Abstract
Purpose
One of the key factors responsible for altered kinematics and joint stability following contemporary total knee arthroplasty (TKA) is resection of the anterior cruciate ligament (ACL). However, ACL retention can present several technical challenges, and in some cases may not be viable due to an absent or nonfunctional ACL. Therefore, the goal of this research was to investigate whether substitution of the ACL through an anterior post mechanism could improve kinematic deficits of contemporary posterior cruciate ligament (PCL) retaining implants.
Methods
Kinematic analysis of different implant types was done using KneeSIM, a previously established dynamic simulation tool. Walking, stair-ascent, chair-sit, and deep knee bend were simulated for an ACL-substituting (PCL-retaining) design, a bi-cruciate-retaining and ACL-sacrificing (PCL-retaining) implant, as well as the native knee. The motion of the femoral condyles relative to the tibia was recorded for kinematic comparisons.
Results
The ACL-substituting and ACL-retaining implants provided similar kinematic improvements over the ACL-sacrificing implant, by reducing posterior femoral shift in extension and preventing paradoxical anterior sliding. During all simulated activities, the ACL-sacrificing implant showed between 7 and 8 mm of posterior shift in extension in contrast to the ACL-retaining implant and the ACL-substituting design, which showed overall kinematic trends similar to the native knee.
Conclusion
The absence of ACL function has been linked to abnormal kinematics and joint stability in patients with contemporary TKA. ACL-substituting implants could be a valuable treatment option capable of overcoming the limitations of contemporary TKA, particularly when retaining the native ACL is not feasible or is challenging.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
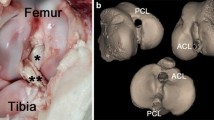
In the native knee, anteroposterior stability is granted by the anterior cruciate ligament (ACL), primarily in early flexion and in conjunction with the posterior cruciate ligament (PCL) throughout knee motion. The ACL contributes to the so-called screw-home mechanism that is associated with anterior location of the femur on the tibia near full extension, while the PCL drives posterior femoral rollback in high flexion [2, 7, 32, 33]. Hence, in the native knee, both ACL and PCL play a major role in joint stability and kinematics.
Current efforts to restore native knee function following total knee arthroplasty (TKA) aim to retain both ACL and PCL through the use of bi-cruciate-retaining (BCR) implants or bi-unicompartmental procedures. In vivo, in vitro (cadaver), and computational studies have shown that ACL preservation provides more normal kinematics than contemporary ACL-sacrificing TKA [10, 19, 23, 35, 43].
Several studies investigating TKA implants found the tibiofemoral contact to be shifted to the posterior portion of the tibia when the ACL was not present [9, 34, 42]. This is in contrast to studies investigating ACL-retaining implants [35, 36]. In functional outcome studies, TKA patients with contemporary ACL-sacrificing implants have reported abnormal feeling knees after joint replacement, which may be linked to these kinematic impairments [8, 25].
However, in spite of potential benefits of ACL retention, ACL-retaining total knee arthroplasty is currently not part of standard TKA practice. This is due to perceived technical difficulties in retaining and balancing both ACL and PCL, lack of availability of such implants, and clinical contraindications including the absence of a functional ACL at surgery. Patients undergoing TKA often present with an absent or nonfunctional ACL at the time of surgery due to the progression of arthritis or due to prior trauma. Incidence of a functional ACL at the time of TKA surgery is reported to range from 25 to 86% of the patients [13, 15]. Concerns have also been raised about the tibial baseplate design changes required to accommodate the ACL, specifically reduction in surface available for implant fixation and the strength of the tibial baseplate [26, 29]. Further, these designs create a tibial bone island around the ACL attachment, which could fracture [20], particularly in the presence of osteoporotic bone or due to improper ligament balancing resulting in increased ACL tension [28].
The hypothesis of this study was that an ACL-substituting tibial implant designed with an anterior post mechanism to replace the ACL function while allowing retention of the PCL (ASCR: ACL-substituting, cruciate (PCL)-retaining) could improve the kinematics of contemporary cruciate-retaining (CR) designs. The primary purpose of such an ACL-substituting implant would be to locate the femur anteriorly in extension like in native knees, while allowing the PCL to guide knee motion at higher flexion angles. An implant incorporating this new concept of an ACL-substituting post that also allows for PCL retention may be of significant clinical value. Such an implant may satisfy surgeons desire to improve kinematic abnormalities of CR implants, without the challenges posed by attempting to retain the native ACL.
