Abstract
Purpose
The purpose of this study was to look at the functional outcomes of arthroscopic repair of anterosuperior rotator cuff tears.
Methods
Sixty-one patients who underwent arthroscopic repair of anterosuperior cuff tears were retrospectively reviewed. At a minimum 6 months of follow-up, shoulder functional outcome scores including the Constant score (CS), simple shoulder test (SST) and visual analogic scale (VAS) were collected. Strength recovery for supraspinatus and subscapularis was investigated.
Results
All patients (mean age 59 ± 7) were available at a mean follow-up of 18 ± 7 months. The average CS improved from 30.8 ± 10.2 preoperatively to 76.5 ± 12.0 postoperatively, average SST from 2.6 ± 2.0 to 8.8 ± 2.9 and average VAS pain scale from 3.8 ± 1 to 0.5 ± 0.5 (p < 0.0001). Strength at belly-press and Jobe tests significantly improved (p < 0.0001). All patients with the exception of one were satisfied with the intervention.
Conclusions
Arthroscopic repair of anterosuperior rotator cuff tears provides a significant improvement in pain relief and shoulder function. Strength recovery is demonstrated in medium correlation with tendon healing.
Level of evidence
Level IV, therapeutic case series.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Subscapularis (SSC) lesions have been more frequently reported after the improvement arthroscopic techniques.
SSC lesions follow a trauma in 68 % of cases, while they are purely degenerative in 32 % of cases. Usual mechanism is forced external rotation or hyperextension [1]. Their incidence is around 30 %, with the majority being partial lesions [2]. For some authors, degenerative lesions may occur because of an anterosuperior impingement with the coracoid process and can be isolated or associated with other tendons tears [3–6]. However, in 90 % of cases a supraspinatus (SS) tear is associated [7]. This configures an anterosuperior rotator cuff tear, which is a tear involving both the SS and the SSC tendons, with or without the involvement of the biceps pulley [8]. Those account for 9.3–23.9 % of all rotator cuff tears [9]. The pathology of the long head of biceps is frequently associated, with instability being observed in 64 % of patients and rupture in 12 % [10]. Several studies described subscapularis lesions treatment, initially by open approach [10–12], and lately by means of arthroscopy [8, 13–17]. Although arthroscopic treatment is now well defined and most series report good outcomes [14, 16, 18–20], some authors still consider only partial lesions to be reparable [21].
The most recent series showed improved results after arthroscopic repair of isolated subscapularis [22, 23] or anterosuperior lesions [9, 24–27] at short- and long-term follow-up.
Aim of our multicentric study was to retrospectively evaluate the early clinical and structural results of the arthroscopic repair of anterosuperior lesions. The outcomes were evaluated in terms of functional results, strength recovery and tendon healing.
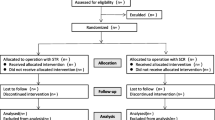
Materials and methods
The series
From February 2011 to February 2013, 1592 patients underwent arthroscopic treatment for painful shoulder in two different hospitals, the Cervesi Hospital of Cattolica (RN, Italy) and the ULSS 17 Hospital of Este (PD, Italy). In 1395 cases, arthroscopy revealed a cuff tear. SSC involvement was detected in 322 cases.
All patients had preoperative standard radiographs (in anteroposterior and lateral views) and MRI. SS tears were classified according to the Patte classification [28]. SSC tears were graded according to the Lafosse classification [19]. The fatty infiltration was graded according to the Fuchs classification [29].
Patients were enrolled according to the following inclusion criteria: (1) arthroscopic evidence of upper one-third part full-thickness tear of the subscapularis tendon (Lafosse type II), (2) evidence of a full-thickness tear of the supraspinatus tendon (Patte grade I or II), (3) a positive Jobe and belly-press tests before the intervention (4) a fatty infiltration 1 or 2 at MRI imaging, (5) above lesions treated by arthroscopic repair, using a suture anchor, (6) a minimum of 6 months of follow-up after the intervention.
