Abstract
Purpose
Invasive pulmonary aspergillosis (IPA) is a dreadful event in patients with hematological malignancies (HM). Recent advances have standardized diagnostic, prophylactic and curative therapeutic strategies. We sought to assess whether these advances actually translate into improved survival in critically ill patients with acute respiratory failure and IPA.
Methods
This was a retrospective, multicenter study. Adult patients with HM, IPA, admitted to the ICU for acute respiratory failure over a 20-year period (January 1998–December 2017) were included. A cox regression model was used to identify variables independently associated with day-90 survival.
Results
Overall, 219 patients were included [138 (63%) men, median age 55 (IQR 44–64)]. Acute myeloid leukemia (30.1%) and non-Hodgkin lymphoma (22.8%) were the most frequent malignancies, and 53 (24.2%) were allogeneic stem cell recipients. Day-1 SOFA score was 9 [7,8,9,10,11,12]. Most patients presented with probable IPA, whereas 15 (7%) underwent lung biopsies or pleurocentesis and met criteria for proven IPA. Overall ICU and day-90 mortality were, respectively, 58.4% and 75.2% (80.4% if invasive mechanical ventilation) without any significant improvement over time. By multivariable analysis adjusted on day-1 SOFA score and ventilation strategies, voriconazole use (HR 0.49, CI 95 0.34–0.73, p < 0.001) and an ICU admission after 2010 (HR 0.67, 0.45–0.99, p = 0.042) were associated with increased survival, whereas a diffuse radiologic pattern (HR 2.07, CI 95 1.33–3.24, p = 0.001) and delayed admission to the ICU (HR 1.51, CI 95 1.05–2.16, p = 0.026) were independently associated with increased mortality.
Conclusions
IPA is associated with high mortality rates in critically ill patients with acute respiratory failure. Routine voriconazole and prompt ICU admission are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Invasive Pulmonary Aspergillosis in patients with hematological malignancies mostly affects patients with neutropenia and allogeneic stem cell transplant recipients. Mortality remains high and stable over the last two decades. |
Introduction
Among hematology patients admitted to the ICU, invasive fungal infections remain associated with highest mortality rates [1, 2]. However, several advances outside the ICU were reported in patients with invasive pulmonary aspergillosis (IPA). Namely, a randomized trial demonstrated the superiority of voriconazole on the proportion of patients who could be cured from IPA, or survived [3]. Moreover, recognition of different clinical-CT patterns has allowed to better appraise diagnostic yield of non-invasive tests such as galactomannan or sputa culture, and to identify those patients in whom bronchoscopy and bronchoalveolar lavage (BAL) can actually assist the diagnosis [4]. Last, the use of prophylaxis in high-risk patients also modified both IPA incidence rates and clinical findings in AML patients or in recipients of allogeneic hematopoietic stem cell recipients [5, 6].
Advances also occurred in the ICU management of hematology patients with acute respiratory failure, in whom up to 10% present with IPA [1, 7,8,9], a condition associated with mortality [1], particularly for patients who met ARDS criteria [10]. For instance, the use of non-invasive diagnostic tests as opposed to bronchoscopy and BAL may avoid respiratory failure. Similarly, progress in oxygenation and ventilation strategies [11] also may decrease the need for invasive mechanical ventilation [1]. Last, as suggested in an earlier study from our group, voriconazole use was associated with lower mortality in this setting [12].
Whether these non-ICU and ICU advances actually translate into improved outcomes has never been properly assessed. Data are needed to guide the clinical decision and identify patients in whom the introduction or maintaining of invasive ventilation would be unreasonable. We then sought to appraise outcomes in hematology patients admitted to the ICU for ARF in whom a diagnosis of probable or proven invasive pulmonary aspergillosis has been established.
