Abstract
The reported functional results of rotator cuff repair performed arthroscopically have been good. Only little is known about the cuff integrity after arthroscopic repair and how it influences the outcome. The aim of the study is to set a baseline of what rate of healing response respectively re-tears to expect and how cuff integrity alters the outcome. Fifty-three consecutive patients with an isolated supraspinatus tendon tear were arthroscopically operated and their tendons repaired. All pre- and postoperative data were prospectively collected. At a minimum follow-up after 24 months (average 26.4 months), the integrity of the cuff was evaluated by an open magnetic resonance imaging and the patients’ function and satisfaction were documented and graded to the sex- and age-related Constant-score also using a dynamometer for strength testing. The re-tear rate was 24.5% with 13 non-healed tendons. The Constant-score of all patients improved significantly. The scores of the patients with a re-tear were significantly lower than those of the patient with an intact cuff. That was due to a less good performance in strength testing. The other categories of the Constant-score did not show any differences. The age of the patients with a re-tear was significantly higher. With the exception of age, we did not find any negative prognostic factor for a re-tear, and with the exception of re-tear no other factor influenced the Constant-score. Arthroscopic supraspinatus tendon repair yields a re-tear rate of 25% which is comparable with the results of open or mini/open repair. Cuff integrity influences postoperative strength and Constant-score. Patients older than 65 years show a higher re-tear rate. Therapeutic Level IV is the level of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ever since the introduction of the concept of rotator cuff tendon repair by Codman in 1934, techniques have been improved over the decades. Open and later on the so-called mini-open rotator cuff repair yielded good clinical results with a high percentage of subjective patients’ satisfaction [6, 8, 13, 32]. With the invention of magnetic resonance imaging (MRI) preoperative evaluation of the tendon, its retraction and grade of muscle atrophy could be determined, developing prognostic factors for operability and postoperative outcome. Furthermore, MRI provides a good tool for postoperative control whether the tendons have healed or not.
In the beginning 1990s of the last century, arthroscopy has been introduced to shoulder surgery, first for instability and later for rotator cuff repair.
So far many studies have been published showing good clinical results of arthroscopic rotator cuff repair (ARCR) [1, 4, 5, 10, 25, 30, 33] but only one has used ultrasound [9] and one MRI, respectively, CT scan [3] for postoperative control of tendon healing. Other studies using these modalities to prove healing of the repaired tendons deal with open or mini-open repairs. Liu and Baker [19] showed a 66% healing rate after mini-open repairs using arthrography and Harryman et al. [13] used ultrasound to show a 65% rate of intact tendons after open repairs. Gerber et al. [12] reported a 66% rate of cuff integrity after open repair of massive tears (defined as involvement of two tendons or more) and used MRI for control. Whether cuff integrity is a significant factor for better outcomes remains controversial. Overall, these studies still recommend attempting rotator cuff repair to achieve improvement in pain, function and even strength [15, 18] rather than just debriding the cuff.
The purpose of our study is twofold: first to establish a base-line of what rate of re-tear to expect after ARCRs and second to find out whether cuff integrity has an influence on clinical outcome.
Materials and methods
Patients and inclusion/exclusion criteria
In order to achieve our goals, we prospectively included 53 patients with an isolated full-thickness tear of the supraspinatus tendon with persistent pain and impairment. Patients presenting with tears involving the infraspinatus or the subscapularis tendon were excluded as well as patients with partial tears or partial repairs, a stiff shoulder, glenohumeral arthritis, upward migration of the head with an acromiohumeral distance of less than 5 mm and severe muscle atrophy or fatty infiltration. Biceps pathology was not an exclusion criterion. Patients showing rotator cuff tears preoperatively were asked to participate in the study. After written consent, the patients were operated and the tear size measured intraoperatively. Once involvement of subscapularis and/or infraspinatus were detected the patient was excluded.
Evaluation and assessment
Preoperative evaluation included X-rays (standard true a.p., axillary and outlet views), MRI and physical examination which were graded to the sex and age related Constant-score. Therefore, the results of the total score are per cent and not absolute points.
