Abstract
Purpose
Characteristics of acute kidney injury (AKI) occurring after out-of-hospital cardiac arrest (OHCA) are incompletely described. We aimed to evaluate the prevalence of AKI, identifying risk factors and assessing the impact of AKI on outcome after OHCA.
Methods
Single-center study between 2007 and 2012 in a cardiac arrest center in Paris, France. All consecutive OHCA patients with at least one weight measurement and one serum creatinine level available and treated by therapeutic hypothermia were included, except those with chronic kidney disease and those dead on arrival. AKI was defined as stage 3 of the Acute Kidney Injury Network (AKIN) classification. Main outcome was day-30 mortality. Factors associated with AKI occurrence and day-30 mortality were evaluated by logistic regression.
Results
580 patients (71.3 % male, median age 59.3 years, initial shockable rhythm in 56.9 % of cases) were included in the analysis. AKI stage 3 occurred in 280 (48.3 %) patients. Age, male gender, resuscitation duration, post-resuscitation shock, public setting, and initial rhythm were associated with AKI stage 3. AKI stage 3 was associated with a significantly higher day-30 mortality rate [OR 1.60; 95 % CI (1.05, 2.43); p = 0.03]. No independent association between AKI and neurologic outcome was observed. At day 30, 67 patients had a normal kidney function (eGFR >75 mL/min/1.73 m2), and five remained dialysis-dependent. Patients with eGFR higher than 75 mL/min/1.73 m2 at day 30 were younger and more frequently male.
Conclusion
AKI stage 3 was frequent after OHCA and was associated with poorer outcome. Improvement strategies in post-resuscitation care should consider AKI as a potential target of treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Out-of-hospital cardiac arrest (OHCA) is a frequent cause of death among adults in European countries with an estimated incidence of 38 per 100,000 person years [1]. Outcome remains poor with a survival rate at hospital discharge of around 8 % [2]. In patients who achieve sustainable return of spontaneous circulation (ROSC) after OHCA, morbidity and mortality are mostly due to the development of a “post cardiac arrest syndrome” that is related to multi-organ ischemic reperfusion injury [3, 4]. Although cardiovascular failure usually dominates the clinical picture, multi-organ failure may be observed [5]. Among organ damage occurring in this setting, previous studies reported a high prevalence of acute kidney injury (AKI) after OHCA [6–9]. It is unknown if targeted temperature management and early coronary angiography, which are recommended by international guidelines [10], could impact on AKI occurrence in these patients [11, 12].
In the general population of critically ill patients, AKI is a well-known prognostic factor associated with poorer outcome during ICU stay. While AKI is an independent risk factor for mortality in critically ill patients [13–16], data remains scarce and discordant in OHCA patients in whom cerebral damage is considered to be the dominating variable. In addition factors contributing to AKI are insufficiently explored in this setting. When performed, early coronary angiogram may increase this risk, particularly in OHCA patients with post-cardiac arrest shock as debated in other settings [17–19]. To date, the contribution of coronary angiogram to the risk of AKI occurrence has been poorly studied in OHCA patients [20].
In this study, we aimed to evaluate the incidence of AKI within the first 48 h after hospital admission in a large cohort of resuscitated OHCA patients, to identify risk factors for developing AKI and to evaluate the impact of AKI on mortality after OHCA.
The present study was previously presented in September 2014 at the European Society of Intensive Care Medicine in Barcelona [21].
Materials and methods
Study setting
We performed a single-center study between January 2007 and December 2012 in the 24-bed cardiac arrest center in Paris. Data were prospectively collected according to Utstein style [22], as previously described [23]. The following information was recorded prospectively for each patient: demographic data, clinical parameters, cardiac arrest location, time from collapse to basic life support (BLS) and time from BLS to ROSC, initial rhythm, hypothermia management, and ICU mortality. Previous use of angiotensin converting enzyme inhibitors and angiotensin 2 receptor antagonists was recorded. Post-resuscitation shock was defined as the need for vasopressors (epinephrine or norepinephrine) lasting more than 6 h despite adequate fluid loading or the need for ventricular assistance (intra-aortic balloon pump).
