Abstract
Extra- and intraneural ganglion cysts have been described in the literature. The tibial nerve ganglion is uncommon and its occurrence without intra-articular extension is atypical. The pathogenesis of cystic degeneration localized to connective and perineural tissue secondary to chronic mechanical irritation or idiopathic mucoid degeneration is hypothesized. Since the above pathology is extremely rare and the magnetic resonance imaging examination detects the defining characteristics of the intrinsic alterations of the tibial nerve, the authors illustrate such a case of tibial intaneural ganglion cyst with its magnetic resonance neurography and sonography appearances.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Peripheral nerve injuries are common conditions with broad-ranging groups of symptoms depending on the severity and nerves involved. Tibial nerve pathologies can be caused by a variety of insults including penetrating injury, indirect trauma, and metabolic conditions, such as diabetes mellitus [1].
Intraneural cysts are uncommon lesions of the peripheral nerves that are usually found in adults and are caused by an accumulation of thick mucinous fluid encased in a dense fibrous capsule within the nerve epineurium. These cysts cause intermittent compression of adjacent nerve fascicles, resulting in pain, paresthesia, weakness, muscle denervation and atrophy [2, 3]. These cysts are believed to be retrograde extensions of synovial fluid along the path of the intra-articular branches of adjoining major nerves, such as those seen in suprascapular or common peroneal nerves [5]. Tibial nerve entrapment or injury in the calf is rare, and the nerve is most commonly affected impinged in the tarsal tunnel because of space-occupying lesions. Soleal sling syndrome has been shown to be a cause of tibial nerve entrapment in the proximal calf [6]. Tibial intraneural ganglion is quite uncommon [4]. Furthermore, isolated cystic degeneration without intra-articular extension is extremely rare. Cross-sectional imaging including magnetic resonance imaging and its modification, magnetic resonance neurography (MRN), as well as sonography aid in narrowing the list of differential diagnoses of tibial nerve pathology. MR neurography in part due to high resolution and contrast capabilities can delineate the extent of the lesion and its relationship to the adjacent neurovascular structures, and it identifies early muscle denervation changes. The authors present a rare case of isolated extra-articular intraneural cyst of the tibial nerve with illustration of the magnetic resonance neurography and sonography appearances.
Case Report
A 51-year-old male consulted with an orthopedist because of the presence of continuous paresthesia of left ankle, foot and all toes for almost 6 months. No pain, local inflammatory changes, or structural deformity was present. The patient denied trauma in the recent months or motor dysfunction. On physical examination, inspection and palpation were unremarkable, with preserved Achilles and patellar reflexes and only mild to moderate ankle sensitivity. Electromyography (EMG) showed signs of a lateral plantar nerve lesion. Magnetic resonance neurography (MRN) of the left ankle was then requested with a clinical suspicion of tarsal tunnel syndrome. Doppler ultrasonography of the leg and ankle was also performed.
A high-field device (Philips Achieva 3.0-T X-series MRI System; Philips Medical Systems, Best, The Netherlands) was used for the leg and ankle MRN using ankle- and leg-specific coils (Sense foot-ankle coil and Sense XL-torso coil) with the following protocol: axial fast spin echo (FSE) T1-weighted imaging, three-dimensional (3D) volumetric T1-weighted imaging, spectral adiabatic inversion recovery (SPAIR) T2-weighted imaging, 3D volumetric short tau inversion recovery (STIR) imaging, 3D diffusion-weighted imaging (DWI), and 3D fat saturated (Fat-sat) T1-weighted sequences both without contrast and after intravenous gadolinium injection. The images were post-processed at a workstation, and multiplanar reconstructions (MPRs) were generated using the thick-slab maximum intensity projection (MIP) technique.
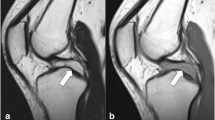
An elongated mass with a cystic appearance was observed, with similar signal intensity to the fluid on 2D T1-weighted, T2-weighted, SPAIR and 3D STIR sequences, without enhancement on post-gadolinium imaging (Fig. 1). The mass had thin and regular walls with no internal blood products, contiguous to the tibial nerve from the mid- and distal one-third of the leg to the ankle, terminating immediately before the emergence of the medial and lateral plantar branches; the latter were not affected by the cystic mass. The lesion measured approximately 20.0 × 1.3 × 1.3 cm (longitudinal × transverse × anteroposterior) and did not cause significant compression of adjacent vascular structures. There was posterior displacement of the fascicles with increased signal on T2W images. Discrete edema and fatty degeneration of the flexor hallucis longus muscle was apparent at the ankle level, characterizing denervation.
