Abstract
Purpose
The proximal tibiofibular joint (PTFJ) is a rather unknown articulation. There is little understanding of its anatomy, physiology, and functional role. The objectives of this research are to describe the normal kinematics of the PTFJ and its relation to the ankle and knee movements.
Methods
Fourteen knees of seven adult fresh frozen whole body cadavers were studied. The proximal tibiofibular joint and ligaments were identified, after which we sequentially sectioned the anterior proximal tibiofibular ligament (APTFL), the posterior proximal tibiofibular ligament (PPTFL), and the interosseous syndesmotic membrane. Models with intact and sectioned ligaments were compared, while the unloaded lower limb was manually mobilized in a pre-defined sequence of combined movements of knee, ankle, and proximal tibiofibular joints. The PTFJ spatial displacement was measured by analyzing the length of a distance vector between two 3D coordinate systems settled over the tibia and fibula.
Results
On the unaltered PTFJ, direct grasping of the head of the fibula with the hip in 45° of flexion and the knee in 90° of flexion was found to produce an average displacement of 7 mm. Knee movements caused the greatest spatial displacements, almost ten times the ones produced by ankle flexion/extension. Flexion/extension of the knee caused 1.8 times more displacement than single rotations with the knee flexed to 90°. It was found that the APTFL was an important stabilizer of the PTFJ when this joint is tensioned accommodating the movements of ankle extension and foot eversion. The APTFL was not a significant stabilizer of the PTFJ during direct manipulation of the fibular head when imprinting a manual force with posterior direction. The PPTFL was an important accommodator of ankle flexion, foot inversion and knee flexion. The interosseous syndesmotic membrane also proved to be a significant PTFJ stabilizer in rotational movements of the ankle and knee.
Conclusions
This is the first cadaver study to illustrate the PTFJ normal spatial displacement, thereby contributing to a deeper insight of this joint. The contribution of each ligament for PTFJ stability was described and, based on these findings; a new mechanism of injury was suggested. Surgeons can translate the results of this study into the clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The proximal tibiofibular joint (PTFJ) is a rather unknown articulation. There is little understanding of its anatomy, physiology and functional role. It is the subject of only a few publications, seldom discussed in the literature as the cause of knee dysfunctions [8].
Most of the published literature on this field emphasizes the variability of this joint’s anatomy across individuals. PTFJ is described as an arthrodial joint surrounded by a fibrous capsule and two prominent ligaments, the anterior proximal tibiofibular ligament (APTFL) and the posterior proximal tibiofibular ligament (PPTFL). The anterior ligament is described in the literature as thicker and stronger, consisting of three bands, while the posterior ligament is a single broad band [1, 11, 12].
Barnett and Napier were the first to describe the PTFJ using four variables: (1) inclination angle; (2) articular surface area; (3) concavity; and (4) articular surface shape [2]. Later, Ogden developed a simpler classification that is currently the most widely used and arbitrarily classifies the articulations with less than 20° as horizontal and those with more than 20° as oblique [14,15,16].
On other attempts to further characterize the PTFJ Eichenblat and Nathan developed a morphological classification of the PTFJ with seven categories finding the plane joint to be more frequent [6].
Conflicting evidence was found by Espregueira-Mendes in a series of 20 specimens, with a majority (17) of oblique joints, 70% of which classified as trochoid according to its morphology [7].
The anatomical variants are believed to explain different biomechanical behaviors and to be implicated in both physiologic and pathologic movements. Barnett and Napier effectively demonstrated an association of the horizontal morphology with more rotational mobility [2].
Likewise, Ogden has shown that oblique joints have smaller articular surface areas decreasing mobility and reducing the joint’s ability to accommodate torsional forces. In contrast, the horizontal joints enable greater flexibility and are, therefore, less prone to injury [14,15,16].
