Abstract
The effect of using gamma irradiation to sterilize bone-patellar tendon-bone (BPTB) allograft on the clinical outcomes of anterior cruciate ligament (ACL) reconstruction with irradiated allograft remains controversial. Our study was aimed to analyze the clinical outcomes of arthroscopic ACL reconstruction with irradiated BPTB allograft compared with non-irradiated allograft and autograft. All BPTB allografts were obtained from a single tissue bank and the irradiated allografts were sterilized with 2.5 Mrad of irradiation prior to distribution. A total of 102 patients undergoing arthroscopic ACL reconstruction were prospectively randomized consecutively into three groups. The same surgical technique was used in all operations done by the same senior surgeon. Before surgery and at the average of 31 months follow-up (range 24–47 months) patients were evaluated by the same observer according to objective and subjective clinical evaluations. Of these patients, 99 (autograft 33, non-irradiated allograft 34, irradiated allograft 32) were available for full evaluation. When compared the irradiated allograft group to non-irradiated allograft group or autograft group at 31 months follow-up by the Lachman test, ADT, pivot shift test and KT-2000 arthrometer testing, statistically significant differences were found. Most importantly, 87.8% of patients in the Auto group, 85.3% in the Non-Ir-Auto group and just only 31.3% in the Ir-Allo group had a side-to-side difference of less than 3 mm according to KT-2000. The failure rate of the ACL reconstruction with irradiated allograft (34.4%) was higher than that with autograft (6.1%) and non-irradiated allograft (8.8%). The anterior and rotational stability decreased significantly in the irradiated allograft group. According to the overall IKDC, functional, subjective evaluations and activity level testing, no statistically significant differences were found between the three groups. However, there was a trend that the functional and activity level decreased and the patients felt uncomfortable more often in the irradiated allograft group. The statistical analysis showed no significant difference between the non-irradiated allograft group and the autograft group according to the aforementioned evaluations, except that patients in the allograft group had a shorter operation time and a longer duration of postoperative fever. When comparing the postoperative duration of fever of the two allograft groups, there was also a trend that the irradiated allograft group was longer than the non-irradiated allograft group, but no significant difference was found. When the patients had a fever, the laboratory examinations of all patients were almost normal (Blood routine was normal, the values of ESR were 5 ~ 16 mm/h, CRP were 3 ~ 10 mg/l). On the basis of our study, we concluded that patients undergoing ACL reconstruction with BPTB non-irradiated allograft or autograft had similar clinical outcomes. Non-irradiated BPTB allograft is a reasonable alternative to autograft for ACL reconstruction. While the short term clinical outcomes of the ACL reconstruction with irradiated BPTB allograft were adversely affected with an increased failure rate. The less than satisfactory results led the senior authors to discontinue the use of irradiated BPTB allograft in ACL surgery and not to advocate that gamma irradiation be used as a secondary sterilizing method. Further research into alternatives to gamma irradiation is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) reconstruction with a bone-patellar tendon-bone (BPTB) autograft has become a gold standard and well-documented procedure over the last several decades. Lots of studies reported that the ACL reconstruction with BPTB autograft produced good clinical results [10, 13, 14, 17, 18]. However, a desire to avoid the sacrifice of autologous tissue and to minimize surgical trauma and postoperative donor site morbidity has promoted the consideration of alternative graft sources [2, 34, 35]. One such alternative is allogenic tissue.
The use of allograft for ACL reconstruction has risen tremendously over the past decade. There are many potential advantages to the use of allograft, including elimination of donor site morbidity, no weakening of the extensor or flexor apparatus, shorter operating time, smaller incisions, less pain, better cosmetic result, easier rehabilitation, lower incidence of postoperative arthrofibrosis, availability of larger grafts and thereby more appropriate for revision surgery, for multiple ligamentous injury or in the presence of patellar baja. Several studies [19, 20, 22, 34] have shown that allograft is a reasonable alternative to BPTB autograft for ACL reconstruction.
There are, however, risks associated with the use of allograft, most notably being the disease transmission, both bacterial and viral, such as HIV, hepatitis B and so on. To minimize the risk of disease transmission by allograft tissue, American Association of Tissue Banks (AATB) and the Food and Drug Administration (FDA) set forth guidelines of allograft tissue processing. In accordance with this, tissue banks adopted various methods of tissue processing, including donor screening, aseptic harvesting technique, and further sterilization techniques, to ensure graft sterility.
Gamma irradiation, which has known bactericidal and virucidal properties, is currently the most popular option for sterilization of allograft. While many published studies [1, 8, 12, 16, 30] have shown that gamma irradiation significantly alters the initial biomechanical properties of allograft in a dose-dependent manner. Dose as low as 2.5 Mrad commonly used by tissue banks has been shown to reduce the initial stiffness and strength of tendon allograft. But up to now, there are only a few clinical investigations [15, 28, 29] studying the clinical outcomes of irradiated allograft for ligament reconstruction. Whether or not the alteration in biomechanical property affects the clinical outcomes of ACL reconstruction with irradiated allograft remains controversial.
