Abstract
Intraarticular ganglion cyst arising from the cruciate ligament is difficult to diagnose by clinical symptom. In our case, Cyst attached anteriorly to posterior cruciate ligament, and limited both flexion and extension of knee. The cyst was excised in a piecemeal fashion arthroscopically. Knee pain and limitation in knee motion disappeared by the day after surgery. We hypothesize that reason of restriction of extension is impingement between anterior cruciate ligament and intracondylar, and reason of restriction of flexion is stimulation nerve ending in the synovial membrane stretched with knee motion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ganglion cysts within the cavity of the knee joint are rare and their findings are uncommon, but not as rare as commonly thought. Reported prevalence of intraarticular ganglion in the knee is 0.2–1% on knee magnetic resonance imaging (MRI) and 0.6% on knee arthroscopy [3]. Even though meniscal degenerative cysts are commonly found, there are only a few case reports of ganglion cysts occurring from posterior cruciate ligament (PCL). They may be asymptomatic, but can cause considerable morbidity usually presenting with pain or mechanical symptoms. The mainstay of treatment for ganglion for the knee has been surgical, by open or arthroscopic excision. We report a case of knee locking caused by ganglion cyst of the PCL treated with arthroscopy.
Case report
A 49-year-old man presented with left knee pain that worsened over a 4-month period. He indicated a worsening of the pain on knee extension, Japanese sitting and gait. There was no history of a specific traumatic event to the knee. Physical examination showed no knee effusion, quadriceps atrophy and joint line tenderness. Range of motion was between 20 and 140°. The results of Lachman’s, anterior drawer, pivot shift and posterior drawer tests were normal. McMurray’s test caused pain but no click. Pain was reproduced on forced knee extension.
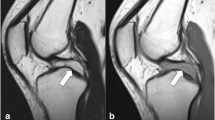
Radiographs showed no bony or soft tissue abnormality, including intraarticular loose bodies. The MRI revealed an oval well-demarcated cystic mass, 15×15×24 mm3 in dimension, anteriorly to the proximal third of the PCL, and the ligament was deformed flatly due to the mass. The mass was manifested by low signal intensity on T-1-weighted images (Fig. 1a) with uniform high signal intensity on T-2-weighted images (Fig. 1b).
Arthroscopic examination identified the mass anteriorly to the proximal third of the PCL. The cyst located between ACL and PCL (Fig. 2). It was tightly attached to the PCL and could not be separated by probing. The cyst was excised in a piecemeal fashion arthroscopically.
Histologic examination confirmed the diagnosis of intraarticular ganglion cyst. Knee pain and limitation in knee motion disappeared by the day after surgery. The patient was asymptomatic with a full range of motion for 10 months postoperatively.
Discussion
A ganglion can arise as a cystic lesion from a tendon sheath or a joint capsule and contain a glassy, clear and jelly-like fluid. Although the dorsum of the wrist and the palm of the hand are the common location, ganglion cysts from the cruciate ligament were very rarely encountered, but not as rare as commonly thought. Since the description of an ACL ganglion by Caan [4] during a routine autopsy in 1924, only a few sporadic, and mainly one, case reports on intraarticular soft tissue knee masses could be found in the literature [1, 2, 12, 13, 18]. But within the increasingly popular and widespread use of MRI and arthroscopy in daily practice, an increasing number of reports on these particular findings have been published. The prevalence of intraarticular cystic knee masses, mostly as incidental findings, is reported up to 1.3% through MRI and 0.6% through arthroscopy [3, 14, 15]. Brown and Dandy [4] reported that of 35 ganglion cysts arising from the cruciate ligament in 6,500 arthroscopic examinations of the knee over a period of 13 years, only 6 arose from the PCL. In a study by Krudwing et al. [11], during a period of 15 years, nearly 8,000 knees were arthoroscopically examined. In total, 85 ganglions were found within the knee cavity. Sixteen ganglion cysts originated from the PCL, 49 from the ACL. As far as we have determined, of 65 ganglion cysts arising from the PCL that have been reported in the literature written in English, 16 have been reported in detail [5, 6, 8, 9, 11, 14].
The pathogenesis of ganglions still remains unknown [16]. Currently, there are several hypotheses; one presumes that the presence of the ganglion is a product of mucinous degeneration of the connective tissue [9]. The second hypothesis considers the cause to be herniation of the synovial tissue through a defect in the joint capsule or tendon sheath, similar to those originating in the wrist joint. Other theories are connective tissue degeneration after trauma, ectopia of synovial, proliferation of pluripotential mesenchymal stem cell [3, 5, 16]. In our patient, there was no past history of trauma to the knee.