Considering the biomechanical behavior, Ogden understood the PTFJ as an “accomodatory joint” with three primary functions (1) dissipation of torsional forces applied to the ankle, (2) dissipation of lateral tibial bending moments, and (3) tensile, rather than compressive weight bearing [14,15,16]. Naturally, movements of the knee and ankle will lead to the movements of the PTFJ in multiple planes. When the ankle is dorsiflexed, the fibula must externally rotate to accommodate the rotation of the talus and the changing of the inclination of the dorsiflexion axis [2]. Likewise, when the knee moves from flexion to extension the fibular head is pulled to posterior as the biceps femoris and lateral collateral ligament become taut.
This is consistent to Ogdens’s proposed mechanism of injury in which a sudden inversion and plantar flexion of the foot with simultaneous flexion of the knee and concomitant twisting of the body would cause a relative external rotation torque of the tibia, pulling the PTFJ laterally and forward [17].
Although most authors agree on that the fibula rotates along its longitudinal axis during ankle and knee movements [10, 19], recent studies have show that both internal and external rotations are possible depending on the anatomy of the specimens studied [3].
In this complex and little understood kinematics, we must consider a secondary component of the PTFJ, the interosseous syndesmotic membrane (IOSM) that spans the space between the tibia and fibula [4]. This ligamentous structure consists of differently oriented fibers providing a rigid support between the two bones, acting as a stabilizer of the PTFJ. It has been reported that the IOSM is capable of withstanding different tensile forces depending on the direction of the applied load, 164 N if the load is perpendicular and 3604 N if the load is parallel to the direction of the main fiber bundles [13]. Identical to the PTFJ, there is still incomplete knowledge regarding the function of the IOSM.
A thorough understanding of the behavior of these structures is important when evaluating both the physiology and pathology of specific knee injuries. Of particular interest is the clinical condition of proximal tibiofibular instability which is so often under recognized and seems to be a possible cause of chronic lateral knee pain in athletes [5, 9, 17, 18].
Acknowledging all, to study the mobility of the PTFJ, a 3D kinematic analysis must be considered. Therefore, this study aimed to analyze the 3D displacement of the PTFJ in whole fresh frozen cadaver specimens by measuring the total spatial displacement of the head of the fibula in relation to the tibia for each foot, ankle, and knee position to evaluate the hypothesis that PTFJ mobility was influenced by adjacent joints position and its ligaments integrity.
A deeper insight of the PTFJ normal kinematics will hopefully help clinicians understand its pathology and plan successful treatments.
Materials and methods
Seven adult fresh frozen whole-body cadavers were studied, 14 knees from 3 men and 4 women, with ages between 62 and 83 years old, and a median height of 161 cm.
Each specimen was positioned in supine on a non-metallic table during the entire study.
The knee and leg were dissected. A lateral approach was used and the iliotibial band was reflected anteriorly. It preserved the biceps femoris tendon, lateral collateral ligament, and popliteus tendon insertions on the fibular head. The proximal tibiofibular joint and ligaments were identified and the injury was sequentially created by sectioning the anterior proximal tibiofibular ligament (APTFL), the posterior proximal tibiofibular ligament (PPTFL), and the interosseous syndesmotic membrane (IOSM) until the superior border of the distal tibiofibular transverse ligament. Following experimental testing, the tibia and fibula were disarticulated exposing the articular surfaces to enable macroscopic inspection and anatomic classification.
To enable the measurement of the relative position and orientation of the studied segments bony landmarks, 3D coordinates were measured on the skin with feet hip-width apart using an electromagnetic system trakSTAR with a reported static accuracy of 0.5° and 1.8 mm (Ascension Technology, Burlington, Vermont) and the Motion Monitor software (Innovative Sports Training, Chicago, IL).
Bony landmarks 3D coordinates were measured with an acrylic-digitizing stylus. Its tip offsets were calculated using a custom calibration grid, obtaining a root-mean-square error of less than 1 mm. The choice of bony landmarks and segments’ local coordinate systems definition was based on the recommendations of the International Society of Biomechanics [20].