On preoperative MRI, the retraction of the tear was graded according to the system of Patte. Retraction stage I is when the tear edge is lateral to the articular cartilage (32 patients), stage II when the edge is between the lateral aspect of the cartilage and the apex of the head (19 patients), Stage III if the edge is medial of the apex to the glenoid (two patients) and stage IV if the tear edge is medial to the glenoid (no patient). Tears size was staged intraoperatively according to the system of Bateman with size I < 1 cm, size II 1–3 cm and size III 3–5 cm in diameter.
Surgery was performed by the first and the senior authors in a standardized matter. In all but one patient acromioplasty was performed and in 14 patients an additional resection of the lateral clavicle for symptomatic AC-joint arthritis had to be carried out. Biceps tenotomy/tenodesis for biceps pathology was done in 18 patients. 1–3 bioabsorbable double-loaded anchors were used to refix the tendon to the supraspinatus footprint where bleeding had been created for healing. A standard trough was not established. Single-row refixation was performed and a modified Mason-Allen stitch used [27]. Mobilization of the cuff was done as necessary performing it subacromially as well as intraarticularily.
There were 34 men and 19 women included in this study with a mean age of 60.9 years (range 46–74 years). Surgery was performed in 38 patients on the right shoulder and in 15 patients on the left, in 37 this was the dominant in 16 the non-dominant arm. Tear extension was size Bateman I in 9 patients, size II in 38 and size III in 6.
Postoperative management
The patients were in the hospital for three nights. The shoulders were immobilized for 3 weeks in an abduction pillow of 15° of abduction. Passive range of motion exercises were commenced the first day after surgery and limited to 60° of abduction and 30° of external rotation for 6 weeks. Active range of motion was begun once the shoulder had gained free forward elevation. Hydrotherapy was emphasized and strengthening exercises carried out for a minimum of four months.
Postoperative assessment
Postoperatively the patients were invited to a follow-up visit at 24 months after surgery, so that the minimum follow-up is 24 months and the average follow-up 26, 4 months.
At the follow-up a physical examination was performed as well as a strength testing using the ISOBEX dynamometer (Cursor AG, Bern, Switzerland) in a sitting position with the arm abducted to 90° in the plane of the scapula and internally rotated (empty can test position). The results again were graded to the sex and age-related Constant-score.
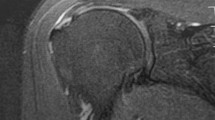
Then, a standardized open MRI (ESAOTE E-scan XQ, Esaote S.p.A, Genova, Italy) was done using a shoulder coil with paracoronal T1 weighted spin-echo sequences (TE 24, TR 770, SE 4.0), paracoronal T2-weighted turbo spin echo sequences (TR 3000, TE 80, SE 4.0), parasagittal T1-weighted spin echo sequences (TE 24, TR 770, SE 4.0) and transaxial T1-weighted spin echo sequences (TR 870, TE 24, SE 4.0). Since we believed that not all patients would agree to the application of contrast medium into the joint, we performed MRI without it.
Two examiners evaluated the MRI looking at tendon integrity. As soon as one of the examiners found that there was a re-tear the other examiner was overruled. Criteria for re-tear were lack of continuity of the tendon in one slice of the coronal plane. Very thin bands of tissue were also defined as failure of healing, assuming that this would not be a normal, but rather a thin tendon or even just fibrous tissue. We only differentiated between re-tear and intact tendon. Evaluation of muscle atrophy and fatty infiltration in the rotator cuff muscles was not performed in this study.
Statistical analysis
The analysis was carried out with the SPSS statistical software and Wilcoxon-signed-rank test was used for the analysis of the pre- and postoperative results and the Mann–Whitney U test for the comparison between the patients with intact or retorn tendons. Correlations were calculated according to Pearson. Statistical significance was reached with P < 0.05.
Results
The mean duration of symptoms prior to surgery was 11.7 months with a range between 1 and 72 months.
