Abstract
The outcomes of 18 patients (11 females, 7 males; age, 40.4±11 years) at 2 years after ACL reconstruction with cryopreserved tibialis anterior allografts using a double bundle technique are presented. Most subjects (72%) described themselves as being moderately active before surgery. After providing written informed consent, subjects completed the 2000 IKDC Knee Form, underwent arthrometric knee measurements, and performed one-leg hop and isokinetic quadriceps and hamstring torque tests (60°/s). Ninety-four percent (17/18) of the subjects had normal or near-normal grades for manual knee ligament tests. Knee arthrometry measurements revealed a mean 1.1-mm involved side increase at 134 N (8.9±2 mm vs 7.8±3 mm) and a 2-mm involved side increase during manual maximum testing (11.3±2 mm vs 9.3±3 mm). Group means revealed active knee flexion (136±8° vs 139±6°) and knee hyper-extension (3±2° vs 5±2°), which were slightly reduced at the involved knee. One-leg hop testing revealed a 15% mean deficit at the involved side (0.81±0.3 m vs 0.95±0.3 m). Isokinetic testing revealed an 11% mean deficit at the involved side (143.4±60 Nm vs 161.8±54 Nm) for the quadriceps and 7% greater strength at the involved side (105.9±35 Nm vs 98.8±35 Nm) for the hamstrings. Side-to-side comparisons revealed that many patients displayed less than normal quadriceps femoris torque (72%, 13/18), hamstring torque (28%, 5/18) and hop test (28%, 5/18) performance. Moderate positive correlations existed between involved side quadriceps (r=0.80) and hamstring (r=0.83) torque/bodyweight and hop test performance. Scores were 77.6±21 (range 28.7–100) and 78.1±16 (range 41.7–100) for the 2000 IKDC Subjective Knee Evaluation and Health Assessment forms. Most subjects (83%, 15/18) rated their current function at ≥91% of pre-injury levels and all subjects continued to participate at their pre-injury perceived activity level. At 2 years after ACL reconstruction with tibialis anterior allografts, this subject group displayed satisfactory functional outcomes. Tibialis anterior allograft use provides an effective ACL reconstruction alternative, particularly for older individuals who want to continue recreational sports.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previous reports have documented the tissue morbidity associated with autogenous bone-patellar tendon-bone (BPTB) graft harvest (including quadriceps femoris inhibition, patella tendon shortening, infrapatellar fat pad fibrosis, patellar fracture) [4, 8, 18, 19, 22, 28] and functional deficits including decreased quadriceps strength, reduced knee range of motion, increased patellofemoral pain and altered patellar alignment [12, 16, 17, 19, 21, 22]. In addition to these early complications, long-term concerns associated with autogenous BPTB graft use include the development of patellofemoral joint arthrosis particularly among individuals who have a predisposition to mal-tracking, and knee joint osteoarthritis [27].
By avoiding tissue harvest in a construct that provides secure bone plug-to-bone tunnel fixation allograft BPTB tissue remains popular for ACL reconstruction. Despite their popularity, BTPB allografts have been shown to have inferior biomechanical properties and less optimal bone tunnel-graft congruity than soft tissue tendon allografts [7, 29]. Additionally, the biomechanical properties of BPTB grafts are more negatively influenced by donor age than are hamstring tendon grafts, and their smaller diameter is more affected by tissue weakening during the remodeling or ligamentization process, particularly at the tendon-bone junctions [29, 30]. Allograft BPTB may also be more likely to display increased immunogenicity compared to other allograft forms, particularly via the osseous component [1, 26].
Problems associated with autogenous and allogeneic BPTB grafts has led to an increased interest in ACL reconstruction using a tripled or quadrupled hamstring autograft consisting of sections of harvested semitendinosus and gracilis muscles. Problems however, such as increased knee joint laxity [3, 16], hamstring muscle group strength deficits [2, 20] and knee flexion range of motion deficits [20] have been reported following ACL reconstruction using hamstring grafts. Given the coxa varus-genu valgus postural alignment common to many athletic females the influence of either autogenous BPTB graft harvest on patellofemoral loading mechanics or semitendinosus-gracilis graft harvest on medial knee joint stability may be detrimental to knee joint function.
