Abstract
Objective
To evaluate whether arterial pressure response during a Valsalva maneuver could predict fluid responsiveness in spontaneously breathing patients.
Design and setting
Prospective clinical study in a 17-bed multidisciplinary intensive care unit.
Patients
Thirty patients without mechanical ventilation and equipped with a radial arterial catheter for whom the decision to give fluids was taken due to suspected hypovolemia.
Intervention
A 10-s Valsalva maneuver was performed before and after volume expansion (VE). Patients were classified as responders if stroke volume index (SVi) increased ≥15% after VE.
Measurements and results
Pulse pressure changes during the Valsalva maneuver (∆VPP) were calculated as the difference between maximal pulse pressure during phase 1 and minimal pulse pressure during phase 2 of the Valsalva maneuver divided by the mean of the two values and expressed as a percentage. Valsalva changes in systolic pressure (∆VSP) were calculated in similar way. SVi changes induced by VE was correlated with baseline values of ∆VPP and ∆VSP (r 2 = 0.71 and r 2 = 0.60; P < 0.0001, respectively), and with VE-induced changes in ∆VPP and ∆VSP (r 2 = 0.56 and r 2 = 0.44; P < 0.0001 and P < 0.001, respectively). A ∆VPP value of 52% and ∆VSP of 30% predicted fluid responsiveness with a sensitivity of 91% and 73% and a specificity of 95 and 90%, respectively.
Conclusions
Arterial response during the Valsalva maneuver is a feasible tool for predicting fluid responsiveness in patients without mechanical ventilatory support.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The superiority of dynamic indices to predict fluid responsiveness compared to static measurements of cardiac preload is widely accepted [1]. Pulse pressure variation, stroke volume variation and surrogate indexes, caused by cyclic changes in left ventricular stroke volume during positive pressure ventilation, have been extensively studied and recognized to assist in decision-making to administrate fluids in hemodynamic unstable patients. However, these parameters have been shown to be reliable predictors of preload-dependence only on deeply sedated patients fully adapted to mechanical ventilation without any spontaneous respiratory effort [2]. Furthermore, predictive value of dynamic parameters in spontaneously breathing patients seems to be inferior to static values of cardiac filling pressures [3].
Passive leg raising maneuver, challenging the cardiovascular system to a reversible and transient fluid challenge [4], has been described as a feasible assessment of fluid responsiveness in a broader population, including patients with cardiac arrhythmias or spontaneous respiratory movements [5]. Nevertheless, this test requires a fast-response device, like esophageal Doppler [5] or transthoracic echocardiography [6], to detect brief hemodynamic changes during the sudden increase in preload due to passive leg raising [7].
The arterial pressure response to the Valsalva maneuver (VM), sustaining a forced expiratory effort against a closed glottis, has been used for decades by cardiologists in the clinical evaluation of patients with congestive heart failure [8, 9] and proposed as a useful and easily applicable tool to detect high ventricular filling pressures [10, 11]. Although cardiovascular changes during the VM are complex, involving both mechanical and neurohormonal factors [12], sudden increases in intrathoracic pressure (ITP) during strain seem to compress cardiac chambers [13], preventing venous emptying to the heart and reducing telediastolic volumes [14]. Since the VM abruptly impairs venous return raising ITP [15], according to the Frank-Starling relationship, patients with both ventricles operating in the ascending part of the cardiac function curve should decrease stroke volume and hence arterial pulse pressure, because of a reduced preload. Whereas patients in the flat portion of the cardiac function curve should not exhibit any significant decrease in stroke volume due to an acute fall in venous return during the strain period. Thus, in this regard, VM could be used as an easy and reversible test to evaluate the preload-dependence condition of a patient.
Therefore, we designed this study to assess the usefulness of arterial pressure changes during a VM to predict fluid responsiveness in spontaneously breathing patients.
Materials and methods
After approval by the institutional Ethics Committee of the hospital, 30 consecutive patients admitted to the multidisciplinary intensive care unit of the Hospital of Jerez were included from July to December 2007. Informed consent was obtained from all patients after inclusion. An additional description of materials and methods can be found in the Electronic Supplementary Material (ESM).