Patients who had complete superior two-thirds tear or more of the subscapularis tendon (Lafosse classification III, IV, and V), a not reparable supraspinatus tear, an infraspinatus tear, an infection or previous surgery of the same shoulder were excluded from the study.
Clinical evaluation was performed both preoperatively and postoperatively by an independent observer with a Constant score, simple shoulder test (SST) and visual analog scale (VAS).
In addition, the strength of the tendons was assessed with a mechanic dynamometer. SS strength was recorded both before surgery and at follow-up, whereas SSC strength was tested at final follow-up and compared with contralateral side. The Jobe test was performed in a standing position, with the arm in 90° of abduction and the elbow fully extended. The belly-press test [12, 30–32] was performed in a standing position, with the back against the wall in order to exclude the influence of other muscles. The wrist was kept in a fixed position (Fig. 1a, b). Belly-press test was considered negative when patients showed the same strength of the unaffected side, lacking when strength was 50 % and positive when was <50 % of the unaffected side.
An ultrasound examination was performed by two senior radiologists in all patients at a minimum follow-up of 6 months to assess the quality of tendon healing. Tendon was classed 1 when completely healed, 2 when presented degenerative appearance or was torn for <50 % of thickness, 3 when 50 % or more was not healed. The correlation between echographic tendon healing and strength recovery was investigated as well.
Surgical technique
All patients had the same anesthesia consisting in peripheral nerve blocks plus general anesthesia.
In lateral decubitus, patients had the arm in a specific traction device with 60° of abduction and 6–7 kg of traction. In the beach-chair position, patients had the affected arm in a traction device in 60° of forward flexion and 3–4 kg of traction. A standard posterior portal was created approximately 2 cm inferior and medial from the posterolateral corner of the acromion. A diagnostic examination was performed. LHB was addressed with tenotomy or tenodesis with lasso-loop technique [33]. Subscapularis tendon insertion was visualized with the arm in flexion and internal rotation [18]. Subscapularis repair was performed first. The tendon was released, if retracted, and debrided through combined anterior and anterolateral portals. The comma sign [34], if present in case of retracted tear, was preserved. Suture was realized in a single-row shape, with a simple or mattress stitch on metallic anchor (SuperRevo® or ThRevo® suture anchor, 5 mm, ConMed Corporation, French Road, Utica, NY, USA). SS repair was then performed. The suture was in a single-row fashion or in a suture-bridge configuration, adding a knot-less anchor for the lateral row (PopLok® knotless anchor, 4.5 mm, ConMed Corporation, French Road, Utica, NY, USA).
Acromioplasty and Mumford procedures were realized in the final part of the intervention, where indicated. Coracoplasty was performed where examination showed a narrow coracohumeral space.
Rehabilitation protocol
All patients were discharged 1 day after surgery with an abduction sling and analgesics. They observed an immobilization period of 30 days. An early rehabilitation program was started from the second week post-op, in supine position and avoiding mobilization in external rotation for 6 weeks. After 1 month, they started active motion. Recovery of passive full range of motion was carefully pursued. Every kind of strain was forbidden for the first 3 months. Mild efforts were then allowed, without lifting heavy weights. From the sixth month, the patients were allowed to regain all daily living activities.
Follow-up
All patients were reviewed at 6 weeks and 3 months to check shoulder ROM. Last evaluation was performed at a minimum follow-up of 6 months. The evaluation was performed with the same preoperative scores (Constant, SST, VAS) and clinical tests by an independent examiner. Strength recovery at the belly-press and the Jobe tests was assessed with a dynamometer. Standard X-rays and ultrasound examination were performed. All patients were asked about satisfaction with the operation (yes/no). All patients gave their informed consent prior to their inclusion in the study.
Statistical analysis
Descriptive analysis consisted of frequencies and percentages for discrete data and means and standard deviations for continuous data. The paired t test was performed to analyze the difference in pre- and post-outcome scores for strength and Constant score. Results of the belly-press test were converted into a 3-point continuous variable ranging from 1 (same strength) to 3 (strength <50 %).