Functional results
The overall sex and age related Constant-score could significantly be improved from 53.4% (range 23–80%) to 84.3% (range 62.5–99.3%). The subcategories of the Constant-score could also be improved (see Fig. 1). The results were rated as excellent in 15 cases (29%), good in 27 cases (51%), satisfying in four cases (7%) and fair in seven cases (13%), with an excellent score from 91–100%, good 81–90%, satisfying 71–80%, fair 61–70% and poor < 60% [2].
Complications
We did not see any superficial or deep wound infections. Re-tears, as a possible complication, are described later. At follow-up examination no patient showed capsular tightness in terms of a frozen shoulder. Some patients reported that they did experience limitations of range of motion but theses limitation disappeared during physiotherapy.
Anatomic results
A re-tear of the rotator cuff was detected in 13 patients (24.5%). The total Constant-score of the patients with an intact cuff totalled to 86% whereas the score of the patients with a re-tear was 79%. The difference was statistically significant (P < 0.0095). Also the age of the re-tear group (65.3 years range 54–74) was significantly higher than that of the intact tendon group (59.5 range 46–73) (P < 0.012).
Pain, activities of daily living and range of motion showed no differences between the groups, but strength was less in the patients with a re-tear, 8.4 points versus 13.8 points equivalent to 4 versus 6.4 kg (P < 0.0043). The differences in strength were responsible for the differences in the total Constant-score, because strength testing adds up to 25% of the total possible value of the Constant-score. The different results concerning the patients with or without a re-tear are shown in Fig. 2 and Table 1.
Age and postoperative Constant-score comparing the patients with an intact tendon or with a re-tear. For significance, see Table 1. Age in years, total score in per cent, other categories in points
Interestingly when dividing the patients in different age groups, the re-tear rate is higher in older patients. Among the 11 patients younger than 55 there was one re-tear (9.1%), with 27 patients between 55 and 65 years the re-tear rate was 14.8% (4 re-tears), but out of 15 patients older than 65 years eight patients showed a re-tear (53.3%) (Fig. 3).
The size of the tear did not influence the chance to suffer a re-tear because the different tear sizes were equally distributed in both groups. There were 15% size Bateman I, 70% size II and 15% size III in the group of the re-tears, respectively, 17% size I, 73% size II and 10% size III in the intact group (P = 0.904 Kolmogorov–Smirnov Z test). Among the patients with a tear size I 77.8% of the tendons healed, with size II 76.3% and with size III 66.7% healed. The number of patients with size III was too low to establish statistical significances. The preoperative tear size did not show any correlation with the post-operative Constant-score (r = 0.0906; P = 0.5187).
The grade of retraction tends to influence the risk for re-tears with greater retraction to cause more re-tears (P = 0.077; Kolmogorov–Smirnov Z test), but this was not statistically significant. The pre-operative retraction did not show any correlation to the post-operative Constant-score (r = −0.2345; P = 0.09).
Biceps treatment and lateral clavicle resection did not influence the post-op Constant-score or the risk of having a re-tear (biceps treatment r = −0.0950; P = 0.4987; lateral clavicle resection r = 0.0563; P = 0.6888).
The patients’ subjective evaluation of their results did not differ, when they were asked if they would undergo the procedure again. No matter if they had a re-tear or not, all patients would undergo the procedure again.
Discussion
This is one of a few studies looking at cuff integrity after ARCR using a diagnostic tool such as ultrasound or MRI for control. Many studies have shown good clinical outcome for this kind of operation without any imaging control. The influence of muscle or tendon changes was not subject of this study. The results of this study demonstrate that a re-tear rate after ARCR of isolated supraspinatus tendon tears of 25% has to be expected by the surgeon and the patient and this has to be made clear to the patient in the preoperative planning. Furthermore, the results emphasize that if a re-tear occurs the strength will be less than that of the patients with intact tendons and that a re-tear is more probable in patients older than 65 years. The study also shows good and very satisfying results objectively and subjectively after ARCR.
The strength of our study is the prospective design and its clear-cut inclusion/exclusion criteria and that only two experienced surgeons performed surgery. The postoperative control used the same MRI in every patient at 2 years or more.
