Abstract
Purpose
Non-invasive continuous positive airway pressure (CPAP) is effective in reducing intubation rate and mortality of patient with acute cardiogenic pulmonary edema (ACPE). We report our experience on pre-hospital application of CPAP by helmet as an adjunct to medical therapy or as a stand alone procedure in patient with presumed ACPE.
Methods
In pre-hospital treatment of 62 patients with presumed ACPE, CPAP was added to standard medical treatment while in another 59 patients, CPAP was used as a sole therapy.
Results
Helmet CPAP was feasible in all patients. No patient required pre-hospital intubation. In both groups, CPAP significantly improved oxygenation (SpO2 went from 79 ± 12 to 97 ± 3% and from 81 ± 13 to 98 ± 3%), reduced respiratory rate (from 26 ± 4 to 21 ± 3 bpm and from 30 ± 9 to 22 ± 8 bpm) and improved hemodynamics, with a more pronounced decrease in blood pressure in the group with medical treatment than in the one without it. In the two cohorts, four and five patients were, respectively, intubated in Emergency Department and 11 and 9 eventually died.
Conclusions
Helmet CPAP is feasible, efficient and safe in pre-hospital treatment of presumed ACPE. A significant improvement of physiological variables was observed also in the group treated with CPAP in the absence of a drug therapy. We propose helmet CPAP as first line pre-hospital treatment of presumed severe ACPE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Respiratory distress is the second most common symptom of adults transported by ambulance and acute cardiogenic pulmonary edema (ACPE) is one of the leading causes of respiratory distress in cardiac patients [1]. In hospital, non-invasive continuous positive airway pressure (CPAP) has proven effective in ameliorating gas exchange and reducing both the need for endotracheal intubation and the overall mortality of patients with ACPE, as suggested by randomized controlled trials and a recent meta-analysis [2–10], although this result has been challenged by a large multicenter trial [11].
With the understanding that immediate advanced medical care is essential to improve the long-term outcome of cardiac patients, we developed a program for the pre-hospital application of CPAP. A similar approach to patients with ACPE has been recently described by Plaisance and co-workers [12]. The study showed that CPAP alone was more effective than medical treatment alone in improving the respiratory function. Moreover, a delayed application of CPAP appeared to be associated with increased intra-hospital mortality.
CPAP is commonly applied through face masks requiring a tight seal to the patient’s face to prevent air leaks and loss of pressure. The application of a face mask requires patient cooperation, an experienced team, and either a reservoir chamber or a high-flow gas source to achieve a constant airway pressure and inspired oxygen fraction. Moreover, face masks are sometimes impossible to use owing to peculiar patient’s characteristics (e.g., in an edentulous patient, or in those wearing a beard); they are sometimes uncomfortable or poorly tolerated, possibly limiting the duration of application [13–15]. The correct application of face masks is therefore somehow difficult even in an intensive care unit (ICU) or in the emergency room (ER), and it may be very problematic or ineffective in the pre-hospital setting.
We therefore selected the helmet for pre-hospital CPAP application: it appears to be as effective as face mask [16], easily applied, well tolerated and clinically beneficial [14, 17, 18].
We report here our experience and observations about the pre-hospital application of helmet CPAP in patient with presumed ACPE. We will discuss:
-
1.
the feasibility, safety, and efficacy of helmet CPAP.
-
2.
the effects of helmet CPAP as an addition to standard medical therapy or as a stand alone treatment.
Methods
The emergency medical system (EMS) of Monza–Brianza
This study was approved by the institutional review board for collecting data from the patient’s medical records. The study was conducted in Brianza, a region located in Lombardia, Italy. All EMS activities are co-ordinated by a local operative center (SSUEM) dispatches a Basic Life Support, and in selected cases (including reported respiratory distress) an advanced life support (ALS) team.