Patient selection
Inclusion criteria were patients with spontaneous breathing without any mechanical ventilation support, who were equipped with an invasive radial arterial catheter as part of standard clinical care and for whom the decision to give fluids was taken because the presence of hypotension, oliguria or tachycardia. Patients were excluded if they had arrhythmia, history of syncope, lack of cooperation to perform the VM or to achieve at least 20 cmH2O of airway pressure.
Cardiac output measurements
A FloTrac™ sensor (Edwards Lifesciences LLC, Irvine, CA, USA) was connected to the arterial line and attached to the Vigileo™ monitor, software version 1.07 (Edwards Lifescience LLC, Irvine, CA, USA). Cardiac output and stroke volume values were averaged as the mean of three consecutive measurements.
The Valsalva maneuver, arterial pressure responses and Valsalva parameters of fluid responsiveness
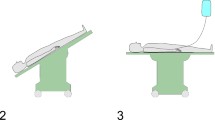
All patients received a brief training to make them familiar in the performance of the VM. The VM was performed in supine position and consisted of a forced expiration after a normal inspiration through a closed mouthpiece connected to a disposable spirometry transducer (Datex-Ohmeda, Helsinki, Finland). Patients were encouraged to maintain a nearly constant pressure level of 30 cmH2O for 10 s, with the assistance of a pressure marker displayed on the bedside monitor, and then to promptly release the strain and resume normal quiet breathing. A cut-off of 20 cmH2O of airway pressure was selected to ensure an effective decrease on venous return and cardiac preload, since this seems to be the minimum pressure level required to produce a significant decrease in arterial pulse pressure in normal subjects [14].
Arterial responses to the Valsalva maneuver
The normal blood pressure response to the VM, including appropriate responses in heart rate and arterial pressure waveform, provides reliable information about the integrity of the heart function and autonomic reflexes of the cardiovascular system [16]. Traditionally, this response shows four well-defined phases and a typical sinusoidal pattern (Fig. 1) [17]. On the other hand, abnormal arterial pressure response or “square-wave response” to the VM (Fig. 2) [18] has been typically described in patients with severe congestive cardiac failure [8, 9] and has also been related to high left ventricular filling pressures [10, 11] and elevated natriuretic peptides [12].
Valsalva parameters of fluid responsiveness
Since changes in venous return due to the VM were produced mainly during its initial stages (early phase 2), we defined Valsalva pulse pressure variation (∆VPP) as the percent variation between the highest pulse pressure during phase 1 (PPmaxphase1) and the lowest pulse pressure during phase 2 (PPminphase2): ∆VPP (%) = 100 × (PPmaxphase1 − PPminphase2)/[(PPmaxphase1 + PPminphase2)/2]. Similarly, Valsalva systolic pressure variation (∆VSP) was calculated.
Study protocol
Supportive therapies and vasopressors, if present, remained unchanged throughout the study. A first set of hemodynamic measurements was obtained at baseline and the VM was performed immediately after that. Central venous pressure (CVP), invasive arterial pressure and airway pressure were continuously recorded on a personal computer during the whole study time. Volume expansion (VE) consisted of 500 ml of synthetic colloid (Voluven®, hydroxyethylstarch 6%; Fresenius, Bad Homburg, Germany) infused over 30 min. New measurements were obtained after VE and a post-infusion VM was performed.
Statistical analysis
Results are expressed as mean ± SD unless otherwise stated. All data were normally distributed as tested by means of a Kolmogorov–Smirnov test. Patients were classified according to the stroke volume index (SVi) increase after VE in responders (SVi ≥ 15%) and nonresponders (SVi < 15%), according to previous studies references [19, 20].
Hemodynamic and respiratory variables were compared between responders and nonresponders using an independent samples t test, and before and after VE using a paired Student′s t test. The relationships between variables were analyzed using a linear regression method. The area under the receiver operating characteristic (ROC) curves for ∆VPP, ∆VSP, PPmaxphase1, PPminphase2, CVP and SVi according to fluid expansion response were calculated and compared using the Hanley–McNeil test. ROC curves are presented as area ± SE.