The weaknesses include the lack of a control group in which either an open/mini-open procedure was performed or a group in which only debridement/subacromial decompression was carried out. Nevertheless, the aim of our study was to find out what rate of re-tears to expect after ARCR and if cuff integrity influences the result.
Re-tear rate
Our re-tear rate is comparable with those studies using MRI or ultrasound for follow-up no matter if the repair was done open, mini-open or arthroscopically [3, 9, 16, 19]. Interestingly, we found a similar age-related increase of re-tears as Boileau et al. [3] did in their study. In their study 57% of patients older than 65 years had a re-tear, in our group this number was 53.3%. Our number of re-tears was lower than that of Gerber et al. [12] but they looked at tears involving at least two tendons whereas our lesions only involved the SSP.
Strength
The strength testing that is necessary for the Constant-score was performed in the accepted manner of a sitting position, the arm abducted to 90° in the plane of the scapula and the arm internally rotated (empty can test) with a dynamometer. The strength was significantly better in patients with a healed cuff and that is conforming to other studies as the ones of Boileau et al. [3] and Klepps et al. [18].
MRI
One can argue that MRI is not the optimal tool to control cuff integrity. First, no contrast medium was applied to control for watertight repairs or leakage into the tendon. Second, MRI is a static instrument and one cannot visualize the dynamic behaviour of the tendon under rotation and elevation. But patients could not be convinced to have an injection into their shoulder. Furthermore, one has to state that the diffuse signal increase in post-operative MRI may lead to overestimation of re-tears according to studies by Owen et al. [26], Spielmann et al. [29] and Motamedi et al. [24]. We believe that because of our very strict criteria for re-tears and the evaluation by two examiners the number of false-negative judgments would be low.
Surgical technique
Only in one patient an acromioplasty was not performed, because no signs of subacromial impingement were detected. Whether the decompression led to the observed pain relief or not cannot be concluded on the basis of our data. One has to assume that the subacromial decompression caused the major pain relief. On the other hand, Gartsman and O’Connor [11] in a prospective, randomized study concluded that arthroscopic subacromial decompression does not appear to change the functional outcome after arthroscopic repair of the rotator cuff. But their results were short term after 1 year. So in the long run, the role of repair versus decompression remains unclear.
The same is true for the numbers concerning resection of the lateral clavicle. The resection was only performed if patients had symptomatic AC-joint arthritis which was confirmed by local anaesthetics test preoperatively. Biceps pathology is also very common in patients with rotator cuff tears especially when the rotator interval is included in the process. The number of 18 biceps tenotomies/tenodesises reveals the fact that in isolated SSP tears the interval is more often intact than in tears including SSC and/or ISP. The influence of biceps treatment was yet not an issue of our study’s aim.
Some authors [3, 28] deal with the delamination of the tendon and consider it a factor for outcome. Boileau et al. [3] could clearly show that additional delamination of the subscapularis and/or the infraspinatus will lead to lower rates of tendon healing in arthroscopic supraspinatus repairs. On the other hand, Sonnabend and Watson [28] could not find any influence on patient satisfaction. We did not look at this problem in our study.
Other formerly stated factors such as tear size and location, weakness in abduction [7] and/or external rotation [14] did neither correlate with the postoperative result nor with the risk of a re-tear according to our data. So it seems that not the size, but rather the ability to mobilize and refix the tendon tension-free on a great contact area is more important for a good healing response as well the biological factors of strong bone and good vascularity. This is supported by the study of Mallon et al. [21] showing that smokers have less favourable results after rotator cuff repair than non-smokers.
Fixation of the tendon to the bone, suture configuration and anchor placement are still under debate. We always debrided the footprint only until bleeding was created and placed the anchor as far lateral as possible. Although Meyer et al. [23] propose to place the anchor subcortically or medial under the articular surface, because of osteopenia at the greater tuberosity, we did not find any complications of anchor loosening or dislocation in this series. A modified Mason-Allen stitch [27] consisting of a horizontal mattress and a vertical single suture was used. We believe with that technique good footprint area contact can be achieved and that it will reduce slippage out of the sutures and off the bony bed as demonstrated by Ma et al. [20] when they showed no significant elongation of the construct and the highest load-to-failure strength.