Patients and methods
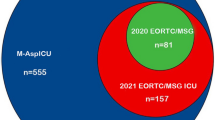
We conducted a multicentric retrospective study among the GRRR-OH study group (17 centers). All patients admitted to the ICU between January 1998 and December 2017 were included if they met the following criteria: (a) age > 18 years, (b) any hematological malignancy (HM), and (c) a recent diagnosis of IPA. IPA was diagnosed based on the 2008 EORTC criteria [13]. Only proven and probable IPA were included. Patients with proven IPA presented with a positive culture from a sterile sample or a pathological finding (needle aspiration or biopsy). Probable IPA required the combination of: host factors (neutropenia, allogeneic stem cell transplant, prolonged use of corticosteroids); clinical features including evocative CT scan lesions, tracheobronchitis observed during bronchoscopy or extrapulmonary (CNS or sinonasal) infection; a mycological criterion (positive fungal culture of respiratory samples or galactomannan antigen detection in serum or BAL).
Data presented in tables and figures were extracted from medical charts at each center. Radiologic presentation was reported from the initial chest x-ray or CT, realized in the previous or consecutive 24 h to ICU admission, and described as focal radiologic pattern, diffuse radiologic pattern or without specific pattern. Focal pattern was defined as a lesion restricted to the pulmonary lobe on chest X-ray or CT scans. Diffuse pattern affected more than one lobe. When patients presented both patterns or none of them, they were characterized as “without any specific radiologic pattern”. The Sepsis-Related Organ Failure Assessment (SOFA) score was calculated at day 1 [14]. Neutropenia was defined as a neutrophil count < 500/mm3. Non-invasive tests were defined as all tests that do not require the realization of a bronchoscopy and profound sampling: serum antigen, tracheal aspiration, sputa analysis and sinus aspiration. The threshold for positive plasma or BAL galactomannan antigen was 0.5 ng/ml [15, 16]. Regarding ventilation support, patients were allocated to one of the following groups: never ventilated, non-invasive ventilation (NIV) or high-flow nasal oxygen (HFNO) success, NIV or HFNO failure, first-line invasive mechanical ventilation (IMV). Delayed ICU admission was characterized as a time from respiratory symptoms onset to ICU admission > 5 days [17].
Statistical analysis
Mean and standard deviation (SD) or median and interquartile ranges were calculated for continuous variables, while numbers and percentages were calculated for categorical parameters. The normal distribution of each continuous variable was assessed with the use of the Shapiro–Wilk test. For univariate risk factor analysis, categorical variables were compared between independent groups using the Fisher or the Chi square tests, and continuous variables were compared using the Mann–Whitney test. Logistic regression analysis was carried out to study the association between ICU or day-90 mortality and year of admission over the 20-year follow-up. The threshold of 5 days for delayed ICU admission was set according the variable median value and previous literature.
A multivariable logistic Cox analysis was performed to identify factors independently associated with day-90 mortality. Variables associated with day-90 mortality in the univariate analysis with a p < 0.10 were suitable for inclusion into the multivariate model and included: cough symptom, viral pneumonia, radiologic presentation, initial SOFA score, vasopressor therapy, voriconazole treatment and ventilation strategy. Two variables were forced into the model: the time between symptoms onset and ICU admission that had previously been observed in the literature [17]; and the year of admission (before/after 2010), which offered a time-dependent variable to reduce selection bias linked with our long inclusion period. Only variables with à p < 0.05 were maintained in the multivariate final model. Furthermore, the vasopressor therapy was removed because of its collinearity with the SOFA score, which presented a more complete and relevant information at ICU admission. Model assumptions for proportional hazards assumption, linear covariate relationship and lack of influential observation were tested and confirmed. To address selection bias, a sensitivity analysis was realized using a mixed-effect cox multivariable model with a random effect on the center of inclusion. Cumulative survival curves as a function of time adjusted on all variables from the cox multivariate model were presented using the Kaplan–Meier plots. All statistical analyses were performed on R (version 3.3.2 for Macintosh, licenses GNU GPL, The R foundation for statistical computing, Vienna, Austria). All tests were 2-sided and a P value < 0.05 was considered for statistical significance.
