Abstract
Objective
To evaluate the relationship between global oxygen delivery (DO2I), microvascular flow and tissue oxygenation in patients who did and did not develop complications following major abdominal surgery.
Design
Prospective observational study.
Setting
Post-operative critical care unit.
Participants
Twenty-five patients receiving standard peri-operative care following major abdominal surgery.
Measurements and main results
Data were collected before, and for 8 h after surgery. DO2I was measured by lithium dilution and arterial waveform analysis. Cutaneous PtO2 was measured at two sites on the abdominal wall using a Clark electrode. The sublingual microcirculation was visualised using sidestream darkfield imaging. Cutaneous red cell flux was measured using laser Doppler flowmetry. Fourteen patients (56%) developed complications with two deaths. Small vessel (<20 μm) microvascular flow index in those patients who developed complications was lower before (P < 0.05) and after surgery (P < 0.0001) compared to patients who did not develop complications. Both the proportion and density of perfused small vessels were also lower in patients who developed complications after surgery (P < 0.01) but not before surgery. DO2I was low in all patients but did not differ between patients who did and did not develop complications. Similarly, there were no associated differences in cutaneous red cell flux or PtO2.
Conclusion
In a group of patients with low DO2I following major abdominal surgery, microvascular flow abnormalities were more frequent in patients who developed complications. However, there were no differences in DO2I, cutaneous PtO2 or red cell flux between the two groups. Impaired microvascular flow may be associated with the development of post-operative complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
It is estimated that 234 million major surgical procedures are performed worldwide each year [1]. Complications following major surgery are a leading cause of morbidity and mortality [2, 3]. High-risk surgical patients account for over 80% of deaths but only 12.5% of in-patient surgical procedures [4, 5]. In the UK, around 170,000 patients undergo high-risk surgical procedures each year, of whom 25,000 patients die and as many as 100,000 develop complications. Data from mainland Europe and North America suggest that this problem is not unique to the UK [6, 7]. Even for those patients who survive to leave hospital, post-operative complications remain an important determinant of long-term survival [6]. It is essential, therefore, that we improve outcomes following major surgery.
The aetiology of post-operative complications is complex. Risk factors include advanced age, co-morbid disease and major and urgent surgery [4, 5]. A number of reports describe an association between derangements in global oxygen delivery (DO2I) or related parameters and poor outcome following major surgery [8–10]. In several small studies, the use of fluid and inotropic therapy to enhance global oxygen delivery has led to a reduction in post-operative complications [11–14]. It has been suggested that the benefits of this approach are a result of improved tissue perfusion and oxygenation. Whilst unconfirmed, this hypothesis is consistent with the findings of a number of previous investigations. Surgical wound infections are associated with reductions in tissue PO2 [15], and may be prevented by the early use of supplemental inspired oxygen [16, 17]. The use of warming blankets to prevent peri-operative hypothermia may also reduce the incidence of wound infection, suggesting a pathophysiological process related to tissue perfusion [18, 19]. The findings of several studies suggest that reductions in microvascular blood flow during gastro-intestinal surgery may be associated with impaired anastomotic healing [20–22]. However, a more detailed knowledge of the relationship between changes in global determinants of oxygen delivery and regional measures of tissue perfusion and oxygenation is required. The objective of this study was to describe the relationship between global oxygen delivery, tissue microvascular flow and oxygenation in high-risk patients who did and did not develop complications following major abdominal surgery.
