Abstract
Objective
To examine the effect of intratracheal heparin instillation on Legionella pneumophila-related acute lung injury (ALI) and systemic dissemination.
Design
Prospective, controlled experimental study.
Setting
University research laboratory.
Interventions
A/J mice received 5 μg of sulfated heparin intratracheally co-instilled with 106 or 108 colony-forming units (CFU) of a virulent isolate of L. pneumophila.
Measurements and results
ALI was assessed in control groups (PBS and PBS-heparin) and on days 1, 2 and 3 post-infection, in terms of the lung wet-to-dry (W/D) weight ratios and of lung endothelial permeability to radio-labeled albumin (Perm-I125). Lung bacterial loads were measured and systemic spread was assessed by blood and target organ culture. The alveolar inflammatory response was evaluated by measuring the cytokine levels (TNF-α, IFN-γ, IL-6 and IL-12p70) in bronchoalveolar lavage fluids (BALF). Co-instilled heparin improved mouse survival after the 108 CFU challenge (p < 0.01). On day 2, heparin co-instillation significantly reduced the W/D ratio and Perm-I125 (p < 0.01 and p < 0.001 respectively), improved lung bacterial clearance (p < 0.001), prevented systemic dissemination (blood, liver, spleen, kidneys and brain cultures, all p < 0.05) and significantly increased IFN-γ and IL-12p70 levels in BALF (p < 0.05).
Conclusions
Heparin co-instillation during intratracheal L. pneumophila challenge has a protective effect on the alveolar–capillary barrier and prevents bacterial dissemination. These results tend to confirm the competitive inhibition by heparin of L. pneumophila attachment to lung epithelium in vivo, and point to the possible involvement of a heparan-sulfate adhesin in L. pneumophila binding to pneumocytes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Legionella pneumophila, a Gram-negative facultative intracellular pathogen, is the causative agent of legionellosis. L. pneumophila causes legionnaires’ disease, a severe form of pneumonia, and Pontiac fever, a milder illness. An estimated 8,000 to 18,000 people contract legionnaires’ disease in the USA every year [1]. When reaching lung alveoli after inhalation in aerosols, L. pneumophila attaches to and is internalized by alveolar macrophages and epithelial cells [2–5]. L. pneumophila then replicates within host cells in a parasitic relationship. The hallmarks of human bacterial pneumonia are increased alveolar permeability with edema and gradual impairment of gas exchanges due to alveolar–capillary barrier injury; these changes are collectively referred to as acute lung injury (ALI) [6, 7]. ALI can be studied in murine models by measuring functional parameters such as lung extravascular water, alveolar – capillary membrane permeability and the lung inflammatory response [8, 9]. Cytokine production during L. pneumophila infection has been characterized as a T1 polarization [10–14].
In the susceptible hosts, pathogens adhere to target tissues in order to escape mechanical clearance and to establish an infectious focus from which dissemination may occur. A number of saccharides can inhibit L. pneumophila attachment to the human respiratory cell line A549 [15, 16]. Polymeric sulfated saccharide heparin is among the most efficient competitive inhibitors of L. pneumophila attachment to A549 cells [15], suggesting that bacteria bind to sulfated glycosaminoglycans borne by trans-membrane proteoglycans (PGs) at the surface of host alveolar pneumocytes. This attachment involves a specialized microbial surface-exposed adhesin [17]. Adhesion to and subsequent invasion of pneumocytes could be an important pathway of ALI development and bacterial dissemination in L. pneumophila pneumonia and could thus represent an attractive therapeutic target. To test the hypothesis that pneumocyte adhesion is central to the pulmonary pathogenicity of L. pneumophila, we examined whether inhibition of bacterial adhesion to lung epithelia through the use of a known competitive inhibitor, sulfated heparin, would reduce L. pneumophila-related ALI, prevent extrapulmonary bacterial dissemination and modulate host cytokine responses.
An experimental A/J mouse model of L. pneumophila lung infection was set up for this study. L. pneumophila-induced ALI was studied in mice that received a single intratracheal dose of heparin by measuring the lung wet-to-dry lung tissue weight ratio and by assessing alveolar–capillary barrier permeability. Bacterial clearance was assessed by measuring the lung bacterial load over time. Extrapulmonary dissemination was assessed by testing blood and target organs (liver, spleen, kidneys and brain) for L. pneumophila. The cytokine response was assessed by measuring IFN-γ, TNF-α, and IL-6, -10, and -12p70 in bronchoalveolar lavage fluid.
Materials and methods
Animals
Female pathogen-free 8- to 9-week-old A/J mice (Harlan UK Laboratory, Oxford, UK) were used for all experiments. They were housed in the Lille University Animal Care Facility and provided with food and water ad libitum. All the experiments were approved by the Lille Institutional Animal Care and Use Committee.
