Abstract
Purpose
To biomechanically evaluate MPTL reconstruction and compare it with two techniques for MPFL reconstruction in regard to changes in patellofemoral contact pressures and restoration of patellar stability.
Methods
This is an experimental laboratory study in eight human cadaveric knees. None had patellofemoral cartilage lesions or trochlear dysplasia as evaluated by conventional radiographs and MRI examinations. The specimens were secured in a testing apparatus, and the quadriceps was tensioned in line with the femoral shaft. Contact pressures were measured using the TekScan sensor at 30°, 60° and 90°. The sensor was placed in the patellofemoral joint through a proximal approach between femoral shaft and quadriceps tendon to not violate the medial and lateral patellofemoral complex. TekScan data were analysed to determine mean contact pressures on the medial and lateral patellar facets. Patellar lateral displacement was evaluated with the knee positioned at 30° of flexion and 9 N of quadriceps load, then a lateral force of 22 N was applied. The same protocol was used for each condition: native, medial patellofemoral complex lesion, medial patellofemoral ligament reconstruction (MPFL-R) using gracilis tendon, MPFL-R using quadriceps tendon transfer, and medial patellotibial ligament reconstruction (MPTL-R) using patellar tendon transfer.
Results
No statistical differences were found for mean and peak contact pressures, medial or lateral, among all three techniques. However, while both techniques of MPFL-R were able to restore the medial restraint, MPTL-R failed to restore resistance to lateral patellar translation to the native state (mean lateralization of the patella [mm]: native: 9.4; lesion: 22; gracilis MPFL-R: 8.1; quadriceps MPFL-R: 11.3; MPTL-R: 23.4 (p < 0.001).
Conclusion
MPTL-R and both techniques for MPFL-R did not increase patellofemoral contact pressures; however, MPTL-R failed to provide a sufficient restraint against lateral patellar translation lateral translation in 30° of flexion. It, therefore, cannot be recommended as an isolated procedure for the treatment of patellar instability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The medial patellofemoral ligament (MPFL) has been identified as the most important soft tissue stabilizer against patellar dislocation [7, 8, 22, 24]. Currently, MPFL reconstruction (MPFL-R) is the most used procedure for the treatment of recurrent patellar instability, and has demonstrated satisfactory outcomes with a low rate of complications [18].
The medial patellotibial ligament (MPTL) is a secondary restraint of patellar lateralization. Biomechanically, the MPTL acts mainly in flexion, being responsible for patellar rotation and tilt when the knee is flexed beyond 45° [24]. Recently some authors have described MPTL reconstruction as an isolated procedure [37] or in combination with MPFL-R [1, 13, 15, 36] for patellar instability. Additional anatomic studies of the MPTL-R have provided further detail and informed the use of this technique for the treatment of patellar instability [16, 17]. However, no study has investigated the kinematics of MPTL-R.
In this context, this study was designed to evaluate and compare three techniques for the reconstruction of static medial patellar restraints: MPFL reconstruction using gracilis tendon (MPFL-R-G) or transfer of a quadriceps muscle tendon strip (MPFL-R-QT), and MPTL reconstruction (MPTL-R).
This study aims to evaluate the influence of these surgical techniques on patellofemoral contact pressures and patellar stability to compare MPTL-R with established MPFL reconstruction techniques using the gracilis or quadriceps tendons as grafts. The hypothesis is that anatomic MPFL-R-G and MPTL-R can restore patellar instability with less influence of patellofemoral pressure than non-anatomic MPFL-R-QT. Clinically, an increase in patellofemoral pressure leads to articular degeneration and better understanding about those techniques would prevent this undesirable outcome.
Materials and methods
Eight fresh-frozen knees, with no history of surgery or disease, obtained from a certified tissue bank were used. All knees underwent MRI and conventional radiographs (AP and Lateral). They presented no meniscal or ligament lesion, patellofemoral chondral lesion, gonarthrosis (Kellgren–Lawrence: II, III, IV), trochlea dysplasia on lateral radiographs, TT–TG > 20 mm and patella alta (Caton ratio > 1.2).
Specimen preparation
The knees were stored in the freezer at – 20 °C. Twenty-four hours before the start of testing, the knees were removed from the freezer and left at room temperature for thawing.
