Abstract
Purpose
Bioactive NO carriers in circulating blood formed during NO inhalation selectively distribute blood flow to areas in need, and may thus improve collateral perfusion to the area-at-risk in acute myocardial infarction (AMI). Here, we tested the hypothesis that NO inhalation during the ischemic phase of AMI may improve left ventricular function and reduce infarct size in rats.
Methods
Following left anterior descending coronary artery (LAD) occlusion, rats received 50 ppm NO for 2 h of ischemia, during subsequent 3 h of reperfusion, or for 5 h of ischemia and reperfusion. Effects of inhaled NO were compared to those of intravenous nitrite as a putative carrier formed during NO inhalation. Downstream signaling via soluble guanylate cyclase was tested by inhibition with 1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one (ODQ).
Results
NO inhalation during myocardial ischemia increased left ventricular systolic pressure, contractility, relaxation, and cardiac output, and reduced myocardial infarction size and area-at-risk as compared to untreated controls. NO inhalation during the reperfusion phase caused a comparable protective effect. Combined inhalation during ischemia and reperfusion did not further improve left ventricular hemodynamics, but had an additive protective effect on the myocardial area-at-risk. NO inhalation increased circulating nitrite levels, and mimicking of this effect by intravenous nitrite infusion achieved similar protection as NO inhalation during myocardial ischemia, while ODQ blocked the protective NO effect.
Conclusions
Inhalation of NO during myocardial ischemia improves left ventricular function and reduces infarct size by mechanisms that increase levels of circulating nitrite and involve soluble guanylate cyclase. NO inhalation may represent a promising early intervention in AMI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In acute myocardial infarction (AMI), the time lag between ischemic insult and onset of reperfusion predicts myocardial infarct size (IS) and hence prognosis. Frequently, however, revascularization cannot occur within the critical interval of 12 h [1]. Current strategies to reduce morbidity and mortality from AMI therefore focus on logistic measures to shorten the time between AMI and revascularization, and on cardioprotective approaches to attenuate myocardial necrosis up to the time of revascularization. Yet, therapeutic interventions initiated after the onset of ischemia are hampered by the problem that systemically delivered drugs will not reach the infarcted tissue because of inadequate perfusion.
Increasing collateral perfusion to the infarcted area provides a promising alternative strategy, as it will increase oxygen and substrate delivery to the area-at-risk (AAR) surrounding the initial infarct core and thus attenuate the progression of IS. However, systemic vasodilators are contraindicated in AMI, as they will not selectively increase collateral perfusion, but instead redistribute blood flow from ischemic to healthy myocardium (“steal effect”) [2] while reducing coronary perfusion pressure [3].
Conversely, early interventions in AMI should aim to selectively improve perfusion to the AAR, thus causing an inversed steal adequately termed the Robin Hood effect [4]. In murine and ovine models of ischemic stroke, we recently realized this effect through inhalation of NO [5]. Inhaled NO (NOi) results in the formation of stable NO carriers in blood, namely nitrite [6, 7], which may conserve and circulate NO bioactivity and release NO when hemoglobin desaturates [8–10], thus redistributing blood flow preferentially to hypoxic tissues. Hence, we hypothesized that NOi may provide a novel and attractive therapeutic option for the treatment of AMI, and tested this concept in a rat model of AMI.
Materials and methods
Animals
Male Sprague–Dawley rats (375 ± 25 g body weight (bw)) were from Charles River (Sulzfeld, Germany). All animals received care in accordance with the Guide for the Care and Use of Laboratory Animals (National Academy Press, Washington, DC 1996). The study was approved by the Animal Care and Use Committee of the local government authorities.
Materials
All substances were from Sigma-Aldrich (Taufkirchen, Germany) unless stated otherwise.
Surgical preparation
Rats were anesthetized as described [11] and placed in supine position on a thermostatic blanket to maintain body temperature at 37.5 °C. Following tracheostomy, rats were ventilated at 70 breaths/min with peak inspiratory and positive end-expiratory pressures of 13.1 ± 1.1 and 5 cmH2O. Right carotid artery and left jugular vein were cannulated for hemodynamic monitoring, blood sampling, and drug delivery. A Mikro-Tip 2-F catheter was advanced from the carotid artery into the left ventricle for continuous recording of left ventricular pressure (LVP) and maximal and minimal rate of LVP change (dp/dt max and dp/dt min). For cardiac index (CI) measurements, a 250-μL bolus of 4 °C cold 0.9 % saline was injected into the right atrium via a catheter inserted from the right jugular vein, and detected by a thermocouple (IT-24P-Microprobe, Physitemp Instruments, Clifton, NJ) positioned in the aorta [12]. Thermodilution measurements were performed in triplicate. Following a midline thoracotomy, the pericardium was opened for left anterior descending coronary artery (LAD) ligation.
