 8–12 weeks and supervised physical therapy twice a week at least during a period of 8 weeks. The symptoms, physical signs, the Visual Analog Scale pain, the Lysholm Knee Scoring scale and IKDC subjective activity level were analyzed at the time of pre-intervention, 6 months, 12 months and the final follow-ups. Most patients had intense mechanical pain initially, but the severity and frequency of pain was decreased within 3 months. Clinical outcome was improved at 12 months follow-up and then declined to a level that was still improved over initial scores at final follow-up. Two patients with Kellgren–Lawrence grade 2 progressed to grade 3 at the median follow-up of 36 months. In conclusion, this study demonstrated that non-operative treatment provided symptomatic relief in most patients with the degenerative posterior root tear of the medial meniscus and functional improvements in a short term follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The posterior root attachment site of the medial meniscus is critical for maintaining hoop strain, preventing extrusion and preserving meniscal function. A posterior root tear of the medial meniscus causes an increase in joint contact pressure and change in knee joint kinematics [3]. There are several studies suggesting that a posterior root tear of the medial meniscus leads to the development of degenerative knee arthritis [1, 8, 10, 12, 14, 18]. Because of these deleterious effects and clinical course, the treatment of posterior root tears of the medial meniscus have been increasingly reported [2, 5, 13, 16, 17].
The degenerative posterior root tear of the medial meniscus is not uncommon in Asian patients due to life style. Some authors reported that the posterior root tear of the medial meniscus might be the source of the mechanical pain, and arthroscopic partial meniscectomy provided symptomatic improvement in most patients with mechanical symptom, although it did not relieve arthritic pain [5, 16]. However, there is still no consensus about the treatment of choice for degenerative posterior root tear of the medial meniscus, and no results of non-operative treatment have been reported. The purpose of this study was to investigate clinical results of non-operative treatment of degenerative (non-traumatic) posterior root tear of the medial meniscus. Our hypothesis was that non-operative treatment would relieve pain and improve knee function in patients with degenerative (non-traumatic) posterior root tear of the medial meniscus.
Patients and methods
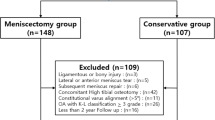
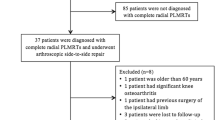
After obtaining institutional ethical committee permission, we reviewed medical records to investigate the results of non-operative treatment of degenerative posterior root tear of the medial meniscus. The inclusion criteria included: (1) Patients with isolated, non-traumatic posterior root tear of the medial meniscus on MRI as diagnosed by a musculoskeletal radiologist, (2) Patients who were treated with non-surgical methods initially and (3) Patients who had follow ups more than 24 months. During the study period, 321 patients with medial meniscus tear were treated with either conservative or arthroscopic procedures at our institution. Of those, 65 patients (20%) had non-traumatic posterior root tear of the medial meniscus. Thirty-one patients (of 65 patients) who underwent arthroscopic surgery due to other combined lesions (25 patients with posterior horn tear, 4 patients with midbody tear, 2 patients with anterior horn tear) were excluded in this study. Data were unavailable for four patients at the minimum two-year follow-up examinations. These patients did not differ from the study cohort in terms of demographic data and baseline symptomatology. Thirty patients who met the criteria were identified between 2004 and 2006 and included in this study. There were 3 men and 27 women with a median age of 59 years old (range, 51–65). The median follow-up period was 36 months (range, 24–51).
The posterior root tear of the medial meniscus was defined as radial tear at its posterior root attachment. A detailed history and standard physical examination was carried out on all patients. All patients were diagnosed with the use of MRI by musculoskeletal radiologist. There were characteristic findings of the posterior root tear of the medial meniscus on MRI [10]. On the coronal images, there was abrupt truncation of the contour of the inner margin of the posterior horn of the medial meniscus. An empty space was shown at the expected site of the posterior meniscal root adjacent to this truncated margin. On the sagittal image, there was loss of shape and signal intensity at the expected site of the meniscal root attachment, anterior to the PCL. In some cases, extrusion of the medial meniscus was shown at the medial joint margin. Anteroposterior, lateral and Merchant radiographs were used to evaluate arthritic changes. The severity of arthritic changes was classified according to Kellgren and Lawrence grade (KL grade) [11]. As graded with the Kellgren–Lawrence system, there were 5 patients with grade 0, 15 patients with grade 1 and 10 patients with grade 2. Pre-intervention MRI showed that 19 patients (63%) had concomitant degeneration of posterior horn of the medial meniscus and 17 patients (57%) had medial extrusion of the medial meniscus more than 3 mm.
Patients with: (1) Isolated, non-traumatic (degenerative) posterior root tear of the medial meniscus, (2) No combined lesion of ligament or associated meniscus tear, (3) Acute onset of knee pain during less than past 4 weeks and (4) No varus malalignment were candidates for non-operative treatment. Non-operative treatments included non-steroidal anti-inflammatory drugs (NSAIDs) daily for 8–12 weeks and supervised physical therapy twice a week at least during a period of 8 weeks. The goal of the physical therapy was to reduce pain, restore full ROM and improve knee function. It consisted of exercises for muscle strength and endurance (Table 1). Each patient visited physiotherapy office and followed a standard exercise program twice a week. The patients were informed to exert exercises with pain free. If the patients could tolerate exercises without any problems, they performed the exercises with increasing weights and resistance.
