Abstract
Aim
There are many alternatives for post-operative pain relief in patients who have had general anaesthesia. The aim of this study was to evaluate the efficacy of intra-articular bupivacaine + morphine and bupivacaine + tenoxicam applications in post-operative pain control in patients undergoing knee arthroscopy with general anaesthesia.
Method
This was a prospective study. Standard anaesthesia procedures were applied to each patient, and the 240 patients chosen at random were then divided into two groups. Each group received a different combination of drugs for this double-blind study. The first group (group A: 120 patients) received 0.5 % bupivacaine 100 mg + tenoxicam 20 mg (22 ml); the second group (group B) received 0.5 % bupivacaine 100 mg + morphine 2 mg (22 ml); both groups received their drugs at the end of the intra-articular operation before tourniquet deflation. Before the operation, patients were asked about their post-operative pain at particular periods over the following 24 hours using the visual analogue scale (VAS) and the numeric rating scale (NRS). An additional analgaesic requirement and possible side effects were also recorded.
Results
Group A patients needed analgaesics sooner after operation than patients in group B. In Group B, VAS and NRS values were statistically higher compared with group A at the 12th hour. There were also fewer side effects seen in group A versus group B.
Conclusion
Effective and reliable results were obtained in post-operative pain control in bupivacaine added to the morphine or tenoxicam groups following arthroscopic meniscectomy. In the tenoxicam group, patients reported less pain, fewer side effects and less need for analgesics at 12 hours after the operation.
Level of evidence: level 1, therapeutic, randomised, multicentric study
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arthroscopic knee operations are very common. Patients are generally discharged either on the day of operation or on the following day, depending upon the procedure. Post-operative pain after arthroscopic surgery is an important drawback for early rehabilitation and early discharge from the hospital. Analgesics and anti-inflammatory drugs may not be enough to relieve post-operative pain, and intramuscular (IM) and intravenous (IV) injection of morphine and other opiates use may be required. Dizziness, nausea and vomiting as a result of systemic opiate use can prevent early discharge from the hospital and can cause late patient mobilisation.
Femoral blocks and intra-articular analgaesic applications are common techniques used in post-operative pain control after arthroscopic surgery. Compared with femoral-block applications, which have some complications [1], intra-articular injection or infusion of local anaesthetic drugs is more efficient, more generally accepted and have been used in post-operative pain control for a considerable time [2]. The application of intra-articular bupivacaine provides enough analgaesia, but this effect is valid for only a short period of time. In order to prolong its analgaesic effect, drugs such as non-steroidal anti-inflammatory drugs (NSAIDs), morphine and ketamine are combined with bupivacaine. However, it is not clear of these drugs produces the optimal combination for pain relief [3, 4]. There is no prospective, randomised, double-blind study comparing combinations of bupivacaine–morphine and bupivacaine–tenoxicam.
In our study, post-operative analgaesic effects of intra-articular bupivacaine–morphine with bupivacaine–tenoxicam combinations, additional post-operative analgaesic requirements and side effects were evaluated in patients undergoing arthroscopic partial meniscectomy.
Patients and method
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Informed consent was obtained from all individuals in the study. This article does not contain any studies with animals performed by any of the authors. Our study was approved by the ethical committee of Istanbul Medeniyet University Goztepe Training and Research Hospital (no. 57/A8), and patients undergoing arthroscopic meniscectomy at the orthopedics and traumatology departments of two different universities were included in the study. Patients who were admitted to the orthopedics outpatient department with complaints of knee pain, who were thought to have meniscal tears as evidenced in physical examinations, whose magnetic resonance imaging (MRI) findings demonstrated a meniscus tear and who then agreed to participate in the study were chosen as the target group. The study included patients with isolated meniscal tears as a preliminary diagnosis. Exclusions were patients with tears and an additional anterior cruciate ligament tear, cartilage damage, radiographic knee osteoarthritis and/or a history of rheumatic disease which would require additional intervention; and patients with bupivacaine, morphine or tenoxicam allergies.
Two hundred and forty-four patients were given a diagnosis of symptomatic meniscal tears and were divided into two randomised groups. Four patients were excluded: one with anterior cruciate ligament tear, one with osteochondral lesion, one with tenoxicam allergy and one with sickle cell anemia. The study was completed by 240 patients. Randomisation was performed according to whether the last digit of the outpatient barcodes was odd or even: odd were designated as group A and even as group B. Patient age, gender and weight were recorded and body mass index (BMI) calculated.
