Abstract
A case of a 42-year-old male patient with symptomatic juxtaarticular osteoid osteoma of the capitulum humeri is presented. After the clinical diagnosis was confirmed with plain radiographs, bone scan, computer tomography and magnetic resonance imaging, the patient underwent arthroscopic removal of the lesion. A partial synoviectomy was performed first and then the center of the lesion was marked with Kirschner wire using the X-ray monitoring. The marked lesion was transarticularly removed with a motorized shaver device. Post-operatively, the patient reported prompt relief of pain that had not reoccurred during 1 year of follow up. To the authors’ knowledge, this is the first report of the arthroscopic removal of juxtaarticular osteoid osteoma of the humeral capitulum which promises to be an effective and less invasive alternative to the existing treatment options.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoid osteoma is a benign osteoblastic bone tumor, generally encountered in the first three decades of life and affecting males twice as frequently as females [1]. The lesion is classified according to the location of the nidus as cancellous or cortical, the later subperiostal, intracortical or subcortical [2]. About 50% of osteoid osteomas occur in the femur and tibia (diaphyseal shaft or toward the metaphysis), followed by the other long bones and the spine [1]. Patients typically complain of pain that is worse at night and is relieved by salicylates. Plain radiographs may reveal a well-demarcated central nidus, usually smaller than 1 cm, surrounded by a distinct zone of reactive sclerosis [3]. The diagnosis is confirmed on the basis of a Technetium-99m bone scan together with thin-section computer tomography (CT) [1, 3]. Juxtaarticular and intraarticular osteoid osteomas are rare and usually present with atypical clinical picture mimicking more common entities such as monoarticular arthritis [4–6]. As plain radiographs may also be inconclusive, these osteoid osteomas tend to be missed, and it may take several months or even more than two years to make a correct diagnosis. During that period, the patients may be unsuccessfully treated or operated on uncritically for some other diagnosis, which may lead to joint contractures, secondary degenerative changes of the articular cartilage and, rarely, to growth disturbances and limb deformities in adolescents [4, 7–9].
Case report
A 42-year-old right-handed man presented in the outpatient office with a two-and-a-half-year history of pain and swelling of his left elbow. The onset of pain coincided with a trivial contusion of the lateral epicondyle. The pain was typically described as mild during the day time and more intense during the night. It was slightly relieved by oral salicylates. The patient had undergone previous unsuccessful conservative treatment and even an operation (Bosworth-Boyd) for suspected lateral epicondylitis.
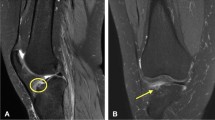
Physical examination revealed a 15° flexion contracture of the left elbow. Palpatory pain was located just above the radial head. Standard plain radiographs of the elbow revealed an 8-mm nidus with 3 mm of central sclerosis, surrounded by a thin layer of reactive sclerosis, located in the region of the humeral capitulum (Fig. 1a). The magnetic resonance imaging (MRI) showed a signal of mixed intensity, surrounded by a distinct layer of decreased intensity that suggested a bone edema in the posterior part of the humeral capitulum (Fig. 1b). There was also mild synovitis. The diagnosis of osteoid osteoma was confirmed by the Technetium-99m bone scan and a CT scan (Fig. 1c, d).
Osteoid osteoma of a right capitulum humeri in 42-year-old male patient—diagnostic investigations. a AP plain radiograph: a nidus in capitulum humeri with small central sclerosis surrounded by reactive sclerosis (arrow). b MRI: a signal of mixed intensity, surrounded by a distinct layer of decreased intensity representing edema of the bone, located in the posterior part of capitulum humeri (arrow). Signs of mild synovitis are present. c Technetium-99m bone scan: clearly visible “hot spot” in the capitulum humeri. d Sagital CT section: A nidus of 8 mm in diameter with 3-mm large central and distinct peripheral reactive sclerosis in posterior region of capitulum humeri (arrow)
The patient underwent arthroscopic removal of the lesion in March 2005. The arthroscope was introduced in the joint through a high posterolateral portal. A partial synoviectomy was performed through a low posterolateral portal, thus, affording visualization of the humeral capitulum (Fig. 2a). The center of the lesion under the smooth articular surface was marked with a 1.2 mm Kirschner wire under radiographic control (Fig. 2b). It was demarcated with a cautious palpation (Fig. 2c) and removed transarticularly through the same low posterolateral portal using a 4.5 mm motorized shaver (Fig. 2d). During the removal, the lesion was fragmented and was therefore not sent for histopathological diagnosis.
The patient reported of a prompt pain relief on the first postoperative day. Normal range of motion was restored within 1 month and the patient gradually returned to full activity. There were no post-operative complications that followed the arthroscopic removal. One year after the surgery, the area from where the lesion had been removed was no longer detectable on radiographs.
