Abstract
Purpose
Increased arterial ammonia levels are associated with high mortality in patients with acute liver failure (ALF). Data on the prognostic impact of arterial ammonia is lacking in hypoxic hepatitis (HH) and scarce in critically ill patients with cirrhosis.
Methods
The patient cohort comprised 72 patients with HH, 43 patients with ALF, 100 patients with liver cirrhosis and 45 patients without evidence for liver disease. Arterial ammonia concentrations were assessed on a daily basis in all patients and the results were compared among these four patient groups and between 28-day survivors and 28-day non-survivors overall and in each group.
Results
Overall 28-day mortality rates in patients with HH, ALF and cirrhosis and in the control group were 54, 30, 49 and 27 %, respectively. Peak arterial ammonia levels differed significantly between transplant-free 28-day survivors and non-survivors in the HH and ALF groups (p < 0.01 for both). Multivariate regression identified peak arterial ammonia concentrations as an independent predictor of 28-day mortality or liver transplantation in patients with HH and ALF, respectively (p < 0.01). There was no association between mortality and arterial ammonia in patients with liver cirrhosis and in the control group. Admission arterial ammonia levels were independently linked to hepatic encephalopathy grades 3/4 in patients with HH (p < 0.01), ALF (p < 0.05) and cirrhosis (p < 0.05), respectively.
Conclusions
Elevated arterial ammonia levels indicate a poor prognosis in acute liver injury and are associated with advanced HE in HH, ALF and cirrhosis. Arterial ammonia levels provide additional information in the risk assessment of critically ill patients with liver disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Elevated arterial ammonia levels are frequently observed in patients with acute liver failure (ALF) and/or liver cirrhosis [1–4]. Diminished ammonia-detoxification capacity and porto-systemic shunting have been deemed responsible for the increased circulating ammonia levels and consequent development of hepatic encephalopathy (HE) [5–9]. In ALF, elevated ammonia levels have been linked to clinical features of HE [10], cerebral complications [1–3, 11] and increased mortality [2]. In contrast, arterial ammonia levels do not predict either the severity of encephalopathy or mortality in cirrhotic patients with HE grades 3/4 in the intensive care unit (ICU) [12]. Hypoxic hepatitis (HH), also known as shock liver or ischemic hepatitis, occurs in approximately 10 % of all patients admitted to medical ICUs and is associated with high morbidity and mortality [13–16]. Yet, arterial ammonia levels in patients with HH and the clinical relevance of these levels have not been investigated.
The primary aim of this study was to compare peak arterial ammonia levels between survivors and non-survivors in a patient cohort of critically ill individuals with different entities of liver disease.
Materials and methods
Patients
The patient cohort comprised 226 critically ill patients who had been admitted to medical ICU 13H1 of the Medical University Vienna. These patients were classified into four groups based on the entity of liver disease (see "Definitions") or the absence thereof: HH (72 patients), ALF (43 patients), liver cirrhosis (100 patients) and control (= no evidence of liver disease; 45 patients).
All data were collected on a daily basis. Arterial ammonia concentration was determined as part of the routine daily laboratory assessment as described below. Twenty-eight-day mortality was assessed in all patients on site or by contacting the patients or their respective attending physician. Presence of HE was assessed by the attending physician and is part of the routine physical examination for patients with liver disease at our unit. The Simplified Acute Physiology Score II (SAPS II) [17], Sequential Organ Failure Assessment (SOFA) score [18], Systemic inflammatory response syndrome (SIRS) score [19] and Model of End-stage Liver Disease (MELD) score were calculated on admission to assess the severity of illness [20]. The study was approved by the ethics committee of the Medical University Vienna, which waived the need for informed consent due to the observational character of the study. Data of patients with HH and cirrhosis and of the control group were collected prospectively between 2008 and 2010 in consecutively admitted patients. The results of this study have been presented in part at the annual congress of the Society of Intensive Care Medicine 2010 [21]; data on patients of the ALF group were collected and analyzed retrospectively.
Therapeutic management of patients
All patients were treated following standardized protocols. Patients meeting shock criteria received fluids intravenously and vasopressors to maintain mean arterial pressure at >65 mmHg. Renal replacement therapy (RRT) was initiated in patients with renal failure and/or metabolic acidosis. Broad-spectrum antibiotics were empirically given to each patient; antimicrobial therapy was initiated and adapted to the culture results where necessary. Cirrhotic patients with signs of HE, but not ALF, and HH patients received l-ornithine-l-aspartate and lactulose. N-acetylcysteine was administered to ALF patients with suspected acetaminophen intoxication. Patients showing HE ≥ grade 3 were intubated and mechanically ventilated.