The symptoms, physical signs, the visual analog scale (VAS) pain (between 0 and 10, with 10 being the most painful), the Lysholm Knee Scoring scale and IKDC subjective activity level [6] were analyzed at the time of pre-intervention, 6, 12 months and the final follow-ups. The radiological change was evaluated by the musculoskeletal radiologist at the time of follow-up.
Statistical analysis was performed with the use of SPSS software package (version 11.0; SPSS, Chicago, IL). An ANOVA test was used to compare the clinical results. P value < 0.05 at a confidence interval of 95% was considered statistically significant.
Results
Most patients (25 patients, 83%) experienced acute onset of severe pain. But the severity and frequency of pain was decreased with time in 23 of 30 patients (77%) within 6 months from the onset of the symptoms. Pain during squatting (21 patients, 70%) and going-up stairs (18 patients, 60%) was the most common presenting symptoms. With regard to IKDC subjective activity level, 15 patients (50%) participated in light activities and 15 patients (50%) were unable to participate in such activities due to pain at initial presentation.
Clinical outcome was improved at 12 months follow-up and then declined to a level that was still improved over initial scores at final follow-up (Table 2). Sixteen patients (53%) participated in light activities and 14 patients (47%) participated in moderate activities at the last follow-up. At the median follow-up of 36 months (range, 24–51), patients with KL grade II had poorer outcomes than did patients with KL grade 0 (Table 3). Two of 10 patients with KL grade 2 progressed to grade 3 at the last follow-up. There was no significant difference of clinical results between patients with medial meniscus extrusion more than 3 mm on MRI and those with less than 3 mm.
Discussion
The most important finding of the present study was that sudden onset of pain resolved gradually within 3 months, and clinical outcome was improved after non-operative treatment. Most patients in our series were presented with sudden onset of mechanical pain around posteromedial aspect of the knee that may have been precipitated by a specific activity such as squatting or kneeling similar with previous studies [5, 16]. Ozkoc and associates [16] reported that arthroscopic partial meniscectomy was effective for patients with a posterior root tear of the medial meniscus, whose main symptoms were mechanical pain. In contrast, the present study showed that sudden onset of mechanical pain at the present mostly resolved during the follow-up period, and clinical outcome was improved at 12 months follow-up and then declined to a level that was still improved over initial scores at final follow-up after non-operative treatment.
Several studies have reported the posterior root tear of the medial meniscus result in loss of hoop stress, the decrease of load bearing capacity, the increase of the joint contact pressure and the progression of degenerative osteoarthritis [3, 4, 14, 18]. Allaire et al. [3] evaluated that biomechanical consequences of the posterior root tear of the medial meniscus. They demonstrated that significant changes in contact pressure and knee joint kinematics due to a posterior root tear of the medial meniscus. Clinically, Ozkoc et al. [16] reported the mean Kellgren–Lawrence grade worsened from grade 2 to grade 3 during the 56 months follow-up period. They concluded that arthroscopic partial meniscectomy did not halter the progression of osteoarthritis. In the present study, 2 of 10 patients with grade 2 progressed to grade 3 at the mean follow-up of 37 months, and patients with KL grade 2 had poorer outcomes than did patients with KL grade 0. One of the possible reasons for decrease in VAS pain score 12 months after onset was due to development of osteoarthritic pain. In chronic posterior root tear of the medial meniscus, development and progression of the osteoarthritis may be major problems. Therefore, in cases of degenerative posterior root tear of the medial meniscus, treatment should be focused on not only clinical symptoms in acute period but also development of degenerative osteoarthritis in chronic period.
Physical exercise is one of effective treatment options for osteoarthritis and it plays an important role to reduce knee pain, improve muscle strength, endurance, activity and quality of life in patients with osteoarthritis [9, 15]. One study reported that physical exercises three times a week during 4 months could lead to more than 35% improvement of knee function [9]. It is our belief that functional improvement was resulted from physical exercise in our patients. However, it is unclear if pain relief was resulted from NSAIDs or physical exercise or combined. Because pain scores can be affected by the fact that patients knew they were given a medical treatment, blinded, comparative study should be required to address the placebo effect.
This study showed that there were no significant differences between meniscal extrusions more than 3 mm group and less than 3 mm group with regard to VAS pain score and Lysholm knee score. However, Meniscal extrusion has two functional significances. First, extrusion of the medial meniscus is the cause of the initial joint space loss seen on radiographs during early stage of osteoarthritis [1]. Advanced osteoarthritis of the knee joint includes both meniscal extrusion and cartilage loss. Second, it is the secondary sign of the posterior root tear of the medial meniscus [10]. Ozkoc et al. [16] found that a mean 4.29 mm peripheral extrusion was measured on preoperative MRI and that nearly half of those extrusions were classified as substantial as described by Costa et al. [7]. In the present study, 17 patients (57%) had medial extrusion of the medial meniscus more than 3 mm. Because a supine MRI may not reveal the true amount of extrusion occurring in weight-bearing conditions, there are high possibilities of underestimation of the meniscal extrusion.