Besides the disease transmission, allograft has its own other problems, such as the possibility of a host immune response against the donor tissue, delayed incorporation, bone tunnel enlargement, increased postoperative traumatic rupture rate, and graft cost. Because of this, some studies [6, 21, 23, 25, 26] reported that the results of using allograft for ACL reconstruction were not satisfactory and did not advocate the use of allogenic tissue.
Surgeons are therefore faced with a dilemma when making a choice to do the reconstruction. Which type of graft should be used: allograft or autograft? If the allograft can be used as alternative to the autograft, which type of allograft should be used: irradiated or non-irradiated? Do they have the similar clinical outcomes or which is the better?
In this prospective randomized clinical study, we used BPTB allograft (irradiated and non-irradiated) versus autograft to reconstruct the ACL. The purpose of the study was to analyze the clinical outcomes of arthroscopic ACL reconstruction with irradiated BPTB allograft compared with non-irradiated allograft versus autograft. We hypothesized that the clinical outcomes of ACL reconstruction with BPTB irradiated allograft had statistically significant differences compared with those receiving BPTB non-irradiated allograft or autograft according to the objective and subjective evaluations. While the clinical outcomes between the non-irradiated allograft and autograft groups showed no statistical significance.
Methods
Patients and inclusion criterion
From July 2004 through June 2006, 158 patients with acute or chronic ACL ruptures underwent ACL reconstruction, 126 of these patients were eligible to participate in the study according to the preoperative examination. The study obtained the permission of the Medical Ethical Committee.
Patients were excluded from the study if they had had a previous injury or surgery on the affected knee, multiple ligamentous injuries, malalignment, or lacked the ability to complete the study protocol. Revision reconstruction and patients with associated injuries of the posterior cruciate ligament or the posterolateral corner, with deficiency or a reconstruction of the anterior cruciate ligament in the contralateral knee, were also excluded. Only primary unilateral reconstructions of the ACL were included in the study. Patients with minor medial collateral ligament sprains (<Grade-II), previous diagnostic arthroscopy or meniscal tears were not excluded from the study.
To meet the inclusion criterion, all patients were examined carefully in clinics and also preoperatively under anesthesia. All patients had a preoperatively magnetic resonance imaging (MRI) scan to exclude combined complicated ligament injuries to their knees.
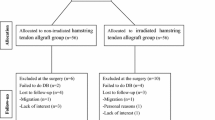
One hundred and two patients provided written informed consent to participate in the study. They were randomized on the day of surgery using a computer to BPTB autograft group (Auto group, number 1–34), irradiated allograft group (Ir-Allo group, number 35–68) and non-irradiated allograft group (Non-ir-Allo group, number 69–102).
Harvest and preparation of grafts
The central third BPTB autograft was harvested through an 8–10 cm incision centered over the medial aspect of the patellar tendon. The paratendon was incised and preserved for closure. Patellar tendon graft, 10 mm wide, was obtained with a 10 × 25 mm patellar bone plug and a 10 × 30 mm tibial bone plug. BPTB allograft was obtained from a certified tissue bank, which was 12 mm wide and prepared with a 10 × 25 mm patellar bone plug and a 10 × 30 mm tibial bone plug.
All the allografts were fresh-frozen and supplied by a certified tissue bank which had policies for serologic and microbiologic testing in accordance with guidelines set forth by AATB and FDA. The irradiated allografts received an irradiation dose of 2.5 Mrad prior to distribution. On the day of the operation the graft was thawed in sterile physiologic fluid at room temperature before preparation, and then preconditioned using the Graftmaster board (Arthrex) at 15 lb of tension for 10–20 min. After that the allograft was soaked in 0.05% PVP for 10 min.
Surgical technique
All patients underwent an examination under anesthesia and diagnostic arthroscopy to confirm the preoperative diagnosis. All the ACL reconstruction procedures were performed by the same experienced arthroscopic surgeon.
The same surgical technique was used in all the groups. This endoscopic technique consisted of the standard arthroscopic ACL reconstruction with grafts. Before the reconstruction, meniscal pathology was addressed. Tears in the red–red or red–white zone were repaired using an inside-out technique. A partial meniscectomy was performed for irreparable tears. Debridement or hole-drilling was done to the chondral damages. No patients needed concomitant surgery for medial or lateral collateral ligament injuries. All the graft fixations were accomplished by using titanium or bioabsorbable interference screws (Arthrex, Naples, FL, USA) that were size-matched to the bone plugs. Note that during fixation on the tibial side the tibia was loaded with a maximal posterior force to minimize graft laxity present at the time of surgery. An intraoperative radiograph was obtained to verify correct placement of graft and screw. Then, the knee was taken through a full ROM to observe any graft impingement. Routine closure of all wounds was performed. After surgery the knee was placed in a standard postoperative brace locked in extension and the rehabilitation protocol was applied.