Definitions
Hypoxic hepatitis
Hypoxic hepatitis was diagnosed according to well-established criteria: (1) a clinical setting of cardiac, circulatory or respiratory failure; (2) a sharp increase in serum aminotransferase levels to at least 20-fold the upper limit of normal; (3) exclusion of other potential causes for increased aminotransferase levels [14, 15, 22]. Patients with HH accompanying cirrhosis were excluded from the analysis.
Acute liver failure
Acute liver failure was diagnosed in patients presenting with evidence of coagulation abnormality [international normalized ratio (INR) > 1.5] and any degree of mental alteration (encephalopathy) in the absence of pre-existing cirrhosis and with duration of illness <26 weeks [23].
Liver cirrhosis
Presence of liver cirrhosis was defined based on histological findings, if available, or by a combination of characteristic clinical (ascites, caput medusae, spider angiomata, among others), laboratory and radiological findings [typical morphological changes of the liver, sings of portal hypertension, etc. in ultrasonography or computed tomography (CT) scanning].
Hepatic encephalopathy
Hepatic encephalopathy was classified according to West–Haven criteria as HE grade 1 (trivial lack of awareness, shortened attention span, tremor, apraxia, incoordination of muscles), HE grade 2 (lethargy or apathy, disorientation, personality change, asterixis, ataxia, dysarthria), HE grade 3 (somnolence to semi-stupor, confusion, responsive to stimuli, asterixis, ataxia) and HE grade 4 (coma ± decerebration, unresponsive) [24–26]. Patients requiring intubation due to neurologic deterioration were considered HE stage 4. Clinical signs of HE were assessed in HH patients who were not intubated or sedated on or before admission to the ICU (22 %) for reasons other than encephalopathy [e.g. respiratory insufficiency, cardiopulmonary resuscitation (CPR), among others]. In sedated HH patients without contraindications for transportation [27], presence of HE was suggested by signs of intracranial hypertension on the CT/magnetic resonance imaging scans [28] or autopsy. Patients who had received CPR [29, 30] and those with pre-existing cerebral/cerebrovascular diseases were excluded from HE assessment.
Systemic inflammatory response syndrome)/sepsis/septic shock
Systemic inflammatory response syndrome, sepsis and septic shock were diagnosed as defined previously [31–33].
Cardiogenic shock
Cardiogenic shock was diagnosed in patients presenting with (1) low arterial blood pressure (systolic blood pressure <90 mmHg) without use of inotropes or requirement for vasopressors; (2) signs of decreased cardiac output (low cardiac output measured by any method, low mixed or central venous oxygen saturation, acute myocardial infarction); (3) absence of hypovolemia; (4) signs of organ malperfusion [34–36].
Measurement of arterial ammonia levels
Plasma ammonia levels were measured on a Beckman Coulter AU2700 chemistry analyzer (Beckman Coulter Diagnostics, Fullerton, CA) using the Ammonia Ultra reagents provided by Sentinel Diagnostics (Sentinel CH, Milan, Italy). The method is based on a glutamate dehydrogenase-mediated enzymatic transformation and UV detection of NADH to NAD+ that is proportionally dependent on the ammonia concentration in the plasma sample examined. The site of blood sampling was the radial artery in all patients. To avoid falsely high results, EDTA-anticoagulated blood samples were immediately placed on ice after blood sampling and typically processed within minutes. Only hemolysis-free plasma samples were eligible for analysis.
Data analysis and statistics
Data are presented as the median and 25–75 % interquartile range (IQR). Metric variables were compared using the Mann–Whitney test, dichotomous variables using chi-square- analysis. The primary aim of this study was to compare arterial ammonia levels between survivors and non-survivors as well as between patients with and without signs of HE in different entities of liver disease (HH, ALF and cirrhosis). Differences in peak arterial ammonia were also studied between survivors and non-survivors without liver disease (control group). A post hoc correction of Bonferroni was performed to correct for these seven primary tests; thus, the needed p value for significant results in the primary analyses was lowered to p < 0.0071 (p < 0.05/7). All further analyses performed were exploratory. Suitable threshold values for predictive metric variables were derived from receiver operating characteristic (ROC) analysis. A forward stepwise procedure was used to identify the most potent predictors for the respective outcome parameter. Model fit for logistic regression models was assessed via the Hosmer–Lemeshow test and Nagelkerke R 2. For all exploratory analyses, a p value of <0.05 was considered to be statistically significant. PASW Statistics ver. 17.0 (SPSS, Chicago, IL) was used for all analyses.
