Abstract
This paper describes the anatomy and function of the proximal tibiofibular joint (PTFJ). The physical dimensions of the joint and the topology of the articular surfaces are described. It is noted that the inclination of the joint is variable, and that joints with a steeper slope away from the transverse plane are less mobile. The ligamentous and tendinous attachments are described. Finally, the histological features of the articular surfaces are presented. The clinical importance of the anatomical features is discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The anatomy, clinical and functional importance of the proximal tibiofibular joint (PTFJ) seems to be neglected in the literature. Some articles explore the anatomy and physiology of this joint more deeply, stressing its biomechanical aspects in weight bearing [10] and in relation to ankle motion [13, 14]. Marshall et al. [12] stressed the importance of lateral stability. The proximal fibula, serving as the point of insertion of the biceps femoris (BF), must play an integral role in this lateral stabilisation, and dislocation of the proximal fibula may disrupt lateral stability.
The tibia and fibula move relative to each other in three regions—the proximal tibiofibular articulation, the interosseous membrane and the distal tibiofibular syndesmosis [13]. Movement is slight at the PTFJ, but it imparts some flexibility during ankle movement and in response to the action of the muscles attached to the fibula [15]. The fluoroscopic studies of Ogden [13] showed that with dorsiflexion of the ankle, the proximal fibula rotated a few degrees with this rotation being more evident in the horizontal than the oblique PTFJ. Barnett and Napier [1] observed that the fibula rotates laterally on its long axis during dorsiflexion of the ankle. Ogden evaluated anteroposterior motion of the proximal fibula with positional changes of the knee. With knee flexion, the fibula moved anteriorly, while in extension of the knee, the proximal fibula was pulled posteriorly. This motion was more evident in young children than in adults. According to Ogden [13], in most patients, with the knee flexed, the fibular head could be moved approximately 1 cm in both anterior and posterior directions. With the knee extended the excursion of the fibular head was minimal.
In lower animals, the fibula is considered one of the most important supporting structures of the leg. With man’s conversion from digitigrade to plantigrade ambulation, anthropologists and anatomists have given a lesser, if not a vestigial, function to the fibula [10]. However, certain clinical situations suggest that the fibula’s function is not so simple or restricted. The tibia’s response in congenital absence of the fibula, in cases in which the fibula has been removed surgically, and the importance of the lateral malleolus in ankle fractures all suggest participation of the fibula in weight bearing [10]. According to Basmajian [2], the PTFJ may be regarded as an ‘accommodatory joint’, designed to give a little play to the fibula to protect it from breaking.
The anatomy of the PTFJ is related to its ability to withstand forces applied axially [13]. While one of the functions of the PTFJ appears to be dissipation of torsional loading applied at the ankle joint, Lambert [10] felt that the fibula also had a weight-bearing function, with approximately one-sixth of the static load applied at the ankle being transmitted to the PTFJ. This force was generated by the fibula’s articulation with the talus and possibly also by the inferior tibiofibular ligaments and was transmitted to the PTFJ. Little of the load was transmitted by the interosseous membrane. While Lambert’s study implied a compressive function at the PTFJ, Preuschoft [14] suggested that the PTFJ functions primarily for tensile dissipation of lateral tibial bending moments. Evans and Band [8] found that the middle and proximal thirds of the fibula had greater tensile strength than any other skeletal component, including tensile regions of the femur.
In conclusion, the primary functions of the PTFJ are dissipation of torsional loads applied at the ankle, dissipation of lateral tibial bending moments and transmission of axial loads in weight bearing. However, there is a lack of knowledge on the details of this joint.
A marked variability in its morphological characteristics has been described. Therefore, basic data on topographical and morphological parameters are necessary. Furthermore, scientific publications lack relevant information on the frequency of osteoarthritic changes, and the type and amount of the covering cartilage has to be evaluated [6, 7, 9].
The general concept of this articulation is that it is a small synovial joint of the planar type between a flat, circular or oval facet on the head of the fibula and a similar facet placed posterolaterally under the overhanging lateral condyle of the tibia. However, in this study we have demonstrated that the planar type is less frequent than previously reported.
With the intent to obtain basic data on topographical and morphological parameters, we have made an anatomic study based on the dissection of cadaver knees and analysis of histological sections.