Patients and methods
The study was approved by the Local Research Ethics Committee. Written informed consent was obtained prior to surgery. Patients admitted to a critical care unit following major elective abdominal surgery were eligible for recruitment. Exclusion criteria were refusal of consent, concurrent lithium therapy, acute myocardial ischaemia, acute arrhythmias, pregnancy, patients receiving palliative treatment only and weight less than 40 kg. Patients were enrolled when a member of the research team was available. General anaesthesia was standardised to include intravenous fentanyl, propofol and atracurium for induction of anaesthesia and maintenance with inhaled isoflurane in oxygen-enriched air alongside epidural analgesia. Clinical staff administered intravenous fluids, blood products and, if required, vasoactive drugs in order to maintain pulse rate, arterial pressure, central venous pressure, urine output, haematological and biochemical parameters within the normal range. Appropriate measures were taken to maintain SpO2 ≥ 94%, haemoglobin above 8 g dl−1 and temperature at 37°C. Following surgery, all patients were managed in a critical care unit. Additional fluid challenges and inotropic therapy were prescribed by clinical staff. Cardiac output data were made available when specifically requested by clinical staff. Patients did not, however, receive specific flow guided haemodynamic therapy in order to attain pre-determined values for stroke volume, cardiac index or global oxygen delivery.
Measurements
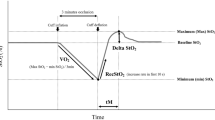
In addition to heart rate, mean arterial pressure and central venous pressure, cardiac output and DO2I were measured by lithium indicator dilution and arterial waveform analysis (LiDCOplus, LiDCO Ltd, Cambridge, UK) [23]. Arterial and central venous blood samples were taken for analysis of blood gases, lactate and haemoglobin concentration (ABL 600 and OSM3, Radiometer, Copenhagen, Denmark). Cutaneous tissue PtO2 was measured at two sites on the abdominal wall using a Clark electrode (TCM400, Radiometer, Copenhagen, Denmark). These probes are designed to warm the skin to 44°C in order to minimise artefact due to local vasoconstriction. Cutaneous red blood cell flux was measured at two sites on the abdominal wall by laser Doppler flowmetry (Moorlab, Moor Instruments, Axminster, UK). Sublingual microvascular flow was evaluated using sidestream darkfield imaging with a 5× objective lens (Microscan, Microvision Medical, Amsterdam, Netherlands) [24]. Microvascular and tissue oxygenation data were obtained on the ward prior to surgery and all data were collected at 2-h intervals after surgery for 8 h. Hour 0 refers to the time of admission to the critical care unit. Image acquisition and subsequent analysis was performed according to published consensus criteria [25]. In brief, SDF images were obtained from at least three sublingual areas at each time point. Microvascular flow index (MFI) was calculated after dividing each image into four equal quadrants. Quantification of flow was determined using an ordinal scale (0: no flow, 1: intermittent flow, 2: sluggish flow, 3: normal flow) for small (<20 μm) and large (>20 μm) vessels. MFI is the average score of all quadrants for a given category of vessel size at a given time point. Images were recorded at three sites at each time point giving 12 quadrants for analysis. Vessel density is calculated by inserting a grid of three equidistant horizontal and three equidistant vertical lines over the image. Vessel density is equal to the number of vessels crossing these lines divided by their total length. Flow is then categorised as present, intermittent or absent to calculate the proportion of perfused vessels and thus the perfused vessel density. Analysis of the videos was performed by two observers (SJ and CL). Patients were followed up for 28-day in-hospital post-operative complications (supplementary file), mortality and duration of hospital stay. The major categories of complications were infectious, respiratory, cardiovascular, renal, neurological and gastrointestinal.
Statistical analysis
For evaluating changes over time between groups, two-way repeated measures analysis of variance (ANOVA) was used. Post hoc t tests were performed at the different time points using the Bonferroni correction for multiple testing. Analysis was performed using GraphPad Prism version 4.0 (GraphPad Software, San Diego, USA). Significance was set at P < 0.05. Data are presented as mean (SD) where normally distributed or median (IQR) where not normally distributed. Inter-observer variability for analysis of the SDF images was assessed by calculating the Kappa coefficient (κ) [26].We did not perform a sample size calculation based on any single variable and instead elected prospectively to recruit 25 patients.