After operation, it was explained to the patients how they might evaluate post-operative pain using the visual analogue scale (VAS) and the numerical rating scale (NRS). For VAS scoring, patients marked the option (0–10) on the 10-cm-long horizontal or vertical straight line that started with absence of pain and ended with unbearable pain according to the severity of their pain. The point relative to the starting point was recorded by measuring the distance between two points as centimetres. Similarly, for the NRS, absence of pain started with 0 and scoring increased to 10 (unbearable pain). Pain intensity was evaluated with NRS numerically [5]. VAS and NRS evaluation was done in both groups at hours one, two, four, six, 12 and 24 post-operatively. Assessment was performed by inpatient nurses who were uninformed about the intra-articular injection in the operating room. Double-blind evaluation was provided in this way.
Thiopental 5 mg/kg and vecuronium 0.1 mg/kg were given to all patients for the induction upon fentanyl 1 μg/kg for premedication. Patients were intubated orotracheally after sufficient time for muscle relaxation. For maintaining anaesthesia, O2N2O 50–50 % and sevoflurane 1 % were given Intravenous administration of analgaesics were not given during the operation or at the end of surgery.
Upon completing the operation, the arthroscopic cannula system was removed from the knee before tourniquet deflation, then 0.5 % bupivacaine (100 mg) and 20 mg tenoxicam (22 ml) was given intra-articularly to group A (120 patients) and 0.5 % bupivacaine (100 mg) and 2 mg morphine (22 ml) was given intra-articularly to group B (120 patients). At the same time, anaesthesia was ended, an elastic bandage was wrapped and the tourniquet was opened for 10 min after intra-articular administration of analgesia. After being extubated, patients were transferred to a post-operative recovery room and then to inpatient service. They were discharged from the hospital the following day. Upon operation, side effects such as hypotension, bradycardia, respiratory depression, nausea and vomiting were recorded. The first post-operative analgaesic requirement time was recorded as time from post extubation to application of the first analgaesic.
First, diclofenac (75 mg) was given IM to patients with VAS values >5. In case of unsuccesful pain control, pethidine hydrochloride was given IM. Patient exercises accompanied by a physiotherapist were started the first postoperative day, before the patient was discharged and they mobilised. No chondrolysis symptoms were seen in this study. We used the Microsoft Excel statistical analysis software package, and p < 0.05 level was assessed. Student’s t test was used to determine differences between groups.
Results
Average patient age, gender distribution, weight and BMI are summarised in Table 1.
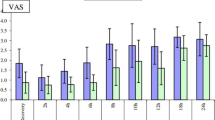
VAS upon extubation were similar. VAS values for group A at post-operative one, two and four hours were statistically significantly higher than for group B (p = 0.012; p < 0.0001, p = 0.003;,respectively) (Table 2). In group B, VAS values at post-operative hour 12 were statistically significantly higher than in group A (p < 0.0001; Table 2). There was no significant difference between groups with respect to average VAS values at post-operative 6 and 24 h (p = 0.66, p = 0.47, respectively) (Table 2).
NRS values of both groups upon extubation were similar but for group B were significantly different at six, 12 and 24 hours post-operatively ( p = 0.04, p < 0.0001 and p = 0.019, respectively) (Table 3). When groups were compared, there was no significant association related to average NRS values at post-operative hours one, two, four and six (p = 0.71, p = 0.91, p = 0.13, p = 0.42;,respectively) (Table 3).
The average time until first post-operative requirement for analgaesics was 4.5 ± 2.51 hours in group A and 11.23 ± 3.96 hours in group B, being statistically significantly longer in group B (p < 0.0001) (Table 4). There was a need for additional analgaesics in 78 cases (65 %) in group B and 30 (25 %) in group A. The first additional analgaesic intake time after operation at 24 hours was 0.45 ± 0.83 hours in group A and 0.85 ± 0.88 hours in group B. The total amount of additional analgaesic used in group B was statistically significantly higher than in group A (p = 0.0004) (Table 4).