Autogenous semitendinosus or gracilis tissue or allograft alternatives such as tibialis anterior tendons present ACL reconstruction substitutes to the knee surgeon that provide considerable graft strength; however, the absence of bone at the tendinous ends remains problematic when graft-bone tunnel fixation is less than optimal [10]. With long-term biomechanical strength characteristics that are comparable to quadruple strand hamstring autografts and superior to BPTB allografts, double strand tibialis anterior tendon allografts provide an effective construct for ACL reconstruction, while avoiding the tissue morbidity commonly associated with autograft harvesting [11, 13, 26, 27]. Haut Donahue et al [11] reported that double strand tibialis anterior grafts provided superior ultimate load (4122±893 N vs 2913±645 N) and comparable linear stiffness (460±101 N/mm vs 418±36 N/mm) to quadrupled semitendinosus-gracilis grafts. Hollis et al. [13] reported mean ultimate load and mean ultimate stress values for fresh frozen single strand tibialis anterior tendons of 3000 N and 84 MPa, respectively.
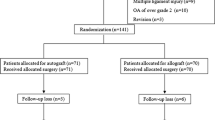
In addition to superior biomechanical characteristics, tibialis anterior allograft use enables decreased operative morbidity, since graft harvest is eliminated and the biarticular semitendinosus and gracilis muscles are spared. The fact that tibialis anterior allografts when used for ACL reconstruction provide comparable biomechanical characteristics to quadrupled semitendinosus-gracilis grafts in a readily available, easily prepared, doubled graft supports consideration of this approach. However, although allograft soft tissue tendon grafts eliminate the donor site morbidity from graft harvest and associated functional deficits, they display slightly greater delays in tendon-bone tunnel osteointegration than their autogenous counterparts [14]. With allograft tissue use there is also an increased possibility of a patient sustaining an immunogenic reaction or disease transfer [1, 14, 26]. The purpose of this retrospective study is to present two-year outcome data of a cohort of patients who underwent unilateral ACL reconstruction with a cryopreserved tibialis anterior allograft using a double bundle technique, and who performed the same accelerated closed kinetic chain emphasis rehabilitation program (6 month duration).
Methods
All subjects received doubled (220 mm), 100 mm×9 mm tibialis anterior allografts (CryoLife, Inc., Marietta, GA) which were tensioned to 10 lb (44.48 N) during preparation. The double bundles were secured with interlocking stitch sutures (no. 5 braided polyester) for 30 mm on the femoral side and for 40 mm on the tibial side, leaving approximately 30 mm of non-stitched intra-articular graft tissue [6]. The graft ends were fixed with bioabsorbable interference screws in bone tunnels that were sized to the nearest 0.5 mm [5]. All patients participated in the same progressive rehabilitation program which focused on the achievement of key functional milestones (Table 1). The rehabilitation program exercise volume parameters reported in Table 1 represent general guidelines. At no time during the rehabilitation program were exercise volume or resistance parameters increased in the absence of appropriate technique (movement quality took precedent over resistance or volume quantity). Whenever possible, individual sports specific activities were included in the treatment plan. Since the knee joint is subjected to 3–5 times greater loading forces during running, jumping and cutting activities than those experienced during walking, appropriate three-dimensional standing postural alignment was deemed essential to facilitate appropriate hip, knee and ankle joint muscle integration during weight bearing activities. The exercise plan was designed to provide safe, progressive impact loading to stimulate functionally relevant lower extremity tissue adaptations and neurodynamic recovery.