Materials and methods
This hypothesis was tested by using dynamic computational simulations performed in KneeSIM software (LifeModeler, San Clemente, CA) to evaluate kinematics of implant designs that either retain (BCR), substitute (ASCR), or sacrifice the ACL (CR) in comparison with the native knee simulation.
KneeSIM is a previously validated software tool that mimics an oxford-type physical test set-up (Fig. 1) commonly used to test/analyse kinematics of knee implant designs in cadaver specimens [27]. This software tool uses rigid body dynamics coupled with elastic foundation contact modelling to simulate knee mechanics and has been used by several researchers to analyse kinematics of different knee implant designs, effect of variation in component positioning, etc. [6, 24, 37, 43]. In particular, Patil et al. validated their computational model within KneeSIM using experimentally measured kinematic and kinetic data, and found major trends plotted as function of knee flexion angle to be similar between the computational and experimental results [6]. Magnetic resonance imaging (MRI) data from a previous IRB-approved study (2003P000337) was used to create average bone and cartilage models of tibia, femur, and patella, and identify average insertion locations for medial/lateral collateral ligaments (MCL/LCL), cruciate ligaments (ACL/PCL), and the patellar tendon [43]. The quadriceps angle was determined to be 14.0° based on the average literature values [1, 18] and the proximal quadriceps insertion was chosen accordingly.
The kinematics of an ACL-substituting implant (ASCR) was compared to that of the same tibial articular surface without a post but with an intact ACL (BCR). This allowed for a direct comparison of the kinematic function of the ACL-substituting post, and the modelled ACL, for a given femoral and tibial articular surface design (identical for all tested implants). The ACL-substituting design tested in this study included an anterior tibial post that substitutes for the native ACL by interacting with the anterior portion of the femoral intercondylar notch. This concept of replacing the native ACL function is analogous to the concept of replacing PCL function in posterior stabilized (PS) implants using a post–cam interaction. The ACL-substituting post is also designed to accommodate the intact PCL (Fig. 2).
Kinematics of the ASCR implant were also compared to the ACL-sacrificing CR implant that consisted of the same articular surface but without an ACL or ACL-substituting post. Additionally, simulations were performed for the average native knee using the average articular cartilage geometry (femur tibia and patella) derived from MRI data (the “native knee”). The native knee model included ACL and PCL. Figure 3 shows a model and cross sections of all the implants and the native knee tested in this study. In the Appendix, there is a further comparison of the ASCR design to a commercially available BCR and CR implant.
Several activities were simulated to capture activities of daily living involving different ranges of knee motion (ROM): walking (60° flexion), stair-ascent (90° flexion), sitting on a chair (105° flexion), and deep knee bend (DKB, 135° flexion). These simulations were carried out with ideal (normative) component placements. The components were mounted perpendicular to the mechanical axis on the average bone models to restore the joint line on the lateral side according to standard surgical technique. The tibial posterior slope was 7.0° for all implants.
Ligaments were modelled as nonlinear, tension-only springs, with average stiffness values obtained from the literature (Table 1), [21, 30, 41]. An initial preload was applied to the collateral ligaments to simulate a balanced knee joint during surgery. The ACL was modelled with initial tension at full extension, while the PCL was modelled to be slack at the starting position (Table 1), [5, 16]. For a given knee flexion, the knee joint was free to move in all other degrees of freedom (internal/external and varus/valgus rotation as well as all translations), and no forces were imposed on the level of the knee joint for any activity. Tibiofemoral contact forces and knee kinematics are interdependent, and are in turn driven by implant geometry, implant placement, soft-tissue properties, and quadriceps muscle forces. Within KneeSIM, different combinations of built-in loading conditions are available to simulate a variety of activities, with the muscle loads being automatically modulated to balance forces applied to the hip/ankle joint centre. For deep knee bend, a constant load of 180.0 N was applied to the hip joint centre, while for chair-sit the same constant load at the hip joint was applied in conjunction with a varying anteroposterior (AP) load at the ankle joint. For stair-ascent, a variable vertical hip load was applied, with a peak force of 670.0 N. For walking simulation, a variable vertical hip load with a peak of 1100.0 N, together with a variable ankle torque around the tibia and an adduction/abduction moment, was applied.