Early management
As previously described [24], our local practices include a strategy of early imaging diagnosis performed within the first 24 h after an immediate assessment of the feasibility of further investigations by the emergency medical services and ICU physicians. According to this strategy, we consider immediate coronary angiography in all patients without obvious extracardiac cause of cardiac arrest, regardless of the initial rhythm and ECG changes. If indicated, patients are admitted directly to the cardiac catheterization laboratory. When coronary angiography is performed, a percutaneous coronary intervention (PCI) is attempted if a culprit coronary lesion is considered to be the cause of OHCA, as previously described [23, 25]. In case of suspected extracardiac cause and in the absence of an obvious etiology, a CT scan can also be performed at admission (brain CT scan and chest CT pulmonary angiography). After this early imaging procedure, patients are then admitted to ICU. At ICU admission, renal replacement therapy (RRT) is initiated in case of severe metabolic acidosis (defined by a pH lower than 7.20 and an admission bicarbonate level lower than 20 mmol/L) and/or in case of life-threatening hyperkalemia (defined by blood potassium level higher than 6 mmol/L with electrocardiographic findings suggestive of hyperkalemia). Therapeutic hypothermia was performed using the forced cold air method.
Study population
After approval by our local ethics committee (IRB number CE-SRLF 12-384), we included all consecutive OHCA patients admitted to our ICU during the study period with at least one weight determination and one serum creatinine level available at ICU admission. In order to obtain an homogeneous population, we restricted the analysis to patients who received therapeutic hypothermia, which is widely used in our center. We excluded patients with chronic kidney disease and patients who died within the first 48 h after ICU admission due to refractory multi-organ failure. Chronic kidney disease was retrieved from medical history. We determined the occurrence of AKI within the first 48 h and used stage 3 of the Acute Kidney Injury Network (AKIN) criteria [26] to define it. According to this definition, patients were classified AKI stage 3 if serum creatinine showed a three-fold rise compared with baseline or reaches an absolute level of 4 mg/dL (i.e., 354 µmol/L) with an increase of at least 0.5 mg/dL (i.e., 44 µmol/L). Since premorbid creatinine is often not available in this situation, we used admission creatinine level as baseline. To ensure that this did not constitute a large deviation from reality, we performed a sensitivity analysis in which baseline creatinine was back-calculated through the MDRD equation assuming a 75 mL/min/1.73 m2 glomerular filtration rate. The AKIN urine output criteria for stage 3 (less than 0.3 mL/kg/h for 24 h or anuria for at least 12 h) were used only during the first 24 h. Finally, patients who received RRT within the first 48 h were considered to have met the criteria for AKIN stage 3 irrespective of other criteria.
Day-30 glomerular filtration rate was estimated with the MDRD equation [27]. Patients with glomerular filtration rate higher than 75 mL/min/1.73 m2 were considered to not have significant renal failure.
Statistical analysis
Descriptive statistics were reported as medians (with interquartile range) and as frequency (percentage) for continuous and categorical variables respectively unless otherwise specified. Characteristics between OHCA patients with and without AKI stage 3 were compared using Mann–Whitney–Wilcoxon’s rank sum test, and Pearson Chi-square test or the Fisher’s exact test, as appropriate, for continuous and categorical variables, respectively.
Factors associated with AKI occurrence and day-30 mortality were assessed by a multiple logistic regression initially including all the Utstein variables [22] and then we applied a stepwise backward selection of the variables which remained significant (p < 0.05). Interactions were searched by introducing an interaction factor in the multivariate model. Linearity of continuous variables was verified.
To maximize the sensitivity of the AKIN definition and to take into account that early RRT at day 1 is sometimes used to optimize metabolic control in severe acidotic patients (thus not a criteria for AKIN), we performed a sensitivity analysis in the group of patients still requiring RRT at day 3. Moreover, the impact of iodinated contrast injection was evaluated as a binary variable but also as an ordinal variable (0, no iodinated contrast injection; 1, one of two complementary investigations requiring iodinated contrast injection, i.e., coronary angiography or CT scan; and 2, requiring both investigations).
