Abstract
This prospective study assessed the postoperative analgesic effect of intra-articular ketorolac, morphine, and bupivacaine during arthroscopic outpatient partial meniscectomy. Group 1 patients (n=20) received postoperative injection of 60 mg intra-articular ketorolac, group 2 patients (n=20) 10 cc intra-articular bupivacaine 0.25%, group 3 patients (n=20) 1 mg intra-articular morphine diluted in 10 cc saline, and group 4 patients (n=20, controls) only 10 cc saline. We evaluated the postoperative analgesic effect (period measured from the end of the surgery until further analgesia was demanded), the level of postoperative pain (by visual analog scale 1, 2, 3, 12, and 24 h after surgery), and the need for additional pain medication (during the first 24 h after surgery). The best analgesic effect was in patients treated with intra-articular ketorolac, and this was statistically significant in: postoperative analgesic effect and the need for additional pain medication immediately after surgery, and after 24 h. No complications were found related to the intra-articular treatment. We conclude that 60 mg intra-articular ketorolac provides better analgesic effect than 10 cc intra-articular bupivacaine 0.25% or 1 mg intra-articular morphine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of arthroscopic techniques in major outpatient surgery means that an effective and safe postoperative analgesic treatment must be found. Local intra-articular anesthetics have commonly been used to treat postoperative pain, and although some studies have confirmed their efficacy [15, 19, 30, 31], others have questioned it [8, 16, 25]. Katz et al. [22] studied the pharmacokinetics of bupivacaine after injecting it into the knee and determined that 30 ml bupivacaine 0.5% is safe and does not lead to toxic plasma concentrations. Nevertheless some side effects of bupivacaine have been reported, some of which are potentially serious: buccal and perioral paresthesias, impaired speech, convulsions [14, 40] disorders in arterial pressure and heart rate, ventricular arrhythmias [33, 39], even heart failure [1], hypersensitive reactions, and urticaria [10]. At the end of the 1980s and beginning of the 1990s Stein et al. [34, 36] showed that opiate receptors were present in the nerve endings anchored to the inflamed synovial tissue. Since then various studies have found contradictory results when using intra-articular morphine after knee arthroscopy [2, 5, 7, 8, 11, 12, 17, 18, 20, 21, 23, 26, 29, 32, 35, 38]. It has been shown that ketorolac administered systemically is an effective analgesic [4, 27] because it alters the sensitivity of the peripheral nociceptors by reducing the local concentration of chemical allogenics that are activated by the injury to the peripheral tissues. Reuben and Connelly [27, 28] obtained promising results by administering ketorolac intra-articularly after arthroscopic surgery. The aim of this study was to evaluate the analgesic efficacy and the safety of 60 mg ketorolac compared with 10 cc bupivacaine 0.25% and 1 mg morphine.
Material and methods
A prospective, double-blind, randomized study was designed and approved by our institution’s committee for research and clinical trials. A total of 80 consecutive patients were studied who had been diagnosed with torn meniscus and recommended to have arthroscopic surgery. Patients were excluded if they were undergoing chronic treatment with nonsteroidal anti-inflammatory drugs, opiates, corticoids, or tricyclic antidepressants, if opiates were contraindicated, if they had severe psychic disorders, if they were unwilling or declined to participate in the study, or if they were a high surgical risk (American Society of Anesthesiologists class IV).
The patients were informed of the nature of the study during the standard preoperative preparation, and they gave their informed consent. They were also trained to use the visual analog scale (VAS). All patients were randomly assigned to a group to be treated with ketorolac, bupivacaine, morphine, or placebo, without their knowledge or that of the physician evaluating the results.
Surgery was carried out under total intravenous anesthesia. The opiate used was alfentanil in doses of 10 µg/kg before the incision and bolus of 10 µg/kg as determined by the anesthetist depending on the presence of hemodynamic disorders. To maintain the airway a laryngeal mask was inserted. Mechanical ventilation was volume controlled to maintain normocapnia and the maximum airway pressures below 20 cmH2O. Once the patient had been anesthetized, the tourniquet was inflated, the surgical field was sterilized, and a standard diagnostic arthroscopy was performed through an anterolateral and anteromedial portal. Partial meniscectomy was performed. The respective drug was injected into the joint after the portals had been stitched to prevent extravasation. A compression bandage was applied, and the tourniquet was removed. Postoperative analgesia was initiated at the patient’s request or when the VAS value was higher than 5, with orally administered paracetamol at 650 mg every 6 h and orally administered tramadol at 50 mg as the rescue dose.