For all simulations, tibiofemoral kinematics were reported as the average of medial and lateral femoral condyle motions relative to the tibia. The posterior femoral shift in extension, defined as shift of the midpoint between the medial and lateral condyle centres relative to KneeSIM’s built-in local tibial coordinate system, was of particular interest for the purpose of this study. Furthermore, the range of knee flexion angles where ACL and PCL were under tension, and range of knee flexion angles where there was contact between the femoral component and the ACL-substituting post were also reported.
Results
Walking Simulation
During walking, the results for the CR implant revealed notable posterior femoral shift in extension (Fig. 4) relative to the native knee (4.9 mm), and predominantly anterior femoral motion with increasing knee flexion (6.2 mm). Neither the ACL-retaining nor ACL-substituting implants showed this posterior femoral shift in extension relative to the native knee during the gait cycle (Table 2). Both ACL-retaining and ACL-substituting implants showed more similar motion trends compared to the native knee than the ACL-sacrificing implant. During walking simulations, the ASCR post was engaged with the intercondylar notch of the femoral component throughout the stance phase of gait (effective flexion range over which the “ACL substitute” was functional), which was similar to the portion over which the ACL was under tension in the BCR simulation and the native knee (Table 3).
Stair-ascent simulation
For the stair-ascent simulation, the CR implant data again showed posterior femoral shift in extension relative to the native knee (5.6 mm) followed by paradoxical anterior sliding. In contrast to ASCR and both BCR implant and native knee that showed posterior femoral rollback, the CR implant had a more anterior location (1.6 mm) of the femur on the tibia at 90° flexion compared to full extension (Table 2).
Chair-sit simulation
The ASCR implant again showed motion similar to the BCR with net posterior femoral rollback of 5.0 mm for ASCR and 6.6 mm for BCR, respectively. The CR data for chair-sit again showed substantial posterior femoral shift in extension relative to the native knee (6.2 mm, Fig. 4), followed by anterior femoral sliding of 4.5 mm until 60° before rollback occurred with higher knee flexion (Table 2).
Deep knee bend simulation
During deep knee bend, the whole range of knee flexion was covered, and the comparison of all implants and the native knee is shown in detail in Fig. 5. Like for all the other simulated activities in low flexion (<30°), the ASCR tibial post-femoral notch interaction provided a similar kinematic effect to that of the retained ACL in the BCR simulation unlike the CR simulation. At higher flexion angles when there was no contribution from either the tibial post in ASCR or the ACL in the BCR implant, the kinematics for all designs were virtually identical. The simulations for the native knee showed very similar trends in low flexion until around 30° knee flexion. With further knee flexion, the native knee showed more femoral rollback than any of the implants (Fig. 5, Table 2).
Table 3 shows the range of knee flexion angles where the tibial post was in contact with the femoral component in the ASCR implant, and where the ACL/PCL were under tension in the BCR/CR implants and the native knee.
Discussion
The most important finding of the present study was that within the simulation environment, the kinematic function of the ACL in low knee flexion was successfully replicated by ACL substitution involving engagement of a tibial post with the femoral component. The anterior substituting cruciate-retaining (ASCR) design showed kinematics close to that of the BCR design, which had the same articular surface geometry as the ASCR design. Thus, like the BCR design, the ASCR implant was able to improve the kinematic abnormalities of the CR implants across the simulated activities in this study (Figs. 4, 5; Table 2). In all activities, the CR implant showed substantial posterior femoral shift in extension (Fig. 4) followed by paradoxical anterior sliding. These findings for the CR implant are consistent with various in vivo, in vitro (cadaver), and simulation studies [23, 34, 39, 42, 43]. Further, we have also compared kinematics of the ASCR design to a commercial BCR and CR device in the appendix. This confirmed the original hypothesis of this study.
The abnormal posterior femoral location in CR implants is largely due to the missing ACL, which is under tension in extension and holds the femur anteriorly on the tibia (Fig. 6). Following this posterior shift, the force imbalance within the joint causes paradoxical anterior sliding of the femur in early flexion. As explained by Blaha, the line of action of the body weight in early flexion lies behind the knee joint. This is balanced by quadriceps activation, and the absence of the ACL and slack state of the PCL in early flexion causes anterior femoral sliding [4]. To reduce such paradoxical anterior sliding, contemporary TKA implants often utilize increased anterior tibial lips, which also cause the femur to sit posteriorly on the tibia in extension. With increased flexion, a reduced tibiofemoral constraint allows additional laxity, and paradoxical anterior sliding occurs until the PCL is adequately tensioned in mid-flexion to guide femoral posterior rollback.