Basic life support teams are staffed by three specifically trained lay volunteers; ALS teams can be staffed either with a technician, a nurse and a physician (ALSdoc) or with two volunteers and a nurse (ALSnurs). According to the Italian legislation at the time of the study, ALSnurs might only perform limited therapeutic interventions and no drug administration. ALSdoc and ALSnurs teams cover different areas and are dispatched according solely to the site of origin of the call. All the ALS crews underwent a 4 h training course on the use of the helmet device.
Patients
We enrolled patients with suspected ACPE rescued by ALSdoc between 1 December 1998 and 31 December 1999 and patients treated by ALSnurs between 1 February 2001 and 1 December 2002.
Protocol
Inclusion and exclusion criteria are reported in Table 1.
The diagnosis of suspected ACPE was based on the medical history positive for cardiovascular disease and physical examinations including orthopnea, diffuse crackles without evidence of pulmonary aspiration of infection, and pulse oximetry. In the ALSnurs group, the diagnosis was always validated on the phone by the physician in charge at the SSUEM. In the ALSdoc group, the severity of ACPE was also assessed by means of a “Wet Rales Score” (WRS), ranging from 1 to 4, based on the extension of crackles and/or rales evaluated at chest auscultation.
Upon arrival, the ALS team administered supplemental oxygen via a bag mask at 15 L/min, secured a venous line and (in the ALSdoc group) pharmacological therapy was started according to ACLS guidelines. ALSnurs avoided drug administration. In the vast majority of cases oxygen administration had been started by basic life support crews before ALS arrival. Respiratory rate, heart rate, non-invasive arterial pressure, pulse oximetry, and WRS were recorded. If the protocol criteria were met, CPAP was applied while medical therapy was continued as indicated. Vital parameters were monitored throughout all transportation period and the final reading upon arrival in the ER was recorded and used for data analysis.
Helmet CPAP was discontinued in case of a worsening level of consciousness, shock, intolerance or whenever endotracheal intubation was required.
In the ER, CPAP was continued as clinically indicated and the hypothesis of ACPE was confirmed after routine diagnostics, including chest X-ray.
We also recorded the need for pre-hospital or in-hospital endotracheal intubation, type of admission (ICU or general ward), length of hospital stay, outcome at discharge.
Helmet CPAP administration
A detailed description of the helmet CPAP system is provided elsewhere [16, 19]. Basically, the helmet consists of an oxygen head tent (Sea Long Med. Sys Inc, Louisville, USA) with two side ports. The inlet port was connected to a high-flow oxygen source while the outlet port was connected to a mechanical spring PEEP valve (PEEP-FLOW, Bird, Dallas, USA). During the on-site application, transport to the ambulance and transfer from the ambulance to the ER, the inlet port was connected to a portable oxygen cylinder (3 L capacity filled at 200 atmospheres); the ambulance oxygen supply was used while on board. An oxygen flow of at least 30 L/min was used to prevent CO2 rebreathing [16]; the presence of a continuous flow from the PEEP valve throughout all the respiratory cycle was used as an indication of an adequate pneumatic circuit performance. ALSdoc could apply PEEP levels between 5 and 15 cm cmH2O according to oximetry and clinical response, while ALSnurs maximum PEEP level was 10 cmH2O. Elastic straps were positioned under the patient’s armpits and fixed to the helmet.
End-points
Primary endpoints of this study were the assessment of the feasibility of helmet CPAP in the out-hospital setting and its efficacy, defined as improvement in the recorded clinical variables. Secondary endpoint was to compare the efficacy of CPAP when administered as a sole treatment or in conjunction with standard medical therapy.
Statistical analysis
Values are expressed as mean ± SD. Changes observed following CPAP administration were compared using paired Student’s t test and Wilcoxon-signed rank test when appropriate. Differences among ALSdoc and ALSnurs groups were evaluated by unpaired Student’s t test and chi-square test when appropriate. P < 0.05 was considered as statistically significant.
Results
General results
We enrolled 62 consecutive patients rescued by ALSdoc and 59 consecutive patients rescued by ALSnurs. Patients’ characteristics and main outcome results are summarized in Table 2.