The knees were prepared by removing skin, subcutaneous fat and muscles, leaving intact all ligaments, the knee joint capsule, as well as the quadriceps muscle. Osteotomies were performed on the femoral and tibial diaphysis at 120 mm distance from the joint line. After the osteotomy, the femoral diaphysis was fixed with bone cement and moulded, to allow fixation in the test apparatus.
The gracilis tendon was dissected and harvested for use as a graft for MPFL reconstruction. The tendon was fitted with a#2 Orthocord® sutures (Manufacturer Ethicon, USA) using Krakow-type locking stitches at each end. The proximal end of the quadriceps muscle was wrapped with surgical gauze and sutured with two, starting approximately 100 mm proximal to the patellar insert. The sutures was tied together to be connected to a cable force by a D-ring during the tests.
For testing the resistance to patellar lateralization, using an ACL reconstruction guide a transverse tunnel was drilled from medial to lateral through the central portion of the patella with a 2-mm Kirschner wire. A #2 Orthocord® suture (Manufacturer Ethicon, USA) was passed through the tunnel, and the two strands tied together to be connected using a D-ring to a cable applying a lateralization force to the patella.
After preparation of the knee, it was attached to the test apparatus. All procedures were performed on the same day, from preparation to testing. During the tests, the knee was periodically moistened with 0.9% saline using a spray bottle.
Surgical procedure
The transection of the static stabilizers was performed at 30° of flexion. The patella was pulled laterally with a force of 22 N while a traction of 9 N was applied to the quadriceps [6, 11]. With a scalpel blade N11, the medial restraints of the patella were released, from proximal to distal, on the medial border of the patella. All medial retinacular complex (MPFL, MPTL, MPML and capsule) was incised. By palpation, it was possible to evaluate if any tight tissue were holding the patella and then release until only a soft articular-sided synovial tissue was intact.
For the MPFL-R with gracilis tendon (MPFL-R-G), the graft was first attached to the patella. A 5.0-mm FASTIN RC titanium anchor with Orthocord® suture was utilized (Manufacturer Depuy Mitek, USA). By visualization, using a ruler, the anchor was positioned at the junction of the proximal third and the two distal thirds of the patella [19], and the central portion of the graft was secured to the anchor with #2 Orthocord® (Manufacturer Ethicon, USA).
After fixation of the graft on the patella, the position of the femoral fixation was identified by palpation and direct visualization, slightly proximal and posterior to the medial epicondyle and distal to the adductor tubercle [23]. A guidewire was placed from medial to lateral in the chosen position. Then the graft length changes were tested, accepting up to 5 mm of graft lengthening with flexion [29]. If the length changes exceeded this value, a new point was chosen. Once an acceptable position had been identified, a 7-mm tunnel was made with a cannulated reamer.
Using blunt dissection, a tunnel was created between layers II and III of the medial soft tissues and the graft sutures were passed from medial to lateral through the femoral tunnel. Once the graft was pulled into the tunnel, the sutures attached to the ends of the graft were passed through a pulley positioned lateral to the femoral shaft and exposed to a 2 N force for 5 min to allow for potential slippage and adjustment of the graft within the femoral tunnel [2]. Then the knee was positioned at 30 °s of flexion, and the suture was clamped at the tunnel exit on the lateral side for static fixation [14].
For MPFL-R with quadriceps tendon (MPFL-R-QT), a strip of the central third of the superficial layer of the quadriceps tendon was dissected and detached proximally, maintaining its patellar insertion. The length of the graft was pre-determined by measuring the distance from the centre of the patella to the medial epicondyle plus 1.5 cm, and the width was set at 7 mm [10, 20]. The graft was angled medially 90° and turned over its axis 180°. To avoid detachment at the patella, the lateral insertion of the tendon was anchored with a #1 Vicryl 1 (Ethicon, USA) suture. The free end of the graft was prepared with a #2 Orthocord® suture (Manufacturer Ethicon, USA) using Krakow-type locking stitches. The position and fixation of the tendon on the femoral side followed the same protocol described above for MPFL-R-G.
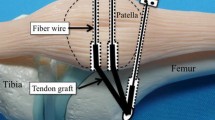
For MPTL-R, the medial third of patellar tendon was dissected maintaining its patellar attachment. Distally the tendon was dissected subperiosteal, and a Krakow-type suture was utilized at the distal free end of the graft. A 5.0-mm FASTIN RC titanium anchor with Orthocord™ suture (Depuy Mitek, USA) was positioned 2 cm distal from the articular line and 2 cm medial from the original medial border of the patellar tendon [15]. The graft was secured with the knee at 90° of flexion and the quadriceps tendon tensioned by a 9 N force. The graft was pulled by a 2 N force distally, in line with the direction of the graft position. Then the graft was attached to the tibial anchor a #2 Orthocord™ suture (Ethicon, USA).
