Abstract
Overstuffing the patellofemoral compartment during TKR leads to complications such as maltracking and wear, predisposing to early failure. However, there is no data describing how the patellar construct thickness affects the retinacula. This study instrumented cadaveric knees that had a Genesis II (Smith & Nephew, Memphis, TN, USA) TKR in situ. Sutures were passed along the medial patellofemoral ligament (MPFL) and the deep transverse fibre band of the lateral retinaculum, from the ilio-tibial band (ITB) to the patella. These sutures were attached to displacement transducers. Length changes in the retinacula were measured during knee flexion-extension against the actions of 175 N quadriceps and 30 N ITB tensions. This was done with the natural patellar thickness, then repeated with the patella 2 mm thinner, 2 mm thicker and 4 mm thicker (overstuffed). Each thickness change caused a significant overall slackening or stretching of the MPFL (P < 0.0001 by ANOVA), with 2.3 mm mean stretching (P < 0.001 all angles of knee flexion by post-testing) at 4 mm thicker. The ITB-patellar band was not slackened (P = 0.491) or stretched (P = 0.346) significantly by 2 mm thickness changes. 4 mm thickening stretched the lateral retinaculum 1.1 mm (P = 0.0108). Patellar thickness affected the MPFL more than the lateral retinaculum. This difference reflected the mobile attachment of the lateral retinaculum to the ITB, whereas the MPFL was stretched directly between bony attachments. 2 mm overstuffing did not stretch the retinacula sufficiently to cause mechanical effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
“Over-stuffing” of a joint occurs during arthroplasty if an insufficient flexion, extension, or patello-femoral space is generated for the thickness of the implants inserted. When the implant has been inserted, the surrounding soft tissues will be tensed and the implant components compressed together. Overstuffing the patellofemoral compartment may lead to decreased flexion, patellofemoral maltracking, subluxation, increased patellofemoral compression and shear forces contributing to increased component wear, and possibly pain compromising the end result [1, 10, 14, 22–24, 26, 28]. An excessively thick patella may also cause practical problems for the surgeon during wound closure, because of the overstretched extensor retinaculum [17]. A thinner than normal patella increases the risk of stress fracture of the patella [15, 24].
The literature to date is in agreement regarding the importance of maintaining the pre-cut thickness of the patella after resurfacing. However, there remains little objective evidence, despite clinical [2, 9, 11, 12, 25] and biomechanical [10, 15, 17, 23, 24, 28] studies, regarding the outcome of over- or understuffing when resurfacing the patella. In some cases with smaller knees or those with severe patellar erosion, it may be impossible to preserve the natural thickness of the patella without either sacrificing the bone stock excessively or stretching the soft tissues to accommodate the construct. Retinacular tensions play an important role in patellofemoral stability, especially in early knee flexion [3, 27]. Abnormal tensions as a result of overstuffing the patellofemoral compartment may contribute to patellar maltracking, component wear and pain. However, although there has been prior work in this area, there has not been any study of how overstuffing the patellofemoral compartment stretches the retinacula.
The aims of this study were: (1) to test the hypothesis that overstuffing the patellofemoral joint during total knee replacement (TKR) would stretch both the medial and lateral retinacula, and (2) to describe the relationship between the thickness of the patella-plus-prosthesis construct and the lengths of both the medial and lateral retinacula.
Materials and methods
Retinacular behaviour was quantified by measuring length change patterns in the medial and lateral retinacula across the range 0°–110° knee flexion. The patellofemoral joint was augmented by altering the thickness of the resurfaced patella.
Specimen preparation
Eight knees were obtained from a tissue bank following approval from the Riverside Research Ethics Committee. They were sealed in polyethylene bags and frozen at −20°C prior to use. The mean age of the donors was 69 years (57–87). The specimens were all right knees and included 20 cm each of femur and tibia. The specimens were thawed in a fridge at 3°C for 24–36 h and kept moist using occasional water spraying. The skin, underlying fat and muscles other than the distal quadriceps were removed. Care was taken to preserve the retinacula, fascia of the quadriceps muscles and the iliotibial band (ITB). The quadriceps were then separated into six components: rectus femoris (RF), vastus intermedius (VI), vastus lateralis longus (VLL), vastus lateralis obliquus (VLO), vastus medialis longus (VML), and vastus medialis obliquus (VMO). The distal tendinous fibres of the muscles merged together and were left intact to ensure that the actions of the muscles were as physiological as possible. Vastus intermedius was separated from the femur. Cloth strips were sutured to the proximal end of each muscle component as well as the ITB to provide attachments for the muscle loading cables. Rectus femoris and vastus intermedius were looped together to form a central muscle group.