In contemporary CR TKA, the ACL is resected and its function is lost, which alters native knee kinematics following TKA surgery [23, 35, 43]. ACL retention is one way to overcome these kinematic abnormalities but presents several challenges as previously discussed. Therefore, the goal of this study was to determine whether the kinematic abnormalities of CR implants could be improved by substituting for the resected ACL. This is achieved by the interaction of a tibial post with the intercondylar notch of the femoral component at low flexion angles to provide anteroposterior stability similar to that provided by the ACL in the native knee (Fig. 6), [33]. Further, the ACL-substituting tibial post is intended to work in conjunction with the native PCL. At higher flexion angles, the ACL post is designed to disengage from the femoral component and allow motion/stability to be governed by the native PCL.
Liu et al. [17] proposed ACL reconstruction following TKA as a different way to improve kinematics in CR implants based on the results of their computational simulations. Other attempts to provide improved knee kinematics through implant design include a bi-cruciate substituting (BCS) device with an anterior and posterior cam–post interaction (Smith and Nephew, London, UK). Publications related to this design have shown kinematic improvements over contemporary PS implants where both ACL and PCL are resected. While the kinematics of this implant has been compared to other contemporary devices and native knees, the effectiveness of the ACL- and PCL-substituting mechanism relative to the actual ligaments has not been directly evaluated [24, 38]. Another commercially available design uses a ball-and-socket-like joint on the medial side to provide AP stability while allowing greater AP motion on the less constrained lateral side also intends to improve joint stability and kinematics (Wright Medical Group, Arlington, TN, USA). Generally, these medially constrained designs are indicated for PCL-sacrificing applications, and use articular surface constraint instead of a post–cam mechanism to substitute for ligament function. Some publications have even debated whether PCL function either through retention (CR) or through substitution (PS) is necessary [31]. Nonetheless, CR and PS both are established and successful treatment options. Our research aimed to analyse the effect of direct substitution for the ACL with an ACL post while leaving the PCL intact providing an improved alternative to contemporary CR implants.
There are several limitations to the present study: The first limitation is that the kinematics evaluated in this study are based on the simulations of an average knee model in KneeSIM. The extent to which kinematics of an individual knee can be replicated by an ACL-substituting post designed for the average population is unclear. Therefore, subject-specific simulation studies should be conducted in future to evaluate inter-subject variations in knee kinematics for the different designs. The second limitation is that while the native knee simulations included geometry of the average articular cartilage, the simulation package did not allow for modelling of the menisci. However, the results for the native knee across different activities showed kinematic trends similar to published in vivo data of normal knees, particularly the activity depended range of AP translation showed very similar trends [12, 14, 22]. Another limitation of this study is although KneeSIM and other such computational tools have been used for design and evaluation of TKA implants, it is still uncertain whether such tools can fully predict kinematic behaviour of knees in vivo. Therefore, continued analysis of this concept via cadaver testing, more advanced full-body musculoskeletal simulations, and eventually in vivo kinematic evaluation is required. Another limitation of this study is also that the effect of articular geometry on implant kinematics was not evaluated. This was because we wanted to achieve a direct comparison of ACL substitution versus ACL retention and ACL sacrifice, without the confounding effect of articular surface variation. Prior studies have shown important effect of articular geometry on kinematics of BCR and CR implants [40, 43]. Therefore, future studies relating to the ASCR should evaluate the effect of changes in articular geometry coupled with the presence and absence of the ACL-substituting post.
The results of the present study suggest that the ASCR post can substitute for kinematic function of the ACL and provide a more natural location of the femur on the tibia. However, proprioception provided by the ACL would still be lost, which may have important implications for joint function [3, 11]. This may be a possible limitation of the ACL substitution concept.