a, b 3D STIR sagittal and coronal reconstructions of the leg, where an elongated mass is identified with similar signal intensity to the fluid in the mid- and distal third of the left leg tibial nerve (arrowheads); c axial STIR image of the ankle, demonstrating a intraneural cystic lesion displacing the hyperintense fascicles posteriorly at this level (short arrow) and denervation of the flexor hallucis longus muscle (long arrow); d 3D DWI (b = 800s/mm²) with MIP reconstruction shows the hyperintense cystic lesion (orange color coded) with excellent background fat, vessel and muscle signal suppression
Ultrasound examination was performed using a 12-MHz linear frequency probe (Philips HD 7. XE, Nesoft Park, Hun Nan Industrial Area, Shenyang), which identified an anechoic, cystic, elongated lesion with no color or pulse Doppler flow, located in the mid-posterior third of the left leg (Fig. 2). The fascicles were displaced along the periphery of the lesion on cross-sectional view; however, MRN resulted in superior depiction of the fascicles because of better soft tissue contrast.
a,b Cross-sectional and longitudinal images showing an anechoic lesion in the distal third of the posterior tibial nerve, with no flow on color Doppler; c longitudinal section showing the anechoic ganglion cyst with peripheral anteriorly displaced fascicles in the distal third of the posterior tibial nerve
The patient did not undergo surgical treatment and, because of the benignity of the lesion, chose to undergo conservative management. In the 1-year follow-up period, the patient continued to experience symptoms of paresthesia with no change in the symptom intensity.
Discussion
Peripheral nerves are composed of axons, Schwann cells, and connective tissue. The axons are arranged in parallel bundles, known as fascicles, wrapped by loose connective tissue. The tissue that surrounds each individual axon is known as the endoneurium. The fascicles are surrounded by a multilayered sheath of flattened cells, known as the perineurium. The epineurium represents the outermost fibrous layer that covers the entire nerve trunk. Axons are electrically isolated by the endoneurium itself and by a lipoprotein complex called the myelin sheath, which is produced by Schwann cells [7] (Fig. 3).
The peripheral nerve may contain various combinations of motor and sensory fibers. Sensory manifestations of neuropathy include hypoesthesia, hypoalgesia, paresthesia, hyperalgesia, and a prickling or tingling sensation. In the setting of entrapment neuropathies, the sensory fibers are usually the first to become compromised as was noted in our case where patients presented with paresthesia. The symptoms of motor neuropathy usually include muscle spasm, clonus, fasciculations, amyotrophy, and loss of dexterity or muscle strength [8]. Muscle denervation change in this case was also confirmed on MRN.
Peripheral nerve lesions can be caused by direct trauma (crush or transection), traction, mechanical or functional compression, or repetitive local friction [9]. Intra- or extraneural ganglion cyst is a rare cause of entrapment [3, 6]. The tibial nerve lies in a protected position, deep in the calf [3].
It is much more common to see such a cyst in the common peroneal nerve or its branches [10, 11]. Other sites of occurrence have been described in the radial, ulnar, median, sciatic, and posterior interosseous nerves. The first case of a tibial nerve cyst was described in 1967, and there have been few reports in the literature since then. Several theories have been proposed to explain the occurrence of intraneural cysts, the most popular being retrograde extension of the synovial fluid along the intra-articular branch [2, 4]. In this most favored synovial theory, the ganglion originates from the articular or periarticular tissue of the neighboring joint and subsequently tracks along the sheath of a small articular nerve and migrates up to its final position in the sheath of a major nerve. A localized degenerative process of connective and perineural tissue secondary to chronic mechanical irritation (the metaplasia of irritated connective tissue) has also been proposed [2, 4, 12]. Other theories include development from embryonic cells of ectopic synovial tissue and evolution of post-traumatic intraneural hematoma with deposition of mucinous substance produced by metaplastic cells [11]. The lack of hemosiderin deposits in such cases including ours renders such a hypothesis less likely [2]. Our case did not show any communication with the joint, and it is hypothesized to be the result of isolated cystic degeneration of connective tissues of the epineurium or perineurium (Fig. 4). Blood products were not seen on the fat-suppressed T1W sequence or ultrasound, similar to previous reports on intraneural ganglion cysts [2].