The femur and tibia were transected at approximately 20 and 15 cm above and below the knee joint line, respectively. The head of the fibula was fixed to the tibia by two screws, to maintain its anatomical position, and then the distal part of the fibula was removed. A brass intramedullary sleeve was cemented into the femur using poly methylmethacrylate bone cement. An intramedullary rod was cemented into the tibia to extend it distally.
Experiment set-up
The knee was mounted in the test rig (Fig. 1) by sliding the femoral intramedullary sleeve over a fixed rod and clamping it with the line joining the most-posterior points of the femoral condyles horizontal. Each muscle head was loaded in its physiological direction relative to the femoral axis [5, 6]. A load of 175 N was applied to the quadriceps muscle groups by hanging fixed weights on a cable and pulley system. The ITB was loaded to 30 N, 0° lateral and 6° posterior to the femoral axis [4, 8]. The quadriceps tension distribution was according to the mean physiological cross-sectional areas of the muscles: RF + VI 35%, VLL 33%, VLO 9%, VML 14%, and VMO 9% [6, 27]. The physiological cross sectional areas of individual specimens could not be measured, because that would have required the whole leg.
Knee mounted in kinematics rig, with motion sensors attached to the tibia at top, left, and to the patella and femur. The hand-held probe is on the femoral medial epicondyle. The displacement transducers are mounted in the triangular blocks on the base. The vastus medialis obliquus is tensed by the string passing over the pulley, central, right. Vastus medialis longus and rectus femoris are at top, right
Total knee replacement
In order to preserve the retinacula and reduce confounding factors such as variable suture tensioning affecting ligament length changes after closure of a standard medial parapatellar approach, a transpatellar approach extending 5 cm proximally into the quadriceps tendon and 3 cm distally into the patellar tendon in the line of fibres was used to access the knee joint. This approach had been validated previously [19].
A cruciate retaining TKR (Genesis II, Smith & Nephew, Memphis, TN, USA) was used. The procedure was performed by the same consultant surgeon on all eight knees. An anterior referencing jig was used so as to resect the anterior trochlea flush with the more proximal normal surface of the femur. The patella was resurfaced using a dome shaped onlay button centred along the median ridge on the undersurface of the patella. It was fixed using a screw through the thickness of the patella. Various patellar thicknesses could then be achieved by placing 2 mm thick nylon washers under the ‘onlay’ button. The thicknesses measured were 2 mm understuff, pre-cut thickness, 2 and 4 mm overstuff. This was checked using a calliper (Fig. 2).
The patella was resurfaced using an onlay button. The thickness of the patella/bone composite was adjusted by adding a series of 2 mm nylon washers between the button and the patella. The overall thickness was checked using callipers. The cut surface of the patella shows the two screw holes for reassembly of the longitudinal osteotomy
Measurements
Tibiofemoral flexion was measured dynamically using a Polaris Optical Tracking System (NDI International, Waterloo, ON, Canada) with one optical tracker on the femur and one on the tibia. Knee flexion was calculated as the angle between the femoral and tibial intramedullary rods in the sagittal plane perpendicular to the medial-lateral axis, using Visual 3D (C-Motion Inc, Rockville, MD, USA).
Length changes in the retinacula medial and lateral to the patella were measured using monofilament sutures attached to Linear Variable Displacement Transducers [8, 19] (LVDTs-Solartron Metrology, Bognor Regis, UK). Length changes (resolution to 1 μm) were recorded using device-specific software (“Orbit” Excel, Solartron Metrology, UK).