When we started and designed the study, ARCR was performed in a single-row fashion. This type of refixation was transformed from open technique in which it still is golden standard to use either transosseous suture techniques or if anchors are used a single row of anchors [16]. Contact area is found to be greater in double row technique as in vitro studies have suggested [22, 31]. Furthermore, fixation strength and stiffness is greater and gap formation smaller in a double-row repair [17]. Concerning contact pressure, the single-row technique scored better than double-row [31]. So far no clinical study has been published to show a difference in healing potential between single- or double-row repair and whether this will make a difference in the re-tear rate or the functional outcome in terms of the Constant or any other score.
Tendon healing is a multifactorial process and with the results of our study we cannot conclude what is the most important factor for healing, respectively, for re-tearing. But with the data available our study can be summarized as follows:
First, arthroscopic repair of supraspinatus tendon tears with subacromial decompression gives good clinical and subjective results at a minimum 2-year follow-up with significantly improved pain, range of motion, activities of daily living no matter if the tendon has healed or not. Second, with an intact cuff the results are significantly better in terms of strength. Third, with MRI control the described procedure will lead to a healing rate of 75%. Fourth, age is one factor that influences healing with a re-tear rate of 53% in patients over 65 years and therefore the indication for cuff repair in patients older than 65 years has to be done critically and individually. Fifth, arthroscopic repair of supraspinatus tendon tears will give comparable results as open or mini-open repairs and therefore can be recommended as a treatment of choice for this entity.
References
Bennett WF (2003) Arthroscopic repair of anterosuperior (supraspinaus/subscapularis) rotator cuff tears: a prospective cohort with 2- to 4-year follow-up: classification of biceps subluxation/instability. Arthroscopy 19:21–33
Boehm TD (2002) Scores. In: Gohlke F, Hedtmann A (eds) Orthopädie und Orthopädische Chirurgie: Schulter. Thieme, Stuttgart, New York, pp 98–104
Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG (2005) Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am 87-A:1229–1240
Burkhart SS (2001) Arthroscopic treatment of massive rotator cuff tears. Clin Orthop 390:107–118
Burkhart SS, Danaceau SM, Pearce CE Jr (2001) Arthroscopic rotator cuff repair: analysis of results by tear size and repair technique: margin convergence versus direct tendon-to-bone repair. Arthroscopy 17:905–912
Cofield RH, Parvizi J, Hoffmeyer PJ, Lanzer WL, Ilstrup DM, Rowland CM (2001) Surgical repair of chronic rotator cuff tears: a prospective long-term study. J Bone Joint Surg Am 83:71–77
Ellman H, Hanker G, Bayer M (1986) Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am 68:1136–1144
Galatz LM, Griggs LM, Cameron BD, Iannotti JP (2001) Prospective longitudinal analysis of postoperative shoulder function: a ten-year follow-up study of full-thickness rotator cuff tears. J Bone Joint Surg Am 83:1052–1056
Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K (2004) The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am 86-A:219–224
Gartsman GM (2001) Arthroscopic rotator cuff repair. Clin Orthop 390:95–106
Gartsman GM, O´Connor DP (2004) Arthroscopic rotator cuff repair with and without arthroscopic subacromial decompression: a prospective, randomized study of one-year outcomes. J Shoulder Elbow Surg 13:424–426
Gerber C, Fuchs B, Hodler J (2000) The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am 82:505–515