Experimental protocol
After 15 min stabilization, baseline hemodynamics were recorded, and arterial blood samples obtained. The LAD was reversibly ligated 2–3 mm from its origin [13], and AMI was evident as acute discoloration of the left ventricle. In experimental groups undergoing reperfusion, the ligature was removed after 120 min. Thirty minutes prior to euthanasia, a bolus of 30 mg Evans Blue (EB) was injected intravenously. Animals were euthanized by exsanguination, and hearts were excised for determination of AAR and IS.
The effects of NOi were studied first in myocardial ischemia alone, then in a model of 2 h of ischemia and 3 h of reperfusion, and finally in the presence of the soluble guanylate cyclase (sGC) inhibitor 1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one (ODQ) [14] (Fig. 1). Nitric oxide was inhaled at 50 ppm for indicated time intervals and the inspiratory NO concentration was continuously monitored (Dräger Pac 3, Dräger, Lübeck). ODQ (10 μg/kg bw) was administered intravenously [15] with the start of NO inhalation. In a subset of experiments, we mimicked the effects of NOi by intravenous nitrite infusion. To this end, we assessed nitrite concentrations in arterial blood during inhalation of 50 ppm NO using an ozone-based chemiluminescence detector (Model 280 nitric oxide analyzer; Sievers Instruments, Boulder, CO) [16–18]. Next, we tested different intravenous nitrite dosing strategies for their ability to reproduce similar plasma levels.
Schematic diagram of the experimental design. The effects of inhaled nitric oxide were assessed in models of myocardial ischemia (2 h), in myocardial ischemia (2 h) with subsequent reperfusion (3 h), and in the presence of the soluble guanylate cyclase inhibitor ODQ, respectively. Similarly, the effects of intravenous nitrite in acute myocardial ischemia (2 h) were determined. Time intervals of NO inhalation and nitrite infusion, respectively, are indicated by horizontal bars. Arrows indicate infusion of ODQ, arrowhead infusion of initial nitrite bolus
Quantification of myocardial area-at-risk and infarct size
Infarct size, i.e., the area in which the myocardium has succumbed to irreversible cell death, and AAR, i.e., the still viable yet unperfused myocardium surrounding the infarct core, were quantified by the EB and tetrazolium chloride staining techniques [19–21]. The left ventricle was cut into 5–6 horizontal slices (each 1.5 mm thick) perpendicular to the LAD axis. Each slice was weighed, immersed in 1 % triphenyl-tetrazolium chloride (TTC) for 20 min, and then bleached with 4 % formaldehyde for 30 min. Pre mortem infusion of EB stained perfused myocardium in blue, demarcating the border of the AAR, while TTC stains viable myocardium red. Consequentially, intact myocardium appears in dark violet, the AAR in red and the infarct core in white. AAR and IS were quantified as surface area in each slice by Image-J (NIH, Bethesda, MD), referred to slice weight, and expressed as percentage of left ventricular mass [22].
Statistical analyses
Data are presented as means ± SEMs. Values of different groups were compared by Mann–Whitney U test for two and Kruskal–Wallis and post hoc Dunn’s multiple comparison test for more than two independent groups, and by two-way repeated measures ANOVA for multiple testing at different time points. Statistical significance was assumed at P < 0.05.
Results
NOi improves left ventricular function in AMI
First, we tested the effect of NOi during 2 h of ischemia without reperfusion (Fig. 2, solid lines). In untreated controls, LAD occlusion caused an instantaneous decline in left ventricular function that was followed by a further deterioration over the 2-h ischemic interval, as demonstrated by the progressive decrease in mean arterial pressure (AP; Fig. 2a), left ventricular systolic pressure (LVSP; Fig. 2b), and the maximal pressure generation velocity dp/dt max as an indicator of left ventricular contractility (Fig. 2c). Left ventricular relaxation speed, reflected by dp/dt min, likewise decreased continuously (Fig. 2d). While the initial decline in left ventricular function after LAD occlusion was equally evident in rats inhaling NO, NOi effectively prevented the subsequent progressive hemodynamic deterioration, resulting in higher AP, LVSP, dp/dt max and lower dp/dt min values as compared to controls from t = 60 min after LAD occlusion. The beneficial effect of NOi was further evident as an attenuated decrease in CI 30 min after LAD occlusion (Fig. 2e). Hemodynamic differences were not attributable to NO effects on central venous pressure, which did not change significantly during experiments, or differed between groups (data not shown). As determination of IS by the TTC method is not feasible in the absence of tissue reperfusion [23], EB staining demarcated a combination of AAR and IS. In untreated controls, this non-perfused area covered approximately 50 % of the left ventricle, while NOi reduced AAR + IS by more than 20 % (Fig. 2f, g).