A P value <0.05 was considered statistically significant. Statistical analyses were performed using MedCalc for Windows, version 9.4.2.0 (MedCalc Software, Mariakerke, Belgium).
Results
Thirty patients (19 nonresponders and 11 responders) were prospectively included. The main characteristics are summarized in Table 1. One patient was unable to maintain the expiratory pressure above 20 cmH2O and was excluded from the study. Four patients received cathecolamines during the study period: dobutamine (5 μg Kg−1 min−1) associated to norepinephrine (n = 2), and norepinephrine alone (n = 2). Mean norepinephrine dose was 0.46 ± 0.34 μg Kg−1 min−1. All the patients survived at discharge of ICU.
Hemodynamic response to volume expansion
Hemodynamic parameters before and after VE are given in Table 2. SVi increased by 19.5 ± 4% (from 15.2 to 25.4%) in responders, and by 3 ± 9% (from −17.7 to 14.1%) in nonresponders. Cardiac index increased by 16.7 ± 10% (from −0.04 to 39.8) in responders, and by 4.8 ± 9% (from −17.7 to 19.4) in nonresponders. Fluid administration also increased CVP from 5 ± 3 mmHg to 9 ± 4 mmHg (P < 0.0001) in the whole studied population, but did not produce any substantial increase in mean arterial pressure. At baseline, neither CVP cardiac index nor SVi were significantly different between the two groups. Only total systemic vascular resistance was significantly higher in responder patients.
Effects of VE on arterial pressure response to a Valsalva maneuver
The effects of the VM on arterial pressure before and after VE are shown in Table 3. Individual values for ∆VPP, ∆VSP and PPminphase2 at baseline are represented in Fig. 3. Although VE significantly decreased ∆VPP, ∆VSP and increased PPminphase2 in both groups, the percentage reduction in ∆VPP and ∆VSP was greater in responders than in nonresponders (45 ± 13 vs. 21 ± 12%, P < 0.0001; 23 ± 7 vs. 12 ± 9%, P < 0.01, respectively), whereas PPminphase2 percentage increase induced by VE was greater in responders than in nonresponders (74 ± 30 vs. 32 ± 32%, P < 0.01). However, only ∆VPP and ∆VSP remained significantly higher in responders after fluid administration.
Distribution of individual values of ΔVPP and ΔVSP (left panel) and PPminphase2 (right panel) before volume expansion. R Responders (stroke volume index increase 15% after volume challenge); NR nonresponders (stroke volume index increase <15% after volume challenge). Points and arrows indicate mean and SD, respectively
A positive linear correlation was found between preinfusion values of ∆VPP and ∆VSP and VE-induced changes in SVi (r 2 = 0.71 and r 2 = 0.60; P < 0.0001, respectively), such that the higher the ∆VPP or ∆VSP, the greater the increase in SVi in response to fluid challenge (Fig. 4). However, a weaker but significant correlation between baseline PPminphase2 and changes in SVi after VE (r 2 = 0.42; P < 0.001) was observed. No relationship was found between PPmaxphase1 and preinfusion CVP with changes in SVi after VE.
Fluid-induced decreases in ∆VPP and ∆VSP were also correlated with changes in SVi after fluid challenge (r 2 = 0.56 and r 2 = 0.44; P < 0.0001 and P < 0.001, respectively). PPminphase2 increase after VE also correlated with SVi increase (r 2 = 0.54, P < 0.0001; Fig. 5).
A threshold ∆VPP value of 52% predicted fluid responsiveness with a sensitivity of 91% and a specificity of 95% (positive and negative predictive values were 91 and 95%, respectively), whereas predictive values for ∆VSP and PPminphase2 were lower: a sensitivity of 73% and a specificity of 90% for a cut-off value of 30% for ∆VSP, and a sensitivity of 91% and a specificity of 79% for a PPminphase2 value of 45 mmHg, respectively.