A single monofilament suture (Ethilon 2/0, Ethicon Co. Somerville, NJ, USA) was used to measure length changes in the medial patellofemoral ligament (MPFL). It was passed from the LVDT through a screw eye secured at the epicondylar attachment of the MPFL, then threaded along the fibres of the ligament and secured at the superomedial corner of the patella.
Because the deep transverse band of the lateral retinaculum joins two mobile structures (the deep aspect of the ITB and the superolateral patella [18]) it was necessary to measure the movements of the two structures separately in order to calculate the length change from the difference between them. One suture passed from an LVDT through an eyelet secured on the ITB to the patella, along the transverse band of fibres. A second LVDT measured length change using a suture attached to the ITB eyelet only.
Before testing, ten preconditioning cycles of passive knee flexion were performed with the muscle groups loaded. The knee was moved into cycles of flexion-extension, against the extending action of the quadriceps tension, by pushing posteriorly against the tibial intramedullary rod, using a nylon rod hand-held transversely across the end of the intramedullary rod to avoid imposing secondary moments. Data was collected continuously while the quadriceps extended the knee slowly from 110° to 0°. Testing was first conducted with the standard TKA where the patellar bone-plus-implant thickness was equal to the natural thickness of the patella. Measurements were then taken with the patellar construct 2 mm thinner, overstuffed to 2 mm thicker, and finally overstuffed 4 mm. The retinacular length changes were calculated relative to the length measured in the natural knee, pre-TKR, at 0° flexion.
Statistical analysis
Two-way repeated-measures analyses of variance (ANOVA) with Bonferroni post-tests were used to test for length changes between different patellar thicknesses and angles of knee flexion, for each retinacular structure. The data were analysed at 10° intervals and significance was set at P < 0.05.
Results
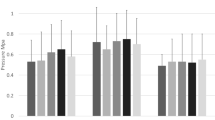
The mean pattern of length change in the MPFL after TKR was close to isometric, with a tightening of 3.1 ± 1.9 mm (mean ± SD) as the knee extended from 100° to 40° followed by a slackening of 0.5 ± 2.2 mm as the knee extended fully (Fig. 3).
The effect of the thickness of the patella plus prosthetic button construct on the length of the medial patello femoral ligament (MPFL), versus knee flexion. Shown as mean ± SD, n = 8. −2 mm: thickness 2 mm less than intact patella, etc. The zero datum was the length of the MPFL in the natural knee, pre-TKR, at full extension. Data shown at 10° increments, nudged ±2° for clarity
Understuffing the patella by 2 mm resulted in the MPFL slackening by 1.4 ± 0.2 mm as the knee extended from 100° to 0°, P < 0.0001 by ANOVA. Post-testing found that this was not significant in the flexed knee (P > 0.05 for 100°–70°), but became significant as the knee extended (P < 0.05 for 50°, 60°; P < 0.01 for 40°–0°) (Fig. 3).
Overstuffing the patella 2 mm stretched the MPFL by 1.0 ± 0.2 mm, P < 0.0001 by ANOVA (Fig. 3). Post-testing found that this was not significant in the flexed knee (P > 0.05 for 100°–30°), became significant near extension (P < 0.05 for 20°, 10°), but was not significant at 0°.
Overstuffing the patella by 4 mm resulted in a significant overall increase in length of the MPFL of 2.3 ± 0.2 mm, P < 0.0001 by ANOVA (Fig. 3). Post-testing found that this was significant at every angle of knee extension: P < 0.001 for 100° to 0°.
The deep transverse band of the lateral retinaculum slackened by a mean of 10.2 ± 6.9 mm (range from 0.7 mm tightening to 16.8 mm slackening) as the knee extended from 100° to 0° (Fig. 4).