While TKA procedures provide excellent pain relief, a significant portion of patients remain dissatisfied due to functional limitations, residual symptoms, and perception of joint instability [8, 25]. ACL has long been recognized as a missing puzzle in the quest for addressing these clinical challenges. However, retention of native ACL in TKA poses many challenges, and may also necessitate the use of advanced tools to obtain reliable outcomes. The proposed concept of ACL substitution may be an alternative to ACL retention, particularly for patients with an absent or nonfunctional ACL. If the kinematic improvements seen here are replicated in vivo, improved patient outcomes could be achieved with such ACL-substituting designs compared to contemporary CR implants. This would allow surgeons to provide better outcomes for their patients, without encountering challenges of ACL retention.
Conclusion
In conclusion, an ACL-substituting design that retains the native PCL showed important kinematic improvements over a CR TKA during dynamic simulations. Particularly, the abnormal posterior femoral shift and paradoxical anterior sliding in low knee flexion seen with the CR implants were addressed with the ASCR design through replacement of the native ACL by an ACL-substituting post. The kinematic results of the ASCR design were similar to an ACL-retaining implant and the native knee.
References
Aglietti P, Insall JN, Cerulli G (1983) Patellar pain and incongruence. I: measurements of incongruence. Clin Orthop Relat Res 176(176):217–224
Amis AA, Bull AM, Gupte CM, Hijazi I, Race A, Robinson JR (2003) Biomechanics of the PCL and related structures: posterolateral, posteromedial and meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc 11(5):271–281
Barrack RL, Skinner HB, Buckley SL (1989) Proprioception in the anterior cruciate deficient knee. Am J Sports Med 17(1):1–6
Blaha JD (2004) The rationale for a total knee implant that confers anteroposterior stability throughout range of motion. J Arthroplasty 19(4 Suppl 1):22–26
Blankevoort L, Huiskes R, de Lange A (1991) Recruitment of knee joint ligaments. J Biomech Eng 113(1):94–103
Colwell CW Jr, Chen PC, D’Lima D (2011) Extensor malalignment arising from femoral component malrotation in knee arthroplasty: effect of rotating-bearing. Clin Biomech 26(1):52–57
Conditt MA, Noble PC, Bertolusso R, Woody J, Parsley BS (2004) The PCL significantly affects the functional outcome of total knee arthroplasty. J Arthroplasty 19(7):107–112
de Beer J, Petruccelli D, Adili A, Piccirillo L, Wismer D, Winemaker M (2012) Patient perspective survey of total hip vs total knee arthroplasty surgery. J Arthroplasty 27(6):865–869
Dennis DA, Komistek RD, Mahfouz MR (2003) In vivo fluoroscopic analysis of fixed-bearing total knee replacements. Clin Orthop Relat Res 410:114–130
Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A (2004) A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res 428:180–189
Godinho P, Nicoliche E, Cossich V, de Sousa EB, Velasques B, Salles JI (2014) Proprioceptive deficit in patients with complete tearing of the anterior cruciate ligament. Rev Bras Ortop 49(6):613–618
Johal P, Williams A, Wragg P, Hunt D, Gedroyc W (2005) Tibio-femoral movement in the living knee. A study of weight bearing and non-weight bearing knee kinematics using ‘interventional’ MRI. J Biomech 38(2):269–276
Johnson AJ, Howell SM, Costa CR, Mont MA (2013) The ACL in the arthritic knee: how often is it present and can preoperative tests predict its presence? Clin Orthop Relat Res 471(1):181–188
Komistek RD, Dennis DA, Mahfouz M (2003) In vivo fluoroscopic analysis of the normal human knee. Clin Orthop Relat Res 410:69–81
Lee GC, Cushner FD, Vigoritta V, Scuderi GR, Insall JN, Scott WN (2005) Evaluation of the anterior cruciate ligament integrity and degenerative arthritic patterns in patients undergoing total knee arthroplasty. J Arthroplasty 20(1):59–65
Li G, Gil J, Kanamori A, Woo SL (1999) A validated three-dimensional computational model of a human knee joint. J Biomech Eng 121(6):657–662
Liu HW, Ni M, Zhang GQ, Li X, Chen H, Zhang Q, Chai W, Zhou YG, Chen JY, Liu YL, Cheng CK, Wang Y (2016) Kinematic analysis of anterior cruciate ligament reconstruction in total knee arthroplasty. Am J Transl Res 8(5):2275–2283
Livingston LA (1998) The quadriceps angle: a review of the literature. J Orthop Sports Phys Ther 28(2):105–109