Results
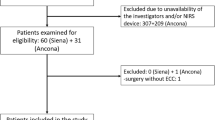
Twenty-five patients were recruited with a median age of 69 (63–72) years. Demographical patient characteristics, peri-operative haemodynamic management and outcome data are summarised in Tables 1 and 2. Two patients were mechanically ventilated after surgery. All other patients were extubated prior to critical care admission. Two patients died (8%) and 14 patients (56%) developed post-operative complications. The median time to first complication was 3 (2–6) days. Ten patients (40%) developed infectious complications (Table 3). Critical care (P < 0.01) and hospital stay (P < 0.001) were significantly longer in those patients who developed complications. There were no differences in PtO2, DO2I, ScvO2, cardiac index, heart rate, mean arterial pressure, serum lactate or cutaneous red cell flux between patients who did and did not develop complications. There was a significant difference in base deficit (Fig. 1; Tables 4, 5). The inspired fractional concentration of oxygen after surgery at all time points was 0.4 (0.4–0.4).
There was a significant difference in sublingual MFI in small vessels (<20 μm) after surgery between those patients who subsequently developed complications and those who did not (Fig. 2). The MFI of the large vessels (>20 μm) remained normal in all patients throughout the study period. Neither the total vessel density nor the small vessel (<20 μm) density was significantly different between these groups. The proportion of perfused small vessels (<20 μm) was significantly lower after surgery in those patients who developed complications. Perfused vessel density, a measure of functional capillary density, was also lower after surgery in patients who developed complications (Table 5). The density and proportion of perfused large vessels (>20 μm) were not significantly different between groups. We were only able to collect sublingual microvascular images prior to surgery in 14 patients. Despite this, MFI for small vessels (<20 μm) was reduced in those patients who subsequently developed complications compared to those who did not (2.6 [2.5–2.9] vs. 3.0 [3.0–3.0]; P < 0.05). Large vessel MFI (>20 μm) was 3.0 (3.0–3.0) in both groups. The kappa coefficient for inter-observer reliability was 0.81 (95%CI 0.72–0.89). In one patient, it was not possible to obtain any SDF images due to painful oral mucositis related to chemotherapy.
Sublingual microvascular flow index (MFI) of small vessels (<20 μm) in patients who did and did not develop complications. Shaded boxes complications, open boxes no complications. Data presented as median (IQR). P < 0.0001 between groups over time (two-way repeated measures ANOVA). * P < 0.01 between groups at this timepoint (post hoc t test with Bonferroni correction)
Discussion
The principle finding of this study is that, in a group of patients with low global oxygen delivery following major abdominal surgery, impairment of microvascular flow was more marked in those patients who developed complications. Importantly, this difference in microvascular flow was present even before surgery. Although the incidence of complications was high, there were no associated differences in global oxygen delivery, cutaneous red cell flux or tissue oxygenation between patients who did and did not develop complications. These data suggest that impairment of microvascular flow may play an important role in the evolution of complications after abdominal surgery. Further research is required to confirm these findings and to investigate this area in more detail.
A number of investigators have described abnormalities in gastro-intestinal total red blood cell flux (laser Doppler flowmetry) in patients who develop post-operative complications [20–22]. This reduction in mucosal blood flow has been associated with an increased incidence of anastomotic breakdown following both oesophagectomy [21] and colorectal surgery [22]. Although oesophageal anastomotic flow improved following the topical application of nitroglycerin [27], this effect was not observed with intravenous infusions of either prostaglandin E1 or nitroglycerin [21, 28].We are not, however, aware of any previous reports of cutaneous red cell flux following gastro-intestinal surgery. In a recent investigation, Boerma et al. [29] did not identify any heterogeneity of microvascular flow in colonic stoma within 24 h of elective colo-rectal surgery. Sublingual microvascular flow was not reported, although it seems likely that the findings would have been similar. There are several reasons why these previous findings in non-septic patients contrast with those of the current study. We identified abnormalities of microvascular flow that were most evident in the early post-operative phase and appeared to be returning to normal by 8 h. In the previous study, stomal microvascular flow was evaluated only once in the first 24 h after surgery and possibly at variable time points. Early changes in microvascular flow may have therefore been missed. Perhaps more importantly, we specifically recruited a high-risk group of patients undergoing complex surgery who were deemed to require post-operative critical care admission whilst patients in the previous study were all admitted to a standard surgical ward. The finding of impaired sublingual microvascular flow prior to surgery in those patients who subsequently developed complications was unexpected. This observation may have related to mild hypovolaemia or to the underlying diagnosis (cancer in almost all cases) but does not appear to have resulted from diabetes or other co-morbid disease. Importantly, microvascular indices continued to deteriorate during and after surgery and appeared to be returning to normal by 8 h after surgery. Further work in a larger group of patients is required to confirm these findings and to explore the underlying explanation in more detail.