The predictive value of the various indices on fluid responsiveness was compared in Fig. 6. The area under the ROC curves for baseline ∆VPP (0.98 ± 0.03; 95% CI: 0.84–0.99) was significantly higher than CVP (0.51 ± 0.11; 95% CI: 0.32–0.70), PPmaxphase1 (0.55 ± 0.11; 95% CI: 0.36–0.73) and SVi (0.65 ± 0.1; 95% CI: 0.45–0.81) before VE (P < 0.001, respectively), but did not differ from ∆VSP (0.90 ± 0.07; 95% CI: 0.73–0.98) and PPminphase2 (0.89 ± 0.06; 95% CI: 0.72–0.97).
Comparison of receiver operating characteristics curves to discriminate responders and nonresponders to fluid expansion. ΔVPP Valsalva pulse pressure variation, ΔVSP Valsalva systolic pressure variation, PPmin phase2 lowest pulse pressure during phase 2 of the Valsalva maneuver, CVP central venous pressure, SVi stroke volume index
Airway pressure during the Valsalva maneuver
Average airway pressure throughout the Valsalva maneuver was not significantly different before and after volume challenge between both responders and nonresponders (Table 4). Average airway pressure was also strongly correlated with the CVP increase during strain before and after fluid administration (r 2 = 0.72 and r 2 = 0.73; P < 0.0001, respectively).
Discussion
The present study demonstrates that arterial pressure waveform variations induced by a VM reliably predict fluid responsiveness in spontaneously breathing patients. A ΔVPP value of 52% was predictive with a high sensitivity and specificity of an increase by more than 15% in SVi after volume administration in patients with spontaneous respiratory efforts.
In normal individuals, the VM triggers a typical sequence of complex hemodynamic events. Initially, as ITP rises due to the exaggerated expiratory effort, the pressure gradient for venous return diminishes reducing cardiac filling, telediastolic volumes [13, 21] and pooling blood volume from thoracic vessels within splanchnic circulation [15]. The increase in right atrial pressure, the downstream pressure for venous return, along with the external compression of both vena cavae [22], seem to be the main mechanisms for decreased venous emptying to the right heart. Although mean systemic pressure probably increases because of the active contraction of the abdominal muscles [23], the net effect should be a reduced driving pressure to the right ventricle, since right atrial pressure and venous resistance also increased. Moreover, as pulmonary volume remains unchanged during strain, we can assume that transpulmonary pressure, and hence right ventricular afterload, should be unaffected by the VM [24]. Thus, the rise in ITP and how it affects the venous return should explain solely the reduction in cardiac output observed during expiratory effort. On the other hand, increases in ITP improve left ventricular outflow impedance [25], whereas reduced right ventricular telediastolic volume due to impeded venous return increases left ventricular compliance [26]; so, in preload-dependent patients, in whom cardiac output is primary conditioned by venous return [23], the overall result of sustained increase in ITP during initial stages of VM should be a marked decrease in stroke volume and arterial pulse pressure.
By contrast, in non-preload-dependent patients, since venous return is not a limiting factor for cardiac output, the effect of increased ITP and reduced cardiac preload should be attenuated. Moreover, in severe heart failure condition, enhanced left ventricular function (through reduced left ventricular afterload) and increased left ventricular compliance (through ventricular interdependence) will support stroke volume during strain [27] and, despite impaired venous return, pulse pressure should remain unchanged producing the known square-wave response [18, 28].
Thereby, the spectrum of arterial pressure responses observed during a VM, from the normal sinusoidal pattern to the square-wave response, should be a function of the cardiac preload and the slope of the Frank-Starling curve, in which the blood pressure drop during early phase 2 depicts the relationship between them. Therefore, VM could be considered as a reversible and transient test to challenge the preload-dependence of a patient, inducing a sharp decrease in venous return and preload in the opposite way from the passive leg raising maneuver.
Differences observed in Valsalva parameters of fluid responsiveness in our patients should be explained under this physiological interpretation. In the present study we found that a ∆VPP threshold value of 52% offers the optimal sensitivity/specificity ratio to predict fluid responsiveness in spontaneously breathing patients. Interestingly, this value is very close to the 50% stroke volume reduction observed during a VM in normal preload-dependent subjects [29]. We also observed a strong relationship between baseline ∆VPP and SVi increase induced by volume expansion, so arterial changes during VM provided not only a characterization of patients according to their operating state on the cardiac function curve, but also a quantification of their response to a fluid challenge.