Results
Overall, 219 patients were included (Table 1 and Supplemental Fig. 1). Of those, 138 (63%) were of male gender and median age was of 55 (IQR 44–64). Acute myeloid leukemia (30.1%) and non-Hodgkin lymphoma (22.8%) were the most frequent malignancies. Fifty-three (24.2%) patients were allogeneic stem cell recipients, including 64.2% presenting Graft-versus-Host Disease. At admission, 134 (62%) patients were neutropenic, and 22 received antifungal prophylaxis (10%). Median SOFA score at admission was 9 [7,8,9,10,11,12]. 159 patients (72.9%) required vasopressors and 60 (27.8%) renal replacement therapy.
Patient were admitted to the ICU within 4.5 [1,2,3,4,5,6,7,8,9,10,11,12,13] days after symptoms onset. In addition to acute respiratory failure, 178 (81.3%) presented with fever, 71 (32.4%) cough, 29 (13.2%) chest pain and 25 (11.4%) presented at least one episode of hemoptysis (Table 1). Patients admitted in the ICU within 5 days after symptoms onset were diagnosed earlier for IPA compared with patient admitted after 5 days [3 (0–8) days vs. 11 [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21], p < 0.001]. IPA diagnosis was based on positive serum or BAL galactomannan (n = 74 patients, 33.8%), fungal cultures (n = 64, 29.2%) or both (n = 81, 37%). 137 patients (62.2%) had an IPA diagnosis made by non-invasive diagnostic test. BAL was the only positive test in 11.9% of patients (Supplemental Fig. 2). IPA diagnosis was made prior to ICU admission in 125 (61%) of our patients. In patients who received invasive mechanical ventilation, 64 (53%) were diagnosed before intubation. Aspergillus fumigatus was the most frequent isolated strain (72.1%), followed by Aspergillus flavus (10.3%) and Aspergillosis niger (2.9%) (Supplemental Table 1). Median time from symptoms onset to IPA diagnosis was 6 days [2–12.5]. Most patients presented with probable IPA, whereas 15 (7%) underwent lung biopsies or pleurocentesis and met criteria for proven IPA.
First-line invasive mechanical ventilation was carried out in 85 (39%) patients, whereas 68 (31%) patients were intubated after failure from NIV or HFNO. In addition, 35 patients underwent non-invasive ventilation or HFNO with success, and 31 patients only received standard oxygen therapy. Time from ICU admission to IMV was 1 [0–3] day, and length of mechanical ventilation was 7 [0–16] days. Patients receiving invasive mechanical ventilation had higher day-90 mortality (80.4% vs 42.3%, p < 0.01). As shown in Fig. 2, need for invasive mechanical ventilation at admission or after failure of non-invasive strategies was associated with high mortality rates. Fifty-four (24.7%) patients met criteria for ARDS.
ICU and day-90 mortality rates were 58.4% and 75.2%, respectively. Case fatality remained high throughout the 20-year study period (Table 2). ICU length of stay was 12 [5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21] days. During study time, no significant association between ICU (p = 0.21) or day-90 mortality (p = 0.28) and year of admission was reported (Fig. 1).
Various changes were reported among our cohort throughout the inclusion period. Patients admitted after 2010 were older (57 vs. 51 years old, p = 0.02), received more allogeneic stem cell transplant (29.2% vs. 16.9%, p = 0.04), were more frequently treated by long-term corticosteroids (51.5% vs. 37.1%, p = 0.04) and showed a trend toward a longer duration of invasive mechanical ventilation (8 vs. 5 days, p = 0.13). However, SOFA admission scores (p = 0.72), number of antifungal lines of treatment (p = 0.270) and time between hematological diagnosis and ICU admission (p = 0.911) were not different (Fig. 2).