Protective effect of NO inhalation during myocardial ischemia. Rats were subjected to either 2 h of ischemia only (I; solid lines in a–e) or 2 h of ischemia, followed by 3 h of reperfusion (I/R; dotted lines). Values between baseline and 90 min show combined data from both I and I/R groups. Concurrent with the onset of ischemia, rats in both I and I/R groups received inhaled NO (50 ppm; I (NO) or I/R (NO–I)) or room air (I (control) or I/R (control)) during the 2-h ischemic interval. Group data show mean arterial pressure (a), left ventricular systolic pressure (b), dp/dt max (c), and dp/dt min (d) determined at baseline and 0, 5, 30, 60, 90, and 120 min after LAD occlusion and 60, 120, and 180 min after initiation of reperfusion. Cardiac index (e) was determined at baseline, 30 and 90 min after LAD occlusion and 60 min after the onset of reperfusion. f Representative TTC- and EB-stained left ventricular sections obtained either after 2 h of ischemia (I) or 2 h of ischemia and 3 h of reperfusion (I/R) in rats inhaling either NO (NO) or room air (control) during the ischemic interval show normal perfused myocardium in dark violet, viable area-at-risk in red, and the necrotic infarct core in white. G Bar graphs show the combined area-at-risk and infarct size determined after 2 h of ischemia only, or area-at-risk and infarct size as determined after 2 h of ischemia and 3 h of reperfusion. *P < 0.05 versus corresponding control, n = 8 animals each
Beneficial effect of NOi is preserved after reperfusion
Next, we addressed whether NO inhalation during ischemia confers protection that extends over a subsequent 3-h reperfusion period without NOi (Fig. 2, dotted lines). Myocardial reperfusion caused a rapid, albeit incomplete, recovery of systemic (Fig. 2a) and left ventricular (Fig. 2b–d) hemodynamic pressures in both control and NOi-treated rats, followed by a subsequent decline in line with progressive reperfusion injury. Cardiac index spontaneously recovered in part during ischemia, and continued to increase gradually during reperfusion (Fig. 2e). In rats who received NOi during the ischemic interval, AP and CI consistently exceeded respective values in untreated controls during reperfusion. A similar beneficial trend was evident for left ventricular hemodynamics (LVSP, dp/dt max, dp/dt min), yet only reached significance for LVSP and dp/dt max at 300 min. AAR and IS were markedly reduced in NOi rats, demonstrating that the beneficial effect of NOi during ischemia was preserved throughout subsequent reperfusion (Fig. 2f, g). Notably, NOi also reduced the ratio IS/AAR from 0.59 ± 0.05 to 0.45 ± 0.04 (P < 0.05), indicating that the protective effect of NOi was not solely attributable to improved collateral blood flow as demonstrated by the reduced AAR, but also to potential cardioprotective effects [24–26].
Continuous NOi during ischemia and reperfusion has additive benefit on area-at-risk
As NOi during reperfusion has previously been shown to reduce IS and improve myocardial perfusion [27, 28], we tested whether continuous NOi during both ischemia and reperfusion may provide additive benefits as compared to NOi during either ischemia or reperfusion. Inhaled nitric oxide during reperfusion alone improved systemic (Fig. 3a, e) and left ventricular (Fig. 3b–d) hemodynamics, and reduced AAR and IS (Fig. 3f). With respect to AP and left ventricular hemodynamics, the beneficial effects of NOi during either ischemia or reperfusion were largely comparable. However, CI after 90 min ischemia was higher in rats receiving NOi during ischemia as compared to NOi during reperfusion, and this difference was preserved for at least 1 h into the reperfusion period. More importantly, NOi during reperfusion resulted only in a moderate reduction of IS by 21 %, a non-significant decrease in AAR, and no reduction in the ratio IS/AAR. Conversely, NOi during ischemia decreased AAR, IS, and the ratio IS/AAR by 22, 41, and 24 %, respectively, and thus exerted a pronounced protective effect. Continuous inhalation of NO during both ischemia and reperfusion did not generate a detectable additive benefit as compared to NOi during either ischemia or reperfusion with respect to systemic or left ventricular hemodynamics. Yet, continuous NOi resulted in the most distinctive reduction in AAR, which was superior to NOi during each interval alone. A similar trend was observed for IS, which was lower as compared to NOi during reperfusion, and just failed to reach significance versus NOi during ischemia (P = 0.065).