At a minimum of 105 weeks after surgery (range 105–140 weeks) 18 patients (7 males, 11 females, ratio 0.64:1), age 40.4±11 years (range 21–58 years), height 1.71±0.08 m, weight 79.1±15 kg, participated in this study. After providing written informed consent, subjects completed the 2000 IKDC Knee Forms. All subjects underwent unilateral ACL reconstruction and had not undergone previous knee surgery. Eriksson et al [9] in an outcome investigation of patients (2.2:1 males to females for BPTB autograft, 0.95:1 for hamstring autograft) who underwent ACL reconstruction reported patient ages of 25.7±6.9 years [9]. Jomha et al. [15] in evaluating the outcomes of 59 patients (2.69:1 males to females) at 7 years post-ACL reconstruction reported ages of 26±7 years during the post-surgery follow-up examination. For this older patient population, scores of 75% or higher were considered to be normal or nearly normal on the 2000 IKDC Health Assessment and Subjective Knee Evaluation, and a grade of normal (A) or nearly normal (B) on the Clinical Examination section of the 2000 IKDC Knee forms was considered indicative of a satisfactory outcome result. Prior to injury, 7 of 18 of patients (39%) perceived themselves to be occasional sporting activity participants, 6 (33%) perceived themselves to be well trained and frequent athletic activity participants, 4 (22%) considered themselves to be non-sporting and 1 (6%) was a highly competitive sports participant. Our standard practice when discussing ACL reconstruction procedures is for patients to be given the option of a tibialis anterior allograft or a semitendinosus-gracilis autograft, following discussion regarding the advantages and disadvantages of each. Because of the aforementioned tissue morbidity concerns following autograft harvest most of our patients select the allograft option. Passive knee range of motion (PROM), peak isokinetic (Biodex Medical Systems Inc., Shirley, NY) quadriceps and hamstring torque (60°/s) and instrumented knee arthrometry tests (Medmetric Corp., San Diego, CA) were also performed. Isokinetic torque grades were based on opposite, nonimpaired side function (normal ≥ 90%, nearly normal = 89–76%, abnormal = 75–50% and severely abnormal <50%). Descriptive statistics and Pearson product moment correlations for delineation of hop test and isokinetic test variable relationships were performed using SPSS version 11.0 software (SPSS Science, Chicago, IL).
Results
During the index surgical procedure, partial medial meniscectomy was performed on 4 of 18 patients, medial meniscal repair was performed on 2 patients, lateral meniscal repair was performed on 1 patient, and partial lateral meniscectomy was performed on 4 patients. At the time of the index surgical procedure 3 patients displayed grade III chondral lesions at the medial femoral condyle, 2 displayed grade II chondral lesions at the medial femoral condyle, and 1 patient displayed a grade III chondral lesion at the lateral femoral condyle. At the time of data collection 4 of 18 patients claimed to be experiencing back pain that limited their activities; however they were not receiving treatment. One subject was receiving treatment for heart disease that limited their activities. Two subjects were receiving treatment for hypertension that limited their activities.
The composite grade from the Clinical Examination section of the 2000 IKDC Knee Examination form revealed that 72% of patients (13/18) graded normal (A), 22% (4/18) of patients graded nearly normal (B), and 6% (1/18) of patients graded abnormal (C). Knee joint laxity, PROM, and isokinetic torque grades are presented in Table 2. Ninety-four percent of subjects (17/18) displayed normal or near normal grades for manual knee ligament tests. Instrumented knee arthrometry revealed similar results at both 134 N (8.9±2 mm vs 7.8±3 mm, 1.1 mm increase) and with manual maximum testing (11.3±2 mm vs 9.3±3 mm, 2 mm increase) for the involved and non-involved knee, respectively. Mean active knee range of motion (136±8° vs 139±6° flexion and 3±2° vs 5±2° hyperextension), peak quadriceps (143.4±60 Nm vs 161.8±53.6 Nm, 11% deficit) and hamstring (105.9±35 Nm vs 98.8±34.8 Nm, 7% increase) torque/bodyweight and single leg hop results (0.81±0.3 m vs 0.95±0.3 m, 15% deficit) were comparable for the involved and non-involved lower extremity. Although involved and non-involved group mean values were comparable, side-to-side comparisons revealed that many patients displayed less than normal isokinetic quadriceps torque (72%, 13/18), hamstring torque (28%, 5/18) and hop test (28%, 5/18) performance capability. Moderate positive correlations existed between surgical side quadriceps torque/bodyweight (r = 0.80), hamstring torque/bodyweight (r = 0.83) and single leg hop test performance capability.