The diagnosis of ACPE was confirmed in hospital in 104 out of 121 patients (86%). Of the 17 non-confirmed ACPE diagnosis, eight patients were diagnosed with pneumonia, five with malignancies and four with ARDS. Twenty-two patients were admitted to an ICU, 91 were transferred to a general ward, while eight died during the first 24 h in the ER. The overall hospital stay was 10 ± 8.3 days and the hospital mortality was 16.6% (20 out of 121 patients).
No patients required a pre-hospital endotracheal intubation, while nine patients were intubated in hospital. Six of these patients had been diagnosed as non-ACPE in the ER. One patient per group was enclosed in the protocol although the recorded SBP was between 80 and 90 mmHg. Vasoactive drugs employed by ALSdoc group are summarized in Table 2. Fifty-six out of 62 patients underwent drugs therapy while in six patients a venous line was not available. No drugs were administered in ALSnurs.
Feasibility and efficacy of helmet CPAP
Helmet CPAP was applied and tolerated for all the pre-hospital phase in all the 121 patients. The application of CPAP did not lead to any adverse event directly related to positive pressure (gastric distension, aspiration of gastric content, pneumothorax), or to helmet use (skin lesions to the neck due to the rubber base, claustrophobia or discomfort).
The PEEP level applied was 10.6 ± 1.7 and 7.4 ± 2.3 cmH2O (P < 0.01) in ALSdoc and ALSnurs respectively.
Selected respiratory and circulatory function data are summarized in Table 3. In both groups, following CPAP administration pulse oximetry values normalized. Respiratory rate and, when available, WRS score decreased toward normality. Heart rate decreased significantly in both groups and systolic blood pressure (SBP) also decreased significantly during the CPAP application. Interestingly, this was also true in the ALSnurs group in which no pharmacological treatment was applied.
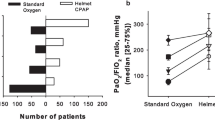
In Fig. 1 relative changes of SBP following helmet CPAP are plotted as a function of their initial values while breathing oxygen in the bag mask. Both groups showed a significant linear inverse relationship, indicating that the higher the initial SBP, the larger will be its reduction after therapy; however, for the lowest values of initial SBP there is no further tendency to a reduction in blood pressure but, on the contrary, a reverse trend toward improvement in blood pressure was observed.
The figure shows the relative variation of the SBP, induced by the application of non-invasive continuous positive airway pressure (CPAP) as a function of the initial value of SBP in patients rescued by advanced life support teams staffed by physicians (empty symbols, dashed line) and by nurses (filled symbols solid line). Notice how the reduction in SBP increases with increasing baseline values of SBP (linear regression P < 0.01 for both lines). Moreover, for the lowest value of baseline SBP (around 100 mmHg), the SBP does not decrease or, rather, increases, suggesting the safety of CPAP also in hypotensive patients
Comparison of helmet CPAP with and without pharmacologic treatment
The baseline data of ALSdoc and ALSnurs were comparable, except for basal respiratory rate, which was higher in the ALSnurs group; a similar proportion of ACPE diagnosis were confirmed (87% in the ALSdoc and 85% in the ALSnurs, P = ns). Nine patients (14.5%) in ALSdoc and 13 (22%) in ALSnurs were admitted to an ICU (P = ns). When only patients with a confirmed ACPE diagnosis are considered, the mortality amounted to 7.4% (4 out of 54) and 10% (5 out of 50) in the ALSdoc and ALSnurs groups respectively (P = ns).
No difference was recorded in the hospital stay averaging 9.2 ± 7.9 and 10.8 ± 8.8 days (P = ns) in the ALSdoc and ALSnurs group, respectively.
On the right hand side of Table 3, relative variations of the selected parameters are displayed: magnitude of variation was not different for all the variables, except for SBP that decreased more in the ALSdoc group (−14 ± 13 versus −7 ± 15%; P < 0.01).