Rehabilitation
Our rehabilitation protocol began at the time of the initial diagnosis. In this period of before surgery, patients participated in physical therapy to restore full knee ROM and a normal gait and to eliminate knee swelling. After ACL reconstruction, all patients of the three groups followed the same postoperative accelerated rehabilitation protocol, which emphasized early restoration of full extension and strengthening exercises. Active, non-weight-bearing straight leg raise was encouraged to strengthen the quadriceps immediately after surgery to prevent extension lag. Hamstring stretches exercises were also done at the same time and progressed to weight-bearing gastroc/soleus stretches. CPM began the day after surgery for two hours twice a day. Patients would start between 0 ~ 45°and increased 10° per day as tolerated to a maximum of 120°. Progression of weight bearing with crutches or canes was on an as tolerated basis, being guided by the presence and degree of pain and swelling. Crutch or cane use could be discontinued when gait was normalized. Closed kinetic chain exercises initiated 6 weeks postoperatively. Proprioception activities, such as slide board, use of ball, raquet with balance activities, etc. as well as aquatic program including pool running and swimming were allowed to do 8 weeks postoperatively and extended through approximately 6 months. Functional activities including walking, jogging and running were permitted at 6 months postoperatively. Usually 10–12 months was needed for patients to return to work or full sports activity. Appropriate modifications to the ROM limits and weight bearing status were made for concomitant meniscal repairs and chondral treatment. A functional brace was recommended for use during sports activities for the first 1 ~ 2 years after surgery.
Clinical evaluation
Assessments of the involved knee were performed pre and postoperatively to obtain objective and subjective measures of the clinical outcomes of the ACL reconstruction.
Evaluations included: the Lachman test, anterior drawer test (ADT), pivot shift test, varus/valgus stress test, KT-2000 arthrometer testing, Harner’s vertical jump and Daniel’s one-leg hop tests, ROM of knee, Tegner activity score and Lysholm knee scoring scale, Cincinnati knee score, as well as the standard knee ligament evaluation form of the International Knee Documentation Committee (IKDC). According to the IKDC, all the parameters can be placed into one of four categories: normal (A), nearly normal (B), abnormal (C), or severely abnormal (D).
Examination of knee laxity included the Lachman test, ADT, the pivot shift test, varus/valgus stress test, as well as the KT-2000 arthrometer testing. Laxity was graded relative to the noninvolved side according to IKDC guidelines. The following definition was used: Lachman test and ADT: grade 0, −1 to 2 mm; grade I, 3–5 mm; grade II, 6–10 mm; grade III, >10 mm. Pivot shift test: grade 0, equal; grade I, glide; grade II, clunk; grade III, gross. The IKDC classifies knees that are within 5 mm of a contralateral normal knee by means of KT-2000 (MedMetric Inc., San Diego, CA, USA) as being of “normal” stability (normal, <3 mm; nearly normal, 3–5 mm). Knees that have a greater than 5 mm difference are classified as having “abnormal” stability (abnormal, 6–10 mm; severely abnormal, >10 mm). Manual-maximum KT-2000 tests were performed to assess anterior laxity with the knee positioned in the 15° flexion. Side-to-side differences in anterior laxity were determined. Varus/valgus stress tests were used to evaluate the conditions of collateral ligaments preoperatively.
Functional tests included ROM of knee, as well as Harner’s vertical jump and Daniel’s one-leg hop tests.
In the IKDC Knee Examination Form, extension was compared to the contralateral normal side and was graded as normal (<3°LOE), nearly normal (3°–5°LOE), abnormal (6°–10°LOE) or severely abnormal (>10°LOE); flexion was compared to the contralateral normal side and was graded as normal (≤5°LOF), nearly normal (6°–15°LOF), abnormal (16°–25°LOF) or severely abnormal (>25°LOF).
The Vertec unit (Sports Imports Inc., Columbus, OH, USA) was used to perform Harner’s vertical jump test and a tape measure affixed to the floor was used to measure the Daniel’s one-leg hop. The patient performed three trials on each leg. The average of the three trials was used to determine the vertical jump and hop indices by dividing the involved leg by the noninvolved leg and multiplying by 100%. A quotient (%)was used to determine the limb symmetry index (normal, ≥90%; nearly normal, 76% ~ 89%; abnormal, 50% ~ 75%; or severely abnormal, <50%).
Subjective evaluation included Cincinnati knee score, and IKDC Subjective Knee Form which consisted of a questionnaire rating symptoms of pain, swelling, instability and so on. According to the subjective IKDC, higher scores (maximum, 100) reflected fewer symptoms and better knee function.