Overall, the 2000 IKDC Health Assessment revealed a score of 78.1±16, range 41.7–100, and the Subjective Knee Evaluation revealed a score of 77.6±21, range 28.7–100 (Fig. 1). All subjects continued to participate at their pre-injury perceived activity level. Subjective function comparisons revealed that 83% (15/18) of patients perceived their current knee joint function to be at ≥91% of pre-injury levels. Three patients perceived their current knee joint function to be <91% of pre-injury levels. One of these patients reported a 28.7 Subjective Knee Evaluation score and a 41.7 2000 IKDC Health Assessment score. This patient displayed abnormal isokinetic quadriceps and hamstring torque values and abnormal single leg hop test performance. This patient also underwent partial medial meniscectomy at the time of ACL reconstruction, and displayed a plethora of activity-limiting health problems including heart disease, high blood pressure and back pain for which treatment was being received. The patient had recently quit smoking within the last 6 months and reported depression as a problem; however, treatment was not being received. A second patient who perceived their current knee joint function to be <91% of pre-injury levels reported a 44.8 Subjective Knee Evaluation score and a 2000 IKDC Health Assessment score of 83.3. This patient displayed nearly normal knee joint laxity during clinical examination and arthrometric testing, and displayed abnormal isokinetic quadriceps torque and nearly normal single leg hop test results. This patient listed back pain and migraines as additional medical problems and had been less than fully compliant with rehabilitation due to taking a new job in a different town. All other patients had been compliant with the outpatient rehabilitation protocol. The third patient who perceived their current knee function to be <91% of pre-injury levels reported a 45 Subjective Knee Evaluation score and a 58.3 2000 IKDC Health Assessment score. This patient displayed abnormal knee joint laxity on clinical examination and arthrometric testing, abnormal isokinetic quadriceps torque and nearly normal single leg hop test results.
Discussion
During ACL reconstruction, the surgeon attempts to re-establish the biomechanical strength and stiffness, physiometry, and knee joint kinematics provided by the native ACL. When the surgeon feels confident that these factors have been adequately re-established progressive rehabilitation is initiated early, with consideration for restoring both local joint and integrated lower extremity joint function to maintain knee joint homeostasis, while creating an environment that facilitates functionally relevant graft ligamentization and neurosensory recovery.
At two-years following ACL reconstruction with tibialis anterior tendon allografts this subject group displayed satisfactory outcome results. Using the original IKDC Knee Ligament Standard Evaluation to evaluate the 5-year outcomes of two groups of 90 patients (BPTB graft vs hamstring tendon graft), Pinczewski et al. [24] reported that more than 95% of patients in each group had an overall subjective functional assessment of normal (grade A) or nearly normal (grade B) at a minimum of 5 years post-surgery. The original IKDC standard evaluation form relied on a 4 category ordinal scale. The Subjective Knee Evaluation section of the 2000 IKDC Knee Form provides a more detailed and potentially more critical consolidated score for the patients perceived knee symptoms, ability to participate in sports activities, and perceived knee function during daily activities. When the survey scores for the two patients who were either non-compliant with rehabilitation or had back pain were removed from the group average, the 2000 IKDC Health Assessment score and the Subjective Knee Evaluation scores would be 80.4±15, and 82.7±18, respectively. We consider these results to be satisfactory given the number of patients with chondral (33%, 6/18) or meniscal (50%, 9/18) lesions at the time of the index surgical procedure. At two-year post-surgery, this patient group reported an 8.5% perceived function deficit compared to pre-operative levels (8.6±1.7 vs 9.4±1.4) and all subjects continued to participate at their pre-injury activity level. There was a fair relationship between subject scores on the 2000 IKDC Subjective Knee Evaluation and Health Assessment (SF-36) (Fig. 2) suggesting how improved knee function displayed a direct, moderate relationship to general health.
The high percentage of patients who displayed below normal peak isokinetic quadriceps torque (72%, 13/18) and below normal hop test results (28%, 5/18) raises concerns over dynamic knee stabilization capability. As discussed earlier, concomitant general health problems, poor patient compliance, and abnormal levels of knee joint laxity at least partially explain the poor results for 3 patients. In a two-center study of 164 patients with unilateral ACL reconstruction at a mean 31 months (24–59 month range) post-surgery, Eriksson et al [9] reported that an associated meniscal and ACL injury at the time of ACL reconstruction was a strong predictive factor for a less than optimal functional outcome. Jomha et al. [15], in evaluating 59 patients 7 years post-ACL reconstruction, reported that lower IKDC grades were associated with meniscectomy, ligamentous laxity and radiologically demonstrable changes. Perhaps the high percentage of our patients who displayed associated meniscal (50%, 9/18) or chondral (33.3%, 6/18) injury negatively influenced our outcome measurement scores. The retrospective nature of the study makes it difficult to relate changes in general health status to changes in knee joint function over time.