All statistical tests were two-sided using a type I error of 0.05 unless otherwise mentioned. Analyses were performed using Stata 11.2 software (Stata, College Station, TX, USA).
Results
Patients
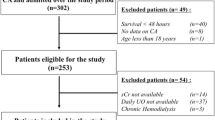
During the study period, 899 patients were admitted to the ICU after resuscitated OHCA. Among these, 22 patients with chronic kidney disease and 247 patients who died within the first 48 h after ICU arrival were excluded from the analysis. Moreover 48/630 patients were not treated by therapeutic hypothermia. Thus, 580/582 patients with documented weight remained in the final analysis (Fig. 1).
Baseline characteristics are described in Table 1. Studied patients were mostly male [n = 413 (71.2 %)] of median age 59.3 (48.9, 70.5) years. Cardiac arrest occurred in a public place in 213 (36.8 %) cases, and was witnessed in 503 (89.5 %) cases. The initial rhythm was shockable in 329 (56.7 %) cases. Post-resuscitation shock occurred in 294 (50.7 %) patients. Immediate coronary angiogram and CT scan were performed in 72.2 and 48.3 % of cases, respectively. No included patient received ECMO.
Prevalence and risk factors of AKI stage 3
AKI stage 3 was observed in 280 (48.3 %) patients. A total of 273 (47.1 %) patients had not evidenced any AKI, and 21 and six met stage 1 and 2 AKI criteria, respectively. A total of 110 patients met the AKI stage 3 definition due to oliguria alone, 77 met the creatinine criterion and another criterion (being RRT in 76), and 93 met all the three criteria (Supplementary Table 1). No patient had RRT as the only criterion and 169 required RRT during the first 48 h. Among patients who received RRT, 11 had evidence of an admission potassium level higher than 6 mmol/L and 81 a metabolic acidosis. AKI stage 3 was observed in 39.5 % of patients still requiring RRT at day 3. In multivariate analysis (Table 2), age, male gender, resuscitation duration, and post-resuscitation shock were associated with AKI stage 3, whereas OHCA in a public setting and an initial shockable rhythm were negatively associated with AKI stage 3. Iodinated contrast injection was not associated with AKI stage 3 occurrence in univariate analysis (80.7 vs. 81.5, p = 0.82). The number of investigations with iodinated contrast injection did not impact on AKI stage 3 occurrence [OR1 vs 0 0.86 (0.55, 1.34), p = 0.50 and OR2 vs. 0 1.71 (0.91, 3.21), p = 0.09]. Previous use of angiotensin converting enzyme inhibitors and angiotensin 2 receptor antagonists was not associated with AKI stage 3 occurrence [OR 1.04 (0.61, 1.77), p = 0.88 and OR 1.63 (0.84, 3.17), p = 0.15, respectively).
Day-30 mortality
Overall day-30 mortality was 57.6 % of included patients. Day-30 mortality was higher in AKI stage 3+ patients than in AKI stage 3− patients [196 (69.8 %) vs. 138 (46.2 %) p < 0.01]. In multivariable analysis (Table 3), AKI stage 3 was associated with a significantly higher day-30 mortality rate [OR 1.60; 95 % CI (1.05, 2.43); p = 0.03]. Others factors associated with day-30 mortality were age and resuscitation duration, whereas an initial shockable rhythm was negatively associated with ICU mortality. Similar results were obtained when we considered patients only requiring RRT at day 3 (Supplementary Table 2) and with AKI definition based on calculated baseline creatinine through MDRD assuming a 75 mL/min/1.73 m2 glomerular filtration rate [OR 1.71; 95 % CI (1.11, 2.63)]. No independent association between AKI and neurologic outcome was observed (Supplementary Table 3).