Discussion
The main results of the present study are that helmet CPAP is feasible and can be safely and easily applied in the pre-hospital setting to patients with a presumed diagnosis of ACPE. Its application is associated to a prompt and sustained improvement of the respiratory and circulatory function, even in the absence of any specific pharmacological intervention (ALSnurs group).
Limitations of the study
Because patients were not randomized to treatment with or without helmet CPAP, one might speculate that the improvement in clinical parameters was due to medical therapy. If this was the case, however, the improvement should have been larger in the ALSdoc than in the ALSnurs group. This was not the case except for a more pronounced reduction in SBP in ALSdoc while all the other vital parameters monitored improved similarly in both groups. There was also no randomization between ALSdoc and ALSnurs teams, since not feasible, as the teams cover different geographic areas: this should, however, minimize the selection bias, since it was impossible to decide, based on patients condition, which team to send. Moreover, neither patients nor rescue teams were blinded to the treatment being administered.
Out of hospital use of CPAP
The efficacy of CPAP in ACPE is well established [2–10]. Despite this background, reports of CPAP application in pre-hospital setting are, to our knowledge quite limited. Kosowsky et al. [20], reported the ambulance use of a high-flow Venturi mask CPAP system and Templier et al. [21], that reported about 50 patients treated by Boussignac CPAP on their way to the hospital. In both studies CPAP was an adjunct to the standard drug protocol; both studies suggested a wider use of CPAP. More recently Plaisance et al. [12] reported the use of out-of-hospital CPAP in patients with ACPE: this study shares some similarities with ours (e.g., sample size, type of patients and study period); even if we did not randomize patients we offer, as well, a comparison between CPAP alone and CPAP plus medical treatment. We used a different interface, able to provide a higher inspired oxygen fraction (FiO2) and, likely, a better patient’s tolerance.
The helmet CPAP
The device we use to deliver CPAP is a head helmet rather than a face mask: local experience justifies this choice, since at our institution we have been using helmet CPAP for more than 20 years in the ICUs, in the ER and in general wards; this might explain such a high rate of successful CPAP application, since most physicians and, particularly, nurses, had gained a good familiarity with helmet in the hospital.
In the specific pre-hospital emergency care, a light, handy system is a must. Helmet CPAP [19] may appear cumbersome when compared with a traditional face mask circuitry [20] or to the Boussignac system [21]. Compared to a face mask; however, the helmet does not require a critical fitting and is easily applied even by a minimally trained crew, causes only minimal discomfort to most patients [14]; it requires however a high enough gas flow to minimize pressure shifts along the respiratory cycle. With a 30 L/min flow CO2 rebreathing is minimal [16, 22] and, since the helmet acts as a compliance chamber, the airway pressure is kept above PEEP throughout the respiratory cycle, provided that, as assessed by ALS crews, the gas flow through the expiratory valve is always present [16]. The spring-loaded valve used could have allowed some pressure swings in the helmet, however it does not increase the work of breathing [23], nor it affects the respiratory pattern, in comparison with an underwater seal valve (which could not have been used in the out-hospital setting anyway). Since it was the only one available at our institution when the study was conducted, we used a specific model of helmet (Sealong) whose use is less frequently reported in the literature than other models. Different (possibly better) results might have occurred using more recent helmet models, subsequently developed and commercialized by other brands.
Kosowsky et al. applied mask CPAP by use of a powerful Venturi system at the expense of an FiO2 reduction; the system however was not portable and could be applied during ambulance transportation only. The Boussignac system tested by Templier et al. [24, 25] is indeed easily transportable but, again, a reduction in FiO2 can be anticipated. Finally, one should always take into account the rather high rate of patient’s intolerance to the face mask (>10% in Kosowsky’s study).
Also the Plaisance study employed a face mask with a powerful Venturi system, with a relatively low FiO2. No intolerance to face mask was reported [12].