Another possible reason for decreased dynamic knee stabilization may have been the rehabilitation emphasis on weight bearing, functional activities and therapist concerns over protecting graft fixation over the initial 8–12 weeks following surgery, given the delayed osteo-integration that has been identified when using soft tissue allografts [23, 25]. Integrated closed kinetic chain exercise regimens are essential for developing dynamic three-dimensional control of the long axis of the femur and tibia via combined hip and knee joint muscle function. However, supplementary isolated quadriceps and hamstring neuromuscular re-education through progressive resistance multi-planar exercises in weight bearing and non weight bearing may effectively minimize patient disability related to quadriceps and hamstring impairments without compromising soft tissue graft fixation during the initial 8–12 weeks following surgery.
Based on these findings we continue to recommend ACL reconstruction with cryopreserved tibialis anterior tendon. However, as with other graft types concern must be given to the effect of associated meniscal and/or chondral injuries and general patient health on functional outcome expectations. Given its inherent biomechanical strength in double bundle configurations the tibialis anterior allograft may also be a promising surgical option for younger, athletic patients who place greater relative loads at higher frequencies and velocities across the knee joint. As with all soft tissue graft constructs, adequate femoral and tibial tunnel fixation in bone of sufficient mineral density and proper graft orientation and tension are vital to ultimate surgical effectiveness [14]. These considerations are especially important given the delayed graft remodeling and revascularization process associated with soft tissue allograft use [14, 21, 26]. These data are presented as an initial step in acquiring a normative patient outcome database. The retrospective nature of this investigation limits a more detailed discussion of changes from time zero prior to surgery. Further prospective studies of age- and sex-specific differences following ACL reconstruction with tibialis anterior allograft tissue and progressive rehabilitation are in progress.
References
Anonymous (2001) Update: Unexplained deaths following knee surgery—Minnesota, 2001. MMWR 50:1080
Aune AK, Holm I, Risberg MA, Jensen HK, Steen H (2001) Four-strand hamstring tendon autograft compared with patellar tendon-bone autograft for anterior cruciate ligament reconstruction. A randomized study with two-year follow-up. Am J Sports Med 29:722–728
Barrett GR, Noojin FK, Hartzog CW, Nash CR (2002) Reconstruction of the anterior cruciate ligament in females: A comparison of hamstring versus patellar tendon autograft. Arthroscopy 18:46–54
Bonatus TJ, Alexander AH (1991) Patellar fracture and avulsion of the patellar ligament complicating arthroscopic anterior cruciate ligament reconstruction. Orthop Rev 20:770–774
Caborn DNM, Selby JB (2002) Allograft anterior tibialis tendon with bioabsorbable interference screw fixation in anterior cruciate ligament reconstruction. Arthroscopy 18:102-105
Charlick DA, Caborn DNM (2000) Technical note: alternative soft-tissue graft preparation technique for cruciate ligament reconstruction. Arthroscopy 16:E20
Cooper DE, Deng XH, Burstein AL, Warren RF (1993) The strength of the central third patellar tendon graft. a biomechanical study. Am J Sports Med 21:818–823
DuMontier TA, Metcalf MH, Simonian PT, Larson RV (2001) Patella fracture after anterior cruciate ligament reconstruction with the patellar tendon: a comparison between different shaped bone block excisions. Am J Knee Surg 14:9–15
Eriksson K, Anderberg P, Hamberg P, Lofgren AC, Bredenberg M, Westman I, Wredmark T (2001) A comparison of quadruple semitendinosus and patellar tendon grafts in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br 83:348–354
Harris NL, Indelicato PA, Bloomberg MS, Meister K, Wheeler DL (2002) Radiographic and histologic analysis of the tibial tunnel after allograft anterior cruciate ligament reconstruction in goats. Am J Sports Med 30:368–373