Contact pressure measurement
Patellofemoral contact pressure was measured using the I-Scan pressure mapping system (Tekscan Inc, Boston, MA). This tool allows accurate pressure analysis at the patellofemoral joint using a thin and flexible sensor [3, 35].The sensor used was the 5051 I-Scan model (Tekscan Inc., Boston, MA) (range, 0–172 kg/cm2, resolution, 0.7 kg/cm2), with total matrix surface of 56 × 56 mm and 1 mm thickness. A new sensor was used for each knee. This system had a test–re-test mean difference of 6.8 ± 2.8% (mean pressure), similar to a previous study [32].
Prior to knee positioning, the sensor was prepared by reinforcing the end with adhesive tape. Reinforcement was performed to allow the passage of two #2 Ethibond Excel™ sutures (Ethicon, USA), without damaging the sensor. The sensor was inserted through an incision in the proximal capsule between the quadriceps and anterior femur. Then the sutures attached to the end of the sensor were retrieved from the joint by two small distal incisions, medial and lateral to the patellar ligament. The sensor was pulled into the joint and positioned between the patella and the trochlea.
Patellofemoral contact pressure was measured in three areas: medial facet, lateral facet and total patella. To determine the border between the medial and lateral facets, during preparation of the knee, a 2-mm tunnel was drilled from the anterior cortex to the articular surface at the apex of the median ridge in the distal portion of the patella. During testing, a 1-mm rod was inserted into the tunnel and gently touched the sensor; this appears in the live screen Tekscan image to determine medial and lateral facet for data acquisition [32].
The patellofemoral contact pressures were evaluated in 30°, 60° and 90° of flexion. For the test, the quadriceps tendon was tensioned with a 178 N force [3, 9].
Patellar lateralization measurement
To measure patellar lateralization, the knee was positioned at 30° of flexion and a 9 N tensile force was applied to the quadriceps tendon to simulate the resting tension [11]. A laterally oriented displacement force was applied to the patella by a cable connected to the transosseous suture placed in the centre of the patella. The cable was passed through the pulley and connected to a load of 22 N [2].
Lateral translation of the patella was measured using a three-dimensional digitizer—Microscribe G2 (Immersion Corp, San Jose CA, USA, precision 0.022 mm).
Lateralization distance was measured as the translation of the patella parallel to the posterior femoral condylar axis. A point marked on the medial border of the patella was acquired in two situations: with and without lateralization force. The difference of the two positions in the plane of the posterior condyles was defined as the lateralization distance.
Test protocol
The knee was secured to a rigid test apparatus. The femoral shaft was oriented parallel to the ground. The rotation of the femur was adjusted with the knee positioned at 90° of flexion so that the tibia was perpendicular to the ground.
For the control of knee flexion, the distal tibia was captured between two parallel bars (anterior and posterior to the tibia) that could be locked at the desired flexion angles to restrict flexion/extension, but allowed secondary movements in rotation, varus and valgus [2, 5, 33].
To evaluate the influence of surgical technique for medial soft tissue reconstruction in terms of patellofemoral contact pressure and lateral translation of the patella, each knee was evaluated in five situations:
-
Native This condition preserved all the original characteristics of the knee, with the limited dissection required to introduce the sensor and prepare the specimen.
-
Lesion Transection of the medial patellar soft tissue stabilizers.
-
MPFL-R-G MPFL reconstruction with gracilis tendon graft.
-
MPFL-R-QT MPFL reconstruction with central quadriceps tendon strip.
-
MPTL-R MPTL reconstruction with a medial patellar tendon strip.
Each knee was initially evaluated in its native form, followed by the lesion state. The other three conditions were tested in a randomized sequence determined by block randomization. For each testing condition, lateralization of the patella was evaluated first followed by patellofemoral contact pressures with knee flexion angles determined by block randomization.