Material and methods
Twenty normal cadaver knees, from fresh autopsy specimens, were dissected according to an adaptation of LaPrade’s technique [11]. There were 7 right and 13 left knees from 20 male cadavers. The average age of the donors was 50 years (SD 10.7, range 35–64). The average weight was 71 kg (SD 7.4 kg) and the average height 175 cm (SD 4.3 cm).
With this technique, the BF was dissected over the proximal area of the fibula and tibia to determine its relationship to the anterior tibiofibular ligament (Fig. 1). These two anatomical structures were fused in all specimens. The BF and anterior tibiofibular ligament were dissected over the PTFJ and the joint capsule was opened (Fig. 2).
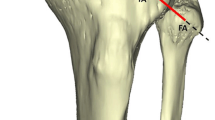
At this moment, the articular surfaces were exposed sufficiently to allow measurement of the inclination of the articular surface (Fig. 3). The inclination of the PTFJ was measured by the method described by Eichenblat and Nattan [5], and 20° was considered the limit of the horizontal-type joint and any inclination greater than that was considered an oblique-type joint according to the classification of Ogden [13]. The inclination was defined as the angle between the line of steepest slope and the horizontal plane.
After that, we opened the articulation entirely and dislocated the articular facets.
The articular facets were classified according to the type of the joint and the shape (contour) of the facets and measurement of the surface area was made.
The type of the joint was classified as plane, trochoid (L-shaped) or double trochoid (L-shaped with a vestigial facet) (Fig. 4). We applied the name ‘double trochoid’ to the type of joint where the articular facet of each bone was composed of two cylindrical segments, one convex and the other concave.
The shape (contour) of the facets was classified as circular, elliptic or triangular. We refer here to the shape of the outline of the articular facets of the tibia and fibula without reference to the type of joint.
The surface area of cartilage was obtained by assuming it to be approximately elliptical and calculated by using the minimal and the maximal diameters [6, 7, 9].
Osteoarthritic changes affecting the PTFJ were recorded and classified into three different degrees (slight, moderate and marked). The degree of osteoarthritic changes was established according to the following criteria:
-
Slight: appearance of fibrillated and eroded cartilage.
-
Moderate: destruction of the cartilage, hypertrophic synovium and capsular thickening.
-
Marked: necrotic areas, gross flapping and osteophytes were present.
-
Ankylosis of the joint may be considered as a final stage.
Some topographical parameters were recorded, like the distance between the PTFJ and the articular line of the knee, and the anterior and posterior limits of the proximal tibia.
Results
Type of joints
Their respective frequencies were: plane type 2, trochoid type 13 and double trochoid type 5 (Fig. 5).
All of the trochoid joints had a convex surface on the tibia and a concave surface on the fibula. As noted by Eichenblat and Nathan [5], the posterolateral half of the fibular facet was concave and the anteromedial facet was convex, and the tibial facet was reciprocally shaped.
Inclination of the articular facets
We have found three articulations of the horizontal type and 17 of the oblique type.
Trochoid surfaces were most frequent in the oblique group, while no difference could be shown in the horizontal group. The results are shown in Fig. 6.
Contour of the articular surfaces
We found three types: elliptical, circular and triangular. The frequencies of the various shapes in the tibia and fibula are shown in Fig. 7.
The articular facet of the tibia was most frequently circular—13 cases (Fig. 8); the most frequent shape in the fibula was triangular—15 cases (Fig. 9).
Dividing the PTFJ into oblique and horizontal types, the circular shape was the most frequent in the tibia with 11 of 17 cases and 2 of 3 cases in the oblique and horizontal types; in the fibula, the triangular shape had a frequency of 12 of the 17 in the oblique type and all three of the horizontal type.
Surface area
The mean of the tibial surface areas was 3.26 cm² (SD 0.43) and the mean fibular surface area was 2.57 cm² (SD 0.36).
Dividing this parameter by the oblique and horizontal types on the tibia, the oblique type had a mean area of 3.2 cm² (SD 0.44), and the horizontal type of 3.6 cm² (SD 0.45). On the fibula, the mean area of the oblique type was 2.52 cm² (SD 0.34), and 2.8 cm² (SD 0.43) for the horizontal type.
On the tibia, the non-planar joints had a mean area of 3.25 cm² (SD 0.44), and the plane type 3.24 cm² (SD 0.5). On the fibula, the mean area of the non-planar (L-shaped) type was 2.55 cm² (SD 0.37), and of the plane type 2.47 cm² (SD 0.31).