Decreased PtO2 has previously been associated with an increased incidence of post-operative wound infection [15]. Furthermore, peri-operative supplemental inspired oxygen [16, 17] and therapies to increase global oxygen delivery [11, 12] seem to decrease the incidence of wound infections. Supplemental oxygen may also improve colonic anastomotic PtO2 in pigs [30]. It is not clear why we did not identify any differences, in either cutaneous tissue oxygenation or DO2I between patients who did and did not develop complications. In the current study, cutaneous PtO2 was considerably greater than previously reported (10 ± 3 kPa vs. 6.5 ± 1.5 kPa) [15], perhaps reflecting the routine use of supplemental oxygen in the current investigation whereas in the previous study patients only received supplemental oxygen if SpO2 decreased to less than 90%. In addition, in the current study, every patient received epidural analgesia, which may also improve abdominal wall cutaneous oxygenation [31, 32]. These differences may also relate to the use of a cutaneous Clark electrode, which warms the skin in order to minimise artefact due to local vasoconstriction as opposed to a subcutaneous catheter. However, PtO2 values in the current study were similar to those previously measured using a subcutaneous catheter in patients receiving 40% oxygen after abdominal surgery [33].
Sublingual sidestream darkfield imaging is a valuable technique, which allows real time imaging of the intact microcirculation in the clinical environment. Whilst not as versatile as laser Doppler flowmetry, the capacity to explore heterogeneity of flow in vessels of different sizes has allowed important advances of our understanding of the microcirculation in critical illness [24, 34]. However, this technique remains semi-quantitative and data reliability may be affected by technical expertise and inter-observer bias. It is uncertain to what extent sublingual microvascular flow correlates with that in other vascular beds [29, 35]. We used the two-way repeated measures ANOVA test to evaluate changes over the entire course of the study rather than at individual time points. Whilst significant differences were identified in three measures of microvascular flow (MFI, proportion of perfused vessels and perfused vessel density), more stringent post-hoc testing identified a difference at only one time point. It seems likely that this relates to the small sample size. A larger study is therefore required to confirm these important preliminary findings and to evaluate this area in more detail.
In summary, we have identified an impairment of sublingual microvascular flow in patients who developed complications both prior to and following major abdominal surgery. However, there were no related differences in cutaneous red cell flux, PtO2 or global oxygen delivery. The findings of previous studies suggest that vasoactive agents may improve sublingual microvascular flow in septic patients [35–37]. Further investigations are indicated to confirm our findings and to evaluate the effects of haemodynamic interventions and vasoactive agents on tissue microvascular flow and oxygenation following major surgery.