Results
Patients
Hypoxic hepatitis
The leading causes for the occurrence of HH among our patient cohort were cardiogenic (n = 31) and septic shock (n = 31), respectively. Other precipitating events were hypoxia/respiratory failure (n = 4), temporary hypotension (n = 2), pericardial effusion (n = 2) and arhythmogenic heart disease (n = 2). All patients had only one episode of HH during their stay in the ICU. Cerebral herniation occurred in only one patient with low arterial ammonia levels as a consequence of hypoxic brain injury following CPR.
Acute liver failure
Causes of ALF were viral (n = 12), amanita intoxication (n = 8), non-acetaminophen drug-induced (n = 7), autoimmune (n = 5), acetaminophen (n = 4), Wilson’s disease (n = 2) and unknown (n = 5). Twenty-six patients (60 %) presented with HE < grade 3 on admission, and 17 (40 %) presented with HE grade 3/4. Sixteen patients were admitted with HE of < grade 3, but subsequently developed HE grade 3/4. Altogether, 33 patients (77 %) showed HE grade 3/4 during their stay in the ICU. The majority of ALF patients (91 %) presented signs of HE at admission. One patient died from cerebral herniation. Fifteen patients (35 %) underwent orthotopic liver transplantation during the observation period.
Liver cirrhosis
Underlying causes of cirrhosis among our patient cohort were alcoholic liver disease (n = 53), hepatitis C (n = 16), combined etiology (all alcoholic + hepatitis C; n = 7), cryptogenic (n = 13) and other (n = 11). The main admission diagnoses were severe sepsis/septic shock (n = 46), gastrointestinal bleeding (n = 21), coma hepaticum/HE grades 3/4 (n = 10), hepatorenal syndrome (n = 9) and other (n = 14). Electronic Supplemental Material (ESM) Table 1 presents the admission and peak ammonia levels and the clinical HE grades stratified according to the main admission diagnoses. Fifty-two patients (52 %) were admitted with HE ≤ grade II and 33 (33 %) with HE grade 3/4; 15 (15 %) had no clinical signs of HE on admission. Six patients (6 %) were admitted with HE ≤ grade 2, but subsequently developed HE grade 3/4. None of the patients died from cerebral herniation, and none of the patients underwent orthotopic liver transplantation within 28 days following ICU admission. The median Child–Pugh score on admission was 12 (IQR 10–13).
Control
The control group consisted of 45 critically ill patients. Of these, 19 (42 %) had septic shock, and 26 (58 %) suffered from cardiogenic shock without signs of severe liver injury, viral or drug-induced hepatitis or cirrhosis or had serum aminotransferase levels that were less than fivefold the upper limit of normal and serum bilirubin levels that were less than 2 mg/dl. The median age of control patients was 61 (IQR 52–75) years. Sixteen patients were female (36 %). The median SOFA score on admission was 11 (IQR 8–12) and median SAPS II score was 61 (IQR 46–74). Twelve patients (27 %) died within 28 days following ICU admission. The SAPS II and SOFA scores did not differ significantly between the control group and the HH group (p = 0.87 and p = 0.78, respectively), although the SOFA score in cirrhotics was significantly higher (Table 1; p < 0.01) and SAPS score in ALF significantly lower (Table 1; p < 0.01).
The main clinical characteristics of patients with liver disease stratified according to 28-day surival are shown in Table 1.
Arterial ammonia levels
The laboratory features of the four study groups are illustrated in Table 2. Peak values of arterial ammonia were observed on day 2 (IQR 1–3 days) in HH and ALF patients, respectively, and on day 1 (IQR 1–3) in patients with cirrhosis following ICU admission. Distribution of measured peak arterial ammonia concentrations in 28-day survivors and non-survivors is shown in Fig. 1. The ESM figure illustrates the time course of arterial ammonia levels in the different study groups.