By multivariable analysis adjusted on day-1 SOFA score and ventilation strategies, use of voriconazole (HR 0.49, CI 95 0.34–0.73, p < 0.001) and an ICU admission after 2010 (HR 0.67, 0.45–0.99, p = 0.042) were associated with improved survival, whereas a diffuse radiologic pattern (HR 2.07, CI 95 1.33–3.24, p = 0.001) and delayed ICU admission (HR 1.51, CI 95 1.05–2.16, p = 0.026) were independently associated with higher day-90 mortality Table 3 and Fig. 3). The sensitivity analysis with a random effect on the center inclusion revealed similar significant results.
Kaplan–Meier plots of adjusted cumulative survival curves as a function of time regarding voriconazole treatment (a), radiologic presentation (b), ventilation strategy (c) and time between symptoms onset and ICU admission (d). NIV Non-invasive ventilation, HFNO High-Flow Nasal Oxygen, IMV invasive mechanical ventilation
Discussion
This is the largest study to date that reports outcomes in critically ill hematology patients admitted to the ICU with acute respiratory failure from probable or proven IPA. These findings collected in 17 ICUs from our study group confirm clinical benefits from voriconazole in this population, and put forward outcome implications of delayed ICU management. Furthermore, the lower survival rate in patients requiring intubation and mechanical ventilation emphasizes the need to improve clinician’s ability for maintaining a high level of IPA suspicion in at-risk patients, as well as to implement appropriate diagnostic workup in these patients.
In our cohort, despite a slight improvement for patients included after 2010, no significant association between ICU or day-90 mortality and time of admission was reported. This differs from recent encouraging trends of survival in hematological patients [18], in the subset admitted to the ICU [2, 19,20,21,22] and in patients with HM and IPA [12, 23, 24]. In an effort to clarify this paradox, we formulate the following hypotheses. First, the chronological beneficial effect expected from the generalization of voriconazole was diluted due to the early availability of the treatment in our cohort, as soon as 2001, 3 year after inclusion began. Second, in our cohort, patient characteristics changed over the study period for older and more immunocompromised subjects and may have impacted overall mortality. Indeed, development of specific hematological care for older patients contributed to the modification of ICU patient profile in hematological centers [25]. Moreover, our observation confirms the high severity and need for invasive and aggressive treatments in IPA patients, and emphasizes on the need for a proper assessment before an admission in the ICU. Furthermore, the introduction of invasive mechanical ventilation remains a strong predictor of mortality in hematological patients [2]. Indeed, the development of NIV [26,27,28] and HFNO [11, 29] has not yet shown its benefits for hematological patient admitted to the ICU.
The management of ICU patients suffering from HM and IPA constitutes a particular challenge as they stigmatize the most profound and complex forms of immunosuppression. In a recent study, IPA was strongly associated with the need for IMV in HM patients with ARF [1]. The development of antifungal prophylaxis for high-risk patients may have lowered the incidence of invasive fungal infections but mortality remains alarming [6]. Nevertheless, rising physician’s focus on invasive fungal infections in HM patients is crucial knowing that at-risk population is constantly growing [30]. Indeed, new treatments indicated for patients with Chronic Lymphocytic Leukemia or Non-Hodgkin lymphoma may increase the incidence of opportunistic infections [31, 32]; as they may in the ageing population suffering from Myelodysplastic syndromes.