Thickness of the cartilage
The mean thickness of the cartilage was 1.9 mm (SD 0.5) (1–2.8 mm) in the tibia and 1.1 mm (SD 0.2) (1–2 mm) in the fibula.
The mean thickness of the cartilage of the lateral femoral condyle was 2.14 mm (SD 0.4) in the weight-bearing area and 1.86 mm (SD 0.5) in the upper part of the lateral condyle (Fig. 10).
The histologic examination at the fibula and tibia showed the typical configuration of hyaline cartilage with predominately small condrons and with narrow interterritories. Cartilage of the tibial and lateral femoral condyle surface. There were no significant differences between the two histologic patterns
Soft parts of the joint
Capsule: In all the knees dissected, the capsule was thicker anteriorly.
Synovial membrane: The synovial membrane covered the recesses created by the capsule inserting at a distance from the fibular and tibial facets. An intervening fat pad was present between the capsule and the bone at this point.
Cartilage: The macroscopic appearance was smooth articular cartilage. In 2 of the 20 dissected joints, the cartilage was fibrillated and eroded; these were graded as slight osteoarthritic changes. Both joints were of oblique-trochoid form. Marked osteoarthritic changes were not seen in any specimens; osteoarthritic changes were only seen in the PTFJ of knees with concomitant osteoarthritis.
Concomitant diseases
Osteoarthritis was seen in 2 of the 20 knees and these also had changes in the PTFJ.
Topographical parameters
Distance between the most superior part of the PTFJ and the articular line of the knee (A–B)—the mean distance was 10.8 mm (SD 2.8) (Fig. 11).
Distance between the most anterior part of the PTFJ and the anterior limit of the proximal tibia (C–D)—the mean distance was 32.6 mm (SD 4.4).
Distance between the most posterior part of the PTFJ and the posterior limit of the proximal tibia (E–F)—the mean distance was 2.1 mm (SD 3.6).
Histology
Material and methods
For the histological portion of the study, blocks of tissue were prepared from the articular cartilage of the tibial and fibular facets of the PTFJ and from the articular cartilage of the inferior and upper parts of the lateral condyle. Anatomic landmarks and measurements paralleling those in the cadaveric portion of the study were present in all sectioned specimens processed for histologic staining and were marked for future identification.
The graft was taken from subchondral bone to avoid a decalcification procedure. For histochemistry investigation, the blocks were fixed in formaldehyde for 2 days, washed, dehydrated in alcohol, embedded in Paraplast and cut into 7 μm sections. Sections were deparaffinised in xylene and rehydrated in graded ethanol. Subsequently, the sections were stained with haematoxylin and counterstained with eosin for qualitative assessment.
Results
The histological examination of the fibula and tibia showed the typical configuration of hyaline cartilage with predominately small condrons and with narrow interterritories (Fig. 10). Unmasked fibres were found sporadically. Immunohistochemically, type II collagen was detected in the studies of Jerosh et al. [9], but was not evaluated in this study.
Discussion
The PTFJ is characterised by its great morphological variability [5, 6, 7, 9, 13]. It is an arthroidal sliding joint located between the lateral tibial condyle and the fibular head. The articular surfaces are variable in size, form and inclination. The facets on the head of the fibula and tibia were circular, triangular or elliptical and were covered with cartilage. Ogden [13] classified this joint into two types considering the inclination with the horizontal plane: horizontal and oblique. The horizontal type is associated with increased rotatory mobility and increased joint surface area, and the oblique with less rotatory mobility and less joint surface area. In this series of 20 specimens, 17 had oblique and 3 had horizontal type PTFJ.
The most common types of joints found were the L-shaped (trochoid and the double trochoid) followed by the plane type: 13 were trochoid, 5 were double trochoid and only 2 were planar, in contrast to the standard anatomised descriptions of a planar form. The observation by Eichenblat and Nathan [5] that in 10 fibulas and 12 tibias no articular facets could be identified suggested that in some cases the PTFJ may not be a synovial joint but a syndesmosis like the distal tibiofibular joint. However, that was not found in this study or in other publications.
The articular surface of the head of the fibula is directed upward and slightly anteriorly and medially to articulate with the posterior part of the lateral condyle of the tibia. These articular surfaces were inferior and posterior to a projection of the lateral edge of the tibia. These posterolateral placements of the articular surfaces give bony stability, preventing anterior displacement of the proximal fibula.