Then, six electromagnetic sensors were rigidly fixed through 2 mm-diameter transcortical pins to the pelvic anterior–superior iliac spine, patella center, femoral lateral epicondyle, tibial crest, fibular head, and lateral calcaneus by the same team of two experienced orthopedic surgeons.
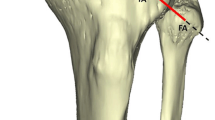
The lower limb was manually mobilized according to an established sequence of movements of knee, ankle and proximal tibiofibular joints. Table 1 describes the relative orientation of the joints and the sequence of movements produced, as illustrated in Fig. 1.
The passive motion of the lower limb was repeated and registered for four different conditions:
-
1.
Intact lower limb.
-
2.
After anterior proximal tibiofibular ligament section.
-
3.
After posterior proximal tibiofibular ligament section.
-
4.
After interosseous syndesmotic membrane section.
Each mobilization was repeated for four trials exploring full ROM (Fig. 2). During each range of motion (ROM) tested, the Motion Monitor 3D kinematic biofeedback was used to ensure that the tasks were performed in the expected joint angles.
Kinematic reconstruction. Up: the image shows the six 3D coordinate systems created and the spatial dislocation between them for a particular joint movement. At bottom: graphic representation of a range of motion, showing the maximal displacement of the fibular head in relation to the tibia during two repetitions of a range of motion (x/y—time/distance)
The fibula and tibia motions were tracked. The systems used enabled us to track the six synchronized sensors with a sampling rate of 100 Hz per sensor.
Three-dimensional angular rotations as sequential rotations about each of the three anatomical axes were described using Euler angles throughout the passive joint movements, as described in Table 1 [20]. The latter angles allowed us to define the two exact time frames in which each pair of applied movements (e.g., ankle flexion and ankle extension) reached the maximum joint angles in the respective joint. PTFJ displacement was defined as the Euclidean length of the distance vector between the fibula head bony landmark 3D coordinates and the tibia coordinate system in each time frame.
Approval was obtained from the Institutional Review Board of Universidade Nova de Lisboa—Faculdade de Ciências Médicas (IRB 3112013) prior to initiation of this study.
Statistical analysis
Statistical analysis was conducted using SPSS Statistics version 20.0 and statistical significance was accepted at p < 0.05. The limited sample size determined the use of non-parametric tests. The studied variables were evaluated using the Wilcoxon test for matched samples and the Kruskal–Wallis test for independent samples.
Results
Anatomically, 12 of the joints were plane and 2 were trochoid. All were classifiable as oblique according to the classification of Ogden, evaluating the inclination of the articular surface. No macroscopic signs for osteoarthritic changes were found in any of the PTFJ evaluated.
Results are summarized in Table 2. The presented values represent multiplanar spatial deviation between two coordinate systems. The values are expressed in length (mm) of the distance vectors between the 3D coordinate system of the fibular head and the 3D coordinate system of the tibia and quantify 3D mobility for every movement tested.
Intact PTFJ
It is worth noting that knee flexion and extension and knee rotations were responsible for the highest average PTFJ spatial displacements. Foot inversion and eversion produced wider displacements than ankle flexion or extension on average.
The manipulation of the PTFJ with manual force imprinted in the posterior direction caused an average spatial mobility identical to the one obtained by the opposite movement in anterior direction.
Post APTFL section
The section of the APTFL produced a significant increase of tibiofibular mobility for the movements of ankle extension (p < 0.05), foot eversion (p < 0.05), knee internal, and external rotations (p < 0.01).
Interestingly, during knee extension, the tibiofibular mobility with the APTFL sectioned was significantly inferior (mean 37.7 mm, SD 24.6 mm) (p < 0.05).
We did not, moreover, find the section of the APTFL to cause significant difference in the tibiofibular motion when a manual force was imprinted over the fibular head on the anterior or posterior directions.