Lo J, Muller O, Dilger T, Wulker N, Wunschel M (2011) Translational and rotational knee joint stability in anterior and posterior cruciate-retaining knee arthroplasty. Knee 18(6):491–495
Lombardi AV (2015) The bi-cruciate retaining TKA: “a thing of beauty is a joy forever”—affirms. Bone Joint J 97(1):69
Momersteeg TJ, Blankevoort L, Huiskes R, Kooloos JG, Kauer JM, Hendriks JC (1995) The effect of variable relative insertion orientation of human knee bone-ligament-bone complexes on the tensile stiffness. J Biomech 28(6):745–752
Moro-oka TA, Hamai S, Miura H, Shimoto T, Higaki H, Fregly BJ, Iwamoto Y, Banks SA (2008) Dynamic activity dependence of in vivo normal knee kinematics. J Orthop Res 26(4):428–434
Moro-oka TA, Muenchinger M, Canciani JP, Banks SA (2007) Comparing in vivo kinematics of anterior cruciate-retaining and posterior cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 15(1):93–99
Morra EA, Rosca M, Greenwald JF, Greenwald AS (2008) The influence of contemporary knee design on high flexion: a kinematic comparison with the normal knee. J Bone Joint Surg Am 90(Suppl 4):195–201
Noble PC, Gordon MJ, Weiss JM, Reddix RN, Conditt MA, Mathis KB (2005) Does total knee replacement restore normal knee function? Clin Orthop Relat Res 431:157–165
Nowakowski AM, Stangel M, Grupp TM, Valderrabano V (2013) Comparison of the primary stability of different tibial baseplate concepts to retain both cruciate ligaments during total knee arthroplasty. Clin Biomech 28(8):910–915
Patil S, Colwell CW Jr, Ezzet KA, D’Lima DD (2005) Can normal knee kinematics be restored with unicompartmental knee replacement? J Bone Joint Surg Am 87(2):332–338
Pritchett JW (2015) Bicruciate-retaining total knee replacement provides satisfactory function and implant survivorship at 23 years. Clin Orthop Relat Res 473(7):2327–2333
Ranawat CS (2015) The bi-cruciate retaining TKA: “A THING of beauty is a joy forever”—opposes. In: The Combined Services Orthopaedic Society (CSOS), Newcastle, UK. Bone Joint J 97(1):70
Robinson JR, Bull AM, Amis AA (2005) Structural properties of the medial collateral ligament complex of the human knee. J Biomech 38(5):1067–1074
Roh Y, Jang J, Choi W, Lee J, Chun S, Lee S, Seong S, Lee M (2013) Preservation of the posterior cruciate ligament is not helpful in highly conforming mobile-bearing total knee arthroplasty: a randomized controlled study. Knee Surg Sports Traumatol Arthrosc 21(12):2850–2859
Rong GW, Wang YC (1987) The role of cruciate ligaments in maintaining knee joint stability. Clin Orthop Relat Res Feb 215:65–71
Shelburne KB, Pandy MG, Anderson FC, Torry MR (2004) Pattern of anterior cruciate ligament force in normal walking. J Biomech 37(6):797–805
Siston RA, Giori NJ, Goodman SB, Delp SL (2006) Intraoperative passive kinematics of osteoarthritic knees before and after total knee arthroplasty. J Orthop Res 24(8):1607–1614
Stiehl JB, Komistek RD, Cloutier JM, Dennis DA (2000) The cruciate ligaments in total knee arthroplasty: a kinematic analysis of 2 total knee arthroplasties. J Arthroplast 15(5):545–550
Suggs JF, Li G, Park SE, Steffensmeier S, Rubash HE, Freiberg AA (2004) Function of the anterior cruciate ligament after unicompartmental knee arthroplasty: an in vitro robotic study. J Arthroplast 19(2):224–229
Tanaka Y, Nakamura S, Kuriyama S, Ito H, Furu M, Komistek RD, Matsuda S (2016) How exactly can computer simulation predict the kinematics and contactstatus after TKA? Examination in individualized models. Clin Biomech 39:65–70
van Duren BH, Pandit H, Price M, Tilley S, Gill HS, Murray DW, Thomas NP (2012) Bicruciate substituting total knee replacement: how effective are the added kinematic constraints in vivo? Knee Surg Sports Traumatol Arthrosc 20:2002–2010
Varadarajan KM, Harry RE, Johnson T, Li G (2009) Can in vitro systems capture the characteristic differences between the flexion-extension kinematics of the healthy and TKA knee? Med Eng Phys 31(8):899–906
Varadarajan KM, Zumbrunn T, Rubash HE, Malchau H, Li G, Muratoglu OK (2015) Cruciate retaining implant with biomimetic articular surface to reproduce activity dependent kinematics of the normal knee. J Arthroplasty 30(12):2149–2153
Woo SL, Hollis JM, Adams DJ, Lyon RM, Takai S (1991) Tensile properties of the human femur-anterior cruciate ligament-tibia complex. The effects of specimen age and orientation. Am J Sports Med 19(3):217–225