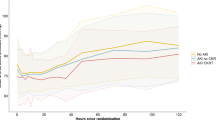
Renal outcome
Day-30 creatinine was available in 83 among 84 AKI stage 3 patients still alive at day 30. Glomerular filtration rate estimated by the MDRD equation was lower than 15 mL/min/1.73 m2 in five cases, between 15 and 29 mL/min/1.73 m2 in two cases, between 30 and 59 mL/min/1.73 m2 in seven cases, between 60 and 75 mL/min/1.73 m2 in two cases, and higher than 75 mL/min/1.73 m2 in 67 cases (Fig. 2, Supplementary Fig. 1). Patients with estimated glomerular filtration rate higher than 75 mL/min/1.73 m2 at day 30 were younger and more frequently male [55.1 (47.7, 65.2) vs. 71.8 (46.8, 87.1) years, p = 0.01 and 82.1 vs. 46.7 %, p < 0.01, respectively] (Supplementary Table 4).
Renal status at day 30 according to stage 3 acute kidney injury within the first 48 h after admission. The first two columns show the proportion of patients alive at day 30 according to stage 3 AKI within the first 48 h after admission. The third column shows the glomerular filtration rate among the 83 patients alive at day 30. AKI acute kidney injury, GFR glomerular filtration rate, RRT renal replacement therapy
Discussion
The present study aimed to evaluate the prevalence and prognosis of AKI after OHCA. We found three relevant messages: AKI stage 3 is frequent after cardiac arrest, is associated with worse outcome, but permanent need of RRT is rare in survivors.
AKI is frequent in critically ill patients [28]. In a large multicenter international survey, Uchino et al. [16] reported AKI in 5.7 % among 29,269 ICU patients, and 72 % of those patients had RRT. In the same manner, Joannidis et al. [29] reported a prevalence of AKIN stage 3 AKI up to 16 % in a large multicentric cohort of 16,784 critically ill patients. In the specific subset of post-cardiac arrest patients, few data are available. In the present study, we report a high prevalence of AKI in OHCA patients (48 %). This is higher than the prevalence reported in previous studies, which ranged from 10 to 30 % [9, 20]. This can be explained by difficulties in evaluating renal function in such patients. Results are difficult to compare because the definition of AKI varies across these different studies. In the present work, we chose to define AKI as stage 3 of the AKIN classification. Even if not perfect, we considered this definition as the most appropriate in such patients. The major criticism in using the AKIN classification is that patients in whom RRT is performed are classified as stage 3 whatever the reason for RRT. However RRT is sometimes used for control of metabolic disturbances (i.e., metabolic acidosis) even if other renal parameters are normal. This could result in an overestimation of AKI prevalence considering patients with only one single RRT at ICU admission as stage 3. To address this issue, we applied as a sensitivity analysis the AKIN definition with RRT at day 3 instead of RRT at day 1. We observed a lower prevalence of AKI (39.5 vs. 48.4 %) but a stronger association with day-30 mortality, which may more accurately reflect the real prognostic impact of AKI in cardiac arrest patients. In the present study, RRT was initiated in a higher proportion of OHCA patients than previously reported. However, patients included in previous studies evidenced less severe hemodynamic failure [9, 20, 30] and more frequently a cardiac cause of cardiac arrest [30]. This may explain the observed differences in RRT rates.
In our population, AKI was independently associated with day-30 mortality. While AKI is usually associated with long-term outcome in critically ill patients [16], data remains scarce and discordant among OHCA patients. Hasper et al. [30] showed an association of creatinine increase within the first 24 h after OHCA with poor neurologic outcome, whereas a decline in serum creatinine (higher than 0.2 mg/dL) indicated a favorable neurologic outcome. Accordingly, in a small cohort of 41 OHCA patients, Vanston et al. [31] showed that AKI was independently associated with poor outcome. On the other hand, Yanta et al. [20] did not evidence any association with AKI development and outcome in a cohort of 311 patients among which 115 (37 %) evidenced a renal injury (OR 0.73; 95 % CI 0.26, 2.05). To the best of our knowledge, the present study is the first to evaluate the association of AKI with mid-term outcome in OHCA patients. Even if we evidenced that AKI was a prognostic factor, only five AKI patients still required RRT at day 30. This result is consistent with those reported by Zeiner et al. [12] who studied the variation of creatinine within the first 4 weeks after OHCA. In the present study, impaired renal function was transient and completely reversible within 4 weeks.