Continuous NO inhalation during ischemia and reperfusion has additive benefit on area-at-risk. Following LAD occlusion, rats received inhaled NO (50 ppm) either only during the 2-h ischemic interval (I/R (NO–I)), only during the 3-h reperfusion interval (I/R (NO–R)), or continuously during 5 h of ischemia-reperfusion (I/R (NO–I/R)). Controls (I/R (control)) inhaled room air during both ischemia and reperfusion. Bar graphs show mean arterial pressure (a), left ventricular systolic pressure (b), dp/dt max (c), dp/dt min (d), area-at-risk, infarct size, and the ratio IS/AAR (all f) as determined after 2 h of ischemia and 3 h of reperfusion. Cardiac index (e) was determined at baseline, 30 and 90 min after LAD occlusion and 60 min after the onset of reperfusion. *P < 0.05 versus I/R (control), #P < 0.05 versus I/R (NO–R), †P < 0.05 versus I/R (NO–I), n = 8 animals each
Beneficial effects of NOi are mediated by sGC
To address the involvement of the sGC–cGMP pathway in the observed beneficial effects, we administered the sGC inhibitor ODQ at the start of NO inhalation. As ODQ by itself may exert hemodynamic effects, subsequent comparisons were confined to differences between ODQ-treated groups. In ODQ-treated rats, inhalation of NO no longer exerted detectable beneficial effects on systemic (Fig. 4a, e) or left ventricular (Fig. 4b–d) hemodynamics, AAR, or IS (Fig. 4f).
Beneficial effects of NO inhalation are mediated by soluble guanylate cyclase. Concurrent with the onset of ischemia, rats received an intravenous bolus of the soluble guanylate cyclase inhibitor ODQ (10 μg/kg bw), followed by inhalation of either NO (50 ppm; ODQ (NO)) or room air (ODQ (control)) during the 2-h ischemic and the subsequent 3-h reperfusion interval. Group data show mean arterial pressure (a), left ventricular systolic pressure (b), dp/dt max (c), and dp/dt min (d) determined at baseline, 0, 5, 30, 60, 90, and 120 min after LAD occlusion and 60, 120, and 180 min after initiation of reperfusion and cardiac index (e) determined at baseline, 30 and 90 min after LAD occlusion and 60 min after the onset of reperfusion, respectively. Bar graph shows (f) area-at-risk and infarct size determined after 2 h of ischemia and 3 h of reperfusion. No significant differences between ODQ (NO) and ODQ (control), n = 8 animals each
Infusion of nitrite iterates the protective effect of NOi
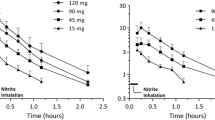
Last, we tested whether the beneficial effect of NOi may be due to formation of nitrite and mimicked by its systemic delivery. While plasma nitrite levels remained unchanged over 2 h in untreated controls undergoing LAD occlusion, inhalation of 50 ppm NO increased nitrite levels by sixfold (Fig. 5a). On the basis of published pharmacokinetic profiles of intravenous nitrite in rats [29], we tested dosing regimens for nitrite infusion with an initial bolus of 0.5–4 nmol/g bw and subsequent continuous infusion of 10 % of the initial dose per min. Combination of an initial 0.5 nmol/g bw bolus followed by infusion of 0.05 nmol g bw−1 min−1 mimicked the effects of 50 ppm NOi, in that it yielded a stable increase in plasma nitrite levels within the range measured during NO inhalation (Fig. 5b). When this dose was applied during 2 h of LAD occlusion, nitrite prevented the progressive decline and in part even restored pre-ischemic levels of systemic (Fig. 5c, g) and left ventricular hemodynamics (Fig. 5d–f), and markedly reduced the percentage of non-perfused left ventricular tissue (Fig. 5h). These findings demonstrate that systemic nitrite levels comparable to those achieved during NO inhalation exert similar protective effects as NOi.