VE produced a significant change in arterial pressure response to the VM in our patients. This volume induced change in the arterial waveform pattern was due mainly to a rise in PPminphase2 (which determines a decrease in ∆VPP and ∆VSP, since PPmaxphase1 remained unchanged), probably as a result of an increase in central blood volume that prevents the fall in venous return and cardiac output during strain [15]. These results are in concordance with previous clinical [11, 18, 30] and experimental [31] studies, in which acute manipulations of plasma volume resulted in reciprocal changes in phase 2 pressure drop during the VM. Therefore, hypovolemic induced condition resulted in a more sinusoidal profile, whereas the hypervolemic state, displacing the cardiac operation point rightward to the flat part of the Frank-Starling curve, produced a more similar square pattern.
Even though this is not the first work that relates arterial pressure changes during the VM and the ventricular function curve [28, 32], this study is pioneer in taking advantage of this relationship to predict fluid responsiveness in a group of patients that represents an important percentage of the critically ill population. Although arterial responses to the Valsalva maneuver had been known for several decades [33], its utility as a clinical tool has been consistently dismissed [8].There is an extensive evidence in clinical literature which supports the VM as a feasible bedside assessment of patients with heart failure [8, 9], since the presence of the arterial square wave response strongly suggests that patients operate in the flat portion of the cardiac function curve. Moreover, a consistent correlation between blood pressure changes during VE and left-sided filling pressure has been demonstrated, putting this forward as a reliable estimation of left ventricular invasive pressures in patients with congestive heart failure [10, 11]. In spite of this evidence, its application in clinical practice remains overlooked. Our small contribution to the knowledge of the mechanisms involved in the hemodynamic consequences of the VM and its potential usefulness to predict fluid responsiveness may encourage interest in this physiological maneuver.
Some limitations of this study must be considered. First, arterial response to the VM has been demonstrated to be posture dependent, mainly due to the effects of orthostatic stress on intrathoracic blood volume [34]. To avoid any confounding factor, all the VMs were performed with patients in supine position, so results may vary in postures other than supine. Second, cardiac arrhythmias can give misleading measurements of arterial blood pressure changes during VM, and patients with arrhythmias were excluded from the present study. Therefore, the predictive value of arterial changes during the Valsalva maneuver may be not reliable in the presence of cardiac arrhythmias. Third, most of the studied population was postsurgical patients with suspected hypovolemia but not established shock, so our results should not be extrapolated to other clinical conditions without caution. Fourth, cardiac output was not measured by the reference thermodilution method. Instead we used the FloTrac/Vigileo™ system, a recently introduced device based on an uncalibrated arterial pulse contour analysis, to track hemodynamic changes after volume administration. Although the accuracy of this system of measuring cardiac output has been criticized in some studies [35], a good agreement with the thermodilution technique was found in more recent papers [36]. Moreover, the ability to detect percentage changes in cardiac output following volume expansion seems to be comparable to the standard bolus thermodilution method [37]. Fifth, although patients were trained to perform a standardized VM, encouraging them to maintain a constant pressure of 30 cmH2O, we cannot guarantee a perfect pressure profile in all patients. Thus, some of the observed differences in the arterial pressure during the VM could be related to these discrepancies. However, the average airway pressure of the VM (a measure for the constant level of applied pressure) was not significantly different between both groups before and after fluid administration. Finally, we selected a 15% cut-off increase in SVi to characterize patients as responders to VE according to previous reported references [19, 20]. Since the intraobserver variability in cardiac output measurements has not been calculated in this study, this threshold may be inaccurate. Therefore, further studies on this regard should be performed.
In conclusion, the present study demonstrates that arterial pressure response to a 10-s VM could be a feasible and useful test to predict fluid responsiveness, without needing for any cardiac output monitoring device, in patients with suspected hypovolemia and without mechanical ventilatory support, completing the available tools to detect preload dependency in spontaneously breathing population, as the passive leg raising test.