References
Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR, Gawande AA (2008) An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet 372:139–144
Campling EA, Devlin HB, Lunn JN (1990) Report of the National Confidential Enquiry into Peri-Operative Deaths. In: Book report of the national confidential enquiry into peri-operative deaths. NCEPOD
Cullinane M, Gray AJ, Hargraves CM, Lansdown M, Martin IC, Schubert M (2003) The 2003 report of the national confidential enquiry into peri-operative deaths. In: Book The 2003 Report of the National Confidential Enquiry into Peri-Operative Deaths. NCEPOD
Pearse RM, Harrison DA, James P, Watson D, Hinds C, Rhodes A, Grounds RM, Bennett ED (2006) Identification and characterisation of the high-risk surgical population in the United Kingdom. Crit Care 10:R81
Jhanji S, Thomas B, Ely A, Watson D, Hinds CJ, Pearse RM (2008) Mortality and utilisation of critical care resources amongst high-risk surgical patients in a large NHS trust. Anaesthesia 63:695–700
Khuri SF, Henderson WG, DePalma RG, Mosca C, Healey NA, Kumbhani DJ (2005) Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg 242:326–341 discussion 341–323
Juul AB, Wetterslev J, Gluud C, Kofoed-Enevoldsen A, Jensen G, Callesen T, Norgaard P, Fruergaard K, Bestle M, Vedelsdal R, Miran A, Jacobsen J, Roed J, Mortensen MB, Jorgensen L, Jorgensen J, Rovsing ML, Petersen PL, Pott F, Haas M, Albret R, Nielsen LL, Johansson G, Stjernholm P, Molgaard Y, Foss NB, Elkjaer J, Dehlie B, Boysen K, Zaric D, Munksgaard A, Madsen JB, Oberg B, Khanykin B, Blemmer T, Yndgaard S, Perko G, Wang LP, Winkel P, Hilden J, Jensen P, Salas N (2006) Effect of perioperative beta blockade in patients with diabetes undergoing major non-cardiac surgery: randomised placebo controlled, blinded multicentre trial. BMJ 332:1482
Clowes GH Jr, Del Guercio LR, Barwinsky J (1960) The cardiac output in response to surgical trauma. A comparison between patients who survived and those who died. Arch Surg 81:212–222
Shoemaker WC (1972) Cardiorespiratory patterns of surviving and nonsurviving postoperative patients. Surg Gynecol Obstet 134:810–814
Pearse R, Dawson D, Fawcett J, Rhodes A, Grounds RM, Bennett ED (2005) Changes in central venous saturation after major surgery, and association with outcome. Crit Care 9:R694–R699
Pearse R, Dawson D, Fawcett J, Rhodes A, Grounds RM, Bennett ED (2005) Early goal-directed therapy after major surgery reduces complications and duration of hospital stay. A randomised, controlled trial [ISRCTN38797445]. Crit Care 9:R687–R693
Boyd O, Grounds RM, Bennett ED (1993) A randomized clinical trial of the effect of deliberate perioperative increase of oxygen delivery on mortality in high-risk surgical patients. JAMA 270:2699–2707
Wilson J, Woods I, Fawcett J, Whall R, Dibb W, Morris C, McManus E (1999) Reducing the risk of major elective surgery: randomised controlled trial of preoperative optimisation of oxygen delivery. BMJ 318:1099–1103
Pearse RM, Belsey JD, Cole JN, Bennett ED (2008) Effect of dopexamine infusion on mortality following major surgery: individual patient data meta-regression analysis of published clinical trials. Crit Care Med 36:1323–1329
Hopf HW, Hunt TK, West JM, Blomquist P, Goodson WH 3rd, Jensen JA, Jonsson K, Paty PB, Rabkin JM, Upton RA, von Smitten K, Whitney JD (1997) Wound tissue oxygen tension predicts the risk of wound infection in surgical patients. Arch Surg 132:997–1004 discussion 1005
Greif R, Akca O, Horn EP, Kurz A, Sessler DI (2000) Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. Outcomes Research Group. N Engl J Med 342:161–167
Belda FJ, Aguilera L, Garcia de la Asuncion J, Alberti J, Vicente R, Ferrandiz L, Rodriguez R, Company R, Sessler DI, Aguilar G, Botello SG, Orti R (2005) Supplemental perioperative oxygen and the risk of surgical wound infection: a randomized controlled trial. JAMA 294:2035–2042
Kurz A, Sessler DI, Lenhardt R (1996) Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med 334:1209–1215