Arterial ammonia levels in survivors and non-survivors in the intensive care unit. Peak arterial ammonia levels in the four study groups (HH hypoxic hepatitis, ALF acute liver failure) categorized into transplant-free 28 day-survivors vs. non-survivors/transplanted patients. Box plot marks median (thick horizontal line), interquartile range (box) and extreme values (whiskers)
Arterial ammonia and 28-day mortality
The predictive value of arterial ammonia levels with respect to 28-day mortality or transplantation, respectively, is shown in Tables 1 and 4.
HH: arterial ammonia and 28-day mortality
There was a trend for lower arterial ammonia levels on admission in 28 day-survivors compared to non-survivors (p = 0.087; Table 1). Peak arterial ammonia levels were significantly higher in 28-day non-survivors (p = 0.0042; Table 1). Peak arterial ammonia concentrations of >75 μmol/l were significantly associated with 28-day mortality (Fig. 2). In the multivariate logistic regression analysis, peak arterial ammonia levels of >75 μmol/l remained an independent predictor of 28-day mortality [odds ratio (OR) 8.59, 95 % confidence interval (CI) 2.15–34.43), p < 0.01] after adjustment for the admission SOFA score and peak INR, which were also associated with 28-day mortality in the univariate analysis (Hosmer–Lemeshow test chi-square 7.2, df = 8, p = 0.52; Nagelkerke R 2 = 0.343).
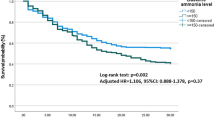
ALF: arterial ammonia and transplant-free 28-day survival
There was a trend for lower arterial ammonia concentrations in 28-day transplant-free survivors at admission (p = 0.101), whereas peak arterial ammonia levels were significantly lower in 28-day transplant-free survivors compared to patients who died or underwent liver transplantation (p = 0.00056; Table 1). The impact of peak arterial ammonia levels of >100 μmol/l is shown in a Kaplan–Meier plot (Fig. 2). After adjustment for SOFA score and peak INR, which were associated with 28-day mortality in the univariate analysis (Table 1), peak arterial ammonia levels of >100 μmol/l remained significantly linked to 28-day mortality or transplantation in the multivariate regression analysis (OR 11.21, 95 % CI 1.33–94.41, p < 0.05). (Hosmer–Lemeshow test chi-square 3.5, df = 8, p = 0.90; Nagelkerke R 2 = 0.663). Predictive values of peak arterial ammonia levels in comparison to commonly used scoring systems in ALF is shown in ESM Table 2.
Liver cirrhosis: arterial ammonia and 28-day mortality
Neither admission nor peak arterial ammonia levels differed significantly between 28-day non-survivors and 28-day survivors (p = 0.860 and p = 0.452, respectively; Table 1). The SOFA score (OR 1.23, 95 % CI 1.07–1.43, p < 0.01] and presence of septic shock (OR 3.72, 95 % CI 1.42-9.74, p < 0.01] remained significant predictors of 28-day mortality in the stepwise multivariate logistic regression model. (Hosmer–Lemeshow test chi-square 2.9, df = 8, p = 0.94, Nagelkerke R 2 = 0.307).
Controls: arterial ammonia and 28-day mortality
Admission and peak arterial ammonia concentrations, respectively, did not differ significantly between 28-day survivors and non-survivors [survivors: median 30 (IQR 27.2–34.6) vs. 35.6 (IQR 25.8–47.3) μmol/l, respectively, p = 0.204; non-survivors: median 39.6 (IQR 33.6–51.4) vs. 44.5 (IQR 32.7–55.6) μmol/l, respectively, p = 0.676]. The SOFA score differed significantly between 28-day survivors and non-survivors [median 9 (IQR 7–11) vs. 11.5 (IQR 11–14.75); p < 0.05].
Arterial ammonia and HE
Features of patients with and without advanced HE are illustrated in Table 3.
HH: arterial ammonia and signs of HE
Signs of HE were present in 12 of 35 patients who were included in the HE evaluation (Table 3). The prognostic value of arterial ammonia levels in predicting signs of HE in HH is shown in Table 4. None of the HH patients with signs of HE died from cerebral herniation, and the main causes of death in these patients were septic shock (n = 4), cardiogenic shock (n = 2), mixed cardiogenic and septic shock (n = 1) and cardiac arrest (n = 1).