The following demographic and clinical data were evaluated: sex, age, weight, duration of anesthetic, duration of surgical procedure, consumption of morphine during the operation, postoperative VAS values every hour during the 3-h stay in the reanimation unit, time between the injection of the drug into the joint and the first administration of paracetamol, VAS values following discharge 12 and 24 h after the procedure, oral analgesic consumption after discharge, and such undesirable effects as nausea, vomiting, pruritus, constipation, gastralgias, and hypersensitive reactions. There were no statistically significant differences in the demographic data (age, sex, weight, duration of anesthetic, duration of surgical procedure) between the four groups studied. No adverse reactions caused by injecting the drugs into the joint were observed in any of the patients.
Quantitative variables were analyzed using analysis of variance and categorical variables using the χ2 test. The level of statistical significance was set at P≤0.05. The statistical packages used for the analysis were BMDP and SPSS.
Results
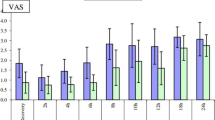
Although the VAS values of the patients treated with ketorolac tended to be lower than those of the other groups, the differences were not statistically significant (Table 1). The duration of postoperative analgesia was significantly longer in the patients treated with ketorolac than in the other groups (P=0.02; Table 2). Additional analgesic treatment was not required immediately after surgery in any of the patients treated with ketorolac, but it was required in 10% of the patients treated with bupivacaine, 24% of those treated with morphine, and 35% of those treated with placebo (P=0.02; Table 2). Likewise, the need to administer a rescue analgesic dose in the 24 h after the arthroscopy when the patient had already been discharged was significantly lower in the patients treated with intra-articular ketorolac (P=0.007; Table 2).
Discussion
Arthroscopic partial meniscectomy is one of the most common procedures in orthopedic surgery. In recent years, with the development of outpatient surgery units, the vast majority of these interventions have been performed by this procedure. One of the most important aspects to be considered is that the patients, who will be discharged shortly after surgery, must be provided with an analgesic treatment that is both effective and safe. Assessing the level of postoperative pain is very difficult. The most commonly accepted method is the VAS for assessing analgesia and the need to take additional analgesics as a rescue dose [6, 17, 18, 28, 30]. Infiltrating local anesthetics into the joint after the intervention has been one of the most widely used analgesic methods [3, 15, 19, 30, 31]. In a study comparing the efficacy of bupivacaine and placebo Chirwa et al. [8] concluded that an intra-articular local anesthetic is effective at calming pain for a short period of approx. 2 h, and that patients needed additional analgesia. Milligan et al. [25] found no statistically significant differences in postoperative pain among the patients who received 50 or 100 mg bupivacaine or saline. Henderson et al. [16] found no differences between patients treated with 75 mg bupivacaine and those treated with saline, which the authors thought was due to the rapid clearance of bupivacaine from the knee and residual pain at the arthroscopic portal. Also, some side effects of using bupivacaine have been reported, and although they are not very frequent, they are potentially serious: hypersensitive reactions and urticaria [10], neurological disorders ranging from perioral paresthesias to convulsions [14, 40], and disorders in arterial pressure and heart rate [33, 39]. In 1979 Albright [1] collected at least ten cases of heart failure attributed to the use of epidural bupivacaine in the induction of labor.
Systemic opiates are of limited use in nonhospitalized patients because they may affect the central nervous systems. However, Stein et al. [34, 36] showed that opiate receptors are present in inflamed peripheral tissues, and this was confirmed by Levine et al. [24] in experimental animals. This cleared the way for opiates to be used as a local analgesic. Stein et al. [35] compared the analgesic effect of opiates administered intra-articularly and intravenously and concluded that injecting 1 mg morphine diluted in 40 mg saline has a greater effect. In addition, this effect was blocked by administering intra-articular naloxone. Raja et al. [26] compared the effect of morphine and bupivacaine and found no benefit of using intra-articular morphine. Ruwe et al. [30] compared the analgesic effect of 1 mg morphine, bupivacaine, and the combination of morphine and bupivacaine in the postoperative period in 124 knee arthroscopies for various diagnoses. They concluded that morphine injected into the joint has no analgesic effect after the arthroscopy; in fact, patients who received morphine or placebo had greater pain than those who received bupivacaine. They observed that the patients with higher preoperative VAS scores also had higher postoperative scores, and they concluded that the critical factor in the perception of postoperative pain is the perception of preoperative pain.