Nitrite infusion iterates the protective effect of NO inhalation. a Nitrite levels were determined by chemiluminescence in rat plasma obtained before or 2 h after induction of AMI in rats receiving inhaled NO (50 ppm; I (NO)) or room air (I (control)). *P < 0.05 versus I (control), n = 8 animals each. b Nitrite levels in rat plasma as determined immediately after intravenous bolus infusion of 0.5, 1, 2, or 4 nmol/g bw nitrite, and 60 and 120 min after subsequent continuous infusion of 10 % of the initial bolus dose per min (n = 4 animals each). Upper and lower limits and average nitrite levels as measured during NO inhalation are indicated by dashed and dotted lines, respectively. In a subsequent set of experiments, rats received an initial nitrite bolus of 0.5 nmol g bw−1 with the onset of ischemia, followed by subsequent continuous infusion at 0.05 nmol g bw−1 min−1 (I (nitrite)) or an equal volume of saline (I (control)) during the 2-h ischemic interval. Group data show mean arterial pressure (c), left ventricular systolic pressure (d), dp/dt max (e), and dp/dt min (f) determined at baseline and 0, 5, 30, 60, 90, and 120 min after LAD occlusion and cardiac index (g) determined at baseline, 30 and 90 min after LAD occlusion, respectively. Bar graph shows the combined area-at-risk and infarct size (h) determined after 2 h of ischemia. *P < 0.05 versus I (control), n = 8 animals each
Discussion
Here, we identify NOi as an emerging early intervention strategy in AMI. In an in vivo rat model of AMI, we demonstrate that NOi during myocardial ischemia improves left ventricular function and systemic hemodynamics and reduces AAR and IS. This protection was to a large degree attributable to improved collateral perfusion, as demonstrated by the findings that NOi reduced AAR, and that this effect markedly, albeit not exclusively, accounted for the resulting decrease in IS. This property of NOi is in line with our recent demonstration of an NOi-induced Robin Hood effect in ischemic stroke [5], and diametrically opposed to the detrimental steal effects exerted by conventional (nitro-)vasodilators in AMI [2]. The protective effect of NOi exceeded the actual time interval of drug inhalation and was preserved over a subsequent 3-h reperfusion phase in the absence of NOi, attesting to a sustained treatment benefit. Extension of NO inhalation into the reperfusion phase further reduced AAR, indicating that prolonged NO inhalation during both ischemia and reperfusion may have additive therapeutic effects. Inhaled nitric oxide effects were blocked by sGC inhibition, confirming that improvement of myocardial function and viability was mediated via the NO–sGC–cGMP axis. Mimicking of the NOi-induced increase in systemic nitrite levels by intravenous nitrite replicated the beneficial effects of NOi, suggesting nitrite as a putative biocarrier of NO activity.
While NOi was originally considered to act exclusively in the lung owing to its short half-life in vivo, several studies have demonstrated extrapulmonary effects of NOi such as increased cerebral blood volume in pigs [30], and increased forearm blood flow in healthy human volunteers [31]. These effects have been attributed to the formation and transport of bioactive NO carriers with the circulating blood which may occur in the form of S-nitrosated proteins [32] and in particular as nitrite which is present in relative abundance in both blood and tissue [33]. Circulating nitrite may again release NO at low oxygen tension owing to the oxygenation-dependent function of hemoglobin as a nitrite reductase [34]. As a result, increased amounts of circulating nitrite as generated by NOi will release NO and induce vasodilation preferentially in areas of tissue hypoxia. In murine and ovine stroke models, we recently provided proof-of-principle for this NOi-induced Robin Hood effect and thus identified NOi as a promising early intervention strategy in tissue ischemia [5].
Here, we show that this approach is equally beneficial in experimental AMI, in that NOi at a clinically relevant concentration of 50 ppm prevented the progressive decline of left ventricular function and systemic perfusion, and reduced AAR and IS. In line with the reported Robin Hood effect in ischemic stroke, the vasodilatory effect of NOi in ischemic myocardium, evident as a decrease in AAR, was not associated with a decrease in total peripheral vascular resistance (data not shown) and increased rather than reduced systemic arterial pressure. However, owing to methodological constraints in the beating rodent heart, the specificity of the vasodilatory effect for the ischemic area that is characteristic for the Robin Hood effect can at this stage not be spatially resolved. Notably, the observed hemodynamic stabilization is in line with previous data attesting to the clinical safety of NOi in patients with AMI and associated cardiogenic shock where NOi did not aggravate systemic arterial hypotension and in contrast increased cardiac index [35].
In line with the proposed role of nitrite as a bioactive NO carrier, NOi increased circulating nitrite levels by sixfold, and elevation of plasma nitrite to comparable levels by intravenous nitrite infusion replicated the effects of NOi. While this finding does not preclude a contribution of other bioactive NO-carriers in blood, it suggests a critical role for nitrite in this scenario. Notably, nitrite has previously proven protective in animal models of ischemia-reperfusion including the heart, liver, and brain [25, 36, 37]. Yet in contrast to the concept of increased collateral perfusion during ischemia these effects were at large attributed to cytoprotective effects during reperfusion due to an NO-dependent modulation of mitochondrial reactive oxygen species production [24–26]. Accordingly, nitrite administration in these studies was either timed to the onset of reperfusion [24, 25, 36, 37], or nitrite was given prophylactically as a dietary supplement [25, 38, 39]. In contrast, the present study was designed to specifically deliver NO (or nitrite) during ischemia with the declared aim to exploit the proposed Robin Hood effect. The effectiveness of this approach was evident in that NOi caused a marked reduction in AAR, thus directly demonstrating improved perfusion of the myocardium surrounding the infarct core. This effect accounted largely, albeit not exclusively, for the decrease in IS which was 41 % larger than would be expected from the 22 % reduction in AAR alone, suggesting that aforementioned cytoprotective effects of nitrite may have added to the beneficial effect.