While there were no cases of hypotension in group A, there were six (5 %) in group B. Other side effects, such as bradycardia, respiratory depression and chondrolysis, were not seen in either group. Nausea and vomiting were observed in four patients (3 %) in group A and in 36 (30 %) in group B (Table 5).
Discussion
In our study, tenoxicam or morphine combined with bupivacaine showed similar results in terms of post-operative pain control. However, both protocols had different influences and side effects. Post-operative pain is an important reason for dissatisfaction after arthroscopic knee surgery. When pain relief cannot be achieved by simple analgaesics, opiates are generally used, which can lead to late mobilisation and rehabilitation due to side effects such as nausea, vomiting and dizziness. However, if acute post-operative pain is not treated, it can become chronic due to the transport of pathophysiological processes from peripheral to central [6, 7].
Some studies have evaluated different combinations of analgaesics applied intra-articularly in the process of arthroscopic knee surgery [8]. However, which combination is most effective and reliable remains uncertain [9]. The ideal analgaesic should have long and local influence with minimal side effects.
Since bupivacaine is more effective than simple anaesthetics, its intra-articular usage is accepted in post-operative analgesia. According to studies, intra-articular concentrations of bupivacaine should be <0.5 %, since it can damage articular cartilage. When Meaning et al. used 150 mg (0.5 %) bupivacaine and Keading et al. used 100 mg (0.25 %), no toxic effects were reported [10, 11]. However, Atik recommended the use of analgaesics at lower concentrations, since their intra-articular use may lead to cartilage damage. Atik also showed that combinations of analgaesics with corticosteroids might cause even more damage [12].
The reason for acute chondrolysis is still unclear. Infections, iatrogenic chondral injuries, thermal necrosis, intra-articular pain pumps and high-dose local anaesthetics have been found responsible [13]. Acute chondrolysis is an undesirable complication that, at the early post-operative stage, knee-flexion contracture and range-of-motion (ROM) limitation can be seen. In our study, we used 100 mg (0.5 %) intra-articularly infused bupivacaine so as not to cause acute chondrolysis.
Many studies indicate post-operative usage of intra-articularly applied bupivacaine. In some of those studies, bupivacaine did not provide sufficient analgesia [14], whereas some studies showed that it was quite effective [3, 15]. Smith et al. used 150 mg (0.5 %) bupivacaine in arthroscopic knee surgery and showed that patients in the bupivacaine group needed fewer post-operative narcotic analgaesics and were discharged from hospital earlier than the placebo group [3].
Bupivacaine applied intra-articularly provides effective post-operative analgesia but its effect is short lived. For this reason, there is a requirement for additional analgaesic. Some studies show that when narcotic analgaesics were initially preferred, the effect of intra-articular application of 1–5 mg morphine began late but continued for 48 hours [16, 17]. In our study, the morphine group required additional analgaesics at later times compared with the tenoxicam group; additionally, the morphine group needed a much greater amount of analgaesics.
Similar to our study, Whitford et al. reported that in the event of opening the tourniquet 10 min after intra-articular application of morphine, better analgesia was provided and the requirement of additional analgaesic decreased [18]. In some studies, intra-articular application of bupivacaine + morphine effectively provided long-lasting pain relief effectively, whereas some other studies showed that this combination was useless. In our study, at about 12 hours after operation, morphine patients indicated more pain than those in the tenoxicam group. We consider that this may occur because of the inflammatory response, which appears to be due to arthroscopic intervention. The anti-inflammatory effect of tenoxicam might have an advantage over morphine. We attempted to assess patients with similar inflammatory responses by choosing patients who required a meniscectomy only. NSAIDs used intra-articularly either alone or with bupivacaine after arthroscopic operations are reported to decrease post-operative analgaesic usage [19]. In our study, we used the combination of bupivacaine and tenoxicam, the latter drug being a long-acting NSAID that decreases the concentration of allogenic chemicals activated by damaged tissues upon intra-articular application. In this manner, it decreases nociceptor sensitivity, prevents inflammation on the knee-joint surface and provides analgesia with minimal systemic effect.
There are some limitations to our study. The most important is the use of spinal anaesthesia, which is much preferable at the present time. However, it is not possible in such cases to assess early post-operative analgaesic effect due to its longer analgesic effect. We had no control group in which intra-articular analgaesic application was not used. However, since the aim of our study was to compare the analgaesic effects of tenoxicam with morphine in terms of improving effectiveness when used with bupivacaine, we did not feel the need to prove the analgaesic effects of the drugs used. The study has a quite large sample size compared with other studies in the literature and is, moreover, prospective, randomised and double-blinded; however larger series should be assessed.