Melling AC, Ali B, Scott EM, Leaper DJ (2001) Effects of preoperative warming on the incidence of wound infection after clean surgery: a randomised controlled trial. Lancet 358:876–880
Pierie JP, De Graaf PW, Poen H, Van der Tweel I, Obertop H (1994) Impaired healing of cervical oesophagogastrostomies can be predicted by estimation of gastric serosal blood perfusion by laser Doppler flowmetry. Eur J Surg 160:599–603
Miyazaki T, Kuwano H, Kato H, Yoshikawa M, Ojima H, Tsukada K (2002) Predictive value of blood flow in the gastric tube in anastomotic insufficiency after thoracic esophagectomy. World J Surg 26:1319–1323
Vignali A, Gianotti L, Braga M, Radaelli G, Malvezzi L, Di Carlo V (2000) Altered microperfusion at the rectal stump is predictive for rectal anastomotic leak. Dis Colon Rectum 43:76–82
Jhanji S, Dawson J, Pearse RM (2008) Cardiac output monitoring: basic science and clinical application. Anaesthesia 63:172–181
Ince C (2005) The microcirculation is the motor of sepsis. Crit Care 9(Suppl 4):S13–S19
De Backer D, Hollenberg S, Boerma C, Goedhart P, Buchele G, Ospina-Tascon G, Dobbe I, Ince C (2007) How to evaluate the microcirculation: report of a round table conference. Crit Care 11:R101
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Meas 20:37–46
Buise MP, Ince C, Tilanus HW, Klein J, Gommers D, van Bommel J (2005) The effect of nitroglycerin on microvascular perfusion and oxygenation during gastric tube reconstruction. Anesth Analg 100:1107–1111
Buise M, van Bommel J, Jahn A, Tran K, Tilanus H, Gommers D (2006) Intravenous nitroglycerin does not preserve gastric microcirculation during gastric tube reconstruction: a randomized controlled trial. Crit Care 10:R131
Boerma EC, van der Voort PH, Spronk PE, Ince C (2007) Relationship between sublingual and intestinal microcirculatory perfusion in patients with abdominal sepsis. Crit Care Med 35:1055–1060
Kimberger O, Fleischmann E, Brandt S, Kugener A, Kabon B, Hiltebrand L, Krejci V, Kurz A (2007) Supplemental Oxygen, but Not Supplemental Crystalloid Fluid, Increases Tissue Oxygen Tension in Healthy and Anastomotic Colon in Pigs. Anesth Analg 105:773–779
Kabon B, Fleischmann E, Treschan T, Taguchi A, Kapral S, Kurz A (2003) Thoracic epidural anesthesia increases tissue oxygenation during major abdominal surgery. Anesth Analg 97:1812–1817
Treschan TA, Taguchi A, Ali SZ, Sharma N, Kabon B, Sessler DI, Kurz A (2003) The effects of epidural and general anesthesia on tissue oxygenation. Anesth Analg 96:1553–1557, table of contents
Chang N, Goodson WH 3rd, Gottrup F, Hunt TK (1983) Direct measurement of wound and tissue oxygen tension in postoperative patients. Ann Surg 197:470–478
Ince C (2006) Go with the flow—recruit the microcirculation!. Intensive Care Med 32:488–489
Creteur J, De Backer D, Sakr Y, Koch M, Vincent JL (2006) Sublingual capnometry tracks microcirculatory changes in septic patients. Intensive Care Med 32:516–523
De Backer D, Creteur J, Dubois MJ, Sakr Y, Koch M, Verdant C, Vincent JL (2006) The effects of dobutamine on microcirculatory alterations in patients with septic shock are independent of its systemic effects. Crit Care Med 34:403–408
Spronk PE, Ince C, Gardien MJ, Mathura KR, Oudemans-van Straaten HM, Zandstra DF (2002) Nitroglycerin in septic shock after intravascular volume resuscitation. Lancet 360:1395–1396
Acknowledgments
This study was supported by the European Society of Intensive Care Medicine/Spacelabs Intelligent Monitoring Award and the loan of equipment from LiDCO Ltd.
Conflict of interest statement
RP has received research grants from LiDCO Ltd and Circassia Holdings Ltd. The data presented in this manuscript have been used in support of a patent application on which SJ, CH and RP are named inventors.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jhanji, S., Lee, C., Watson, D. et al. Microvascular flow and tissue oxygenation after major abdominal surgery: association with post-operative complications. Intensive Care Med 35, 671–677 (2009). https://doi.org/10.1007/s00134-008-1325-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1325-z