Statistical analysis
The power analysis of the sample size for this study was calculated considering 0.2 MPa as a significant difference in the contact pressure, with a variance of ± 0.3 MPa, according to a previous study, which used the same evaluation system [31]. Based on these parameters, a sample of eight knees would be necessary to detect a significant difference with 80% of power and 95% of confidence. For statistical analysis, the five conditions evaluated in this study and the degree of knee flexion were considered as dependent categorical variables. The patellofemoral contact pressure and lateral patellar translation were considered continuous independent variables. The independent variables were presented as mean and standard deviation in the five conditions evaluated for each degree of flexion. The Shapiro–Wilk test was used to evaluate the normality of the sample. When the sample failed to demonstrate a normal distribution, in both independent variables, the Kruskal–Wallis test was used to determine the existence of significant differences between the test conditions in each degree of flexion. Post hoc analysis using Wilcoxon with Bonferroni correction was applied when the significant differences between the test conditions were noted. The statistical significance was defined a priori for p < 0.05.
Results
Eight knees (mean age 46 years, 5 male and 3 female) were included for the final analysis of this study.
The three surgical techniques for the reconstruction of the medial static stabilizers of the patella showed patellofemoral contact pressures similar to those recorded in the native knee, regardless of the degree of knee flexion (p < 0.05). No statistical differences were found between native knee and lesion condition. The graphs represented in Figs. 1, 2 and 3 demonstrate the patellofemoral contact pressure in the five tested conditions, in the three degrees of flexion evaluated.
Regarding lateralization of the patella, the MPFL-R-G and MPFL-R-QT techniques demonstrated values similar to the native knee without statistically significant differences. MPTL-R, however, showed increased patellar lateralization, similar to the lesion condition. Both conditions, MPTL-R and lesion, showed lateralization of the patella that was significantly higher than the native situation (p = 0.0002; p = 0.0001) (Fig. 4).
Discussion
This study demonstrated that while none of the techniques abnormally elevated patellofemoral pressures at any flexion angle, MPTL-R was unable to restore resistance to lateral patellar displacement at 30° of flexion. MPFL-R-QT and MPFL-R-G restored resistance to values similar to the native condition.
Recently, the MPTL has gained greater attention in the literature and some authors have suggested MPTL reconstruction, either in isolation or concomitant with MPFL-R, to restore patellofemoral stability in patients with recurrent patellar dislocation [15]. However, in comparison to the extensive literature on the MPFL, MPTL reconstruction is still poorly studied, and there is scarce evidence in the literature on the anatomy and biomechanics of MPTL reconstruction for the treatment of patellofemoral instability [16, 17, 25].
The MPTL functions as a restraint of the proximal and lateral force vector of the quadriceps muscle towards the end of active knee extension [4]. Thus, although the indications of MPTL-R are not completely defined, its use could be potentially advantageous in skeletally immature patients, either in isolation to avoid the femoral growth plate, or in association with MPFL-R for patients with significant anatomical risk factors such as a lateralized tibial tubercle, trochlea dysplasia and patella alta as these abnormalities are generally treated with tibial tubercle osteotomy, which is contraindicated with open physes due to the high risk of growth arrest. MPTL-R is also being utilized in combination with other procedures for rare cases of dislocation in deep flexion as seen with hypoplastic lateral femoral condyles. While our study did not provide data to support the use of MPTL-R in this scenario, at least contact pressures were not increased.
This study evaluated two techniques of MPFL-R. Use of the gracilis tendon was selected because it is a well-established technique that is able to restore patellar kinematics, as previously evaluated in other similar biomechanical studies [19, 27, 33]. Thus, MPFL-R-G was used as an internal reference to validate the test protocol and reconstruction technique. MPFL-R with quadriceps tendon has also been widely used, with favourable clinical results [10, 12, 21, 30]. MPFL-R-QT does not require additional fixation on the patella, and thus has the advantages of lower cost and avoidance of complications arising from patellar fixation. The main difference between MPFL-R-G and MPFL-R-QT lies in the patellar position of the graft. The findings of no significant differences in pressures and resistance to lateralization are in agreement with previous biomechanical studies, demonstrating that the variation in graft placement in the patella has less influence on the isometry of the ligament [34].
This study had limitations. It shares the intrinsic limitations of all cadaveric studies, chiefly, the use of knees without significant anatomical risk factors such as patella alta, lateralized tibial tubercle or trochlear dysplasia, potentially limit the extrapolation of our data for patients with these abnormalities. Traction was applied to the quadriceps muscle tendon by a single 178 N force mimicking the traction of the rectus femoris (RF) and vastus intermedius (VI). Biomechanical studies [26, 28] demonstrated that single traction (RF + VI) or multiple traction (for each quadriceps muscle bundle: RF + VI + vastus lateralis + vastus medialis) did not significantly alter patellofemoral kinematics at 30°–90° of flexion, as tested in the present study.