Other studies, however, have obtained good analgesic results with morphine alone or combined with bupivacaine [6, 21, 29, 38]. In a systematic review of all clinical randomized trials Kalso et al. [20] concluded that morphine has some effect on the reduction in postoperative pain and the decrease in the consumption of analgesics. Joshi et al. [18] obtained good results by using 5 mg morphine. In a study comparing the analgesic effect of 4 mg morphine with bupivacaine Jaureguito et al. [17] showed that the effect of morphine depends on the dose, with doses four times greater than normal producing good results. Richardson et al. [29] compared the analgesic effect of 1 and 5 mg morphine. They concluded that 5 mg provides immediate and lasting analgesia. They observed that some patients experienced nausea and vomiting, but they concluded that this reaction is idiosyncratic and does not depend on the dose. Ketorolac administered systemically showed effective analgesic levels after anterior cruciate ligament surgery [4]. However, Thwaites et al. [37] showed defects in the platelet function of patients treated with intravenous ketorolac and who had been given intradural anesthesia. Reuben and Connelly [27, 28] obtained good analgesic levels with intra-articular ketorolac, particularly when associated with bupivacaine. Convery et al. [9] showed that administering low doses of intra-articular ketorolac has the same analgesic effect as administering 10 mg intravenously. Gupta et al. [13] compared the analgesic effect of intra-articular ketorolac and morphine, and the results were best when the two were administered together. This suggests that there is a synergic effect between them.
In the present study the analgesic effects of administering a single 60-mg dose of intra-articular ketorolac were found to be good. No side effects were noted. In the literature there is considerable controversy about the analgesic efficacy of administering intra-articular morphine and bupivacaine, as well as the possibility of potentially serious side effects, particularly at high doses. In the light of our results we believe that administering ketorolac is a good alternative to the analgesic treatment of patients who undergo outpatient arthroscopic meniscectomy.
References
Albright GA (1979) Cardiac arrest following regional anesthesia with etidocaine or bupivacaine. J Anesth 51:285–287
Allen GC, Amand MA, Lui ACP, et al (1993) Postarthroscopy analgesia with intraarticular bupivacaine/ morphine. Anesthesiology 79:475–480
Ates Y, Kinik H, Bínnet MS, Ates Y, Canakçi N, Keçik Y (1994) Comparison of prilocaine and bupivacaine for post-arthroscopy analgesia: a placebo-controlled double blind trial. Arthroscopy 10:108–109
Barber FA, Gladu DE (1998) Comparison of oral ketorolac and hydrocodone for pain relief after anterior cruciate ligament reconstruction. Arthroscopy 14:605–612
Bjornsoon A, Gupta A, Vegfors M, et al (1994) Intraarticular morphine for postoperative analgesia following knee arthroscopy. Reg Anesth 19:104–108
Boden BP, Fassler S, Cooper S, Marchetto PA, Moyer RA (1994) Analgesic effect or intraarticular morphine, bupivacaine, and morphine/bupivacaine after arthroscopic knee surgery. Arthroscopy 10:104–107
Calmet J, Vicente A, Boada S, Solsona B, Giné J (2001) Efecto analgésico de la morfina intraarticular en la artroscopia de rodilla. Cuader Artroscopia 8:26–31
Chirwa SS, MacLeod BA, Day B (1989) Intraarticular bupivacaine (marcaine) after arthroscopic meniscectomy. Arthroscopy 5:33–35
Convery PN, Milligan KR, Quinn P, Scott K, Clarke RC (1998) Low-dose intra-articular ketorolac for pain relief following arthroscopy of the knee joint. Anaesthesia 53:1125–1129
Craft DV, Good RP (1994) Delayed hypersensitivity reaction of the knee after injection of arthroscopy portals with bupivacaine (marcaine). Arthroscopy 10:305–308
Dalsgaard J, Felsby S, Juelsgaard P, Froekjaer J (1994) Low-dose intraarticular morphine analgesia in day case knee arthroscopy: a randomized double-blinded prospective study. Pain 56:151–154
Gentili M, Guhel A, Bonnet F (1997) Peripheral analgesic effect of intraarticular clonidine. Br J Anaesth 79:660–661
Gupta A, Axelsson K, Allvin R, Liszka-Hackzell J, Rawal N, Althoff B, Augustini BG (1999) Postoperative pain following knee arthroscopy: the effects of intra-articular ketorolac and/or morphine. Reg Anesth Pain Med 24:225–230
Hasselstrom L, Morgensen T (1984) Toxic reaction of bupivacaine at low plasma concentration. Anesthesiology 61:99–100
Heard SO, Edwards WT, Ferrari D, et al (1992) Analgesic effect of intraarticular bupivacaine or morphine after arthroscopy knee surgery: a randomized, prospective, double blind study. Anesth Analg 74:822–826