Discussion
Juxta- and intraarticular osteoid osteomas, as well as their atypical clinical presentation and possible absence of nidus surrounded by reactive sclerosis on plain radiographs, may delay the diagnosis and treatment for months or even years [4–6]. The same holds true for the case reported: a review of our patient’s records and radiographs revealed no evidence that would suggest the diagnosis of osteoid osteoma. The history of contusion injury and the patient’s age were further misleading. Juxta- and intraarticular osteoid osteomas tend to be manifested by pain, which is usually less severe, and the response to salicylates is less dramatic than in the diaphyseal lesions, which was also reported by our patient [4–6]. Despite the vagueness of diagnosis, the patient was scheduled for an “empirical” operation, which turned to be inadequate.
Thin-section CT scan is the best diagnostic tool to confirm the nidus surrounded by sclerosis typical of osteoid osteoma and to locate precisely the site of the lesion.
Juxta- and intraarticular osteoid osteoma, however, are difficult to distinguish from chronic osteomyelitic lesion, and in this patient, the use of Technetium-99m bone scan is recommended [3]. A photopenic area of an osteomyelitic lesion on Technetium-99m bone scan corresponding to the plain radiograph lucency represents an avascular focus of purulent material, while osteoid osteoma in the early stages may appear as a “hot spot”. MRI scan is not necessary for diagnosis of osteoid osteoma, and may be sometimes misleading due to its over-estimation of the bone pathology. However, in juxta- and intraarticular osteoid osteomas, it helps to identify co-existed synovial proliferation and joint effusion [1, 3].
Conservative treatment of symptomatic osteoid osteomas with salicylates is seldom successful, is time consuming and has possible side effects (e.g., gastric ulcers) [1]. Pain caused by osteoid osteoma usually promptly subsides after complete removal of the nidus. For a more accurate identification of the nidus during open surgery, further, less invasive percutaneous ablative proceedings under CT guidance have been developed [1, 10, 11]. Arthroscopic excision of intraarticular osteoid osteoma was first reported in the knee [12]. The technique has also been used for the excision of juxta- and intraarticular osteoid osteomas in the ankles, hips and shoulder. Franceschi et al. reported on an arthroscopy-assisted en block antegrade resection in a case of intra-articular osteoid osteoma of the elbow [13].
To the authors’ knowledge, this is the first report on the arthroscopic removal of juxtaarticular osteoid osteoma of the humeral capitulum. The results are comparable to those reported for the other joints. The technique affords faster rehabilitation and minimized risk of neurovascular injury or postoperative infection compared to the open excisions. Yet, we would recommend the use of a less aggressive instrument than a motorized shaver because it causes tissue fragmentation and thereby impedes the histopathologic evaluation.
References
Dorfman HD, Czerniak B (1998) Benign osteoblastic tumors. In: Dorfman HD, Czerniak B (eds) Bone tumors. Mosby, St Louis, pp 85–127
Eideken J, De Palma AF, Hodes PJ (1966) Osteoid osteoma. Clin Orthop 49:201–206
Helms CA (2005) Miscellaneous conditions. In: Helms CA (ed) Fundamentals of skeletal radiology. Elsevier, Philadelphia, pp 155–165
Brabants K, Geens S, van Damme B (1986) Subperiosteal juxtaarticular osteoid osteoma. J Bone Joint Surg (Br) 68B:320–324
Mullin DM, Rodan BA, Bean WJ, Sehayik S, Sehayik R (1986) Osteoid osteoma in unusual locations: detection and diagnosis. South Med J 79:1299–1301
Kenzora JE, Abrams RC (1981) Problems encountered in the diagnosis and treatment of osteoid osteoma of the talus. Foot Ankle 2:172–178
Takaoka K, Yoshikawa H, Masuhara K, Sugano N, Ono K (1994) Ectopic ossification associated with osteoid osteoma in the acetabulum: a case report. Clin Orthop Relat Res 299:209–211
Alani WO, Bartal E (1987) Osteoid osteoma of the femoral neck stimulating an inflammatory synovitis. Clin Orthop Relat Res 223:308–312
Giustra PE, Freiberger RH (1970) Severe growth disturbance with osteoid osteoma. A report of two cases involving the femoral neck. Radiology 96:285–288
De Berg JC, Pattynama PM, Obermann WR, Bode PJ, Vielvoye GJ, Taminiau AH (1995) Percutaneous computed-tomography-guided thermocoagulation for osteoid osteomas. Lancet 346:350–351
Gangi A, Dietemann JL, Gasser B, Mortazavi R, Brunner P, Mourou MY, Dosch JC, Durckel J, Marescaux J, Roy C (1997) Interstitial laser photocoagulation of osteoid osteomas with use of CT guidance. Radiology 203:843–848
Heuijerjans W, Dandy DJ, Harris D (1986) Arthroscopic excision of an intra-articular osteoid osteoma at the knee. Arthroscopy 2:172–178
Franceschi F, Marinozzi A, Papalia R, Longo UG, Gualdi G, Denaro E (2006) Intra- and juxta-articular osteoid osteoma: a diagnostic challenge: misdiagnosis and successful treatment: a report of four cases. Arch Orthop Trauma Surg 126:660–667
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zupanc, O., Šarabon, N. & Stražar, K. Arthroscopic removal of juxtaarticular osteoid osteoma of the elbow. Knee Surg Sports Traumatol Arthr 15, 1240–1243 (2007). https://doi.org/10.1007/s00167-007-0376-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-007-0376-y