ALF: arterial ammonia and HE
The predictive value of arterial ammonia levels in predicting HE grade 3/4 in ALF patients is shown in Tables 3 and 4. Twenty-six ALF patients were admitted to the ICU with HE ≤ grade 2, of whom 16 subsequently developed HE grades 3/4 and showed significantly higher arterial ammonia levels than those who did not [median 86.6 (IQR 67.3–123.7) vs. 60.0 (IQR 50.0–61.9) μmol/l, respectively; p < 0.01). The area under the receiver operating characteristic curve (AUROC) for admission arterial ammonia levels in predicting new onset of HE grades 3/4 in ALF was 0.825 (95 % CI 0.659–0.991, p < 0.01). There was a trend for higher SIRS scores in patients with peak HE grades3/4 compared to those with HE < grade 3 (Table 3).
Liver cirrhosis: arterial ammonia and encephalopathy
Both admission and peak ammonia levels were associated with peak HE grades 3/4 (Tables 3, 4). In patients who were admitted with HE ≤ grade 2, neither admission nor peak arterial ammonia levels predicted new onset of HE grades 3/4 (p = 0.69 and p = 0.43, respectively). Admission SIRS scores were significantly higher in cirrhotic patients admitted with HE ≤ grade 2 who subsequently developed HE grades 3/4 (median 3 (IQR 2.5–3.25) vs. 2 (IQR 1–2), respectively, p < 0.05). The AUROC for admission SIRS score in predicting new onset of HE grades 3/4 was 0.776 (95 % CI 0.568–0.984, p < 0.05). In the multivariate regression analysis, an admission SIRS score >2 (OR 9.65, 95 % CI 2.38–39.14, p < 0.01) and admission arterial ammonia levels of >75 μmol/l (OR 8.37, 95 % CI 1.81–38.78, p < 0.01) remained independent predictors for peak HE grades 3/4. (Hosmer–Lemeshow test chi-square 4.6, df = 2, p = 0.10, Nagelkerke R 2 = 0.382).
Discussion
To the best of our knowledge, this is the first study to compare the clinical impact of arterial ammonia levels among critically ill patients with different entities of liver disease.
Ammonia and 28-day mortality
Our results suggest that peak arterial ammonia values during the first 72 h following ICU admission are associated with 28-day mortality or transplantation, respectively, in patients with liver disease addmitted to the ICU (Table 1). However, the predictive value of arterial ammonia levels for 28-day mortality was restricted to HH and ALF among our patient cohort (Fig. 2). Neither admission nor peak arterial ammonia levels predicted 28-day mortality in our cirrhotic patients, which is in keeping with the results of previous studies [12, 37]. Chronic elevation of ammonia levels in cirrhosis would seem to abolish the predictive potential of ammonia observed in patients with acute liver injury.
Ammonia and HE
Both admission and peak arterial ammonia levels were associated with HE grades 3/4 independent of the etiology of liver disease (Table 3). Recent publications indicate that the SIRS score, but not arterial ammonia levels, differs significantly between cirrhotic patients with HE grade 3 and HE grade 4 [12]. In our exploratory analysis, arterial ammonia levels and admission SIRS scores were independently linked to HE grades 3/4 in our cirrhotic patients. This association may be explained by the different study populations observed (HE grades 3/4 in [12] vs. all cirrhotic patients with all grades of HE in our study population). Our results further support the crucial role of systemic inflammation for the development of HE in cirrhosis as high SIRS scores on admission were associated with new onset of HE grades 3/4 in cirrhotic patients initially presenting HE ≤ grade 2.
Arterial ammonia in clinical practice
High arterial ammonia levels are an active contributor to HE and a prognostic marker in patients with acute liver injury admitted to the ICU. However, it remains unclear whether a therapy targeting the lowering of ammonia levels would improve outcome. In ALF, treatment with l-ornithine-l-aspartate failed to lower ammonia levels or improve survival [38]. A recent meta-analysis of ten prospective trials investigating the use of extracorporeal liver support devices in ALF did not show significant survival benefits for patients treated with these devices, although an improvement in HE was observed [39]. Mechanisms other than HE seem to contribute to high mortality in ALF. Accordingly, we observed higher peak arterial ammonia levels in patients (HH, ALF and cirrhosis) requiring RRT versus those who did not [median 97.7 (IQR 61.2–162.8) vs. 73.2 (55.0–121.2) μmol/l, respectively; p < 0.05). Thus, patients showing high peak ammonia levels were more severely ill and required RRT more frequently. Future studies are needed to clarify potential benefits of targeted ammonia-lowering therapies, such as lactulose, rifaximin or even extracorporeal support systems, not only for patients with HE but also on survival in patients with HH and ALF.