The Tegner activity score (maximum, 10) and the Lysholm knee scoring scale (maximum, 100) were also used to assess patient’s activity level and knee function preoperatively, postoperatively and at the final follow-up.
At the clinical follow-up, all patients were examined by an orthopedic surgeon who was not the operative surgeon and did not know which type of graft being used for the patient’s ACL reconstruction. The patients were aware of the type of procedure at the follow-up examination as they had been informed by the senior surgeon. The clinical follow-up was similar to the preoperative examination.
Statistical analysis
We used SPSS for Windows (version 12.0; SPSS Inc., Chicago, IL, USA) for statistical analysis. Descriptive statistics, including frequency counts for categorical and ordinal variables and means, medians, standard deviations, and ranges for continuous variables, were calculated. The independent t test was used for the comparison of continuous variables, and the chi-squared test was used for the categorical variables. The significance level was set at P ≤ 0.05; a P value above this threshold would indicate a lack of statistical significance.
Results
Subjects
At the time of surgery, it was determined through arthroscopy that 2 of the 102 patients enrolled in the study were ineligible for participation (1 who did not sustain an ACL rupture, 1 who also had posterior ligament injuries). Of those remaining 100 patients, 99 (Auto 33, Non-Ir-Allo 34, Ir-Allo 32) were available for the full evaluation, only one patient was lost to follow-up, who was known having died with a satisfactory clinical outcome of the ACL reconstruction.
These 99 patients (70 men and 29 women) had a mean 31 months (range 24–47 months) follow-up after ACL reconstruction. The average age of the 99 patients at the time of index operation was 30.6 years (range 16–64 years). The median interval between the injury and the ACL reconstruction was 1.6 months (range, 2 weeks–3 months). Sporting activities were the main cause of injury of the patients. Playing football and basketball were the most common injury-causing sports. Patients’ demographics and characteristics are outlined in Table 1.
General results
The average duration of the autograft procedure (mean 95.6 min; range 75–120 min) was 29.8 min longer compared to allograft procedure (mean 65.8 min; range 55–90 min). The mean postoperative duration of fever (>37°C) of the Non-Ir-Allo group (mean 7.8 days; range 5–13 days) was 3.1 days longer than the Auto group (mean 4.7 days; range 3–7 days). Significant difference was found between the two groups according to the evaluation above (P < 0.001). For the Ir-Allo group, the average of the postoperative duration of fever was 8.8 days (range 6–15 days), when compared this with the Non-Ir-Allo group, no statistically significant difference was found (P > 0.05), but there was a trend that the Ir-Allo group had a longer duration of fever postoperatively. When the patients had fever, the laboratory examinations of all patients were almost normal (Blood routine was normal, the values of ESR were 5 ~ 16 mm/h, CRP were 3 ~ 10 mg/l). In the three groups there was no patient with early postoperative infection or wound problems. There was one patient (2.9%) in the Non-Ir-Allo group with a late infection that needed antibiotic treatment. The laboratory examinations of the patient were abnormal with the highest values of ESR, 20 mm/h; CRP, 13 mg/l and WBC, 12 × 109 L−1. After conservative therapy, the case with late infection was cured without arthroscopic procedure or revision surgery. No late infection occurred in the other two groups. There were no other complications happened in the three groups.
Intraoperative findings
Lesions to the meniscus, cartilage and ligament, as well as their arthroscopic therapy to meniscus and cartilage were outlined in Table 2, no treatment was done to the medial ligament injuries.
Objective clinical results
Patients of the Auto group showed no significant better rating according to the χ2 test for the overall IKDC compared to the Ir or Non-Ir-Allo groups (P > 0.05). Though there was a trend of decrease according to IKDC in the Ir-Allo group (Table 3).
The average manual-maximum KT-2000 side-to-side difference in anterior tibial displacement of 15° knee flexion was 2.4 mm in the Auto group, 2.6 mm in the Non-Ir-Allo group and 5.5 mm in the Ir-Allo group. 29 (87.8%) of patients in the Auto group, 29 (85.3%) of patients in the Non-Ir-Auto group and just only 10 (31.3%) in the Ir-Allo group had a side-to-side difference of less than 3 mm. 2 (6.1%) patients in the Auto group and 3 (8.8%) patients in the Non-Ir-Auto group had a side-to-side difference of more than 5 mm, respectively. The rate of laxity with the side-to-side difference more than 5 mm in the Ir-Allo group was as high as 34.4% (11/32). When compared the Ir-Allo group to the other two groups according to KT-2000 test, significant differences were found. There was, however, no significant difference between the Auto and Non-Ir-Allo groups. The average of anterior tibial displacement of patients in the Ir-Allo group was also significantly higher than the other two groups (Table 4).