We reported that a delayed admission in the ICU of more than 5 days after respiratory symptoms onset was associated with higher day-90 mortality. This finding is consistent with the literature. Indeed, in a recent cohort of immunocompromised patients with ARF, a direct admission to the ICU resulted in a significant decrease in hospital mortality [1]. Same observation was noted among cancer patients with ARF with a lower survival rate when the time between respiratory symptoms onset and ICU admission was superior to 2 days [17]. In our cohort, patients admitted in the ICU within 5 days after symptoms onset benefited from a faster IPA diagnosis, and by proxy, a probable faster initiation of antifungal therapy. Our interpretation of these results is that faster diagnosis and treatment initiation, made possible by accessing the technical platform available in the ICU setting, may explain partly the improved day-90 mortality associated with early admission. Faster introduction of antifungal therapy may moderate respiratory symptoms and prevent, in some cases, the introduction of invasive mechanical ventilation, a factor highly associated with a grim prognosis. Furthermore, we believe that the time of admission in the ICU also reflects the type of IPA presentation. Late admission may be associated with more insidious and indolent forms with long term mild symptoms. These presentations could reflect a more profound or less controlled level of immunosuppression and may constitute an alarming signal announcing grim outcome. This observation is corroborated by the profound gap observed between ICU and day-90 mortality (Fig. 2), even in patients that did not require invasive respiratory support.
We also reported the negative impact of a diffuse radiologic pulmonary pattern compared to a focal pattern on patient survival. This confirms the correlation between the volume of the aspergillosis lesion and patient outcome [33]. Consequently, the necessity of conducting early CT scans on HM patients with ARF appears timely to avoid delaying diagnosis, assess treatment’s response and predict patient’s evolution.
Finally, voriconazole use was associated with higher survival rates in hematology patients with ARF from IPA. This is in line with a previous report from our group [12]. Hence, the superiority of voriconazole compared to other antifungal therapies is widely established and recommended outside the ICU [34, 35]. However, increasing reports mentioning azole resistance in Aspergillus fumigatus leading to treatment failure [36] raises concerns about the use of azole derivatives in patients previously exposed to posaconazole prophylaxis.
Strengths of our study include the large number of critically ill patients with probable or proven IPA, making this cohort the largest to date, including key messages that may remind clinicians of the specificity and complexity of critically ill hematology patients. Our results also put forward the need of early admission for at-risk patients as soon as they present signs of respiratory distress or high oxygen requirements. All physicians of hematology patients need to optimize patient trajectory and avoid delaying appropriate management, enabling a faster diagnosis and treatment initiation leading to better survival [37].
The present study has several limitations, however. First, the study design was retrospective due to the low incidence of the disease. Nevertheless, to avoid selection bias, we identified 219 patients from a dedicated study group with a majority of centers of expertise specialized in the care of hematological patients. Second, our inclusion was limited to patients in France; however, the majority of our epidemiologic observations and results are in agreement with previous data available in the literature and implies an acceptable external validity. Third, radiological signs were gathered only in exams realized in the previous or consecutive 24 h to ICU admission, which made it impossible to study the dynamic evolution of aspergillosis lesions under treatment; a useful and validated clinical information associated to patient outcomes [33, 38]. Fourth, given the retrospective study design, two major concerns had to be addressed. The first one is the inevitable omission of a few cases of probable/proven invasive aspergillosis given the high incidence of unknown cause of ARF in critically ill patients, the necessary time to identify fungal pathogen and the still insufficient number of autopsies carried out in deceased patients. Indeed, a recent study presented the results of 893 post-mortem examinations of critically ill patients over a 25-year period [39]. Only 10 of 25 (40%) patients with invasive aspergillosis were diagnosed before death. The second concern, that stems from the previous observation, is that only crude mortality, and not attributable mortality, was reported in our study. Hematological patients with ARF are often the result of multiple concomitant factors that are inseparable from each other, even in the eyes of the ICU physicians in charge of them. Assessing the causality of IPA, without an autopsy, in a deceased patient who suffered from ARF, is based on a set of arguments, including the chronology of the fungal infection and the specificity of clinical and radiological sign. To overcome this potential weakness, sustained attention was paid to report all variables that could help characterize, in the best way, the multiple factors implicated in the respiratory failure and all potential confusion factors that may have influenced patient mortality. Last, this study mentions tracheobronchial ulceration evidenced by fiberscopy or sinonasal infection as part of invasive pulmonary aspergillosis. However, according to the EORTC criteria these clinical features are suggestive of tracheobronchial aspergillosis and sinonasal aspergillosis. We do, however, consider that our patients had all invasive pulmonary aspergillosis. Indeed, all had acute respiratory failure whereas co-infections were documented in a minority of patients; data have emphasized that there were two different patterns of IPA, the halo sign being typical only in patients with neutropenia [4].; and 3/no patient had isolated sinonasal aspergillosis but only a continuum of airway-invasive aspergillosis also involving the upper respiratory tract.