Conclusion
None of the three reconstruction techniques led to abnormal increases in patellofemoral contact pressures; however, MPTL reconstruction failed to provide a sufficient restraint against lateral patellar translation lateral translation in 30° of flexion. Therefore, its use as an isolated procedure for the treatment of conventional patellar instability appears questionable.
References
Baumann CA, Pratte EL, Sherman SL, Arendt EA, Hinckel BB (2018) Reconstruction of the medial patellotibial ligament results in favorable clinical outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc 26:2920–2933
Beck P, Brown NAT, Greis PE, Burks RT (2007) Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med 35:1557–1563
Beck PR (2005) Trochlear contact pressures after anteromedialization of the tibial tubercle. Am J Sports Med 33:1710–1715
Ebied AM, El-Kholy W (2011) Reconstruction of the medial patello-femoral and patello-tibial ligaments for treatment of patellar instability. Knee Surg Sports Traumatol Arthrosc 20:926–932
Farahmand F, Tahmasbi MN, Amis AA (1998) Lateral force-displacement behaviour of the human patella and its variation with knee flexion-a biomechanical study in vitro. J Biomech 31:1147–1152
Fithian DC, Mishra DK, Balen PF, Stone ML, Daniel DM (1995) Instrumented measurement of patellar mobility. Am J Sports Med 23:607–615
Franciozi CE, Ambra LF, Albertoni LJB, Debieux P, de Mello Granata GS, Kubota MS, Carneiro M, Abdalla RJ, Luzo MVM, Cohen M (2019) Anteromedial Tibial tubercle osteotomy improves results of medial patellofemoral ligament reconstruction for recurrent patellar instability in patients with tibial tuberosity-trochlear groove distance of 17 to 20 mm. Arthroscopy 35:566–574
Franciozi CE, Ambra LF, Albertoni LJB, Debieux P, Rezende FC, de Oliveira MA, de Ferreira MC, Luzo MVM (2016) Increased femoral anteversion influence over surgically treated recurrent patellar instability patients. Arthroscopy 33:633–640
Garretson RB (2004) Contact pressure at osteochondral donor sites in the patellofemoral joint. Am J Sports Med 32:967–974
Goyal D (2013) Medial patellofemoral ligament reconstruction. Am J Sports Med 41:1022–1029
Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM (1998) Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res 349:174–182
Hernandez AJ, Favaro E, Almeida A, Bonavides A, Demange MK, Camanho GL (2009) Reconstruction of the medial patellofemoral ligament in skeletally immature patients. Tech Knee Surg 8:42–46
Hetsroni I, Mann G, Dolev E, Nyska M (2019) Combined reconstruction of the medial patellofemoral and medial patellotibial ligaments: outcomes and prognostic factors. Knee Surg Sports Traumatol Arthrosc 27:507–515
Higuchi T, Arai Y, Takamiya H, Miyamoto T, Tokunaga D, Kubo T (2010) An analysis of the medial patellofemoral ligament length change pattern using open-MRI. Knee Surg Sports Traumatol Arthrosc 18:1470–1475
Hinckel BB, Gobbi RG, Demange MK, Bonadio MB, Pécora JR, Camanho GL (2016) Combined reconstruction of the medial patellofemoral ligament with quadricipital tendon and the medial patellotibial ligament with patellar tendon. Arthrosc Tech 5:e79–84
Hinckel BB, Gobbi RG, Demange MK, Pereira CAM, Pécora JR, Natalino RJM, Miyahira L, Kubota BS, Camanho GL (2017) Medial patellofemoral ligament, medial patellotibial ligament, and medial patellomeniscal ligament: anatomic, histologic, radiographic, and biomechanical study. Arthroscopy 33:1862–1873
Kaleka CC, Aihara LJ, Rodrigues A, Medeiros SF, Oliveira VM, Cury RPL (2016) Cadaveric study of the secondary medial patellar restraints: patellotibial and patellomeniscal ligaments. Knee Surg Sports Traumatol Arthrosc 25:144–151
Kyung H-S, Kim H-J (2015) Medial patellofemoral ligament reconstruction: a comprehensive review. Knee Surg Relat Res 27:133–138
Lorbach O, Haupert A, Efe T, Pizanis A, Weyers I, Kohn D, Kieb M (2016) Biomechanical evaluation of MPFL reconstructions: differences in dynamic contact pressure between gracilis and fascia lata graft. Knee Surg Sports Traumatol Arthrosc 22:1–9