According to the pivot shift test, ADT and the Lachman test, 31 (93.9%) of patients in the Auto group showed a negative pivot shift test (grade 0) and 2 (6.1%) a grade 1 pivot shift test; 28 (84.8%) showed a negative ADT and 4 (12.1%) a grade 1 ADT; 28 (84.8%) showed a negative Lachman test and 3 (9.1%) a grade 1 Lachman test. The rate of more than grade 1 according to ADT and the Lachman test was 3.0% and 6.1%, respectively. In the Non-Ir-Allo group, 31 (91.2%) of patients showed a negative pivot shift test and 3 (8.8%) a grade 1 pivot shift test; 28 (82.4%) showed a negative ADT and 4 (11.8%) a grade 1 ADT; 28 (82.4%) showed a negative Lachman test and 3 (8.8%) a grade 1 Lachman test. The rate of more than grade 1 according to ADT and Lachman test was 5.9 and 8.8%, respectively. There was no significant difference between the two groups according to the data aforementioned, which showed that the ACL reconstruction with non-irradiated BPTB allograft could also achieve the similar satisfactory stability compared with the BPTB autograft. But the clinical outcomes of ACL reconstruction with irradiated allograft were not satisfied. The negative rate of pivot shift test was 62.5% (20/32), 8 (25.0%) patients showed a grade I and 4 (12.5%) showed a grade II pivot shift test. The laxity rate according to ADT was 28.1% (9/32). When being evaluated according to the more accurate Lachman test, the rate was even much higher, which was 34.4% (11/32). Significant differences were found compared the Ir-Allo group to Auto and Non-Ir-Allo groups according to the tests evaluating laxity rate (Table 5).
Concerning ROM, the vertical jump and one-leg hop tests, all data was collected and comparable between groups at follow up (Table 3). In the Auto group, the normal rates (normal and nearly normal) of ROM, one-leg hop test and vertical jump test compared to the uninjured leg were 91.0, 97.0 and 97.0% respectively, which were 94.1, 94.1 and 97.1%, respectively in the Non-Ir-Allo group, 93.8, 87.5 and 90.6%, respectively in the Ir-Allo group. No significant differences were found between groups undergoing ACL reconstruction.
Subjective clinical results
According to the subjective IKDC, there was no significant difference among the three groups (P > 0.05). The average scores were 88, 89, 84 points, respectively for the Auto, Non-Ir-Allo and Ir-Allo groups. The mean Lysholm and Tegner scores were 90 points and 7.7 points for the Auto group, respectively, 91 points and 7.5 points for the Non-Ir-Allo group, respectively, and 87 points and 7.0 points for the Ir-Allo group, respectively. There was no significant difference between groups. Most patients were satisfied with their performance in sporting activity. For the Cincinnati knee score, no significant differences were found yet between groups. The exact data was shown in Table 6. From the data, we found that there was a trend of decrease of activity level and patients’ subjective rating scores in the Ir-Allo group.
Radiographs
Standardized radiographs (anteroposterior and lateral views) were performed on all patients preoperatively and at final follow-up, to document the pre and postoperative osteoarthritis and the position of the implants. There were no severe preoperative osteoarthritic changes, and at follow-up we did not observe significant progression.
Discussion
Rupture of the ACL is one of the most common sports injuries in active young people [3]. Lots of studies [9, 11] have proved that a torn ACL cannot heal with conservative management and repair alone. Today, arthroscopic reconstruction of the injured ACL with autologous BPTB is considered the gold standard and first choice of many surgeons for a variety of reasons [13]. However, BPTB autograft ACL reconstruction is also associated with troublesome donor-site morbidity, including patellar fracture, patellar tendonitis or rupture, patellar infra syndrome, quadriceps weakness, arthrofibrosis, anterior knee pain, tenderness, disturbance in anterior knee sensitivity and the inability to kneel. In addition, the overall costs of autograft ACL reconstruction can be greater than that of allograft because of increased surgical and anesthesia time according to recent report [7]. As a result, many surgeons have been using allografts in an attempt to avoid such problems.
In 1984, Shino et al. [33] described the replacement of the ACL by an allogenic tendon graft. Since then there has been an increasing interest in the use of allografts for primary ACL reconstruction and its role is expanding. There are several published clinical studies [6, 19–23, 25, 26, 34] evaluating autograft and allograft used in ACL reconstruction, the findings vary greatly, these discrepancies are due in a large part to the variety of tissues used, the tremendous variation in surgical technique, fixation and postoperative protocols.
In our study, similar clinical outcomes of ACL reconstruction with autograft versus non-irradiated allograft BPTB were found, with no significant difference in postoperative symptoms, active level, functional outcomes, or physical examination measures. From this, we can demonstrate that satisfactory results of ACL reconstruction with non-irradiated allograft can be got with good choice of the type of allograft, correct surgical technique, firm graft fixation, and reasonable rehabilitation protocol. We conclude that allograft can be a reasonable alternative to autograft for ACL reconstruction.