In summary, IPA still mostly affects patients with neutropenia and allogeneic stem cell transplant recipients. Case fatality remains high and stable throughout the 20-year follow-up. Voriconazole treatment is associated with improved survival whereas diffuse radiologic pattern and delayed admission to the ICU are associated with a poor prognosis. Strategies to improve survival in these high-risk patients are warranted.
References
Azoulay E, Pickkers P, Soares M et al (2017) Acute hypoxemic respiratory failure in immunocompromised patients: the Efraim multinational prospective cohort study. Intensive Care Med 43:1808–1819. https://doi.org/10.1007/s00134-017-4947-1
Azoulay E, Mokart D, Pène F et al (2013) Outcomes of critically Ill patients with hematologic malignancies: prospective multicenter data from france and belgium—a groupe de recherche respiratoire en réanimation onco-hématologique study. JCO 31:2810–2818. https://doi.org/10.1200/JCO.2012.47.2365
Herbrecht R, Denning DW, Patterson TF et al (2002) Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med 347:408–415. https://doi.org/10.1056/NEJMoa020191
Bergeron A, Porcher R, Sulahian A et al (2012) The strategy for the diagnosis of invasive pulmonary aspergillosis should depend on both the underlying condition and the leukocyte count of patients with hematologic malignancies. Blood 119:1831–1837. https://doi.org/10.1182/blood-2011-04-351601
Ullmann AJ, Lipton JH, Vesole DH et al (2007) Posaconazole or fluconazole for prophylaxis in severe graft-versus-host disease. N Engl J Med 356:335–347. https://doi.org/10.1056/NEJMoa061098
Cornely OA, Maertens J, Winston DJ et al (2007) Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med 356:348–359. https://doi.org/10.1056/NEJMoa061094
Azoulay E, Mokart D, Rabbat A et al (2008) Diagnostic bronchoscopy in hematology and oncology patients with acute respiratory failure: prospective multicenter data*. Crit Care Med 36:100–107. https://doi.org/10.1097/01.CCM.0000295590.33145.C4
Azoulay E, Thiéry G, Chevret S et al (2004) The prognosis of acute respiratory failure in critically ill cancer patients. Medicine 83:360–370
Contejean A, Lemiale V, Resche-Rigon M et al (2016) Increased mortality in hematological malignancy patients with acute respiratory failure from undetermined etiology: a groupe de recherche en réanimation respiratoire en onco-hématologique (Grrr-OH) study. Ann Intensive Care 6:102. https://doi.org/10.1186/s13613-016-0202-0
Azoulay E, Lemiale V, Mokart D et al (2014) Acute respiratory distress syndrome in patients with malignancies. Intensive Care Med 40:1106–1114. https://doi.org/10.1007/s00134-014-3354-0
Frat J-P, Ragot S, Girault C et al (2016) Effect of non-invasive oxygenation strategies in immunocompromised patients with severe acute respiratory failure: a post hoc analysis of a randomised trial. Lancet Respir Med 4:646–652. https://doi.org/10.1016/S2213-2600(16)30093-5
Burghi G, Lemiale V, Seguin A et al (2011) Outcomes of mechanically ventilated hematology patients with invasive pulmonary aspergillosis. Intensive Care Med 37:1605–1612. https://doi.org/10.1007/s00134-011-2344-8
De Pauw B, Walsh TJ, Donnelly JP et al (2008) Revised definitions of invasive fungal disease from the european organization for research and treatment of cancer/invasive fungal infections cooperative group and the national institute of allergy and infectious diseases mycoses study group (EORTC/MSG) consensus group. Clin Infect Dis 46:1813–1821. https://doi.org/10.1086/588660