References
Michard F, Teboul JL (2002) Predicting fluid responsiveness in ICU patients: a critical analysis of the evidence. Chest 121:2000–2008
De Backer D, Pinsky MR (2007) Can one predict fluid responsiveness in spontaneously breathing patients? Intensive Care Med 33:1111–1113
Heenen S, De Backer D, Vincent JL (2006) How can the response to volume expansion in patients with spontaneous respiratory movements be predicted? Crit Care 10:R102
Boulain T, Achard JM, Teboul JL, Richard C, Perrotin D, Ginies G (2002) Changes in BP induced by passive leg raising predict response to fluid loading in critically ill patients. Chest 121:1245–1252
Monnet X, Rienzo M, Osman D, Anguel N, Richard C, Pinsky MR, Teboul JL (2006) Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med 34:1402–1407
Lamia B, Ochagavia A, Monnet X, Chemla D, Richard C, Teboul JL (2007) Echocardiographic prediction of volume responsiveness in critically ill patients with spontaneously breathing activity. Intensive Care Med 33:1125–1132
De Backer D (2006) Can passive leg raising be used to guide fluid administration? Crit Care 10:170
Felker GM, Cuculich PS, Gheorghiade M (2006) The Valsalva maneuver: a bedside “biomarker” for heart failure. Am J Med 119:117–122
Zema MJ, Caccavano M, Kligfield P (1983) Detection of left ventricular dysfunction in ambulatory subjects with the bedside Valsalva maneuver. Am J Med 75:241–248
Remmen JJ, Aengevaeren WR, Verheugt FW, Jansen RW (2006) Detection of elevated pulmonary capillary wedge pressure in elderly patients with various cardiac disorders by the Valsalva manoeuvre. Clin Sci Lond 111:153–162
Weilenmann D, Rickli H, Follath F, Kiowski W, Brunner-La Rocca HP (2002) Noninvasive evaluation of pulmonary capillary wedge pressure by BP response to the Valsalva maneuver. Chest 122:140–145
Brunner-La Rocca HP, Weilenmann D, Rickli H, Follath F, Kiowski W (1999) Is blood pressure response to the Valsalva maneuver related to neurohormones, exercise capacity, and clinical findings in heart failure? Chest 116:861–867
Parisi AF, Harrington JJ, Askenazi J, Pratt RC, McIntyre KM (1976) Echocardiographic evaluation of the Valsalva Maneuver in healthy subjects and patients with and without heart failure. Circulation 54:921–927
Korner PI, Tonkin AM, Uther JB (1976) Reflex and mechanical circulatory effects of graded Valsalva maneuvers in normal man. J Appl Physiol 40:434–440
Stewart JM, Montgomery LD (2005) Reciprocal splanchnic-thoracic blood volume changes during the Valsalva maneuver. Am J Physiol Heart Circ Physiol 288:H752–H758
McIntyre KM, Scharf SM, Parisi AF (1989) The use of Valsalva and Mueller maneuvers as diagnostic tests for coronary artery disease. In: S SM, Cassidy SS (eds) Heart-lung interactions in health and disease. Marcel Dekker, New York, pp 1021–1046
De Lee GJ, Matthews MB, Sharpey-Schafer EP (1954) The effect of the Valsalva manoeuver on the systemic and pulmonary arterial pressure in man. Br Heart J 16:311–316
Judson WE, Hatcher JD, Wilkins RW (1955) Blood pressure responses to the Valsalva maneuver in cardiac patients with and without congestive failure. Circulation 11:889–899
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, Richard C, Pinsky MR, Teboul JL (2000) Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med 162:134–138
Tavernier B, Makhotine O, Lebuffe G, Dupont J, Scherpereel P (1998) Systolic pressure variation as a guide to fluid therapy in patients with sepsis-induced hypotension. Anesthesiology 89:1313–1321
Brooker JZ, Alderman EL, Harrison DC (1974) Alterations in left ventricular volumes induced by Valsalva manoeuvre. Br Heart J 36:713–718
Gindea AJ, Slater J, Kronzon I (1990) Doppler echocardiographic flow velocity measurements in the superior vena cava during the Valsalva maneuver in normal subjects. Am J Cardiol 65:1387–1391