While restriction of NO inhalation to the ischemic interval could not prevent subsequent reperfusion injury as indicated by the parallel decline in hemodynamic parameters in both the NOi and the corresponding control group during reperfusion (Fig. 2), the benefits gained by NO inhalation during the period of ischemic injury were largely preserved during subsequent reperfusion. This finding attests to the fact that bridging of the ischemic interval by NOi may provide long-lasting benefits in AMI, which could be therapeutically supplemented by additional interventions targeted specifically at the reperfusion phase. Hemodynamic effects of NO inhalation during reperfusion were largely equipotent to those of NOi during ischemia, a finding that is in line with previously reported beneficial effects of NOi during myocardial reperfusion that have been attributed to anti-inflammatory and anti-aggregatory effects of NO [27, 28, 40]. However, reductions in AAR, IS, and the IS/AAR ratio were more prominent when NO was delivered during ischemia rather than reperfusion. Myocardial protection was further enhanced when NO was administered continuously, a finding that is in line with the different proposed mechanisms of action during ischemia (improved collateral perfusion) and reperfusion (anti-inflammatory and -aggregatory) that may provide synergistic benefits. The fact that the sGC inhibitor ODQ completely prevented the effect of NOi confirms that NOi conferred its beneficial effects by stimulation of the sGC–cGMP pathway.
The present data identify a protective effect of NOi in myocardial ischemia and reperfusion which—in contrast to existing paradigms—focuses on the ischemic rather than the reperfusion phase. Inhalation of this clinically approved gas may be rapidly implementable as a first-line interventional strategy with the dual-pronged approach to either prolong cell survival in the AAR up to the time of interventional reperfusion, or to reduce total IS in cases where timely revascularization is not feasible.
References
Schomig A, Ndrepepa G, Kastrati A (2006) Late myocardial salvage: time to recognize its reality in the reperfusion therapy of acute myocardial infarction. Eur Heart J 27:1900–1907
Harrison DG, Bates JN (1993) The nitro vasodilators. New ideas about old drugs. Circulation 87:1461–1467
Moore PG, Nguyen DK, Reitan JA (1994) Inhibition of nitric oxide synthesis causes systemic and pulmonary vasoconstriction in isoflurane-anesthetized dogs. J Cardiothorac Vasc Anesth 8:310–316
Crea F, Pupita G, Galassi AR, el-Tamimi H, Kaski JC, Davies GJ, Maseri A (1989) Comparative effects of theophylline and isosorbide dinitrate on exercise capacity in stable angina pectoris, and their mechanisms of action. Am J Cardiol 64:1098–1102
Terpolilli NA, Kim SW, Thal SC, Kataoka H, Zeisig V, Nitzsche B, Klaesner B, Zhu C, Schwarzmaier S, Meissner L, Mamrak U, Engel DC, Drzezga A, Patel RP, Blomgren K, Barthel H, Boltze J, Kuebler WM, Plesnila N (2012) Inhalation of nitric oxide prevents ischemic brain damage in experimental stroke by selective dilatation of collateral arterioles. Circ Res 110:727–738
Demoncheaux EA, Higenbottam TW, Foster PJ, Borland CD, Smith AP, Marriott HM, Bee D, Akamine S, Davies MB (2002) Circulating nitrite anions are a directly acting vasodilator and are donors for nitric oxide. Clin Sci (Lond) 102:77–83
Lundberg JO, Gladwin MT, Ahluwalia A, Benjamin N, Bryan NS, Butler A, Cabrales P, Fago A, Feelisch M, Ford PC, Freeman BA, Frenneaux M, Friedman J, Kelm M, Kevil CG, Kim-Shapiro DB, Kozlov AV, Lancaster JR Jr, Lefer DJ, McColl K, McCurry K, Patel RP, Petersson J, Rassaf T, Reutov VP, Richter-Addo GB, Schechter A, Shiva S, Tsuchiya K, van Faassen EE, Webb AJ, Zuckerbraun BS, Zweier JL, Weitzberg E (2009) Nitrate and nitrite in biology, nutrition and therapeutics. Nat Chem Biol 5:865–869
Cantu-Medellin N, Vitturi DA, Rodriguez C, Murphy S, Dorman S, Shiva S, Zhou Y, Jia Y, Palmer AF, Patel RP (2011) Effects of T- and R-state stabilization on deoxyhemoglobin–nitrite reactions and stimulation of nitric oxide signalling. Nitric Oxide 25:59–69