Part of the benefits observed with CPAP in this study may be ascribed to the increase in FiO2 warranted by the helmet application. The device was indeed introduced to maximize FiO2 during hyperbaric treatment and it is entirely conceivable that FiO2 rose going from the bag mask to the helmet. Given its high compliance the head helmet guarantees a stable airway pressure also with a relatively low (30 L/min) fresh gas flow rate. This is not the case for the face mask, requiring a compromise between an elevated FiO2 and a good pneumatic performance. The demand for a very high fresh gas flow rate (Plaisance et al. report 140 L/min), prevents the use of pure oxygen and mandates the use of a Venturi system with a consequent drop in FiO2. Although acceptable in the majority of the patients, this “trade-off” might become more problematic with the mostly hypoxic ones and we wonder if, with the use of higher FiO2, some of the out-of-hospital intubations occurring in the Pleisance study might have been avoided.
Efficacy of helmet CPAP
At variance with previous reports [21, 26], no patient required intubation or mechanical ventilation during transport.
In-hospital intubation rate was nine out of 121 (7.4%) homogeneously distributed between ALSdoc and ALSnurs groups. Among the intubated patients, six out of nine were diagnosed as non-ACPE at ER discharge. This result compares favorably with the study by Kosowsky et al. reporting an in-hospital intubation rate of 7 out of 19 (37%). Intubation rate and overall mortality of the present study is in line with the recent reports on the in-hospital [4, 7–10, 27] and out-hospital [12] application of CPAP and pressure support ventilation in ACPE. Oxygen saturation improved, respiratory rate, heart rate, and blood pressure decreased in both groups. Figure 1 shows that the reduction in blood pressure is proportional to the initial value. Moreover, it can be observed that when SBP is near normal the application of CPAP does not lead to any significant hypotension. It could be speculated that CPAP, by improving oxygenation and decreasing the work of breathing, may indeed decrease the sympathetic tone. With this mechanism, CPAP may contribute to break the vicious circle that leads to pulmonary edema. Moreover, CPAP may actually improve cardiac function by decreasing left ventricular afterload through an increased intrathoracic pressure. This is, in turn, due to a direct increase in airway pressure and an indirect effect due to reduced negative pressure swings as a consequence of improved respiratory mechanics. Even in the subset of patients later diagnosed as non-ACPE, helmet CPAP improved arterial oxygenation and did not influence negatively the hemodynamic status, confirming the safety of the procedure, although basic physiological knowledge suggests that the technique should be applied with caution in hypovolemic patients.
Helmet CPAP with and without drug therapy (ALSdoc vs. ALSnurs)
The comparison between the ALSdoc group and the ALSnurs group allows us to separate the effects of ventilatory support from those of pharmacological therapy. Somehow unexpectedly, CPAP with or without pharmacological therapy had strikingly similar effects on the clinical variables recorded until patients arrival in the ER, where all patients were treated with drugs. The two patient population appeared to be comparable except for a higher respiratory rate in the ALSnurs group. Despite a lower PEEP applied in ALSnurs (due to study design) both group responded similarly to helmet CPAP administration. In six patients of the ALSdoc group, a venous line was not available; nonetheless in this small group of patients helmet CPAP was extremely effective so that the absence of pharmacological treatment was not regretted. This observation actually prompted the application of CPAP by ALSnurs crews, not allowed to use drugs. Not surprisingly, given the possibility of applying an aggressive pharmacological therapy, the reduction in blood pressure was more pronounced in the ALSdoc than in the ALSnurs group (−14 versus –7%, see Table 3). However, no relevant differences were seen in the improvement of the remaining clinical parameters and in the clinical outcomes. Although the relative short period of evaluation (on average around 30 min) might not have allowed the medical therapy to be fully effective, taken together these findings strongly suggest that the bulk of the observed effect are related to CPAP rather than to the pharmacological treatment. This is in keeping with the findings by Plaisance et al. [12], demonstrating a more pronounced reduction in blood pressure with medical therapy as opposed to CPAP alone; however, the comparison between the groups with an “early” and a “late” application of CPAP clearly shows that medical therapy alone (a condition which was not tested in our study) or as an adjunct to CPAP has a modest efficacy, if any, in improving respiratory conditions. If confirmed, this interpretation could actually suggest that an ALS crew staffed by nurses might manage out-of-hospital ACPE patients as effectively as a physician staffed crew until the necessary pharmacologic treatment is initiated.