While associated with the use of allograft tissue, one of the major concerns is the risk of disease transmission. Although the risks of transmitting bacterial and viral diseases are low, with the risk for HIV being assessed to be 1 in 1,667,000 [4], in order to provide sterile allograft, significant efforts are being made by tissue banks to further minimize this risk. Apart from donor screening and aseptic harvesting technique, gamma irradiation, which has known bactericidal and virucidal properties, is currently the most popular option for sterilization of allograft.
However, studies [8, 12] have shown that gamma irradiation has adverse effects on biomechanical properties of allograft in a dose-dependent manner. Fideler et al. [12] demonstrated a dose dependent effect of irradiation on both the structural and mechanical properties of human BPTB allograft. Doses as low as 2 Mrad resulted in a statistically significant reduction in biomechanical properties. The effect became more significant with the increase of the dose. More recently, Curran et al. [8] also studied the effect of irradiation on the cyclic and failure properties of human BPTB allograft. The study showed that the low dose of 2 Mrad of irradiation could reduce the initial stiffness and strength of tendon allograft. The authors thought that the alteration in biomechanical properties may be detrimental to graft function and affect the clinical outcomes when used to reconstruct the ACL. They suggested the use of non-irradiated rather than irradiated allograft to avoid weakening effects of radiation on the graft. Rappe et al. [28] studied the effect of irradiation on clinical outcomes of ACL reconstruction, they found the irradiated group had an unacceptable higher rate (33%) than the non-irradiated group (2.4%). However, in 2006, Rihn et al. [29] reported patients undergoing ACL reconstruction with irradiated BPTB allograft had similar clinical outcomes compared to those reconstructed with BPTB autograft.
Resuming our study, when comparing the clinical outcomes of ACL reconstruction with irradiated BPTB allograft to non-irradiated allograft and autograft, we found an increase in anterior laxity or rate of graft rupture in patients who underwent reconstruction with irradiated BPTB allograft according to the ADT, Lachman test and maximal manual KT-2000 test. The rate of rotational instability also increased according to pivot shift test. The difference was statistically significant. Similarly, a meta-analysis [27] of the stability of irradiated allograft compared to non-irradiated allograft showed that irradiated grafts had an abnormal stability rate of 31 versus 12% for non-irradiated grafts, another reason against the use of irradiated allograft.
Therefore in recent years most grafts have been used without any form of sterilization to avoid the known adverse effects of radiation on the graft. But it has been shown that a time window exists after obtaining certain bacterial or viral infections [5], which cannot be detected with currently available techniques. It is felt by many surgeons that unsterilized grafts pose unacceptable levels of risk to patients. The use of radiation is increasing now.
In our study, although every effort was made, the postoperative duration of fever in Allo group was still much longer than that in Auto group, but there was no difference in laboratory examinations which were almost all normal except the one patient in Non-Ir-Allo group with late septic arthritis. We considered the reason of long time fever was associated with the host immune response to allograft, heat of absorption and the real ability of tissue banks in our country to process allografts. The exact reason need to be further studied. Fortunately, the longer duration of fever did not affect the clinical outcomes of patients. For the one case of late septic arthritis in the Non-Ir-Allo group, as we did not get specimen for culture and the patient was cured with conservative treatment, the exact reason for the infection was unclear.
The aim of the use of gamma irradiation was to sterilize the allograft. However, Fideler et al. [12] found that the dose of 2.5 Mrad, which was a dose commonly used by tissue banks for sterilization, was just bacteriocidal but ineffective in eliminating viruses such as HIV. Doses of 3 ~ 4 Mrad were necessary to inactivate the virus. Grieb et al. [16] also proved that lower levels of radiation may be inadequate to kill hepatitis and HIV viruses with a dose of 5 Mrad being necessary. When dose is increased, its clinical implications increase correspondingly. We must ask that as there are adverse effects to gamma irradiation and its failure to sterilize as required, why are we using this method? To avoiding the disease transmission thoroughly, new alternative sterilization techniques are needed that provide not only a complete protection against bacterial and viral infections but also without interference with the biomechanical properties of the grafts.
With regards to IKDC, function and activity level of the operated knee at the follow-up, maybe the follow-up time was not long enough. No significant differences were found among the three groups according to the overall IKDC rating, Harner’s vertical jump and Daniel’s one-leg hop tests, Tegner activity score and the Lysholm knee scoring scale. There was also no significant difference according to the subjective evaluations. But there was a trend toward decrease of the IKDC rating, functional and active level of the operated knee with the irradiated BPTB allograft for reconstruction. The patients in the Ir-Allo group also felt uncomfortable more often than the other two groups. We believe that as time goes on, the functional and active levels of the patients in irradiated group will decrease significantly, as the operated knee now has represented serious laxity.