This reversible characteristic raised the question of pathogenesis of AKI after OHCA. Mechanisms explaining AKI after cardiac arrest are probably multiple. First of all, the post-cardiac arrest period can be marked by a cardiovascular failure leading to ischemic kidney injury, as observed in all types of shock. Similar conditions between septic shock and post-resuscitation shock have already been reported [32] and may lead one to consider that kidney injury could be related, on the one hand, to abrupt decrease of renal blood flow by hemodynamic failure and, on the other hand, to the inflammatory storm provoked by the huge release of pro-inflammatory cytokines. In the present study, we evidenced a strong association between post-resuscitation shock and AKI occurrence. These findings are consistent with those published by Chua et al. [9] who evidenced a higher prevalence of AKI in patients with compared to those without post-resuscitation shock (51.7 vs. 6.4 %, p < 0.01). This pathological condition may explain why AKI is reversible in most cases after cardiac arrest. Resuscitated cardiac arrest is also a global ischemia–reperfusion phenomenon [3, 5]. Reperfusion provoked by CPR and ROSC leads to the formation of radical oxygen species that may cause cell death [5]. Disseminated vascular endothelium damage leads to systemic inflammation and associated coagulation activation and increased capillary permeability [32]. These microvascular abnormalities may induce renal lesions [5] and may contribute to AKI occurrence after cardiac arrest.
Another striking result of the present study is the absence of association between AKI and iodinated contrast injection during the early phase. Indeed, AKI remains a major point of debate regarding the risk–benefit ratio of an early imaging strategy in post-cardiac arrest patients [24]. Considering immediate coronary angiography, several studies reported a benefit as it allows one to treat the cause of the arrest by performing a PCI in many patients [23, 25, 33]. However the direct toxic effect of iodinated agents and the local vasoconstriction they can provoke may lead to ischemic kidney injury [34, 35]. In the present study, iodinated contrast injection was not associated with AKI occurrence after OHCA. Even if we cannot exclude a direct toxicity of iodinated contrast products in such patients, our results suggest that the risk–benefit ratio of these early diagnosis interventions is acceptable looking at renal outcome.
We acknowledge several limitations. First, we only collected urine output within the first 24 h and evaluated urine output criteria of the AKIN classification on the basis of this data. Even if there are some consistent data suggesting that urine output may drop faster than serum creatinine increases, this is a potential limitation. Second, we did not collect the exact volume of iodinated contrast product injected in each patient. We could hypothesize that the higher the volume, the higher the risk for AKI. However, we performed a sensitivity analysis taking into consideration the fact that one (PCI or CT scan) or both radiologic examinations were performed and we did not evidence any relationship between AKI occurrence and the number of iodinated exams. Third, we used estimated glomerular filtration rate by the MDRD equation to assess day-30 creatinine clearance. Significant changes between estimated and calculated glomerular filtration rates have been recently reported at ICU discharge [36] leading to the misevaluation of the glomerular filtration rate in patients from our study. Fourth, we did not report volume kinetics and its impact on serum creatinine level. Pickering et al. [37] have already reported that volume load could artificially decrease serum creatinine level and mislead on real glomerular filtration rate. Fifth, we used admission creatinine level as a surrogate of baseline characteristics. Even if unperfected, we performed a sensitivity analysis in which baseline creatinine was back-calculated through the MDRD equation assuming a 75 mL/min/1.73 m2 glomerular filtration rate and found similar results. Last, the present study is a single-center study that limits the generalization of our results.
To conclude, AKI occurs in half of patients successfully resuscitated from OHCA. Older age and post-resuscitation shock were independently associated with the occurrence of AKI, whereas an initial shockable rhythm and male gender were associated with a decreased risk of AKI. Finally AKI was independently associated with day-30 mortality, but nearly all survivors with initial AKI were free of dialysis at day 30.