The effect of the thickness of the patella plus prosthetic button construct on the length of the transverse ITB-patellar band, versus knee flexion. Shown as mean ± SD, n = 8. −2 mm: thickness 2 mm less than intact patella, etc. The zero datum was the length of the ITB-patellar band in the natural knee, pre-TKR, at full extension. Data shown at 10° increments, nudged ±2° for clarity
Reducing the thickness of the patella by 2 mm did not have a significant overall effect on the length of the lateral retinaculum (P = 0.4912 by ANOVA), nor did overstuffing by 2 mm (P = 0.3464). When the patella had been overstuffed by 4 mm, the lateral retinaculum was stretched by 1.1 ± 0.5 mm (P = 0.0108 by ANOVA), but there were no significant changes found at any specific angle of knee flexion on post-testing (P > 0.05) (Fig. 4).
Discussion
This study found that over- or under-stuffing the patellofemoral joint caused more stretching-slackening of the MPFL than of the deep transverse ITB-patellar band of the lateral retinaculum. The length changes that were caused in the retinacula were overlaid onto the patterns of length changes that occurred in response to the knee flexing and extending. In view of the well-known occurrence of lateral retinacular releases in some series of TKR, the lack of effect of overstuffing the patellofemoral compartment on the lateral retinaculum, accompanied by significant effects on the MPFL, was not what had been anticipated, and did not conform to the initial hypothesis.
The differing effects of overstuffing the patellofemoral compartment, on the MPFL versus the ITB-patellar band, may be explained by reference to their structural properties and attachments. The ITB-patellar band has much greater tensile stiffness than the MPFL [20, 21], which means that, as the patella is lifted away from the femur, it will stretch less in response to the same load. The dome of the patellar button is usually medialised during TKR, as in this experiment, in order to reproduce the relative sizes of the medial and lateral facets of the patella and to reduce the need for lateral releases. The corollary of this is that for the reduction of stretching and tension in the lateral retinaculum, so the tension in the MPFL will rise for the patella to remain balanced. The graphs in Figs. 3 and 4, as well as our prior work [8], show that the MPFL was relatively isometric as the knee flexed-extended, whereas the ITB-patellar band slackened by 10 mm as the knee extended. This reflects the ITB moving anteriorly alongside the knee during extension, as it passes to Gerde’s tubercle. This mobile lateral attachment means that, instead of stretching the ITB-patellar fibres, overstuffing could result simply in a slight anterior movement of the ITB.
The main limitations of this study arose from the use of normal cadaveric knees, without obvious degenerative disease. We could not simulate pathological changes in the soft tissues that may be relevant, such as tight bands in the lateral retinaculum. It has been proposed that, in degenerative disease, these structures are stiffer and tethered to the bone [7], resulting in abnormal tensioning of the lateral retinaculum if the patellofemoral joint is overstuffed. The force applied to the quadriceps was limited by tearing of the muscles, and so normal physiological magnitudes were not attained. In addition, the quadriceps and ITB tensions were constant at all angles of knee flexion, whereas in life the quadriceps tension increases as we squat down. This may have had significant effects on the length change patterns of the retinacula. Knee flexion beyond 110° would have been desirable; however aspects of the rig design prevented this. Despite these limitations this is the first study to measure the effects of patellofemoral overstuff on length change patterns in the intact retinacula. Measurements were made dynamically in order to capture transient events. The muscles were loaded in physiological directions. The ITB was also loaded; it is known to affect patellar tracking [13, 16].
Although there is no published literature on the effect of overstuffing the patellofemoral compartment on the lengths of the retinacula, there have been related studies. The tensile strain in the anterior surface of the patella increases following over-resection [15, 24, 30]. The joint contact compression and shear forces increase in response to 2 mm overstuffing [10, 23, 28] and patellofemoral kinematics are altered: Hsu et al. [10] found that a thicker patella (+2 mm) was tilted laterally and shifted medially across most of the arc of knee flexion. These kinematic changes match the smaller length changes in the ITB-patellar band in this study. Conversely, it has also been shown that reducing the thickness of the patella reduced the contact force [29], and that may arise from relaxing the retinacula, as well as altering the force vectors of the patellar tendon and quadriceps.