There are several limitations in this study. First, the outcome of non-operative treatment was not compared with operative treatment modalities such as arthroscopic meniscectomy, repair, or osteotomy. This study showed that non-operative treatment improved knee function and pain in a short term basis. But a comparative study with a long term follow-up would be required that which treatment is more beneficial to improve knee function and prevent the progression of osteoarthritis. Second, other factors were not evaluated influencing the results of non-operative treatment, such as patient’s occupation and life style. Data were not available due to retrospective study design. Third, most patients were female. Although this kind of meniscus tear is prevalent in female patients more than 50 years old, sex and age can affect individual activity. Fourth, even though high sensitivity of the MRI, some patients with a posterior root tear of the medial meniscus may be underdiagnosed or overdiagnosed. Those patients also can affect the results of this study.
The degenerative posterior root tear of the medial meniscus is not uncommon in Asian patients. Most patients experience sudden onset of mechanical symptoms such as catching, locking and buckling, which are gradually relieved within several months, and clinical outcomes can be improved after non-operative treatment such as protective weight bearing, medication, well-designed quadriceps and hamstring exercise. Arthroscopic partial meniscectomy should be considered complementary to non-operative treatment. Operative indications still need to be refined for superior results compared to non-operative treatment.
Conclusions
This study demonstrated that non-operative treatment provided symptomatic relief in most patients with the degenerative posterior root tear of the medial meniscus. The clinical outcome was improved at 12 months follow-up and then declined to a level that was still improved over initial scores at final follow-up.
References
Adams JG, McAlindon T, Dimasi M, Carey J, Eustace S (1999) Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin Radiol 54:502–506
Ahn JH, Wang JH, Yoo JC, Noh HK, Park JH (2007) A pull out suture for transection of the posterior horn of the medial meniscus: using a posterior trans-septal portal. Knee Surg Sports Traumatol Arthrosc 15:1510–1513
Allaire R, Muriuki M, Gilbertson L, Harner CD (2008) Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am 90:1922–1931
Berthiaume MJ, Raynauld JP, Martel-Pelletier J, Labonte F, Beaudoin G, Bloch DA, Choquette D, Haraoui B, Altman RD, Hochberg M, Meyer JM, Cline GA, Pelletier JP (2005) Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis 64:556–563
Bin SI, Kim JM, Shin SJ (2004) Radial tears of the posterior horn of the medial meniscus. Arthroscopy 20:373–378
Committee IKDC (2000) IKDC knee forms http://www.sportsmed.org/tabs/research/ikdc.aspx
Costa CR, Morrison WB, Carrino JA (2004) Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol 183:17–23
Gale DR, Chaisson CE, Totterman SM, Schwartz RK, Gale ME, Felson D (1999) Meniscal subluxation: association with osteoarthritis and joint space narrowing. Osteoarthritis Cartilage 7:526–532
Herrlin S, Hallander M, Wange P, Weidenhielm L, Werner S (2007) Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc 15:393–401
Jones AO, Houang MT, Low RS, Wood DG (2006) Medial meniscus posterior root attachment injury and degeneration: MRI findings. Australas Radiol 50:306–313
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Kenny C (1997) Radial displacement of the medial meniscus and Fairbank’s signs. Clin Orthop Relat Res 339:163–173
Kim YM, Rhee KJ, Lee JK, Hwang DS, Yang JY, Kim SJ (2006) Arthroscopic pullout repair of a complete radial tear of the tibial attachment site of the medial meniscus posterior horn. Arthroscopy 22:791–794
Lerer DB, Umans HR, Hu MX, Jones MH (2004) The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol 33:569–574
Mangione KK, McCully K, Gloviak A, Lefebvre I, Hofmann M, Craik R (1999) The effects of high-intensity and low-intensity cycle ergometry in older adults with knee osteoarthritis. J Gerontol A Biol Sci Med Sci 54:M184–190
Ozkoc G, Circi E, Gonc U, Irgit K, Pourbagher A, Tandogan RN (2008) Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc 16:849–854
Petersen W, Zantop T (2006) Avulsion injury to the posterior horn of the lateral meniscus: Technique for arthroscopic refixation. Unfallchirurg 109:984–987
Sugita T, Kawamata T, Ohnuma M, Yoshizumi Y, Sato K (2001) Radial displacement of the medial meniscus in varus osteoarthritis of the knee. Clin Orthop Relat Res 387:171–177
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lim, H.C., Bae, J.H., Wang, J.H. et al. Non-operative treatment of degenerative posterior root tear of the medial meniscus. Knee Surg Sports Traumatol Arthrosc 18, 535–539 (2010). https://doi.org/10.1007/s00167-009-0891-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-009-0891-0