The state of the tendon as detected by the US examination was converted into a 3-point continuous variable where: score = 1 referred to a completely healed tendon, score = 2 was given when the tendon had degenerative appearance or was torn for less than 50 % of thickness, score = 3 was given when 50 % or more was not healed.
The association between strength recovery and US tendon healing was determined using Pearson’s correlation. All tests were two-tailed, and significance was set with an alpha value of 0.05.
Results
Sixty-one cases matched with the criteria, and all of them gave their consent for inclusion in the study. Forty-three patients were treated in lateral decubitus (LD), and 18 patients in beach-chair position (BC). There were 34 males and 27 females with an average age at the time of the intervention of 59 ± 7 years. Right shoulder was involved in 37 cases, and the dominant arm in 44 cases. Median time between symptoms onset and intervention was 8 ± 3 months. The tear was caused by a traumatic injury in 34 out of 61 cases. In those patients, mean time between trauma and surgical procedure was 6 ± 1 months. All patients were available at an average follow-up of 18 ± 7 months (minimum follow-up of 6 months in all cases).
All patients had acromioplasty, 5 had Mumford procedure, 1 patient had coracoplasty. Average Constant score improved from 30.8 ± 10.2 preoperatively to 76.5 ± 12.0 postoperatively, average SST from 2.6 ± 2.0 to 8.8 ± 2.9 and average VAS pain scale from 3.8 ± 1 to 0.5 ± 0.5 (p < 0.0001) (Fig. 2). Mean strength at Jobe test improved from 1.2 to 6.7 (p < 0.0001). Mean strength at belly-press was 5.5 contralateral value of 9.1 (p < 0.0001) (Fig. 3). Mean strength recovery data are reported in Table 1. All patients were satisfied with the operation except for one, who complained of a persistent neck pain although her cuff was healed. The ultrasound examination showed a healed SS tendon in 61 %, a degenerative pattern in 28 % and a tear in 11 % of cases. SSC was intact in 78 % and presented some heterogeneity of the fibers in 22 % of cases. There were not retears of SSC. A significative correlation between ultrasound tendon healing and strength recovery was found (p = 0.05): 0.59 for SS and 0.45 for SSC.
Discussion
Clinical presentation of subscapularis tendon tears depends on the tear size, the degree of tear propagation to the adjacent cuff and the involvement of the LHB. Some patients may have no symptoms or only mild symptoms despite having several lesions, while others may have a complete impairment and severe pain with only an isolated SSC tendon tear [25]. Biceps tendon is thought to be a major source of pain [35]. In the present series, subscapularis tear was in most cases only a clinical preoperative finding. The belly-press test showed a good sensitivity. MRI did not show any SSC tear in 40 % of cases. These data are in accordance with the existing literature [36]. In some cases, SSC lesions were supposed by clinical examination and indirect MRI signs such as LHB instability and tendinosis in T2-weighted images. Additionally conventional intraoperative inspection revealed almost normal articular morphology, and estimating the extension of the lesion was not possible. A complete visualization of the SSC footprint was only possible with the arm in internal rotation and aiming the scope at the lesser tuberosity, as described by Burkhart and Brady [18]. Concurrent supraspinatus tear permitted to have good access to subscapularis tendon and to easily perform its release once it was tractioned laterally. The comma sign [34] was visible in all retracted tears and was preserved during repair (Fig. 4a–c). This allowed a partial reduction in the supraspinatus tear and facilitated its reinsertion.
Several studies have documented high success rates following arthroscopic or open treatment of subscapularis tendon tears [13, 14, 19, 37, 38]. Open repair of anterosuperior tears have been associated with good clinical outcomes at long follow-up [39]. More recently, some studies have reported the outcomes of combined surgical treatment of anterosuperior cuff tears with biceps pathology by means of arthroscopy [24–27, 40].