We agree with Ogden [13] that the articular surfaces in the oblique type were much more variable in surface area, configuration and inclination.
The articulation is surrounded by a fibrous capsule which is attached to the margins of the articular facets on the tibia and fibula; it is thicker anteriorly than posteriorly, as described by Davies [4]. Tobias and Arnold [16] found the capsule thicker posteriorly in only 10% of cases. The capsule is strengthened by two prominent accessory ligaments, which provide additional stability (Fig. 2). The posterior aspect of the capsule consists of a single weak band running from the fibular head to the posterior aspect of the popliteus tendon. Superiorly, support to the joint is provided by the lateral collateral ligament (LCL). The anterior (anterosuperior) ligament consists of two or three flat fibrous bands, which pass obliquely upwards from the front of the head of the fibula to the front of the lateral condyle of the tibia. The posterior (posterosuperior) ligament is a thick single broad band, which passes obliquely upwards from the back of the head of the fibula to the back of the lateral condyle of the tibia. It is covered by the tendon of the popliteus. These ligaments are not entirely separable from the fibrous capsule.
In all specimens, the BF tendon was inserted into the fibular head, the LCL of the knee and the lateral tibial condyle, with expansions to the crural fascia covering the anterior, lateral and posterior compartments of the leg. It was difficult to distinguish the anterior tibiofibular ligament in all specimens as a separated band because it was fused intimately with the BF. Marshall et al. [12] studied the anatomy of the BF and discussed its functional significance. They found that in knees in which there was a low bifurcation of the tibial attachment of the BF tendon’s deep layer, it was difficult to distinguish the anterior tibiofibular ligament as a separate band because it was fused intimately with the BF.
The synovial membrane of the joint is continuous with that of the knee joint through the subpopliteal recess in 10% of the specimens. According to Eichenblat and Nathan [5], 12% of PTFJ communicated with the knee joint thought the subpopliteal recess, while Weeks found it to be 15% [18]. The synovial cavities are in close proximity when a communication between the joints does not exist. In such a case, there is a risk of opening the knee joint when excising the fibular head. Bozkurt et al. [3] observed communication between the PTFJ and the knee in 9 of 14 specimens (64%) by MRI arthrography. This difference may be attributable to the use of different methods. During MRI arthrography, the hydrostatic pressure of the dye might have shown the communication, which is undetectable during cadaver dissections. Veth et al. [17] reported such a communication in one of their two cases by arthrography. The current findings may be clinically important because either joint may be affected when joint pressure is elevated.
Eichenblat and Nathan [5] studied the types and angles of inclination of the PTFJ in relation to the presence of osteoarthritis affecting the same joint, and in neither case was a correlation found. Clinically, however, osteoarthritis of this joint is a rare finding, suggesting that osteoarthritis of the PTFJ is either asymptomatic or its symptoms are in part attributed to osteoarthritis of the knee joint, which is frequently affected and produces severe pain. They found a statistically significant correlation in their specimens between the presence of osteoarthritis of the PTFJ and osteoarthritis of the knee, particularly affecting the medial compartment. It may well be that varus deformity of the knee plays a role in the development of osteoarthritis of the PTFJ. Varus deformity imposes stress on the lateral ligament structures, including the LCL and the BF which are both attached to the fibular head, and during the stance phase of walking increased pressure may develop in the PTFJ.
In this study, osteoarthritic changes were found in 2 of 20 knees (10%), while Eichenblat and Nathan [5] found osteoarthritis of some degree in 38% of dried specimens. The noticeable difference from our findings might be due to the difficulty of differentiating in bone specimens between physiological features and osteophytes. Possible signs to distinguish physiological and pathological aspects are the evenness and the border to the surrounding bone. Our results showed that even in the older bodies we have dissected, the hyaline cartilage of the PTFJ was of surprisingly good quality.
The nerves to the joint are derived from the common peroneal nerve (PN) and from the nerve to the popliteus [15]. Surgical approaches to the proximal PTFJ especially endanger the PN, the anterior tibial artery and the LCL. In our study, the mean distance from the inferior part of the joint to the PN was 19.5 mm (Fig. 3).