Yue B, Varadarajan KM, Moynihan AL, Liu F, Rubash HE, Li G (2011) Kinematics of medial osteoarthritic knees before and after posterior cruciate ligament retaining total knee arthroplasty. J Orthop Res 29(1):40–46
Zumbrunn T, Varadarajan KM, Rubash HE, Malchau H, Li G, Muratoglu OK (2015) Regaining native knee kinematics following joint arthroplasty: a novel biomimetic design with ACL and PCL preservation. J Arthroplasty 30(12):2143–2148
Acknowledgements
The work reported herein was supported by departmental grants at Massachusetts general Hospital. The authors would also like to thank Rajan Patel for technical assistance with various aspects of the analysis.
Author’s contribution
All authors contributed to the implant concept described herein, and the study design. Authors TZ, MPD, and KMV conducted the implant design and simulation work. Authors HER and HM gave clinical inputs and assisted with cadaver surgeries. Author OKM gave advice regarding material strength and testing of the implant design. Authors TZ and KMV wrote the manuscript, and all authors read and provided feedback on various aspects of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
One or more co-authors are listed inventors on a patent application related to the technology analysed as part of this research.
Funding
This study was funded in part by departmental research grant.
Ethical approval
Although this study did not involve human participants, it made use of data collected from past studies involving human subjects. All such past studies were in accordance with the ethical standards of the institutional and/or national research committee, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Although this study did not involve human participants, it made use of data collected from past studies involving human subjects. Informed consent was obtained from all individual participants included in these prior studies.
Appendix
Appendix
Methods
Further implants were tested by using dynamic computational simulations performed in KneeSIM software (LifeModeler, San Clemente, CA) to evaluate kinematics of the ACL-substituting design (ASCR) against commercially available implants.
Therefore, kinematics of the ASCR implant were also compared to that of a widely used contemporary ACL-sacrificing CR TKA (NexGen CR, Zimmer, Warsaw, IN), and an existing ACL-retaining implant (TKO BCR, Biopro, Port Huron, MI). The implant geometries and sagittal cross sections are shown in Fig. 7, and the same activities were simulated.
The simulations were also carried out with ideal (normative) component placements, mounted perpendicular to the mechanical axis on the average bone models with a tibial posterior slope of 7°. The same tibiofemoral kinematic parameters were analysed for a direct comparison to the ASCR implant and the native knee with a particular interest in posterior femoral shift in extension relative to KneeSIM’s built-in local tibial coordinate system.
Results
The results for the NexGen CR implant revealed notable posterior femoral shift in extension relative to the native knee for all simulated activities (7–10 mm), which was the most of all tested implants (Fig. 8). The TKO BCR implant did not show this posterior femoral shift in extension relative to the native knee, which is in line with the ASCR and BCR implants analysed in this study. Overall, the NexGen CR implant showed similar abnormalities to the tested CR implant in this study, including posterior femoral shift in extension followed by paradoxical anterior sliding. The femur only moved posterior on the tibia with deeper knee flexion, and no overall femoral rollback was observed in any activity. The TKO BCR showed results more closely resembling the native knee as well as the ACL-substituting and ACL-retaining implants of this study. Particularly, there was no excessive posterior femoral shift in extension; however, reduced femoral rollback was observed compared to the implants evaluated in this study and the native knee (Table 4).
Rights and permissions
About this article
Cite this article
Zumbrunn, T., Duffy, M.P., Rubash, H.E. et al. ACL substitution may improve kinematics of PCL-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26, 1445–1454 (2018). https://doi.org/10.1007/s00167-016-4372-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4372-y