Cosby K, Partovi KS, Crawford JH, Patel RP, Reiter CD, Martyr S, Yang BK, Waclawiw MA, Zalos G, Xu X, Huang KT, Shields H, Kim-Shapiro DB, Schechter AN, Cannon RO, Gladwin MT (2003) Nitrite reduction to nitric oxide by deoxyhemoglobin vasodilates the human circulation. Nat Med 9:1498–1505
Gladwin MT (2008) Evidence mounts that nitrite contributes to hypoxic vasodilation in the human circulation. Circulation 117:594–597
Bueltmann M, Kong X, Mertens M, Yin N, Yin J, Liu Z, Koster A, Kuppe H, Kuebler WM (2009) Inhaled milrinone attenuates experimental acute lung injury. Intensive Care Med 35:171–178
Morita Y, Yu P, Martin CM (2000) An alternative thermodilution method to measure cardiac output in a rat model of stagnant hypoxia. Shock 14:550–554
Remondino A, Rosenblatt-Velin N, Montessuit C, Tardy I, Papageorgiou I, Dorsaz PA, Jorge-Costa M, Lerch R (2000) Altered expression of proteins of metabolic regulation during remodelling of the left ventricle after myocardial infarction. J Mol Cell Cardiol 32:2025–2034
Garthwaite J, Southam E, Boulton CL, Nielsen EB, Schmidt K, Mayer B (1995) Potent and selective inhibition of nitric oxide-sensitive guanylyl cyclase by 1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one. Mol Pharmacol 48:184–188
Garcia M, Moran A, Luisa MM, Barthelmebs M, San RL (2006) The nitric oxide synthesis/pathway mediates the inhibitory serotoninergic responses of the pressor effect elicited by sympathetic stimulation in diabetic pithed rats. Eur J Pharmacol 537:126–134
MacArthur PH, Shiva S, Gladwin MT (2007) Measurement of circulating nitrite and S-nitrosothiols by reductive chemiluminescence. J Chromatogr B Analyt Technol Biomed Life Sci 851:93–105
Wang X, Bryan NS, MacArthur PH, Rodriguez J, Gladwin MT, Feelisch M (2006) Measurement of nitric oxide levels in the red cell: validation of tri-iodide-based chemiluminescence with acid-sulfanilamide pretreatment. J Biol Chem 281:26994–27002
Pelletier MM, Kleinbongard P, Ringwood L, Hito R, Hunter CJ, Schechter AN, Gladwin MT, Dejam A (2006) The measurement of blood and plasma nitrite by chemiluminescence: pitfalls and solutions. Free Radic Biol Med 41:541–548
Fishbein MC, Meerbaum S, Rit J, Lando U, Kanmatsuse K, Mercier JC, Corday E, Ganz W (1981) Early phase acute myocardial infarct size quantification: validation of the triphenyl tetrazolium chloride tissue enzyme staining technique. Am Heart J 101:593–600
Hu X, Xu C, Zhou X, He B, Wu L, Cui B, Lu Z, Jiang H (2010) Sodium butyrate protects against myocardial ischemia and reperfusion injury by inhibiting high mobility group box 1 protein in rats. Biomed Pharmacother. doi:10.1016/j.biopha.2010.09.005
Khalil PN, Siebeck M, Huss R, Pollhammer M, Khalil MN, Neuhof C, Fritz H (2006) Histochemical assessment of early myocardial infarction using 2,3,5-triphenyltetrazolium chloride in blood-perfused porcine hearts. J Pharmacol Toxicol Methods 54:307–312
Richard V, Kaeffer N, Tron C, Thuillez C (1994) Ischemic preconditioning protects against coronary endothelial dysfunction induced by ischemia and reperfusion. Circulation 89:1254–1261
Schwarz ER, Somoano Y, Hale SL, Kloner RA (2000) What is the required reperfusion period for assessment of myocardial infarct size using triphenyltetrazolium chloride staining in the rat? J Thromb Thrombolysis 10:181–187
Hendgen-Cotta UB, Merx MW, Shiva S, Schmitz J, Becher S, Klare JP, Steinhoff HJ, Goedecke A, Schrader J, Gladwin MT, Kelm M, Rassaf T (2008) Nitrite reductase activity of myoglobin regulates respiration and cellular viability in myocardial ischemia-reperfusion injury. Proc Natl Acad Sci U S A 105:10256–10261
Shiva S, Sack MN, Greer JJ, Duranski M, Ringwood LA, Burwell L, Wang X, MacArthur PH, Shoja A, Raghavachari N, Calvert JW, Brookes PS, Lefer DJ, Gladwin MT (2007) Nitrite augments tolerance to ischemia/reperfusion injury via the modulation of mitochondrial electron transfer. J Exp Med 204:2089–2102