Post APTFL + PPTFL section
The cumulative section of the APTFL and PPTFL accounted for a significant increase in the tibiofibular motion as compared to the intact state for the movements of ankle extension, ankle flexion, knee internal and external rotations (p < 0.05, p < 0.05, p < 0.01, p < 0.01, respectively).
With both APTFL and PPTFL separated, foot eversion and foot inversion did no longer significantly change the tibiofibular motion and the same was for knee flexion and extension.
In this condition of both APTFL and PPTFL separated, fibular head manual manipulation in both anterior and posterior directions, caused a significant increase in the tibiofibular mobility (p < 0.01).
Post APTFL + PPTFL + IOSM section
When the IOSM lesion was associated with both APTFL and PPTFL, ankle flexion did not produce a significant change in tibiofibular motion.
On the contrary, foot eversion and foot inversion could now produce a significantly increased tibiofibular displacement (p < 0.05).
Knee flexion and extension did not produce significantly different mobility but knee internal rotation and knee external rotation maintained the ability to further increase significantly the 3D tibiofibular spatial displacement (p < 0.05).
The cumulative lesion of the IOSM increased significantly the tibiofibular motion elicited by manual manipulation of the fibular head that reached in this condition average values of 31.2 mm (SD ± 42.7) (force applied posteriorly) and 30.6 mm (SD ± 42.0) (force applied anteriorly) (p < 0.01).
Discussion
The most important finding of the present study was the characterization of the 3D displacement of the PTFJ when manual mobilizing the unloaded inferior limb, which unveiled the contribution of each ligament structure to the stability of the PTFJ and the influence of each knee, ankle and foot movement over the mobility of this joint.
All included PTFJ were found to be oblique of which 12 were classified as plane and 2 as trochoid. This is in accordance with the literature considering the Ogden classification but more apart in terms of the morphological type. This can be explained by the small sample size and possible inter-observer variability.
Analyzing the 3D displacement of the fibular head in relation to the tibia, we found interesting data. In the intact PTFJ, knee flexion/extension caused almost ten times more joint mobility than ankle flexion/extension. Flexion/extension of the knee caused 1.8 times more displacement than single rotations with the knee flexed to 90°. In addition, with the knee at 90° of flexion, it was found that a displacement of 7.7 mm on average could be reproduced by manual manipulation of the head of the fibula.
We also could observe that the APTFL is an important stabilizer of the PTFJ when this joint is tensioned accommodating the movements of ankle extension and foot eversion. It also plays a significant role in stabilizing the joint during knee internal and external rotations.
Interestingly, the APTFJ ligament did not appear to be a significant stabilizer of the PTFJ when this is subject to application of a manual posteriorly directed force. This finding was previously unknown. It is useful to compare it with published literature that describes the APTFL complex as stronger and with more ligamentous area than the PPTFL complex [12]. Probably this finding reflects that isolated injury of the APTFL is not sufficient to alter the kinematics in the presence of the other stabilizers integrity.
Most of the understanding of the PTFJ lesions is based on the descriptions of case reports and the extrapolated data of anatomic and biomechanical studies.
Ogden described the mechanism of lesion of the PTFJ as the result of a sudden inversion and plantar flexion of the foot, with simultaneous flexion of the knee and concomitant twisting of the limb, causing a relative external rotatory torque of the tibia on the foot which is already fixed in inversion [14,15,16].
Based in the present analysis of tibiofibular 3D displacement, Ogden’s theory is suggested to be consistent with the lesion mechanism of the PPTFL. In fact, the movements of ankle flexion, foot inversion and knee flexion do not significantly change the tibiofibular displacement when the PPTFL is intact. After its injury, however, these movements are shown to produce significant change.
On the other hand, the mechanism of injury of the APTFJ is proposed to be a different one.
The ankle extension and foot eversion are the movements restrained by the APTFL, according to the data found.
Moreover, when APTFL is sectioned, knee extension causes less overall 3D displacement of the PTFJ comparing to the intact joint. This suggests that in the intact joint, full extension of the knee fully recruits the APTFL producing maximal excursion of the joint.