When we compared groups, we found that the time period before which patients first required analgaesics post-operatively was longer but the incidence of side effects was higher in the bupivacaine + morphine group. Side effects and additional analgaesic usage were lower in the bupivacaine + tenoxicam group. We believe that 0.5 % bupivacaine 100 mg + tenoxicam 20 mg intra-articularly for arthroscopic meniscectomy decreases the amount of additional analgaesics required and causes fewer side effects.
References
Fredricson MJ, Kilfoyle DH (2009) Neurological complication analysis of 1000 ultrasound guided peripheral nerve blocks for elective orthopaedic surgery: a prospective study. Anaesthesia 64:836–844
Alford JW, Fadale PD (2003) Evaluation of postoperative bupivacaine infusion for pain management after anterior cruciate ligament reconstruction. Arthroscopy 19:855–861
Smith I (1991) Effects of local anesthesia on recovery after out patient arthroscopy. Anaesth Analg 73:536–539
Brill S, Plaza M (2004) Non narcotic adjuvants may improve the duration and quality of analgesia after knee arthroscopy: a brief review. Can J Anaesth 51:975–978
Jamison RN (1993) Clinical Measurement of Pain. In: Ferrante FM, VadeBonceur TR (eds) Postoperative Pain Management, 6th edn. Churchill Livingstone Inc., New York, pp 119–130
Perkins FM (2000) Chronic pain as an outcome of surgery- a review of predictive factors. Anaesthesiology 93:1123–1133
Macrae WA (2001) Chronic pain after surgery. Br J Anaesth 87:88–98
Alagol A, Calpur OU et al (2005) Intraarticular analgesia after arthroscopic knee surgery comparison of neostigmine, clonidine, tenoxicam, morphine and bupivacaine. Knee Surg Sports Traumatol Arthrosc 13:658–663
Elhakim M (1999) Combination of intraarticular tenoxicam, lidocaine and pethidine for out patient knee arthroscopy. Acta Anaesthesiol Scand 43:803–808
Meining R (1988) Plasma bupivacaine levels following single dose instillation for arthroscopy. Am J Sport Med 16:295–300
Keading CC, Hill JA et al (1990) Bupivacaine use after knee arthroscopy: Pharmaco kinetic and Pain Control Study. Arthroscopy 6:33–39
Atik OS (2012) Is single-dose local anesthetic chondrotoxic. (Article inTurkish). Eklem Hastalik Cerrahisi 23:111–112
Slabaugh MA, Friel NA et al (2010) Rapid Chondrolysis of the Knee After Anterior Cruciate Ligament Reconstruction: a case report. J Bone Joint Surg Am 92:186–189. doi:10.2106/JBJS.I.00120
Henderson BC (1990) Post arthroscopy analgesia with bupivacaine. A prospective, randomized, blinded evaluation. Am J Sports 18:614–617
Geutjens G, Hambridge JE (1994) Analgesic effects of intra articular bupivacaine after day- case arthroscopy. Arthroscopy 10:299–300
Dalsgaard J (1994) Low dose intra articular morphine analgesia in day –case knee arthroscopy. Pain 56:151–154
Heine MF, Tillet ED (1994) Intraarticular morphine after arthroscopic knee operation. Br J Anaesth 73:413–415
Whitford A (1997) The effect of tourniquet release time on the analgesic efficacy of intraarticular morphine after arthroscopic knee surgery. Anaesth And Analg 84:791–793
Talu G (2002) Comparison of efficacy of intra articular application of tenoxicam, bupivacaine and tenoxicam bupivacaine combination in arthroscopic knee surgery. Knee Surg Sports Traumatol Arthrosc 10:355–360
Conflict of interest
All authors in this study declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sanel, S., Arpaz, O., Unay, K. et al. Comparison of intra-articular bupivacaine–morphine with bupivacaine–tenoxicam combinations on post-operative analgesia in patients with arthroscopic meniscectomy: a prospective, randomised study. International Orthopaedics (SICOT) 40, 601–605 (2016). https://doi.org/10.1007/s00264-015-2990-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2990-5