Bennett [8] reviewed 19 cases (out of 35 operated) of anterosuperior tears in 139 arthroscopic rotator cuff repair performed in beach-chair position. Partial SSC tears were also included. Care was taken to repair the biceps pulley, and biceps tenodesis was performed only if LHB was severely frayed. LHB lesions were present in 18 of 19 cases. Only 2 patients had persistent biceps inflammation after the operation. The average Constant score improved from 53 to 77. The authors reported that belly-press test and lift-off test could detect partial and full-thickness tears of the subscapularis tendon only in case of normal internal rotation with the arm at 90° of abduction compared with the normal side (despite false positive findings). Definitive tests for rerupture or nonhealing were not used, and conclusions were based on clinical examination findings and the acromiohumeral distance.
More recently Kim et al. [25] retrospectively reviewed 20 (out of 32 operated) patients at a minimum 2-year follow-up after an anterosuperior repair. Only the repair of partial subscapularis tears was included. The treatment was performed percutaneously with a spinal needle in lateral decubitus. LHB was fixed to the rotator interval. Good strength recovery compared to unaffected side was reported with a digital device, but the measurement method was not described. A positive belly-press test was observed in 6 cases at last follow-up. A long-lasting tenderness at the bicipital groove was also noted. A MRI control at follow-up was available in 12 of 20 patients and showed a SS retear in 4 cases and a SS and SSC retear in 1 case. Nevertheless, the functional results were good to excellent regardless of an evident retear at MRI. Constant score improved from 39.6 to 71.2.
Katthagen et al. [24] described a prospective series of 65 patients. Isolated tears of the SSC tendon were also included. The strength was not assessed, and there was not any imaging analysis to confirm structural integrity of the tendon at the time of last follow-up. A good outcome at 1 year was reported (89.3). LHB tenotomy was associated with better results than tenodesis.
Schnaser et al. [26] reviewed 155 cases of rotator cuff tears. In 44 cases, a SSC tear was found on preoperative imaging. In 17 cases, a full-thickness anterosuperior cuff tear was repaired and reviewed at an average follow-up of 15 months, with clinical scores and postoperative MR or CT imaging. Two SS retears were reported, whereas no SSC retears were found.
Maqdes et al. [27] performed a prospective multicentric study on 53 anterosuperior tears. An improvement from 49 to 73 points in the Constant score was recorded at an average follow-up of 15 months. A global retear rate of 6 % was reported. Constant score was lower in case of severe subscapularis fatty infiltration. However, the improvement in the Constant score was similar regardless the initial subscapularis fatty infiltration. The rate of tendon healing was correlated with subscapularis fatty infiltration. Subscapularis tendon rupture size was not significantly correlated with outcomes.
Kim et al. [40] analyzed 59 anterosuperior cuff tears, treated by means of arthroscopy either by disrupting the margin between the subscapularis and supraspinatus or by performing the repair in continuity without disrupting the margin. The two groups showed the same clinical and structural outcomes at 2-year follow-up. This is a relevant finding about the role of the comma sign, which was usually preserved in the previous series.
Most of the reported series show similar incidence for the anterosuperior lesions and comparable functional results after operative treatment. The outcomes of the present study are similar to those reported in literature.
Only one patient was not satisfied with the operation for a persistent neck pain in presence of a healed cuff. One patient developed a facioscapulohumeral dystrophy within a year after the operation. She had just pain relief because of a Mumford procedure on her acromioclavicular joint.
The strength recovery of the rotator cuff in terms of forward elevation, abduction, internal and external rotation at 6-month follow-up was statistically significant. Furthermore, dynamometric strength assessment was evaluated in all cases. Affected and unaffected shoulders showed similar strength at the final follow-up, with the exception of the cases where rerupture occurred. In some cases, the passive range of external rotation did not come back to the level of the contralateral shoulder; however, this did not seem to restrict the daily activities, as it had already been described [25]. Ultrasound examination showed tendon healing in medium correlation with strength recovery.
This study has several limitations. First of all, it is a cohort study with a quite short follow-up. The absence of a control group may limit its clinical relevance.