Imaging including sonography and MRI are very helpful in the diagnosis of peripheral nerve lesions. Using high-frequency transducers and Doppler imaging, one can detect and characterize these lesions adequately. The intra-neural cysts show an expansive appearance that is homogeneous, anechoic, or heterogeneous with septations, with no internal Doppler flow. Panoramic sonography shows the full extent of the lesion like MRI [13]. MRN performed on high-field scanners allows multi-planar 3D imaging with vascular signal suppression and depicts the lesion extent, fascicular detail, altered signal intensity of the fascicles, and regional muscle denervation changes [14,15,16]. We could not detect denervation of the flexor hallucis muscle on sonography as on MRN, which was also not apparent clinically. In addition, the use of diffusion-weighted imaging (DWI) as part of MRN leads to selective depiction of nerves with adequate background muscle and fat signal suppression, neuropathy-related hyperintensity, and related muscle denervation lesions [17,18,19]. DW-MRN allows the spinal cord and peripheral nerves to be viewed because of the relatively lower apparent diffusion coefficients, fiber orientation (diffusion anisotropy), and tissue organization. Cysts typically present as homogeneous, multilocular, soft-tissue masses with fluid signals. The intravenous use of gadolinium helps in characterization, as there is no impregnation of the contrast medium in these cysts [20], as in our case. There was no enhancement of the affected tibial nerve due to the subacute to chronic neuropathy situation and possibly maintained blood-nerve barrier, as with metabolic neuropathies, such as diabetes mellitus [21].
The clinical diagnosis of a cyst of the tibial nerve from tumor lesions of the peripheral nerve is impossible when the patient presents with isolated sensory and/or motor symptoms. The ability of ultrasound, CT, and MRI to differentiate soft tissue structures and delineate abnormalities in trauma, nerve entrapment syndromes, and tumors aids in clinical diagnosis. MR imaging is particularly useful in the diagnosis of cystic lesions (fluid characteristics) from benign and malignant peripheral nerve sheath tumors (target sign, internal heterogeneity, and internal enhancement, etc.) [22, 23].
The treatment of tibial nerve cysts ranges from periodic follow-up to surgical excision of the lesion. Due to lack of motor symptoms and potential tibial nerve injury during surgery, the patient decided to forego surgical treatment over a year of follow-up.
Ultrasound-guided cyst aspiration can be used to avoid injury to the adjacent nerve fascicles and potential infection of the incision site. However, the cyst has high propensity of recurrence, especially if the communicating intra-articular branch is not addressed. Surgical treatment includes a simple decompression by evacuation of the cyst contents with or without excision of the cyst walls. The surgical treatment may be complicated as the lesion commonly infiltrates between the nerve fascicles, and in the absence of an expert surgical specialist, one may not be able to separate the lesion from the parent nerve, and complete excision may result in sacrifice of the nerve. Intra-articular branch clipping or excision is only available at specialized centers [24]. In our case, the attending physician and patient opted for clinical follow-up instead of surgery.
In conclusion, we present an illustrative case of intraneural cyst of the tibial nerve, a condition that, although rare, should be considered as a differential diagnosis of extra-articular calf neuropathy. Ultrasonography is a satisfactory method for the diagnosis of a cystic lesion of the tibial nerve; however, MRN allows more objective characterization of the fascicular detail and regional muscle denervation change.
References
Kim DH, Ryu S, Tiel RL, Kline DG. Surgical management and results of 135 tibial nerve lesions at the Louisiana State University Health Sciences Center. Neurosurgery. 2003;53(5):1114–24.
Patel P, Schucany WG. A rare case of intraneural ganglion cyst involving the tibial nerve. Proc (Bayl Univ Med Cent). 2012;25(2):132–5.
Chalian M, Soldatos T, Faridian-Aragh N, Williams EH, Rosson GD, Eng J, et al. 3T magnetic resonance neurography of tibial nerve pathologies. J. Neuroimaging. 2013;23(2):296–310.
Adn M, Hamlat A, Morandi X, Guegan Y. Intraneural ganglion cyst of the tibial nerve. Acta Neurochir (Wien). 2006;148(11):885–90.
Wilson TJ, Hébert-Blouin MN, Murthy NS, García JJ, Amrami KK, Spinner RJ. The nearly invisible intraneural cyst: a new and emerging part of the spectrum. Neurosurg Focus. 2017;42(3):E10.
Chhabra A, Williams EH, Subhawong TK, Hashemi S, Soldatos T, Wang KC, et al. MR neurography findings of soleal sling entrapment. AJR Am J Roentgenol. 2011;196(3):W290–7.
Junqueira LC, Carneiro J. Histologia Básica. 12° edition. Guanabara Koogan; 2013.