Henderson RC, Campion ER, De Massi RA. (1990) Postarthroscopy analgesia with bupivacaine. Am J Sports Med 18:614–617
Jaureguito JW, Wilcox JF, Cohn SJ, Thisted RA, Reider B (1995) A comparison of intraarticular morphine and bupivacaine for pain control after outpatient knee arthroscopy. A prospective, randomized, double-blinded study. Am J Sports Med 23:350–353
Joshi GP, McCarroll SM, Cooney CM, Blunnie WP, O’Brien TM, Lawrence AJ (1992) Intra-articular morphine for pain relief after knee arthroscopy. J Bone Joint Surg Br 74:749–751
Kaeding CC, Hill JA, Katz J, Benson L (1990) Bupivacaine use after knee arthroscopy: pharmacokinetics and pain control study. Arthroscopy 6:33–39
Kalso E, Tramer RM, Carroll D, McQuay HJ (1997) Pain relief from intra-articular morphine after knee surgery: a qualitative systematic review. Pain 71:127–134
Karlsson J, Rydgren B, Eriksson B, Järvholm U, Lundin O, Swärd L, Hedner T (1995) Postoperative analgesic effects of intra-articular bupivacaine and morphine after arthroscopic cruciate ligament surgery. Knee Surg Sports Traumatol Arthroscopy 3:55–59
Katz J, Kaeding CS, Hill JR (1998) The pharmocokinetics of bupivacaine when injected intraarticularly after knee arthroscopy. Anesth Analg 67:872–875
Khoury GF, Chen ACN, Garland DE, et al (1992) Intaarticular morphine, bupivacaine, and morphine/bupivacaine for pain control after knee videoarthroscopy. Anesthesiology 77:263–266
Levine JD, Taiwo YO (1989) Involvement of the mu-opiate receptor in peripheral analgesia. Neuroscience 32:571–575
Milligan DA, Mowbray MJ, Mulrooney L (1988) Intraarticular bupivacaine for pain relief after arthroscopy surgery of the knee joint in daycase patients. Anaesthesia 43:563–564
Raja SN, Dickstein RE, Johnson CA (1992) Comparison of postoperative analgesic effects of intraarticular bupivacaine and morphine following arthroscopic knee surgery. Anesthesiology 77:1143–1147
Reuben SS, Connelly NR (1995) Posotoperative analgesia for outpatient arthroscopic knee surgery with intraarticular bupivacaine and ketorolac. Anesth Analg 80:1154–1157
Reuben SS, Connelly NR (1996) Postarthroscopic meniscus repair analgesia with intraarticular ketorolac or morphine. Anesth Analg 82:1036–1039
Richardson MD, Bjorksten AR, Hart JAL, Orth FA, McCullough K (1997) The efficacy of intra-articular morphine for postoperative knee arthroscopy analgesia. Arthroscopy 13:584–589
Ruwe PA, Klein I, Shields CL (1995) The effect of intraarticular injection of morphine and bupivacaine on postarthroscopic pain control. Am J Sports Med 23:59–64
Smith I, Hemerlrijk JV, White PF, Shivley R (1991) Effects of local anesthesia on recovery after outpatient arthroscopy. Anesth Analg 73:536–539
Söderlund A, Westman L, Esmark H, et al (1997) Analgesia following arthroscopy. A comparison of intrarticular morphine, pethidine and fentanyl. Acta Anaesthesiol Scand 41:6–11
Solanki DR, Enneking FK, Ivey FM, Scarborough M, Johnston RV (1992) Serum bupivacaine concentrations after intraarticular injection for pain relief after knee arthroscopy. Arthroscopy 8:44–47
Stein C, Millan MJ, Yassouridis A, Herz A (1988) Antinociceptive effect of μ- and k- agonists in inflamation are enhanced by a peripheral opioid receptor specific mechanism. Eur J Pharmacol 155:255–264
Stein C, Comisel K, Haimerl E, Yassouridis A, Lehrberger K, Herz A, Peter K (1991) Analgesic effect of intraarticular morphine after arthroscopic knee surgery. N Engl J Med 325:1123–1126
Stein C, Hassan A, Lehrberger K, Glefing J, Yassouridis A (1993) Local analgesic effect of endogenous opioid peptides. Lancet 342:321–324
Thwaites BK, Nigus DB, Bouska GW, Mongan PD, Ayala EF, Merrill GA (1996) Intravenous ketorolac tromethamine worsens platelet function during knee arthroscopy under spinal anesthesia. Anesth Analg 82:1176–1181
Uysalel A, Keçik Y, Kirdemir P, Sayin M, Binnet M (1995) Comparison of intraarticular bupivacaine with the addition of morphine or fentanyl for analgesia after arthroscopic surgery. Arthroscopy 11:660–663
Wasudev G, Smith BE, Limbird TJ (1990) Blood levels of bupivacaine after arthroscopy of the knee joint. Arthroscopy 6:40–42
Willis J (1983) Adverse reactions with bupivacaine. FDA Drug Bull 13:23
Acknowledgement
We acknowledge Mr. John Bates from the Linguistic Service of the Rovira i Virgili University for revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Calmet, J., Esteve, C., Boada, S. et al. Analgesic effect of intra-articular ketorolac in knee arthroscopy: comparison of morphine and bupivacaine. Knee Surg Sports Traumatol Arthrosc 12, 552–555 (2004). https://doi.org/10.1007/s00167-003-0483-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-003-0483-3