As to the ROM, none of the patients in each of the three groups developed loss of extension or flexion postoperatively that required manipulation or debridement. As several studies [18, 24, 29, 32] reported, we found that individuals who had an autograft reconstruction had significant numbness and dysesthesia in the area of the incision than individuals who underwent allograft reconstruction, but there was no difference in patient-reported problems with kneeling.
Mentioning radiograph, Rihn et al. [29] showed that the development of radiographic degenerative changes were related to the patient age, time from initial injury to surgery, and the status of the cartilage and menisci at the time of reconstruction. Shelbourne et al. [31] also reported similar findings in patients who had articular cartilage and meniscus damage at the time of ACL reconstruction increased arthritic changes on follow-up. Learning from this, in our study, at the time of the primary ACL reconstruction, partial meniscectomy and meniscal repair were done for the meniscal injury, debridement and hole-drilling were given for the cartilage damage. At the postoperative follow-up all patients undergoing BPTB ACL reconstruction had normal radiographs of the medial, lateral and femorotibial compartments and no significant degenerative changes were found. This may be explained by the restoration of stability of the injured knee according to ACL reconstruction, treatment for the meniscus and cartilage, the relative young age, short median time from injury to surgery, as well as the strict inclusion criteria of patients.
This study had several limitations. The first was the observer bias. The data was collected by only one fellowship-trained surgeon at one institution and was not collected in a blinded fashion. Patients were informed as to the type of surgery by the surgeon after surgery, so the data collector may also have been aware at the time of the follow up. Additionally the incisions could also tip off the observer to the type of surgery. Secondly, although a standardized therapy protocol was prescribed to all patients postoperatively, the quality and consistency of the physical therapy may have varied at outside institutions. This can be a factor that affects the clinical outcomes. Furthermore, the follow-up time of the study is relatively short, long term follow-up should be done to further evaluate the clinical outcomes of irradiated allograft and non-irradiated grafts. Finally, this is a single-surgeon study, and the results may not be generalized.
Conclusion
Patients undergoing ACL reconstruction with non-irradiated BPTB allograft or autograft had similar clinical outcomes. Non-irradiated BPTB allograft is a reasonable alternative to autograft for ACL reconstruction. While the short term clinical outcomes of the ACL reconstruction with irradiated BPTB allograft were adversely affected. The less than satisfactory results led the senior authors to discontinue the use of irradiated BPTB allograft in ACL surgery and not to advocate the use of gamma irradiation as a secondary sterilized method. Further research into alternatives to gamma irradiation is needed.
References
Balsly CR, Cotter AT, Williams LA et al (2008) Effect of low dose and moderate dose gamma irradiation on the mechanical properties of bone and soft tissue allografts. Cell Tissue Bank 9:289–298
Barrett G, Stokes D, White M (2005) Anterior Cruciate Ligament Reconstruction in Patients Older Than 40 Years: Allograft versus Autograft Patellar Tendon. Am J Sports Med 33:1505–1512
Boni DM, Herriott GE (2002) Hamstring tendon graft for anterior cruciate ligament reconstruction. AORN J 76:610–624
Buck BE, Malinin TI, Brown MD (1989) Bone transplantation and human immunodeficiency syndrome (AIDS). Clin Orthop 240:129–135
Busch MP, Kleinman SH (2000) Committee report. Nucleic acid amplification testing of blood donors for transfusion-transmitted infectious diseases: report of the interorganizational task force on nucleic acid amplification testing of blood donors. Transfusion 40:143–159
Chang SKY, Egami DK, Shaib MD et al (2003) Anterior cruciate ligament reconstruction: allograft versus autograft. Arthroscopy 19:453–462
Cole DW, Ginn TA, Chen GJ et al (2005) Cost comparison of anterior cruciate ligament reconstruction: autograft versus allograft. Arthroscopy 21:786–790
Curran AR, Adams DJ, Gill JL et al (2004) The biomechanical effects of low-dose irradiation on bone-patellar tendon-bone allografts. Am J Sports Med 32:1131–1135
Daniel DM, Stone ML, Dobson BE et al (1994) Fate of the ACL-injured patient: a prospective outcome study. Am J Sports Med 22:632–644
Deehan DJ, Salmon LJ, Webb VJ et al (2000) Endoscopic reconstruction of the anterior cruciate ligament with an ipsilateral patellar tendon autograft. J Bone Joint Surg Br 82B:984–991