Vincent JL, Moreno R, Takala J et al (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the european society of intensive care medicine. Intensive Care Med. 22(7):707–710
Sulahian A, Boutboul F, Ribaud P et al (2001) Value of antigen detection using an enzyme immunoassay in the diagnosis and prediction of invasive aspergillosis in two adult and pediatric hematology units during a 4-year prospective study. Cancer 91:311–318
Meersseman W, Lagrou K, Maertens J et al (2008) Galactomannan in bronchoalveolar lavage fluid: a tool for diagnosing aspergillosis in intensive care unit patients. Am J Respir Crit Care Med 177:27–34. https://doi.org/10.1164/rccm.200704-606OC
Mokart D, Lambert J, Schnell D et al (2013) Delayed intensive care unit admission is associated with increased mortality in patients with cancer with acute respiratory failure. Leuk Lymphoma 54:1724–1729. https://doi.org/10.3109/10428194.2012.753446
Pulte D, Jansen L, Castro FA, Brenner H (2016) Changes in the survival of older patients with hematologic malignancies in the early 21st century. Cancer 122:2031–2040. https://doi.org/10.1002/cncr.30003
Zuber B, Tran T-C, Aegerter P et al (2012) Impact of case volume on survival of septic shock in patients with malignancies. Crit Care Med 40:55–62. https://doi.org/10.1097/CCM.0b013e31822d74ba
Larché J, Azoulay E, Fieux F et al (2003) Improved survival of critically ill cancer patients with septic shock. Intensive Care Med 29:1688–1695. https://doi.org/10.1007/s00134-003-1957-y
Legrand M, Max A, Peigne V et al (2012) Survival in neutropenic patients with severe sepsis or septic shock. Crit Care Med 40:43–49. https://doi.org/10.1097/CCM.0b013e31822b50c2
Mokart D, Pastores SM, Darmon M (2014) Has survival increased in cancer patients admitted to the ICU? Yes. Intensive Care Med 40:1570–1572. https://doi.org/10.1007/s00134-014-3433-2
Nicolle M-C, Bénet T, Thiebaut A et al (2011) Invasive aspergillosis in patients with hematologic malignancies: incidence and description of 127 cases enrolled in a single institution prospective survey from 2004 to 2009. Haematologica 96:1685–1691. https://doi.org/10.3324/haematol.2011.044636
Sun K-S, Tsai C-F, Chen SC-C, Huang W-C (2017) Clinical outcome and prognostic factors associated with invasive pulmonary aspergillosis: an 11-year follow-up report from Taiwan. PLoS One 12:e0186422–10. https://doi.org/10.1371/journal.pone.0186422
de Vries VA, Müller MCA, Sesmu Arbous M et al (2018) Time trend analysis of long term outcome of patients with haematological malignancies admitted at dutch intensive care units. Br J Haematol 181:68–76. https://doi.org/10.1111/bjh.15140
Hilbert G, Gruson D, Vargas F et al (2001) Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N Engl J Med 344:481–487. https://doi.org/10.1056/NEJM200102153440703
Gristina GR, Antonelli M, Conti G et al (2011) Noninvasive versus invasive ventilation for acute respiratory failure in patients with hematologic malignancies: a 5-year multicenter observational survey. Crit Care Med 39:2232–2239. https://doi.org/10.1097/CCM.0b013e3182227a27
Lemiale V, Mokart D, Resche-Rigon M et al (2015) Effect of noninvasive ventilation vs oxygen therapy on mortality among immunocompromised patients with acute respiratory failure. JAMA 314:1711–1719. https://doi.org/10.1001/jama.2015.12402