Clinical studies have found that the patellofemoral joint is able to withstand a degree of overstuffing. Ritter et al. [25] in a case series of 1,146 TKRs found no difference in clinical outcome between groups with patellar composites that were 2 mm more versus 2 mm less than the original thickness. They refuted the need for reproducing the original patellar thickness after resurfacing. Bengs and Scott [2] found an average of 3° loss of intraoperative knee flexion per 2 mm of additional composite thickness; however, they did not see (but did not measure) gross alteration in patellar tracking with as much as 8 mm overstuffing. However, their observations were made with the medial parapatellar retinaculum open, in contrast to this study. Greenfield et al. [9] found a significant reduction in lateral release rates for patellar maltracking in knees where the patella/bone composite was thinner than the natural patella.
The extensor retinaculum contributes significantly to patellar stability, particularly in early knee flexion [5, 27]. Abnormal retinacular tensions as a result of patellar overstuff may lead to a number of patellofemoral complications leading to early failure and pain. This experiment has shown that overstuffing the patellofemoral joint caused an increase in length of the principal medial and lateral retinacular structures. However, this was not a direct relationship: the medial structures were affected more significantly than the lateral structures, contrary to popular understanding. This was explained by the MPFL linking directly from bone to bone, whereas the ITB-patellar fibres had a mobile lateral attachment. The results suggest that overstuffing the patellofemoral compartment by 2 mm may be acceptable in terms of soft tissue tension, because the ITB-patellar band was not stretched significantly and the MPFL by only approximately 1 mm. This may be useful when it is not possible to preserve the pre-cut patellar thickness during TKR without excessive loss of bone stock.
References
Barrack RL, Burak C (2001) Patella in total knee arthroplasty. Clin Orthop Relat Res 389:62–73 (Review). doi:10.1097/00003086-200108000-00011
Bengs BC, Scott RD (2006) The effect of patellar thickness on intraoperative knee flexion and patellar tracking in total knee arthroplasty. J Arthroplasty 21:650–655. doi:10.1016/j.arth.2005.07.020
Bicos J, Fulkerson JP, Amis AA (2007) Current concepts review: the medial patellofemoral ligament. Am J Sports Med 35:484–492. doi:10.1177/0363546507299237
Bull AM, Andersen HN, Basso O, Targett A, Amis AA (1999) Incidence and mechanism of the pivot shift. An in vitro study. Clin Orthop Relat Res 363:219–231. doi:10.1097/00003086-199906000-00029
Christoforakis J, Bull AM, Strachan RK, Shymkiw R, Senavongse W, Amis AA (2006) Effects of lateral retinacular release on lateral stability of the patella. Knee Surg Sports Traumatol Arthrosc 14:273–277. doi:10.1007/s00167-005-0699-5
Farahmand F, Senavongse W, Amis AA (1998) Quantitative study of the quadriceps muscles and trochlear groove geometry related to instability of the patellofemoral joint. J Orthop Res 16:136–143. doi:10.1002/jor.1100160123
Fishkin Z, Miller M, Ritter C (2002) Changes in human knee ligament stiffness secondary to osteoarthritis. J Orthop Res 20:204–207. doi:10.1016/S0736-0266(01)00087-0
Ghosh KM, Merican AM, Iranpour-Boroujeni F, Deehan DJ, Amis AA (2009) Length change patterns of the extensor retinaculum and the effect of total knee replacement. J Orthop Res (Epub ahead of print)
Greenfield MA, Insall JN et al (1996) Instrumentation of the patellar osteotomy in total knee arthroplasty: the relationship of patellar thickness and lateral retinacular release. Am J Knee Surg 9:129–131
Hsu HC, Luo ZP, Rand JA et al (1996) Influence of patellar thickness on patellar tracking and patellofemoral contact characteristics after total knee arthroplasty. J Arthroplasty 11:69–80. doi:10.1016/S0883-5403(96)80163-X