Conclusion
Helmet CPAP was feasible, safe and effective in the pre-hospital treatment of presumed ACPE: it allowed prompt improvement in vital parameters both in association with pharmacological support and as a sole treatment. Out of hospital emergency intubation was avoided and in hospital intubation rate was low. The indication for pharmacologic treatment in ACPE is out of discussion. However, these observations suggest that helmet CPAP (along with drugs and especially before these can be administered) could be used as first line intervention in the pre-hospital treatment of severe presumed ACPE.
References
Stiell IG, Spaite DW, Field B, Nesbitt LP, Munkley D, Maloney J, Dreyer J, Toohey LL, Campeau T, Dagnone E, Lyver M, Wells GA (2007) Advanced life support for out-of-hospital respiratory distress. N Engl J Med 356:2156–2164
Rasanen J, Heikkila J, Downs J, Nikki P, Vaisanen I, Viitanen A (1985) Continuous positive airway pressure by face mask in acute cardiogenic pulmonary edema. Am J Cardiol 55:296–300
Bersten AD, Holt AW, Vedig AE, Skowronski GA, Baggoley CJ (1991) Treatment of severe cardiogenic pulmonary edema with continuous positive airway pressure delivered by face mask. N Engl J Med 325:1825–1830
Crane SD, Elliott MW, Gilligan P, Richards K, Gray AJ (2004) Randomised controlled comparison of continuous positive airways pressure, bilevel non-invasive ventilation, and standard treatment in emergency department patients with acute cardiogenic pulmonary oedema. Emerg Med J 21:155–161
Lin M, Yang YF, Chiang HT, Chang MS, Chiang BN, Cheitlin MD (1995) Reappraisal of continuous positive airway pressure therapy in acute cardiogenic pulmonary edema. Short-term results and long-term follow-up. Chest 107:1379–1386
Masip J, Roque M, Sanchez B, Fernandez R, Subirana M, Exposito JA (2005) Noninvasive ventilation in acute cardiogenic pulmonary edema: systematic review and meta-analysis. JAMA 294:3124–3130
Nava S, Carbone G, DiBattista N, Bellone A, Baiardi P, Cosentini R, Marenco M, Giostra F, Borasi G, Groff P (2003) Noninvasive ventilation in cardiogenic pulmonary edema: a multicenter randomized trial. Am J Respir Crit Care Med 168:1432–1437
Pang D, Keenan SP, Cook DJ, Sibbald WJ (1998) The effect of positive pressure airway support on mortality and the need for intubation in cardiogenic pulmonary edema: a systematic review. Chest 114:1185–1192
Park M, Sangean MC, Volpe Mde S, Feltrim MI, Nozawa E, Leite PF, Passos Amato MB, Lorenzi-Filho G (2004) Randomized, prospective trial of oxygen, continuous positive airway pressure, and bilevel positive airway pressure by face mask in acute cardiogenic pulmonary edema. Crit Care Med 32:2407–2415
Peter JV, Moran JL, Phillips-Hughes J, Graham P, Bersten AD (2006) Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary oedema: a meta-analysis. Lancet 367:1155–1163
Gray A, Goodacre S, Newby DE, Masson M, Sampson F, Nicholl J (2008) Noninvasive ventilation in acute cardiogenic pulmonary edema. N Engl J Med 359:142–151
Plaisance P, Pirracchio R, Berton C, Vicaut E, Payen D (2007) A randomized study of out-of-hospital continuous positive airway pressure for acute cardiogenic pulmonary oedema: physiological and clinical effects. Eur Heart J 28:2895–2901
Mehta S, Hill NS (2001) Noninvasive ventilation. Am J Respir Crit Care Med 163:540–577