References
Atwood C, Eisenberg MS, Herlitz J, Rea TD (2005) Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation 67:75–80. doi:10.1016/j.resuscitation.2005.03.021
Sasson C, Rogers MAM, Dahl J, Kellermann AL (2010) Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 3:63–81. doi:10.1161/CIRCOUTCOMES.109.889576
Neumar RW, Nolan JP, Adrie C et al (2008) Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, Inter American Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation 118:2452–2483. doi:10.1161/CIRCULATIONAHA.108.190652
Lemiale V, Dumas F, Mongardon N et al (2013) Intensive care unit mortality after cardiac arrest: the relative contribution of shock and brain injury in a large cohort. Intensive Care Med 39:1972–1980. doi:10.1007/s00134-013-3043-4
Mongardon N, Dumas F, Ricome S et al (2011) Postcardiac arrest syndrome: from immediate resuscitation to long-term outcome. Ann Intensive Care 1:45. doi:10.1186/2110-5820-1-45
Mattana J, Singhal PC (1993) Prevalence and determinants of acute renal failure following cardiopulmonary resuscitation. Arch Intern Med 153:235–239
Domanovits H, Schillinger M, Müllner M et al (2001) Acute renal failure after successful cardiopulmonary resuscitation. Intensive Care Med 27:1194–1199
Domanovits H, Müllner M, Sterz F et al (2000) Impairment of renal function in patients resuscitated from cardiac arrest: frequency, determinants and impact on outcome. Wien Klin Wochenschr 112:157–161
Chua H-R, Glassford N, Bellomo R (2012) Acute kidney injury after cardiac arrest. Resuscitation 83:721–727. doi:10.1016/j.resuscitation.2011.11.030
O’Connor RE, Bossaert L, Arntz H-R et al (2010) Part 9: acute coronary syndromes: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 122:S422–S465. doi:10.1161/CIRCULATIONAHA.110.985549
Susantitaphong P, Alfayez M, Cohen-Bucay A et al (2012) Therapeutic hypothermia and prevention of acute kidney injury: a meta-analysis of randomized controlled trials. Resuscitation 83:159–167. doi:10.1016/j.resuscitation.2011.09.023
Zeiner A, Sunder-Plassmann G, Sterz F et al (2004) The effect of mild therapeutic hypothermia on renal function after cardiopulmonary resuscitation in men. Resuscitation 60:253–261. doi:10.1016/j.resuscitation.2003.11.006
Barrantes F, Tian J, Vazquez R et al (2008) Acute kidney injury criteria predict outcomes of critically ill patients. Crit Care Med 36:1397–1403. doi:10.1097/CCM.0b013e318168fbe0
Mandelbaum T, Scott DJ, Lee J et al (2011) Outcome of critically ill patients with acute kidney injury using the acute kidney injury network criteria. Crit Care Med 39:2659–2664. doi:10.1097/CCM.0b013e3182281f1b
Vaara ST, Pettilä V, Kaukonen K-M et al (2014) The attributable mortality of acute kidney injury: a sequentially matched analysis. Crit Care Med 42:878–885. doi:10.1097/CCM.0000000000000045
Uchino S, Kellum JA, Bellomo R et al (2005) Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 294:813–818. doi:10.1001/jama.294.7.813
Abe D, Sato A, Hoshi T et al (2013) Clinical predictors of contrast-induced acute kidney injury in patients undergoing emergency versus elective percutaneous coronary intervention. Circ J 78:85–91
Tsai TT, Patel UD, Chang TI et al (2014) Contemporary incidence, predictors, and outcomes of acute kidney injury in patients undergoing percutaneous coronary interventions: insights from the NCDR Cath-PCI registry. JACC Cardiovasc Interv 7:1–9. doi:10.1016/j.jcin.2013.06.016
Rihal CS, Textor SC, Grill DE et al (2002) Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation 105:2259–2264
Yanta J, Guyette FX, Doshi AA et al (2013) Renal dysfunction is common following resuscitation from out-of-hospital cardiac arrest. Resuscitation. doi:10.1016/j.resuscitation.2013.03.037
Guillemet L et al (2014) Acute kidney injury after out-of-hospital cardiac arrest: prevalence, risk factors and outcome. Presented at the European Society of Intensive Care Medicine (ESICM) congress, Barcelona, 27 September–1 October 2014