Ikezawa Y, Gustilo RB (1999) Clinical outcome of revision of the patellar component in total knee arthroplasty: a 2 to 7 year follow-up study. J Orthop Sci 4:83–88. doi:10.1007/s007760050079
Koh JSB, Yeo SJ et al (2002) Influence of patellar thickness on results of total knee arthroplasty. J Arthroplasty 17:56–61. doi:10.1054/arth.2002.29320
Kwak SD, Ahmad CS, Gardner TR et al (2000) Hamstrings and iliotibial band forces affect knee kinematics and contact pattern. J Orthop Res 10:101–108. doi:10.1002/jor.1100180115
Laskin R, Beksac B (2004) Stiffness after total knee arthroplasty. J Arthroplasty 19(Suppl 1):41–46. doi:10.1016/j.arth.2004.02.008
Lie DTT, Gloria N, Amis AA et al (2005) Patellar resection during total knee arthroplasty: effect on bone strain and fracture risk. Knee Surg Sports Traumatol Arthrosc 13:203–208. doi:10.1007/s00167-004-0508-6
Luo ZP, Sakai N, Rand JA, An KA (1997) Tensile stress of the lateral patellofemoral ligament during knee motion. Am J Knee Surg 10:139–144
Marmor L (1988) Technique for patellar resurfacing in total knee arthroplasty. Clin Orthop Relat Res 230:166–171
Merican AM, Amis AA (2008) Anatomy of the lateral retinaculum of the knee. J Bone Joint Surg Br 90-B:527–534. doi:10.1302/0301-620X.90B4.20085
Merican AM, Ghosh KM, Deehan D, Amis AA (2009) The trans-patellar approach (patellar split): a less-invasive approach for the knee in the laboratory. J Orthop Res 27:330–334. doi:10.1002/jor.20755
Merican AM, Sanghavi S, Iranpour-Boroujeni F, Amis AA (2009) The structural properties of the lateral retinaculum of the knee. J Biomech (submitted)
Mountney J, Senavongse W, Amis AA, Thomas NP (2005) Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br 87-B:36–40
Mihalko W, Fishkin Z (2006) Patellofemoral overstuff and its relationship to flexion after total knee arthroplasty. Clin Orthop Relat Res 449:283–287. doi:10.1097/01.blo.0000218756.89439.06
Oishi CS, Kaufman KR et al (1996) Effects of patellar thickness on compression and shear forces in total knee arthroplasty. Clin Orthop Relat Res 331:283–290. doi:10.1097/00003086-199610000-00040
Reuben JD, McDonald CL, Woodard PL et al (1991) Effect of patella thickness on patella strain following total knee arthroplasty. J Arthroplasty 6:251–258. doi:10.1016/S0883-5403(06)80172-5
Ritter MA, Pierce MJ et al (1999) Patellar complications (total knee arthroplasty): effect of lateral release and thickness. Clin Orthop Relat Res 367:149–157. doi:10.1097/00003086-199910000-00018
Scuderi GR, Insall JN, Scott NW (1994) Patellofemoral pain after total knee arthroplasty. J Am Acad Orthop Surg 2:239–246
Senavongse W, Amis AA (2005) The effects of articular, retinacular, or muscular deficiencies on patellofemoral joint stability. J Bone Joint Surg Br 87:577–582. doi:10.1302/0301-620X.87B4.14768
Star MJ, Kaufman KR, Irby SE et al (1996) The effects of patellar thickness on patellofemoral forces after resurfacing. Clin Orthop Relat Res 322:279–284. doi:10.1097/00003086-199601000-00033
Vaquero J, Arriaza R (1993) The patella thinning osteotomy. An experimental study of a new technique for reducing patellofemoral pressure. Int Orthop 16:372–376
Wulff W, Incavo SJ (2000) Arthroplasty on patellar strain—a comparison of resurfacing versus inset implants. J Arthroplasty 15:778–782. doi:10.1054/arth.2000.6636
Acknowledgments
During this study, KM Ghosh was supported by a grant from Smith & Nephew (UK) Ltd; AM Merican was supported by the University of Malaya Medical Centre and the Arthritis Research Campaign (ARC), and F Iranpour by a grant from the Furlong Charitable Foundation for Research. The tissue specimens were supplied by the International Institute for the Advancement of Medicine, Jessup, PA, USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ghosh, K.M., Merican, A.M., Iranpour, F. et al. The effect of overstuffing the patellofemoral joint on the extensor retinaculum of the knee. Knee Surg Sports Traumatol Arthrosc 17, 1211–1216 (2009). https://doi.org/10.1007/s00167-009-0830-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-009-0830-0