Nevertheless, it is a consecutive series of homogeneous patients with the same preoperative diagnosis and having been treated with the same surgical procedure. In addition all patients had the same preoperative and postoperative evaluation (clinical and imaging) as well as the same postoperative protocol. Finally, a correlation between echographic tendon structures at the last follow-up was found in medium correlation with the recovery of the strength in internal rotation. There are few similar series in the literature, and none of them reported a strength recovery analysis.
Forthcoming studies are warranted to investigate a relationship between clinical and anatomical results.
Conclusions
The treatment of SSC tears requires precise clinical and imaging diagnosis, and consequent arthroscopic surgery must confirm the exact pathologic anatomy. Arthroscopic repair of anterosuperior cuff tears provides good clinical pain relief and functional recovery at a short follow-up. In particular, a good strength improvement was recorded.
References
Edwards TB et al (2006) Arthroscopic debridement in the treatment of patients with isolated tears of the subscapularis. Arthroscopy 22(9):941–946
Bennett WF (2001) Subscapularis, medial, and lateral head coracohumeral ligament insertion anatomy. Arthroscopic appearance and incidence of “hidden” rotator interval lesions. Arthroscopy 17(2):173–180
Gerber C, Terrier F, Ganz R (1985) The role of the coracoid process in the chronic impingement syndrome. J Bone Joint Surg Br 67(5):703–708
Gerber C, Sebesta A (2000) Impingement of the deep surface of the subscapularis tendon and the reflection pulley on the anterosuperior glenoid rim: a preliminary report. J Shoulder Elb Surg 9(6):483–490
Lo IK, Burkhart SS (2003) The etiology and assessment of subscapularis tendon tears: a case for subcoracoid impingement, the roller-wringer effect, and TUFF lesions of the subscapularis. Arthroscopy 19(10):1142–1150
Lo IK, Parten PM, Burkhart SS (2003) Combined subcoracoid and subacromial impingement in association with anterosuperior rotator cuff tears: an arthroscopic approach. Arthroscopy 19(10):1068–1078
Kim TK, Rauh PB, McFarland EG (2003) Partial tears of the subscapularis tendon found during arthroscopic procedures on the shoulder: a statistical analysis of sixty cases. Am J Sports Med 31(5):744–750
Bennett WF (2003) Arthroscopic repair of anterosuperior (supraspinatus/subscapularis) rotator cuff tears: a prospective cohort with 2- to 4-year follow-up. Classification of biceps subluxation/instability. Arthroscopy 19(1):21–33
Nho SJ et al (2010) Arthroscopic repair of anterosuperior rotator cuff tears combined with open biceps tenodesis. Arthroscopy 26(12):1667–1674
Edwards TB et al (2005) Repair of tears of the subscapularis. J Bone Joint Surg Am 87(4):725–730
Nove-Josserand L et al (1994) Isolated lesions of the subscapularis muscle. Apropos of 21 cases. Rev Chir Orthop Reparatrice Appar Mot 80(7):595–601
Gerber C, Hersche O, Farron A (1996) Isolated rupture of the subscapularis tendon. J Bone Joint Surg Am 78(7):1015–1023
Burkhart SS, Tehrany AM (2002) Arthroscopic subscapularis tendon repair: technique and preliminary results. Arthroscopy 18(5):454–463
Bennett WF (2003) Arthroscopic repair of isolated subscapularis tears: a prospective cohort with 2- to 4-year follow-up. Arthroscopy 19(2):131–143
Lafosse L et al (2010) Arthroscopic repair of subscapularis tear: surgical technique and results. Orthop Traumatol Surg Res 96(8 Suppl):S99–S108
Adams CR, Schoolfield JD, Burkhart SS (2008) The results of arthroscopic subscapularis tendon repairs. Arthroscopy 24(12):1381–1389
Nove-Josserand L et al (2012) Clinical and structural results of arthroscopic repair of isolated subscapularis tear. J Bone Joint Surg Am 94(17):e125
Burkhart SS, Brady PC (2006) Arthroscopic subscapularis repair: surgical tips and pearls A to Z. Arthroscopy 22(9):1014–1027