Cummins RO, Chamberlain D, Hazinski MF et al (1997) Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital “Utstein style”. American Heart Association. Circulation 95:2213–2239
Dumas F, Cariou A, Manzo-Silberman S et al (2010) Immediate percutaneous coronary intervention is associated with better survival after out-of-hospital cardiac arrest: insights from the PROCAT (Parisian region out of hospital cardiac arrest) registry. Circ Cardiovasc Interv 3:200–207. doi:10.1161/CIRCINTERVENTIONS.109.913665
Chelly J, Mongardon N, Dumas F et al (2012) Benefit of an early and systematic imaging procedure after cardiac arrest: insights from the PROCAT (Parisian region out of hospital cardiac arrest) registry. Resuscitation 83:1444–1450. doi:10.1016/j.resuscitation.2012.08.321
Spaulding CM, Joly LM, Rosenberg A et al (1997) Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. N Engl J Med 336:1629–1633. doi:10.1056/NEJM199706053362302
Mehta RL, Kellum JA, Shah SV et al (2007) Acute kidney injury network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 11:R31. doi:10.1186/cc5713
Levey AS, Bosch JP, Lewis JB et al (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130:461–470
Nisula S, Kaukonen K-M, Vaara ST et al (2013) Incidence, risk factors and 90-day mortality of patients with acute kidney injury in Finnish intensive care units: the FINNAKI study. Intensive Care Med 39:420–428. doi:10.1007/s00134-012-2796-5
Joannidis M, Metnitz B, Bauer P et al (2009) Acute kidney injury in critically ill patients classified by AKIN versus RIFLE using the SAPS 3 database. Intensive Care Med 35:1692–1702. doi:10.1007/s00134-009-1530-4
Hasper D, von Haehling S, Storm C et al (2009) Changes in serum creatinine in the first 24 hours after cardiac arrest indicate prognosis: an observational cohort study. Crit Care 13:R168. doi:10.1186/cc8144
Vanston VJ, Lawhon-Triano M, Getts R et al (2010) Predictors of poor neurologic outcome in patients undergoing therapeutic hypothermia after cardiac arrest. South Med J 103:301–306. doi:10.1097/SMJ.0b013e3181d3cec2
Adrie C, Adib-Conquy M, Laurent I et al (2002) Successful cardiopulmonary resuscitation after cardiac arrest as a “sepsis-like” syndrome. Circulation 106:562–568
Dumas F, White L, Stubbs BA et al (2012) Long-term prognosis following resuscitation from out of hospital cardiac arrest: role of percutaneous coronary intervention and therapeutic hypothermia. J Am Coll Cardiol 60:21–27. doi:10.1016/j.jacc.2012.03.036
Tumlin J, Stacul F, Adam A et al (2006) Pathophysiology of contrast-induced nephropathy. Am J Cardiol 98:14K–20K. doi:10.1016/j.amjcard.2006.01.020
Hoste EAJ, Doom S, De Waele J et al (2011) Epidemiology of contrast-associated acute kidney injury in ICU patients: a retrospective cohort analysis. Intensive Care Med 37:1921–1931. doi:10.1007/s00134-011-2389-8
Schetz M, Gunst J, Van den Berghe G (2014) The impact of using estimated GFR versus creatinine clearance on the evaluation of recovery from acute kidney injury in the ICU. Intensive Care Med 40:1709–1717. doi:10.1007/s00134-014-3487-1
Pickering JW, Ralib AM, Endre ZH (2013) Combining creatinine and volume kinetics identifies missed cases of acute kidney injury following cardiac arrest. Crit Care 17:R7. doi:10.1186/cc11931
Acknowledgments
GG, LG, VL, CV, and AC designed the study. GG, LG, JC, MA, VL, and WB collected the data. GG performed the statistical analysis. GG and LG wrote the manuscript. FD, VL, LL, JPM, and AC reviewed the manuscript. GG and AC take responsibility for the integrity of the work. We thank Nancy Kentish-Barnes for her help in preparing the manuscript.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
G. Geri and L. Guillemet equally contributed to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Geri, G., Guillemet, L., Dumas, F. et al. Acute kidney injury after out-of-hospital cardiac arrest: risk factors and prognosis in a large cohort. Intensive Care Med 41, 1273–1280 (2015). https://doi.org/10.1007/s00134-015-3848-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-3848-4