There are several limitations to our study. First, the sample sizes of the patient groups were rather small, which limits the applicability of multivariate regression models. However, our sample sizes are comparable those of other studies in this field. Second, this study was conducted in a medical ICU. Thus, the conclusions drawn by the authors may not entirely be applicable to patients in surgical wards. Third, there was no blinding to arterial ammonia levels during HE assessment.
In conclusion, in our study elevated arterial ammonia levels were almost exclusively found in critically ill patients with acute and acute-on-chronic liver disease. High arterial ammonia levels predicted poor outcome in our HH and ALF patients and were associated with advanced encephalopathy in those patients with acute and acute-on-chronic liver disease. Future studies should clarify whether targeted ammonia-lowering interventions may improve outcome in critically ill patients with acute hepatic injury.
Abbreviations
- ALF:
-
Acute liver failure
- AUROC:
-
Area under receiver operating characteristic (ROC) curve
- CPR:
-
Cardiopulmonary resuscitation
- CT:
-
Computed tomography
- HE:
-
Hepatic encephalopathy
- HH:
-
Hypoxic hepatitis
- ICU:
-
Intensive care unit
- INR:
-
International normalized ratio
- MELD:
-
Model of end stage liver disease
- SIRS:
-
Systemic inflammatory response syndrome
- SAPS II:
-
Simplified acute physiology score II
- SOFA:
-
Sequential organ failure assessment score
References
Bernal W, Hall C, Karvellas CJ, Auzinger G, Sizer E, Wendon J (2007) Arterial ammonia and clinical risk factors for encephalopathy and intracranial hypertension in acute liver failure. Hepatology 46:1844–1852
Bhatia V, Singh R, Acharya SK (2006) Predictive value of arterial ammonia for complications and outcome in acute liver failure. Gut 55:98–104
Clemmesen JO, Larsen FS, Kondrup J, Hansen BA, Ott P (1999) Cerebral herniation in patients with acute liver failure is correlated with arterial ammonia concentration. Hepatology 29:648–653
Bernal W, Auzinger G, Dhawan A, Wendon J (2010) Acute liver failure. Lancet 376:190–201
Haussinger D (1986) Regulation of hepatic ammonia metabolism: the intercellular glutamine cycle. Adv Enzyme Regul 25:159–180
Haussinger D (1990) Nitrogen metabolism in liver: structural and functional organization and physiological relevance. Biochem J 267:281–290
Haussinger D (2006) Low grade cerebral edema and the pathogenesis of hepatic encephalopathy in cirrhosis. Hepatology 43:1187–1190
Lockwood AH, McDonald JM, Reiman RE, Gelbard AS, Laughlin JS, Duffy TE, Plum F (1979) The dynamics of ammonia metabolism in man. Effects of liver disease and hyperammonemia. J Clin Invest 63:449–460
Walker CO, Schenker S (1970) Pathogenesis of hepatic encephalopathy–with special reference to the role of ammonia. Am J Clin Nutr 23:619–632
Kundra A, Jain A, Banga A, Bajaj G, Kar P (2005) Evaluation of plasma ammonia levels in patients with acute liver failure and chronic liver disease and its correlation with the severity of hepatic encephalopathy and clinical features of raised intracranial tension. Clin Biochem 38:696–699
Jalan R, Olde Damink SW, Hayes PC, Deutz NE, Lee A (2004) Pathogenesis of intracranial hypertension in acute liver failure: inflammation, ammonia and cerebral blood flow. J Hepatol 41:613–620
Shawcross DL, Sharifi Y, Canavan JB, Yeoman AD, Abeles RD, Taylor NJ, Auzinger G, Bernal W, Wendon JA (2011) Infection and systemic inflammation, not ammonia, are associated with Grade 3/4 hepatic encephalopathy, but not mortality in cirrhosis. J Hepatol 54:640–649
Henrion J, Descamps O, Luwaert R, Schapira M, Parfonry A, Heller F (1994) Hypoxic hepatitis in patients with cardiac failure: incidence in a coronary care unit and measurement of hepatic blood flow. J Hepatol 21:696–703
Fuhrmann V, Kneidinger N, Herkner H, Heinz G, Nikfardjam M, Bojic A, Schellongowski P, Angermayr B, Kitzberger R, Warszawska J, Holzinger U, Schenk P, Madl C (2009) Hypoxic hepatitis: underlying conditions and risk factors for mortality in critically ill patients. Intensive Care Med 35:1397–1405