Therefore, when knee extension occurs simultaneously with forced ankle extension and foot eversion what occurs is recruitment of the PTFJ, maximal tensioning of the restraining APTFL and eventually injury. This could then be considered as a possible lesion mechanism of the anterior ligament complex, in a movement similar to the reception of a soccer ball and ball control, the opposite of that described by Ogden.
Another important finding of this study accounts for the rotation stability of the PTFJ. We found that both APTFL and PPTFL are important stabilizers of rotation with the knee flexed at 90°, when biceps femoris and lateral collateral ligaments are relaxed. The IOSM also proved to be a significant stabilizer of the PTFJ during rotational movements of the ankle and knee, which is a new finding.
This current study has some limitations. The lesions were modeled as progressively cumulative. Therefore, with this study design, we could not evaluate the contribution of each single lesion for the results attained. However, we could characterize the normal displacement of the PTFJ and evaluate the significance of the progressive instability.
Other limitation of this study is that the limb was not loaded during the experiments and we might speculate that this condition could have unveiled other aspects of the behavior of the PTFJ. More biomechanical studies are needed that can explore the effect of axial loading over this joint mobility and its clinical relevance.
Finally, there is a limit to the clinical extrapolation of the experimental cadaver studies. Additional in vivo instrumented trials are needed to evaluate the clinical aspects of patients suffering PTFJ lesions.
Despite this, to the best of the authors’ knowledge this is the first cadaver study to unveil the PTFJ normal 3D displacement, and evaluate the effect of conjoined lower limb joint movements over PTFJ spatial behavior.
A deeper knowledge of these joint will help the clinician focus in injury evaluation when managing PTFJ instability. In particular, knowing the contribution of each ligament structure and understanding the injury pattern will be useful when considering a repair of PTFJ.
Conclusion
The PTFJ behaves as an accommodation joint with a mobility pattern closely determined by the mobility of the adjacent knee and ankle joints. The APTFL stabilizes the joint when it is subject to movements of ankle extension and foot eversion and the PPTFL act as stabilizer when the joint is tensioned by ankle flexion, foot inversion and knee flexion.
Both ligaments as well as the interosseous syndesmotic membrane play a significant role in rotational stability of this joint.
Abbreviations
- PTFJ:
-
Proximal tibiofibular joint
- Distal TFJ:
-
Distal tibiofibular joint
- APTFL:
-
Anterior proximal tibiofibular ligament
- PPTFL:
-
Posterior proximal tibiofibular ligament
- IOSM:
-
Interosseous syndesmotic membrane
- ROM:
-
Range of motion
References
Anavian J, Marchetti DC, Moatshe G, Slette EL, Chahla J, Brady AW, Civitarese DM, LaPrade RF (2018) The forgotten joint: quantifying the anatomy of the proximal tibiofibular joint. Knee Surg Sports Traumatol Arthrosc 26:1096–1103
Barnett H, Napier JR (1952) The axis of rotation at the ankle joint in man; its influence upon the form of the talus and the mobility of the fibula. J Anat 86:1–9
Bozkurt M, Tonuk E, Elhan A, Tekdemir I, Doral MN (2008) Axial rotation and mediolateral translation of the fibula during passive plantarflexion. Foot Ankle Int 29:502–507
Burkhart TA, Asa B, Payne MWC, Johnson M, Dunning CE, Wilson TD (2015) Anatomy of the proximal tibiofibular joint and interosseous membrane, and their contributions to joint kinematics in below-knee amputations. J Anat 226:143–149
Cazeneuve JF, Bracq H, Meeseman M (1997) Weinert and Giachino ligament arthroplasty for the surgical treatment of chronic superior tibiofibular joint instability. Knee Surg Sports Traumatol Arthrosc 5:36–37