Importance of the clinical anatomy
The observations reported in this study can contribute to the understanding of the pathology of the PTFJ. The anatomical characteristics of this joint explain the instability of the oblique type and the behaviour on rotation of the horizontal type.
The variation of the BF tendon’s insertion and the communication of the PTFJ and the knee in the oblique type of PTFJ may be associated with problems of this type of joint. Additionally, because of this communication, the PTFJ might be construed as the fourth compartment of the knee to explain subtle knee problems [3].
Espregueira-Mendes et al. [6] and Jerosh et al. [9] reported that the PTFJ can be a good source of osteochondral autograft to treat cartilage lesions with less morbidity. This joint provides good articular cartilage without damage to the weight-bearing surface of the knee joint. It is possible to collect at least six cylinders with a diameter of 6 mm (2.16–5 cm² of resurfacing potential) (Fig. 12).
The PTFJ is pain-free after resection in a large majority of cases [7] and this can be used as an associated procedure in upper valgus tibial osteotomies.
References
Barnett CH, Napier JR (1952) The axis of rotation of the ankle joint in man. Its influence upon the form of the talus and the mobility of the fibula. J Anat 86:1
Basmajian JV (1970) Primary anatomy, 6th edn. Williams and Wilkins, Baltimore, pp 111–112
Bozkurt M, Yilmaz E, Atlihan D, Tekdemir I, Havitçioglu H, Gunal I (2003) The proximal tibiofibular joint—an anatomic study. Clin Orthop 406:136–140
Davies DV (1967) Gray’s anatomy, 34th edn. Longman, London
Eichenblat M, Nathan H (1983) The proximal tibiofibular joint: an anatomical study with clinical and pathological considerations. Int Orthop 7:31–39
Espregueira-Mendes JD, Cabral T, Teles C, da Silva B, Lima P (1983) Tratamento de Osteocondrite Dissecante do joelho com um novo enxerto osteocartilagineo de peróneo—a propósito de um caso clinico. Revista Portuguesa de Ortopedia e Traumatologia 1(2):181–183
Espregueira-Mendes JD, Monteiro A, Amado P, Miranda A (1999) A new osteocondral autogenous graft from the upper tibioperoneal joint—GUT, Congress of the International Society of the Knee Surgery (ISAKOS), Washington
Evans FG, Band S (1966) Physical and histological differences between human fibular and femoral compact bone. In: Evans FG (eds) Studies on the anatomy and function of bone and joints. Springer, Berlin Heidelberg New York, pp 142–155
Jerosh J, Filler TJ, Peuker ET (2002) The cartilage of the tibiofibular joint: a source for the autologous osteochondral grafts without damaging weight-bearing joint surfaces. Arch Orthop Trauma Surg 122:217–221
Lambert KL (1971) The weight-bearing function of the fibula. J Bone Joint Surg Am 53:507–513
LaPrade RF, Hamilton CD (1997) The fibular collateral ligament—biceps femoris bursa. Am J Sports Med 25(4):439–443
Marshall JG, Girgis FG, Zelko RR (1972) The biceps femoris tendon and its functional significance. J Bone Joint Surg Am 54:1444–1450
Ogden JA (1974) The anatomy and function of the proximal tibiofibular joint. Clin Orthop 101:186–191
Preuschoft H (1971) Die mechanische Beanspruchung der Fibula bei Primaten. Gegenbaurs Morph Jahrb 117:211–216
Sobotta J (1982) Atlas der Anatomie des Menschen. Urban & Schwarzenberg, Munich, pp 297–307
Tobias PV, Arnold M (1967) Man’s anatomy III. Witwatersrand University Press, Johannesburg
Veth RPH, Kingma LM, Nielson HKL (1984) The abnormal proximal tibiofibular joint. Arch Orthop Trauma Surg 102:167–171
Weeks C (1930) Occasional communications between the synovial sacs of knee and proximal tibiofibular joints. Am J Surg 4:798–800
Acknowledgments
The authors express their extreme gratitude to Serviço de Anatomia Patológica do HGSA-Porto (Dr. Isabel Calhim) for histological preparation and evaluation; Instituto de Medicina Legal do Porto for providing the cadavers for dissection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Espregueira-Mendes, J.D., Vieira da Silva, M. Anatomy of the proximal tibiofibular joint. Knee Surg Sports Traumatol Arthrosc 14, 241–249 (2006). https://doi.org/10.1007/s00167-005-0684-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-005-0684-z