Principi T, Pantanetti S, Catani F, Elisei D, Gabbanelli V, Pelaia P, Leoni P (2004) Noninvasive continuous positive airway pressure delivered by helmet in hematological malignancy patients with hypoxemic acute respiratory failure. Intensive Care Med 30:147–150 Epub 2003 Oct 2031
Tonnelier JM, Prat G, Nowak E, Goetghebeur D, Renault A, Boles JM, L’Her E (2003) Noninvasive continuous positive airway pressure ventilation using a new helmet interface: a case-control prospective pilot study. Intensive Care Med 29:2077–2080
Patroniti N, Foti G, Manfio A, Coppo A, Bellani G, Pesenti A (2003) Head helmet versus face mask for non-invasive continuous positive airway pressure: a physiological study. Intensive Care Med 29:1680–1687
Delclaux C, L’Her E, Alberti C, Mancebo J, Abroug F, Conti G, Guerin C, Schortgen F, Lefort Y, Antonelli M, Lepage E, Lemaire F, Brochard L (2000) Treatment of acute hypoxemic nonhypercapnic respiratory insufficiency with continuous positive airway pressure delivered by a face mask: a randomized controlled trial. JAMA 284:2352–2360
Squadrone V, Coha M, Cerutti E, Schellino MM, Biolino P, Occella P, Belloni G, Vilianis G, Fiore G, Cavallo F, Ranieri VM (2005) Continuous positive airway pressure for treatment of postoperative hypoxemia: a randomized controlled trial. JAMA 293:589–595
Bellani G, Patroniti N, Greco M, Foti G, Pesenti A (2008) The use of helmets to deliver non-invasive continuous positive airway pressure in hypoxemic acute respiratory failure. Minerva Anestesiol 74:651–656
Kosowsky JM, Stephanides SL, Branson RD, Sayre MR (2001) Prehospital use of continuous positive airway pressure (CPAP) for presumed pulmonary edema: a preliminary case series. Prehosp Emerg Care 5:190–196
Templier F, Dolveck F, Baer M, Chauvin M, Fletcher D (2003) ‘Boussignac’ continuous positive airway pressure system: practical use in a prehospital medical care unit. Eur J Emerg Med 10:87–93
Taccone P, Hess D, Caironi P, Bigatello LM (2004) Continuous positive airway pressure delivered with a “helmet”: effects on carbon dioxide rebreathing. Crit Care Med 32:2090–2096
Pelosi P, Chiumello D, Calvi E, Taccone P, Bottino N, Panigada M, Cadringher P, Gattinoni L (2001) Effects of different continuous positive airway pressure devices and periodic hyperinflations on respiratory function. Crit Care Med 29:1683–1689
Villa F, Cereda M, Colombo E, Foti G, Pesenti A (1999) Evaluation of four noninvasive CPAP systems. Intensive Care Med S6:A246
Templier F, Dolveck F, Baer M, Chauvin M, Fletcher D (2003) Laboratory testing measurement of FIO2 delivered by Boussignac CPAP system with an input of 100% oxygen. Ann Fr Anesth Reanim 22:103–107
Kallio T, Kuisma M, Alaspaa A, Rosenberg PH (2003) The use of prehospital continuous positive airway pressure treatment in presumed acute severe pulmonary edema. Prehosp Emerg Care 7:209–213
Domenighetti G, Gayer R, Gentilini R (2002) Noninvasive pressure support ventilation in non-COPD patients with acute cardiogenic pulmonary edema and severe community-acquired pneumonia: acute effects and outcome. Intensive Care Med 28:1226–1232
Acknowledgments
All authors received a salary from their respective institutions. No additional funding was received for the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Foti, G., Sangalli, F., Berra, L. et al. Is helmet CPAP first line pre-hospital treatment of presumed severe acute pulmonary edema?. Intensive Care Med 35, 656–662 (2009). https://doi.org/10.1007/s00134-008-1354-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1354-7