Eichenblat M, Nathan H (1983) The proximal tibio fibular joint. An anatomical study with clinical and pathological considerations. Int Orthop 7:31–39
Espregueira-Mendes JD, Vieira Da Silva M (2006) Anatomy of the proximal tibiofibular joint. Knee Surg Sports Traumatol Arthrosc 14:241–249
Horst PK, LaPrade RF (2010) Anatomic reconstruction of chronic symptomatic anterolateral proximal tibiofibular joint instability. Knee Surg Sports Traumatol Arthrosc 18:1452–1455
Jabara M, Bradley J, Merrick M (2014) Is stability of the proximal tibiofibular joint important in the multiligament-injured knee? Clin Orthop Relat Res 472:2691–2697
Lambert KL (1971) The weight-bearing function of the fibula. A strain gauge study. J Bone Jt Surg Am 53:507–513
Marchetti DC, Chahla J, Moatshe G, Slette EL, LaPrade RF (2018) Quantitative radiographic assessment of the anatomic attachment sites of the anterior and posterior complexes of the proximal tibiofibular joint. Knee Surg Sports Traumatol Arthrosc 26:1104–1109
Marchetti DC, Moatshe G, Phelps BM, Dahl KD, Ferrari MB, Chahla J, Turnbull TL, LaPrade RF (2017) The proximal tibiofibular joint: a biomechanical analysis of the anterior and posterior ligamentous complexes. Am J Sports Med 45:1888–1892
Minns RJ, Hunter JA (1976) The mechanical and structural characteristics of the tibio-fibular interosseous membrane. Acta Orthop Scand 47:236–240
Ogden JA (1974) Subluxation and dislocation of the proximal tibiofibular joint. J Bone Jt Surg Am 56:145–154
Ogden JA (1974) The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res 101:186–191
Ogden JA (1974) Subluxation of the proximal tibiofibular joint. Clin Orthop Relat Res 101:192–197
Semonian RH, Denlinger PM, Duggan RJ (1995) Proximal tibiofibular subluxation relationship to lateral knee pain: a review of proximal tibiofibular joint pathologies. J Orthop Sports Phys Ther 21:248–257
Sijbrandij S (1978) Instability of the proximal tibio-fibular joint. Acta Orthop Scand 49:621–626
Soavi R, Girolami M, Loreti I, Bragonzoni L, Monti C, Visani A, Marcacci M (2000) The mobility of the proximal tibio-fibular joint. A roentgen stereophotogrammetric analysis on six cadaver specimens. Foot Ankle Int 21:336–342
Wu G, Siegler S, Allard P, Kirtley C, Leardini A, Rosenbaum D, Whittle M, D’Lima DD, Cristofolini L, Witte H, Schmid O, Stokes I (2002) ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—part I: ankle, hip, and spine. Int Soc Biomech J Biomech 35:543–548
Acknowledgements
We thank Professor João Goyri O’Neil and the Department of Anatomy of Medical College, Universidade Nova de Lisboa for provision of the specimens and assistance with laboratory setup. We thank Escola Superior de Saúde, Instituto Politécnico de Setúbal for providing the hardware and software for the 3D kinematic analysis. We thank Physiotherapist Mario Valerio and PhD Candidate Rodrigo Brandão Martins for providing support during data collection and analysis.
Funding
No funding has been received for this study.
Author information
Authors and Affiliations
Contributions
TAS, PP, and FGP conceived the study, participated in its design and coordination, carried out the experimental study, participated in the sequence alignment, and drafted the manuscript. RM participated in the study design and data analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests with respect to the research, authorship and publication of this article. The authors received no financial support for the research, authorship and publication of this article.
Ethical approval
This article does not contain any studies with living human participants performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Alves-da-Silva, T., Guerra-Pinto, F., Matias, R. et al. Kinematics of the proximal tibiofibular joint is influenced by ligament integrity, knee and ankle mobility: an exploratory cadaver study. Knee Surg Sports Traumatol Arthrosc 27, 405–411 (2019). https://doi.org/10.1007/s00167-018-5070-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5070-8