Kraychete CD, Sakata KR. Neuropatias periféricas dolorosas. Rev Bras Anestesiol. 2011;61(5):649–58. doi:10.1590/S0034-70942011000500014.
Hochman MG, Zilberfarb JL. Nerves in a pinch: imaging of nerve compression syndromes. Radiol Clin N Am. 2004;42(1):221–45. doi:10.1016/S0033-8389(03)00162-3.
Prasad NK, Desy NM, Howe BM, Amrami KK, Spinner RJ. Subparaneurial ganglion cysts of the fibular and tibial nerves: a new variant of intraneural ganglion cysts. Clin Anat. 2016;29(4):530–7.
Martins SR, Martinez JP, de Aguiar PH, Nakagawa E, Tedesco Marchese JA. Cisto sinovial intraneural do nervo fibular: relato de caso. Arq Neuro-Psiquiatr. 1977;55(4):831–3. doi:10.1590/S0004-282X1997000500022.
Vandenbulcke R, Marrannes J, Vandenbulcke B, Herman M, Laridon E, Van Holsbeeck B. Intraneural ganglion cyst of the tibial nerve. J Belgian Soc Radiol. 2015;99(1):125–6. doi:10.5334/jbr-btr.860.
Suk IJ, Walker OF, Cartwright SM. Ultrasound of peripheral nerves. Curr Neurol Neurosci. 2014; 13 (2): 328. doi: 10.1007/s11910-012-0328-x.
Chhabra A, Flammang A, Padua A Jr, Carrino JA, Andreisek G. Magnetic resonance neurography: technical considerations. Neuroimaging Clin N Am. 2014;24(1):67–78.
Spinner RJ, Atkinson JL, Harper CM Jr, Wenger DE. Recurrent intraneural ganglion cyst of the tibial nerve. J Neurosurg. 2000;92(2):334–7.
Petchprapa CN, Rosenberg ZS, Sconfienza LM, Cavalcanti CF, Vieira RL, Zember JS. MR imaging of entrapment neuropathies of the lower extremity. Part 1. The pelvis and hip. Radiographics. 2010;30(4):983–1000.
Takahara T, Hendrikse J, Yamashita T, Willem P, Mali MT, Kwee CT, et al. Diffusion-weighted MR neurography of the brachial plexus: Feasibility study. Radiology. 2008;249(2):653–60. doi:10.1148/radiol.2492071826.
Andreou A, Sohaib A, Collins DJ, Takaraha T, Kwee TC, Leach MO, et al. Diffusion-weighted MR neurography for the assessment of brachial plexopathy in oncological practice. Cancer Imag. 2015;15(1):6.
Takahara T, Iman Y, Yamashita T, Yasuda S, Nasu S, Cauteren M. Diffusion weighted whole body imaging with background body signal suppression (DWIBS): technical improvement using free breathing, STIR and high resolution 3D display. Radiat Med. 2004;22(4):275–82.
Ahlawat S, Chhabra A, Blakely J. Magnetic resonance neurography of peripheral nerve tumors and tumorlike conditions. Neuroimaging Clin N Am. 2014;24(1):171–92.
Thakkar RS, Del Grande F, Thawait GK, et al. Spectrum of high-resolution MRI findings in diabetic neuropathy. AJR Am J Roentgenol. 2012;199(2):407–12.
Leal Filho MB, Aguiar AAX, Almeida BR, et al. Schwanoma de plexo braquial: relato de dois casos. Arq. Neuro-Psiquiatr. 2004; 62 (1): 162-166.
Chung WJ, Chung HW, Shin MJ, et al. MRI to differentiate benign from malignant soft-tissue tumours of the extremities: a simplified systematic imaging approach using depth, size and heterogeneity of signal intensity. Br J Radiol. 2012;85:e831–6.
Desy NM, Lipinski LJ, Tanaka S, et al. Recurrent intraneural ganglion cysts: pathoanatomic patterns and treatament inplications. Clin Anatomy. 2015;28:1058–69.
Acknowledgements
The authors of this article declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
A. Chhabra receives royalties from Wolters and Jaypee. A. Chhabra also serves as a consultant with ICON Medical.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Silveira, C.R.S., Vieira, C.G.M., Pereira, B.M. et al. Cystic degeneration of the tibial nerve: magnetic resonance neurography and sonography appearances of an intraneural ganglion cyst. Skeletal Radiol 46, 1763–1767 (2017). https://doi.org/10.1007/s00256-017-2753-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-017-2753-z