The symptoms and signs of a ganglion cyst included pain, swelling, joint line tenderness, a positive result of the McMurray’s sign and limitations in the range of motion. These can also be suggestive of other intraarticular lesion, such as meniscal tear, a cartilage lesion or a free body, although the limitation in the range of knee motion is relatively greater than with other lesions. Knee locking seemed to be influenced by the location of the cyst. Cysts located mainly anterior to the cruciate ligaments tended to limit to extension of the knee, whereas those located mainly posterior to cruciate ligaments tended to limit to flexion. Sumen [17] reported that the reason for this tendency is that a cyst located anterioly could have been impinged between the ACL and intracondylar roof, resulting extension block, whereas a cyst located posterior to the ligaments could have been impinged between the PCL and intracondylar roof, resulting in a flexion block. However, this case located anterior to PCL limited both flexion and extension. The limitation cannot be completely explained by the location of the cyst only. Sumen [17] reported that the changes in the length and torsion of cruciate ligaments with knee motion might provoke traction or compression on the cyst, which may offer another explanation for limitations in knee motion. Kim [10] suggested that the changes in the shape and dimension of the ganglion cyst with knee motion and posture stimulated nerve ending in the synovial membrane stretched, and the knee pain was developed and knee motion limitation flexion and extension. Girgis [7] reported that the anterior portion of PCL was stretched in flexion position. Ganglion cyst attached anterior to PCL such as this case is stretched on knee flexion, knee motion limited in flexion. We hypothesize that reason of restriction of extension is impingement between ACL and intracondylar, and the reason of restriction of flexion is stimulation nerve ending in the synovial membrane stretched with knee motion.
References
Bromley JW, Cohen P (1965) Ganglion of the posterior cruciate ligament. Report of a case. J Bone Joint Surg Am 47:1247–1249
Brown MF, Dandy DJ (1990) Intra-articular ganglia in the knee. Arthroscopy 6:322–323
Bui-Mansfield LT, Youngberg RA (1997) Intraarticular ganglion of the knee: prevalence, presentation, etiology and management. AJR Am J Radial 168:123–127
Caan P (1924) Cyst formation (ganglion) in the anterior cruciate ligamnet of the knee (Zystenblidung (Ganglion) im Ligamentum cruciatum ant. Genus). Dtsch Z Chir 186:403–408
Deutsch A, Veltri DM, Altchek DW (1994) Symptomatic intraarticular ganglia of the cruciate ligaments of the knee. Arthroscopy 10:219–223
Garcia A, Hodler J, Vaughn L (1991) Case report 677: intraarticular ganglion arising from the posterior cruciate-ligament. Skeletal Radiol 20:373–375
Girgis FG, Marchall JL, Monajem ARS (1975) The cruciate ligaments of the knee joint : anatomical, functional and experimental analysis. Clin Orthop 106:216–231
Kaempffe F, D’Amato C (1989) An unusual intra-articular ganglion of the knee with interosseous extension: a case report. J Bone Joint Surg Am 71:773–775
Kang CN, Kim DW, Kim DJ, Kim SJ (1999) Intra-articular ganglion cysts of the knee. Arthroscopy 15:373–378
Kim RS, Kim KT, Lee JY, Lee KY (2003) Ganglion cysts of the posterior cruciate ligament. Arthroscopy 19:36–40
Krudwig WK, Schulte KK, Heinemann C (2004) Intra-articular ganglion cysts of the knee joint: a report of 85 cases and review of the literature. Knee Surg Sports Traumatol Arthrosc 2:123–129
McLaren DB, Buckwalter KA, Vahey TN (1992) The prevalence and significance of cyst-like changes at the cruciate ligament attachments in the knee. Skeletal Radiol 21:365–369
Muckle DS, Monahan P (1972) Intra-articular ganglion of the knee; report of two cases. J Bone Joint Surg Br 54:520
Nokes SR, Koonce TW, Montanez J (1994) Ganglion cysts of the cruciate ligaments of the knee; recognition on MR images and CT-guided aspiration. AJR Am J Roentgenol 162:1503
Pawlas R, Szlachta Z (1994) Arthroscopic diagnostics and treatment for cysts of the anterior cruciate ligament. Chir Narzadow Ruchu Ortop Pol 59:227–230
Recht MP, Applegate G, Kaplan P, Dussault R, Schweitzer M, Dalinka MK, Resnick D (1994) The MR appearance of cruciate ganglion cysts; a report of 16 cases. Skeletal Radiol 23:597–600
Sumen Y, Ochi M, Deie D, Adachi N, Ikuta Y (1999) Int Orthop (SICOT) 23:58–60
Yasuda K, Majima T (1988) Intra-articular ganglion blocking extension of the knee: brief report. J Bone Joint Surg Br 70:837
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seki, K., Mine, T., Tanaka, H. et al. Locked knee caused by intraarticular ganglion. Knee Surg Sports Traumatol Arthr 14, 859–861 (2006). https://doi.org/10.1007/s00167-005-0017-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-005-0017-2