Azoulay E, Lemiale V, Mokart D et al (2018) Effect of high-flow nasal oxygen vs standard oxygen on 28-day mortality in immunocompromised patients with acute respiratory failure: the high randomized clinical trial. JAMA 320:2099–2107. https://doi.org/10.1001/jama.2018.14282
Harpaz R, Dahl RM, Dooling KL (2016) Prevalence of immunosuppression among US adults, 2013. JAMA 316:2547–2548. https://doi.org/10.1001/jama.2016.16477
Varughese T, Taur Y, Cohen N et al (2018) Serious infections in patients receiving ibrutinib for treatment of lymphoid cancer. Clin Infect Dis 67:687–692. https://doi.org/10.1093/cid/ciy175
Ghez D, Calleja A, Protin C et al (2018) Early-onset invasive aspergillosis and other fungal infections in patients treated with ibrutinib. Blood 131:1955–1959. https://doi.org/10.1182/blood-2017-11-818286
Vehreschild JJ, Heussel CP, Groll AH et al (2017) Serial assessment of pulmonary lesion volume by computed tomography allows survival prediction in invasive pulmonary aspergillosis. Eur Radiol 27:3275–3282. https://doi.org/10.1007/s00330-016-4717-4
Patterson TF, Thompson GR, Denning DW et al (2016) Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the infectious diseases society of America. Clin Infect Dis 63:e1–e60. https://doi.org/10.1093/cid/ciw326
Ullmann AJ, Aguado JM, Arikan-Akdagli S et al (2018) Diagnosis and management of aspergillus diseases: executive summary of the 2017 ESCMID–ECMM–ERS guideline. Clin Microbiol Infect 24(Suppl 1):e1–e38. https://doi.org/10.1016/j.cmi.2018.01.002
Snelders E, van der Lee HAL, Kuijpers J et al (2008) Emergence of azole resistance in Aspergillus fumigatus and spread of a single resistance mechanism. PLoS Med 5:e219. https://doi.org/10.1371/journal.pmed.0050219
Nucci M, Nouér SA, Cappone D, Anaissie E (2013) Early diagnosis of invasive pulmonary aspergillosis in hematologic patients: an opportunity to improve the outcome. Haematologica 98:1657–1660. https://doi.org/10.3324/haematol.2013.094359
Caillot D, Latrabe V, Thiebaut A et al (2010) Computer tomography in pulmonary invasive aspergillosis in hematological patients with neutropenia: an useful tool for diagnosis and assessment of outcome in clinical trials. Eur J Radiol 74:e172–e175. https://doi.org/10.1016/j.ejrad.2009.05.058
Tejerina EE, Abril E, Padilla R et al (2019) Invasive aspergillosis in critically ill patients: an autopsy study. Mycoses 62:673–679. https://doi.org/10.1111/myc.12927
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Pr. Azoulay declares having received fees for lectures and travel to conference from Pfizer, Gilead, Baxter, Alexion and Ablynx. Dr Lemiale reported being a member of a research group that has received grants from Fisher & Paykel, Alexion, Baxter, Pfizer, and Gilead. Pr. Darmon report having received consulting fees from Sanofi and Gilead-Kite, research support from Astute Medical and MSD, and speaker fees from MSD, Gilead-Kite and Astellas. Dr. De Jong reports personal fees from Baxter and Medtronic, and travel reimbursements from Fresenius-Kabi, MSD France, Astellas, Pfizer and Fisher Paykel. Other authors declare having no conflicts of interest in relation with this publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pardo, E., Lemiale, V., Mokart, D. et al. Invasive pulmonary aspergillosis in critically ill patients with hematological malignancies. Intensive Care Med 45, 1732–1741 (2019). https://doi.org/10.1007/s00134-019-05789-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-019-05789-6