Pinsky MR (1984) Instantaneous venous return curves in an intact canine preparation. J Appl Physiol 56:765–771
Pinsky MR (2005) Cardiovascular issues in respiratory care. Chest 128:592S–597S
Buda AJ, Pinsky MR, Ingels NB Jr, Daughters GT 2nd, Stinson EB, Alderman EL (1979) Effect of intrathoracic pressure on left ventricular performance. N Engl J Med 301:453–459
Santamore WP, Heckman JL, Bove AA (1984) Right and left ventricular pressure-volume response to respiratory maneuvers. J Appl Physiol 57:1520–1527
Scharf SM (2001) Ventilatory support in the falling heart. In: Scharf SM, Pinsky MR, Magder S (eds) Respiratory-circulatory interactions in health and disease. Marcel Dekker, New York, pp 519–550
Gorlin R, Knowles JH, Storey CF (1957) The Valsalva maneuver as a test of cardiac function; pathologic physiology and clinical significance. Am J Med 22:197–212
Little WC, Barr WK, Crawford MH (1985) Altered effect of the Valsalva maneuver on left ventricular volume in patients with cardiomyopathy. Circulation 71:227–233
Fritsch-Yelle JM, Convertino VA, Schlegel TT (1999) Acute manipulations of plasma volume alter arterial pressure responses during Valsalva maneuvers. J Appl Physiol 86:1852–1857
Wilkinson PL, Stowe DF, Tyberg JV, Parmley WW (1977) Pressure and flow changes during Valsalva-like maneuvers in dogs following volume infusion. Am J Physiol 233:H93–H99
Sharpey-Schafer EP (1955) Effects of Valsalva’s manoeuvre on the normal and failing circulation. Br Med J 1:693–695
Hamilton WF, Woodbury RA, Harper HTJ (1944) Arterial, cerebrospinal and venous pressures in man during cough and strain. Am J Physiol 141:42–50
Singer W, OpferGgehrking TL, McPhee BR, Hilz MJ, Low PA (2001) Influence of posture on the Valsalva manoeuvre. Clin Sci (Lond) 100:433–440
Mayer J, Boldt J, Schollhorn T, Rohm KD, Mengistu AM, Suttner S (2007) Semi-invasive monitoring of cardiac output by a new device using arterial pressure waveform analysis: a comparison with intermittent pulmonary artery thermodilution in patients undergoing cardiac surgery. Br J Anaesth 98:176–182
Mayer J, Boldt J, Wolf MW, Lang J, Suttner S (2008) Cardiac output derived from arterial pressure waveform analysis in patients undergoing cardiac surgery: validity of a second generation device. Anesth Analg 106:867–872
Cannesson M, Attof Y, Rosamel P, Joseph P, Bastien O, Lehot JJ (2007) Comparison of FloTracTM cardiac output monitoring system in patients undergoing coronary artery bypass grafting with pulmonary artery cardiac output measurements. Eur J Anaesthesiol 24:832–839
Monge García MI, Gil Cano A, Díaz Monrové JC (2008) Arterial pressure changes during the Valsalva maneuver to predict fluid responsiveness in spontaneously breathing patients. Crit Care 12(Suppl 2):P88
Acknowledgments
Part of this work was presented in the twenty-eighth International Symposium on Intensive Care and Emergency Medicine, 2008, Brussels, Belgium, and published as abstract [38].
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: doi:10.1007/s00134-008-1294-2.
Electronic supplementary material
Below is the link to the electronic supplementary material.
134_2008_1295_MOESM1_ESM.doc
Arterial pressure changes during the Valsalva maneuver to predict fluid responsiveness in spontaneously breathing patients (DOC 1223 kb)
Rights and permissions
About this article
Cite this article
Monge García, M.I., Gil Cano, A. & Díaz Monrové, J.C. Arterial pressure changes during the Valsalva maneuver to predict fluid responsiveness in spontaneously breathing patients. Intensive Care Med 35, 77–84 (2009). https://doi.org/10.1007/s00134-008-1295-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1295-1