Engebretsen L, Benum P, Fasting O et al (1990) A prospective, randomized study of three surgical techniques for treament of acute ruptures of the anterior cruciate ligament. Am J Sports Med 18:585–590
Fideler BM, Vangsness CT Jr, Lu B et al (1995) Gamma irradiation: effects on biomechanical properties of human bone-patellar tendon-bone allografts. Am J Sports Med 23:643–646
Fu FH, Bennett CH, Ma CB et al (2000) Current trends in anterior cruciate ligament reconstruction. Part II: operative procedures and clinical correlations. Am J Sports Med 28:124–130
Gorschewsky O, Klakow A, Mahn H et al (2007) Clinical comparison of the autologous quadriceps tendon (BQT) and the autologous patella tendon (BPTB) for the reconstruction of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 15:1284–1292
Gorschewsky O, Klakow A, Riechert K et al (2005) Clinical comparison of the tutoplasty allograft and autologous patellar tendon (bone-patellar tendon-bone) for the reconstruction of the anterior cruciate ligament: 2- and 6-year results. Am J Sports Med 33:1202–1209
Grieb TA, Forng RY, Bogdansky S et al (2006) High-dose gamma irradiation for soft tissue allografts: high margin of safety with biomechanical integrity. J Orthop Res 24:1011–1018
Han HS, Seong SC, Lee S et al (2008) Anterior cruciate ligament reconstruction. Quadriceps versus patellar autograft. Clin Orthop Relat Res 466:198–204
Harner CD, Olson E, Fu FH et al (1996) Allograft versus autograft anterior cruciate ligament reconstruction: 3- to 5-year outcome. Clin Orthop 324:134–144
Kustos T, Balint L, Than P et al (2004) Comparative study of autograft or allograft in primary anterior cruciate ligament reconstruction. Int Orthop 28:290–293
Lawhorn KW, Howell SM (2003) Scientific justification and technique for anterior cruciate ligament reconstruction using autogenous and allogeneic soft-tissue. Orthop Clin North Am 34:19–30
Malinin TI, Levitt RL, Bashore C et al (2002) A study of retrieved allograft used to replace anterior cruciate ligaments. Arthroscopy 18:163–170
Nyland J, Caborn DN, Rothbauer J et al (2003) Two-year outcomes following ACL reconstruction with alograft tibialis anterior tendons:a retrospective study. Knee Surg Sports Traumatol Arthrosc 11:212–218
Olson EJ, Harner CD, Fu FH et al (1992) Clinical use of fresh, frozen soft tissue allograft. Orthopedics 15:1225–1232
Peterson RK, Shelton WR, Bomboy AL (2001) Allograft versus autograft patellar tendon anterior cruciate ligament reconstruction: a 5-year follow-up. Arthroscopy 17:9–13
Pritchard JC, Drez D Jr, Moss M, Heck S (1995) Long-term followup of anterior cruciate ligament reconstructions using freeze-dried fascia lata allografts. Am J Sports Med 23:593–596
Prodromos CC, Fu FH, Howell SM et al (2008) Controversies in soft tissue anterior cruciate ligament reconstruction: graft, bundles, tunnels, fixation, and harvest. J Am Acad Orthop Surg 16:376–384
Prodromos CC, Joyce B, Shi K (2007) A meta-analysis of stability of autografts compared to allografts after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 15:851–856
Rappe M, Horodyski M, Meister K et al (2007) Nonirradiated versus irradiated Achilles allograft: in vivo failure comparison. Am J Sports Med 35:1653–1658
Rihn JA, Irrgang JJ, Chhabra A et al (2006) Does irradiation affect the clinical outcome of patellar tendon allograft ACL reconstruction? Knee Surg Sports Traumatol Arthrosc 14:885–896
Schwartz HE, Matava MJ, Proch FS et al (2006) The effect of gamma irradiation on anterior cruciate ligament allograft biomechanical and biochemical properties in the caprine midel at time zero and at 6 months after surgery. Am J Sports Med 34:1747–1755
Shelbourne KD, Gray T (2000) Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery. Five- to fifteen-year evaluations. Am J Sports Med 28:446–452
Shelton WR, Papendick L, Dukes AD (1997) Autograft versus allograft anterior cruciate ligament reconstruction. Arthroscopy 13:446–449
Shino K, Kawasaki T, Hirose H et al (1984) Replacement of the anterior cruciate ligament by an allogeneic tendon graft. J Bone Joint Surg Br 66:672–681
Siebold R, Buelow JU et al (2003) Primary ACL reconstruction with fresh-frozen patellar versus Achilles tendon allografts. Arch Orthop Trauma Surg 123:180–185
Stringham DR, Pelmas CJ, Burks RT et al (1996) Comparison of anterior cruciate ligament reconstructions using patellar tendon autograft or allograft. Arthroscopy 12:414–421
Conflict of interest statement
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by Provincial Science Foundation of China (2004GG2202034).
Rights and permissions
About this article
Cite this article
Sun, K., Tian, S., Zhang, J. et al. Anterior cruciate ligament reconstruction with BPTB autograft, irradiated versus non-irradiated allograft: a prospective randomized clinical study. Knee Surg Sports Traumatol Arthrosc 17, 464–474 (2009). https://doi.org/10.1007/s00167-008-0714-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-008-0714-8