Mariscalco MW, Magnussen RA, Mitchell J, Pedroza AD, Jones MH, Andrish JT, Parker RD, Kaeding CC, Flanigan DC (2014) How much hamstring graft needs to be in the femoral tunnel? A MOON cohort study. Eur Orthop Traumatol 6:9–13
Nelitz M, Williams SRM (2014) Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents using a pedicled quadriceps tendon graft. Arthrosc Tech. https://doi.org/10.1016/j.eats.2014.01.005
Nomura E, Horiuchi Y, Inoue M (2002) Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee 9:139–143
Nomura E, Inoue M, Osada N (2005) Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc 13:510–515
Philippot R, Boyer B, Testa R, Farizon F, Moyen B (2012) The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc 20:331–336
Placella G, Tei M, Sebastiani E, Speziali A, Antinolfi P, Delcogliano M, Georgoulis A, Cerulli G (2015) Anatomy of the medial patello-femoral ligament: a systematic review of the last 20 years literature. Musculoskelet Surg 99:93–103
Powers CM, Lilley JC, Lee TQ (1998) The effects of axial and multi-plane loading of the extensor mechanism on the patellofemoral joint. Clin Biomech 13:616–624
Rood A, Hannink G, Lenting A, Groenen K, Koëter S, Verdonschot N, van Kampen A (2015) Patellofemoral pressure changes after static and dynamic medial patellofemoral ligament reconstructions. Am J Sports Med 43:2538–2544
Shalhoub S, Maletsky LP (2014) Variation in patellofemoral kinematics due to changes in quadriceps loading configuration during in vitro testing. J Biomech 47:130–136
Steensen RN, Dopirak RM, McDonald WG (2004) The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med 32:1509–1513
Steiner TM, Torga-Spak R, Teitge RA (2006) Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med 34:1254–1261
Stephen JM, Dodds AL, Lumpaopong P, Kader D, Williams A, Amis AA (2015) The ability of medial patellofemoral ligament reconstruction to correct patellar kinematics and contact mechanics in the presence of a lateralized tibial tubercle. Am J Sports Med 43:2198–2207
Stephen JM, Kader D, Lumpaopong P, Deehan DJ, Amis AA (2013) Sectioning the medial patellofemoral ligament alters patellofemoral joint kinematics and contact mechanics. J Orthop Res 31:1423–1429
Stephen JM, Kittl C, Williams A, Zaffagnini S, Marcheggiani Muccioli GM, Fink C, Amis AA (2016) Effect of medial patellofemoral ligament reconstruction method on patellofemoral contact pressures and kinematics. Am J Sports Med 44:1186–1194
Stephen JM, Lumpaopong P, Deehan DJ, Kader D, Amis AA (2012) The medial patellofemoral ligament. Am J Sports Med 40:1871–1879
Van Haver A, De Roo K, De Beule M, Labey L, De Baets P, Dejour D, Claessens T, Verdonk P (2015) The effect of trochlear dysplasia on patellofemoral biomechanics: a cadaveric study with simulated trochlear deformities. Am J Sports Med 43:1354–1361
Yang Y, Zhang Q (2019) Reconstruction of the medial patellofemoral ligament and reinforcement of the medial patellotibial ligament is an effective treatment for patellofemoral instability with patella alta. Knee Surg Sports Traumatol Arthrosc 27:2599–2607
Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, Luetzow WF, Vaccari V, Benzi A, Marcacci M (2013) Medial patellotibial ligament (MPTL) reconstruction for patellar instability. Knee Surg Sports Traumatol Arthrosc 22:2491–2498
Acknowledgements
Luiz Felipe Ambra was supported by Coordination for the Improvement of Higher Education Personnel (CAPES) of Brazil.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
IRB approval by Partners Human Research Committee Protocol # 2016P000021/BWH.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ambra, L.F., Franciozi, C.E., Phan, A. et al. Isolated MPTL reconstruction fails to restore lateral patellar stability when compared to MPFL reconstruction. Knee Surg Sports Traumatol Arthrosc 29, 793–799 (2021). https://doi.org/10.1007/s00167-020-06015-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06015-3