Shiva S, Gladwin MT (2009) Nitrite mediates cytoprotection after ischemia/reperfusion by modulating mitochondrial function. Basic Res Cardiol 104:113–119
Liu X, Huang Y, Pokreisz P, Vermeersch P, Marsboom G, Swinnen M, Verbeken E, Santos J, Pellens M, Gillijns H, Van de Werf F, Bloch KD, Janssens S (2007) Nitric oxide inhalation improves microvascular flow and decreases infarction size after myocardial ischemia and reperfusion. J Am Coll Cardiol 50:808–817
Hataishi R, Rodrigues AC, Neilan TG, Morgan JG, Buys E, Shiva S, Tambouret R, Jassal DS, Raher MJ, Furutani E, Ichinose F, Gladwin MT, Rosenzweig A, Zapol WM, Picard MH, Bloch KD, Scherrer-Crosbie M (2006) Inhaled nitric oxide decreases infarction size and improves left ventricular function in a murine model of myocardial ischemia-reperfusion injury. Am J Physiol Heart Circ Physiol 291:H379–H384
Basireddy M, Isbell TS, Teng X, Patel RP, Agarwal A (2006) Effects of sodium nitrite on ischemia-reperfusion injury in the rat kidney. Am J Physiol Renal Physiol 290:F779–F786
Kuebler WM, Kisch-Wedel H, Kemming GI, Meisner F, Bruhn S, Koehler C, Flondor M, Messmer K, Zwissler B (2003) Inhaled nitric oxide induces cerebrovascular effects in anesthetized pigs. Neurosci Lett 348:85–88
Cannon RO, Schechter AN, Panza JA, Ognibene FP, Pease-Fye ME, Waclawiw MA, Shelhamer JH, Gladwin MT (2001) Effects of inhaled nitric oxide on regional blood flow are consistent with intravascular nitric oxide delivery. J Clin Invest 108:279–287
Stamler JS, Simon DI, Osborne JA, Mullins ME, Jaraki O, Michel T, Singel DJ, Loscalzo J (1992) S-Nitrosylation of proteins with nitric oxide: synthesis and characterization of biologically active compounds. Proc Natl Acad Sci U S A 89:444–448
Gladwin MT, Schechter AN (2004) NO contest: nitrite versus S-nitroso-haemoglobin. Circ Res 94:851–855
Huang Z, Shiva S, Kim-Shapiro DB, Patel RP, Ringwood LA, Irby CE, Huang KT, Ho C, Hogg N, Schechter AN, Gladwin MT (2005) Enzymatic function of haemoglobin as a nitrite reductase that produces NO under allosteric control. J Clin Invest 115:2099–2107
Inglessis I, Shin JT, Lepore JJ, Palacios IF, Zapol WM, Bloch KD, Semigran MJ (2004) Hemodynamic effects of inhaled nitric oxide in right ventricular myocardial infarction and cardiogenic shock. J Am Coll Cardiol 44:793–798
Duranski MR, Greer JJ, Dejam A, Jaganmohan S, Hogg N, Langston W, Patel RP, Yet SF, Wang X, Kevil CG, Gladwin MT, Lefer DJ (2005) Cytoprotective effects of nitrite during in vivo ischemia-reperfusion of the heart and liver. J Clin Invest 115:1232–1240
Jung KH, Chu K, Ko SY, Lee ST, Sinn DI, Park DK, Kim JM, Song EC, Kim M, Roh JK (2006) Early intravenous infusion of sodium nitrite protects brain against in vivo ischemia-reperfusion injury. Stroke 37:2744–2750
Bryan NS, Calvert JW, Elrod JW, Gundewar S, Ji SY, Lefer DJ (2007) Dietary nitrite supplementation protects against myocardial ischemia-reperfusion injury. Proc Natl Acad Sci U S A 104:19144–19149
Raat NJ, Noguchi AC, Liu VB, Raghavachari N, Liu D, Xu X, Shiva S, Munson PJ, Gladwin MT (2009) Dietary nitrate and nitrite modulate blood and organ nitrite and the cellular ischemic stress response. Free Radic Biol Med 47:510–517
Nagasaka Y, Fernandez BO, Garcia-Saura MF, Petersen B, Ichinose F, Bloch KD, Feelisch M, Zapol WM (2008) Brief periods of nitric oxide inhalation protect against myocardial ischemia-reperfusion injury. Anesthesiology 109:675–682
Acknowledgments
This study was supported by the Canadian Institutes of Health Research (CIHR MOP #93584), the Heart and Stroke Foundation Ontario (NA #6900), and the McLaughlin Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Neye, N., Enigk, F., Shiva, S. et al. Inhalation of NO during myocardial ischemia reduces infarct size and improves cardiac function. Intensive Care Med 38, 1381–1391 (2012). https://doi.org/10.1007/s00134-012-2605-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2605-1