Lafosse L et al (2007) Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am 89(6):1184–1193
Paribelli G, Boschi S (2005) Complete subscapularis tendon visualization and axillary nerve identification by arthroscopic technique. Arthroscopy 21(8):1016
Bartl C, Imhoff AB (2007) Management of isolated subscapularis tendon tears. Orthopade 36(9):848–854
Toussaint B et al (2012) Arthroscopic repair of subscapularis tears: preliminary data from a prospective multicentre study. Orthop Traumatol Surg Res 98(8 Suppl):S193–S200
Denard PJ et al (2012) Long-term outcome of a consecutive series of subscapularis tendon tears repaired arthroscopically. Arthroscopy 28(11):1587–1591
Katthagen JC et al (2013) Anterosuperior rotator cuff tears: rupture configurations and results after arthroscopic therapy—a prospective study. Unfallchirurg 116(2):151–160
Kim DY et al (2012) Arthroscopic percutaneous repair of anterosuperior rotator cuff tear including biceps long head: a 2-year follow-up. Clin Orthop Surg 4(4):284–292
Schnaser E et al (2013) Arthroscopic treatment of anterosuperior rotator cuff tears. Orthopedics 36(11):e1394–e1400
Maqdes A et al (2014) Does preoperative subscapularis fatty muscle infiltration really matter in anterosuperior rotator cuff tears repair outcomes? A prospective multicentric study. Orthop Traumatol Surg Res 100(5):485–488
Patte D (1990) Classification of rotator cuff lesions. Clin Orthop Relat Res 254:81–86
Fuchs B et al (1999) Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elb Surg 8(6):599–605
Tokish JM et al (2003) The belly-press test for the physical examination of the subscapularis muscle: electromyographic validation and comparison to the lift-off test. J Shoulder Elb Surg 12(5):427–430
Gilmer B et al (2007) Normalization of the subscapularis belly-press test. J Shoulder Elb Surg 16(4):403–407
Paladini P et al (2012) Long-term subscapularis strength assessment after Bristow-Latarjet procedure: isometric study. J Shoulder Elb Surg 21(1):42–47
Lafosse L, Van Raebroeckx A, Brzoska R (2006) A new technique to improve tissue grip: “the lasso-loop stitch”. Arthroscopy 22(11):1246e1–1246e3
Lo IK, Burkhart SS (2003) The comma sign: an arthroscopic guide to the torn subscapularis tendon. Arthroscopy 19(3):334–337
Kontakis GM (2007) The long biceps tendon as the main cause of shoulder pain in rotator cuff tears. Orthopedics 30(3):185
Garavaglia G, Ufenast H, Taverna E (2011) The frequency of subscapularis tears in arthroscopic rotator cuff repairs: a retrospective study comparing magnetic resonance imaging and arthroscopic findings. Int J Shoulder Surg 5(4):90–94
Deutsch A et al (1997) Traumatic tears of the subscapularis tendon. Clinical diagnosis, magnetic resonance imaging findings, and operative treatment. Am J Sports Med 25(1):13–22
Flury MP et al (2006) Rupture of the subscapularis tendon (isolated or in combination with supraspinatus tear): when is a repair indicated? J Shoulder Elb Surg 15(6):659–664
Di Schino M, Augereau B, Nich C (2012) Does open repair of anterosuperior rotator cuff tear prevent muscular atrophy and fatty infiltration? Clin Orthop Relat Res 470(10):2776–2784
Kim SJ et al (2015) Arthroscopic repair of a significant (>50 %) partial-thickness subscapularis tear concomitant with a full-thickness supraspinatus tear: technical considerations for subscapularis repair (transtendon technique versus tear completion). J Shoulder Elb Surg. doi:10.1016/j.jse.2014.10.009
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Visonà, E., Paladini, P., Merolla, G. et al. Strength recovery after arthroscopic anterosuperior cuff repair: analysis of a consecutive series. Musculoskelet Surg 99 (Suppl 1), 37–42 (2015). https://doi.org/10.1007/s12306-015-0369-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-015-0369-9