Harryman DT, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA III (1991) Repairs of the rotator cuff: correlation of functional results with integrity of the cuff. J Bone Joint Surg Am 73:982–989
Hawkins RJ, Misamore GW, Hobeika PE (1985) Surgery for full-thickness rotator cuff tears. J Bone Joint Surg Am 67:1349–1355
Jost B, Pfirrmann CW, Gerber C (2000) Clinical outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am 82:304–314
Kessler MA, Lichtenberg S, Habermeyer P (2003) Reconstruction of big rotator cuff ruptures. A new technique of tendon refixation with the corkscrew suture anchor system. Unfallchirurg 106:826–33
Kim DH, Elattrache NS, Tibone JE, Jun BJ, Delamora SN, Kvitne RS, Lee TQ (2005) Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med Nov 10 (Epub ahead of print)
Klepps S, Bishop J, Lin J, Cahon O, Strauss A, Hayes P, Flatow EL (2004) Prospective evaluation of the effect of rotator cuff integrity on the outcome of open rotator cuff repairs. Am J Sports Med 32:1716–1722
Liu SH, Baker CL (1994) Arthroscopically assisted rotator cuff repair: correlation of functional results with integrity of the cuff. Arthroscopy 10:54–60
Ma CB, MacGillivray JD, Clabeaux J, Lee S, Otis JC (2004) Biomechanical evaluation of arthroscopic rotator cuff stitches. J Bone Joint Surg Am 86:1211–1216
Mallon WJ, Misamore G, Snead DS, Denton P (2004) The impact of preoperativesmoking habits on the results of rotator cuff repair. J Shoulder Elbow Surg 13:129–132
Mazzocca AD, Millett PJ, Guanche CA, Santangelo SA, Arciero RA (2005) Arthroscopic single-row versus double-row suture anchor rotator cuff repair. Am J Sports Med 33:1861–1868
Meyer DC, Fucentese SF, Koller B, Gerber C (2004) Association of osteopenia of the humeral head with full-thickness rotator cuff tears. J Shoulder Elbow Surg 13:333–337
Motamedi AR, Urrea LH, Hancock RE, Hawkins RJ, Ho C (2002) Accuracy of magnetic resonance imaging in determining the presence and size of recurrent rotator cuff tears. J Shoulder Elbow Surg 11:6–10
Murray TF Jr, Lajtai G, Mileski RM, Snyder SJ (2002) Arthroscopic repair of medium to large full-thickness rotator cuff tears: outcome at 2- to6-year follow-up. J Shoulder Elbow Surg 11:19–24
Owen RS, Iannotti JP, Kneeland JB, Dalinka MK, Deren JA, Oleaga L (1993) Shoulder after surgery: MR imaging with surgical validation. Radiology 186:443–447
Scheibel MT, Habermeyer P (2003) A modified Mason-Allen technique for rotator cuff repair using suture anchors. Arthroscopy 19:330–333
Sonnabend DH, Watson EM (2002) Structural factors affecting the outcome of rotator cuff repair. J Shoulder Elbow Surg 11:212–218
Spielmann AL, Forster BB, Kokan P, Hawkins RJ, Janzen DL (1999) Shoulder after rotator cuff repair: MR imaging findings in asymptomatic individuals—initial experience. Radiology 213:705–708
Tauro JC (1998) Arthroscopic rotator cuff repair: analysis of technique and results at 2- and3-year follow-up. Arthroscopy 14:45–51
Tuoheti Y, Itoi E, Yamamoto N, Seki N, Abe H, Minagawa H, Okada K, Shimada Y (2005) Contact area, contact pressure, and pressure patterns of the tendon–bone interface after rotator cuff repair. Am J Sports Med 33:1869–1874
Watson Em, Sonnabend DH (2002) Outcome of rotator cuff repair. J Shoulder Elbow Surg 11:201–211
Wilson F, Hinvov V, Adams G (2002) Arthroscopic repair of full-thickness tears of the rotator cuff: 2- to 14-year follow-up. Arthroscopy 18:136–144
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lichtenberg, S., Liem, D., Magosch, P. et al. Influence of tendon healing after arthroscopic rotator cuff repair on clinical outcome using single-row Mason-Allen suture technique: a prospective, MRI controlled study. Knee Surg Sports Traumatol Arthrosc 14, 1200–1206 (2006). https://doi.org/10.1007/s00167-006-0132-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-006-0132-8