Fuhrmann V, Kneidinger N, Herkner H, Heinz G, Nikfardjam M, Bojic A, Schellongowski P, Angermayr B, Schoniger-Hekele M, Madl C, Schenk P (2011) Impact of hypoxic hepatitis on mortality in the intensive care unit. Intensive Care Med 37:1302–1310
Henrion J (2012) Hypoxic hepatitis. Liver Int 32:1039–1052
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European society of intensive care medicine. Intensive Care Med 22:707–710
Talmor M, Hydo L, Barie PS (1999) Relationship of systemic inflammatory response syndrome to organ dysfunction, length of stay, and mortality in critical surgical illness: effect of intensive care unit resuscitation. Arch Surg 134:81–87
Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, D’Amico G, Dickson ER, Kim WR (2001) A model to predict survival in patients with end-stage liver disease. Hepatology 33:464–470
Drolz AJB, Michl B, Furtmüller GJ, Wewalka M, Kitzberger R, Zauner C, Schenk P, Fuhrmann V (2010) Arterial ammonia in patients with hypoxic hepatitis. Intensive Care Med 36[Suppl 2]:380
Henrion J, Schapira M, Luwaert R, Colin L, Delannoy A, Heller FR (2003) Hypoxic hepatitis: clinical and hemodynamic study in 142 consecutive cases. Medicine (Baltimore) 82:392–406
Polson J, Lee WM (2005) AASLD position paper: the management of acute liver failure. Hepatology 41:1179–1197
O’Grady JG (2005) Acute liver failure. Postgrad Med J 81:148–154
Cash WJ, McConville P, McDermott E, McCormick PA, Callender ME, McDougall NI (2010) Current concepts in the assessment and treatment of hepatic encephalopathy. QJM 103:9–16
Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT (2002) Hepatic encephalopathy—definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998. Hepatology 35:716–721
Warren J, Fromm RE Jr, Orr RA, Rotello LC, Horst HM (2004) Guidelines for the inter- and intrahospital transport of critically ill patients. Crit Care Med 32:256–262
Wijdicks EF, Plevak DJ, Rakela J, Wiesner RH (1995) Clinical and radiologic features of cerebral edema in fulminant hepatic failure. Mayo Clin Proc 70:119–124
Inamasu J, Miyatake S, Suzuki M, Nakatsukasa M, Tomioka H, Honda M, Kase K, Kobayashi K (2010) Early CT signs in out-of-hospital cardiac arrest survivors: temporal profile and prognostic significance. Resuscitation 81:534–538
Naples R, Ellison E, Brady WJ (2009) Cranial computed tomography in the resuscitated patient with cardiac arrest. Am J Emerg Med 27:63–67
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent JL (2008) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 36:296–327
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31:1250–1256
Muckart DJ, Bhagwanjee S (1997) American college of chest physicians/society of critical care medicine consensus conference definitions of the systemic inflammatory response syndrome and allied disorders in relation to critically injured patients. Crit Care Med 25:1789–1795
Califf RM, Bengtson JR (1994) Cardiogenic shock. N Engl J Med 330:1724–1730
Goldberg RJ, Spencer FA, Gore JM, Lessard D, Yarzebski J (2009) Thirty-year trends (1975 to 2005) in the magnitude of, management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction: a population-based perspective. Circulation 119:1211–1219
Heinz G (2006) Cardiogenic shock–an inflammatory disease. Wien Klin Wochenschr 118:382–388
Shawcross DL, Davies NA, Williams R, Jalan R (2004) Systemic inflammatory response exacerbates the neuropsychological effects of induced hyperammonemia in cirrhosis. J Hepatol 40:247–254
Acharya SK, Bhatia V, Sreenivas V, Khanal S, Panda SK (2009) Efficacy of l-ornithine l-aspartate in acute liver failure: a double-blind, randomized, placebo-controlled study. Gastroenterology 136:2159–2168
Vaid A, Chweich H, Balk EM, Jaber BL (2012) Molecular adsorbent recirculating system as artificial support therapy for liver failure: a meta-analysis. ASAIO J 58:51–59
Acknowledgments
No financial support was received for this study.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Drolz, A., Jäger, B., Wewalka, M. et al. Clinical impact of arterial ammonia levels in ICU patients with different liver diseases. Intensive Care Med 39, 1227–1237 (2013). https://doi.org/10.1007/s00134-013-2926-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-2926-8