Haut Donahue TL, Howell SM, Hull ML, Gregersen C (2002) A biomechanical evaluation of anterior and posterior tibialis tendons as suitable single-loop anterior cruciate ligament grafts. Arthroscopy 18:589–597
Heimstra LA, Webber S, MacDonald PB, Kriellaars DJ (2000) Knee strength after hamstring tendon and patellar tendon anterior cruciate ligament reconstruction. Med Sci Sports Exerc 32:1472–1479
Hollis JM, Pearsall AW IV, Stutuz JD, Russell GV (2001) The biomechanical properties of the tibialis anterior, tibialis posterior and peroneus longus tendons as potential graft sources. Orthop Trans 26, abstract 715
Jackson DW, Corsetti J, Simon T (1996) Biologic incorporation of allograft anterior cruciate ligament replacements. Clin Orthop Rel Res 324:126–133
Jomha NM, Pinczewski LA, Clingeleffer A, Otto DD (1999) Arthroscopic reconstruction of the anterior cruciate ligament with patellar-tendon autograft and interference screw fixation: the results at seven years. J Bone Joint Surg Br 81:775–779
Kartus J, Movin T, Karlsson J (2001) Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy 17:971–980
Keays SL, Bullock-Saxton J, Keays AC, Newcombe P (2001) Muscle strength and function before and after anterior cruciate ligament reconstruction using semitendinosus and gracilis. Knee 8:229–234
Miller MD, Nichols T, Butler CA (1999) Patella fracture and proximal tendon rupture following arthroscopic anterior cruciate ligament reconstruction. Arthroscopy 15:640–643
Moebius UG, Georgoulis AD, Papageorgiou CD, Papadonikolakis A, Rossis J, Soucacos PN (2001) Alterations of the extensor apparatus after anterior cruciate ligament reconstruction using the medial third of the patellar tendon. Arthroscopy 17:953–959
Nakamura N, Horibe S, Sasaki S, et al (2002) Evaluation of active knee flexion and hamstring strength after anterior cruciate ligament reconstruction using hamstring tendons. Arthroscopy 18:598–602
Noyes FR, Barber-Westin SD (1996) Reconstruction of the anterior cruciate ligament with human allograft. Comparison of early and later results. J Bone Joint Surg Am 78:524–537
Petsche TS, Hutchinson MR (1999) Loss of extension after reconstruction of the anterior cruciate ligament. J Am Acad Orthop Surg 7:119–127
Pinczewski LA, Clingeleffer AJ, Otto DD, Bonar SF, Corry IS (1997) Integration of hamstring tendon graft with bone in reconstruction of the anterior cruciate ligament. Arthroscopy 13:641–643
Pinczewski LA, Deehan DJ, Salmon LJ, Russell VJ, Clingeleffer A (2002) A five-year comparison of patellar tendon versus four-strand hamstring tendon autograft for arthroscopic reconstruction of the anterior cruciate ligament. Am J Sports Med 30:523–536
Rodeo SA, Arnoczky SP, Torzilli PA, Hidaka C, Warren RF (1993) Tendon-healing in a bone tunnel. A biomechanical and histological study in the dog. J Bone Joint Surg Am 75:1795-1803
Shino K, Inoue M, Horibe S, Hamada M, Ono K (1990) Reconstruction of the anterior cruciate ligament using allogeneic tendon: long term follow up. Am J Sports Med 18:457–465
Shino K, Kimura T, Hirose H, Inoue M, Ono K (1986) Reconstruction of the anterior cruciate ligament by allogeneic tendon graft. An operation for chronic ligamentous insufficiency. J Bone Joint Surg Br 68:739–746
Shino K, Nakagawa S, Inoue M, Horibe S, Yoneda M (1993) Deterioration of patello-femoral articular surfaces after anterior cruciate ligament reconstruction. Am J Sports Med 21:206–211
Shino K, Oakes BW, Horibe S, Nakata K, Nakamura N (1995) Collagen fibril populations in human anterior cruciate ligament allografts. Am J Sports Med 23:203–209
Tomita F, Yasuda K, Mikami S, Sakai T, Yamazaki S, Tohyama H (2001) Comparisons of intraosseous graft healing between the doubled flexor tendon graft and the bone-patella tendon-bone graft in anterior cruciate ligament reconstruction. Arthroscopy 17:461–476
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nyland, J., Caborn, D.N.M., Rothbauer, J. et al. Two-year outcomes following ACL reconstruction with allograft tibialis anterior tendons: a retrospective study. Knee Surg Sports Traumatol Arthrosc 11, 212–218 (2003). https://doi.org/10.1007/s00167-003-0371-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-003-0371-x