Bacteria and culture conditions
The clinical strain L. pneumophila serogroup 1 strain Lens wild type was kindly provide by the French National Reference Center for Legionella. This epidemic strain, which was recently sequenced, caused the largest outbreak of community-acquired legionnaires’ disease in France (2003–2004), with a high case fatality rate (21%) [18, 19]. It was grown on buffered charcoal-yeast extract (BCYE) agar with L-cysteine (bioMerieux, Marcy l’Etoile, France) for 48 h. For mouse challenge, colonies were resuspended in sterile phosphate buffered saline (PBS) at 2 × 107 colony-forming units (CFU)/ml or 2 × 109 CFU/ml according to the group.
Preparation of a heparin instillate
Lipopolysaccharide-free sulfated heparin sodium salt with an average molecular weight of 6,000 Da extracted from porcine intestinal mucosa (Sigma-Aldrich, USA) was added to PBS and to PBS bacterial suspension at a concentration of 100 μg/ml corresponding to 5 μg of heparin per mouse, 30 min prior to instillation.
Mouse challenge
A/J mice were infected by intratracheal (i.t.) inoculation, in dorsal recumbence, after sevoflurane anesthesia (Servorane™, Abbott, UK). A 24-G animal feeding needle was used to instill 50 μl of bacterial suspension (106 or 108 bacteria per mouse). Negative control mice received 50 μl of sterile PBS or PBS-heparin in the same conditions.
Bacterial cultures
Immediately after the instillation (T0) and on days 1, 2 and 3, groups of mice were exsanguinated by intracardiac puncture. The lungs, liver, spleen, kidneys and brain were aseptically removed. The organs were homogenized in sterile containers with 1 ml of sterile PBS, serially diluted, and cultured on Legionella BCYE agar plates for 3 days at 37°C. The results were expressed in CFU/ml.
Bacteria were also quantified 5 h post-infection. Mice were killed humanely, and bronchoalveolar lavage (BAL) was performed by cannulating the trachea with a 22-G catheter and 1.5 ml of sterile PBS. The BAL samples were filtered (5 μm pore size) to eliminate resident phagocytes. They were then serially diluted and cultured on Legionella BCYE agar plates for 3 days at 37°C.
Evaluation of alveolar–capillary barrier injury
Albumin flux across the endothelial barrier was measured with a method initially described for use in a rat model [20]. Briefly, 0.5 ml of 125I-labeled bovine serum albumin (1 µCi) (HAS; CIS Biointernational, Gif-sur-Yvette, France) was injected intraperitoneally 2 h before intraperitoneal injection of pentobarbital sodium (Sanofi, Libourne, France), followed by sternotomy, exsanguination and lung removal. Radioactivity and the hemoglobin (Hb) concentration were measured in blood. The lungs were weighed and radioactivity was counted prior to homogenization and centrifugation (Polytron, PT 1600E; Fischer Bioblock Scientific, Switzerland). The Hb content of the supernatant was also measured. Blood and lung-homogenate samples were then desiccated to calculate extravascular lung water. The wet-to-dry weight ratio (W/D) of each pair of lungs was determined from the difference between the wet weight and the dry weight (measured after 7 days in a 37°C incubator) [8]. A permeability index was used to express the permeability of the alveolar–capillary membrane [20].
Cytokine levels in BAL fluid
At T0 and on days 1 and 2 post-inoculation, groups of mice were killed humanely and their lungs were lavaged with two 0.8-ml aliquots of sterile PBS. BAL fluid was filtered and immediately frozen at –80°C after collection. It was then concentrated down to 50 µl by ultrafiltration on a Millipore Ultrafree-0.5 filter device (Biomax-5 membrane). BAL cytokines were quantified with BD™ Cytometric Bead Array (CBA) technology (Becton-Dickinson), which employs a series of particles with discrete fluorescence intensities to simultaneously detect multiple soluble analytes in a small sample volume. The BD™ CBA Mouse Inflammation Kit was used as recommended by the supplier to quantitatively measure gamma interferon (IFN-γ), tumor necrosis factor alpha (TNF-α), and interleukin-6 (IL-6) and -12p70 (IL-12p70) levels in the different samples. Briefly, each concentrated BAL sample was incubated for 2 h at room temperature in the presence of mixed antigen-coupled beads (50 ml) and Phycoerythrin Detection Reagent (50 ml), followed by two washes. Bead fluorescence was then measured using the BD FACSArray™ Bioanalyzer. The median relative fluorescence intensities were converted into cytokine concentrations by using nine-point calibration curves created by serially diluting cytokine standards.
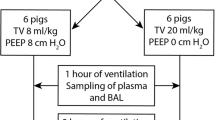
Experimental groups
The experimental groups were: the controls instilled with sterile PBS or PBS containing 100 µg/ml of heparin (n = 5 per group) and the infected groups challenged i.t. with L. pneumophila strain Lens with or without 100 µg/ml of co-instilled heparin (n = 8 per group). Groups of animals were killed humanely at T0 and on days 1, 2 and 3. All the experiments were conducted in duplicate, except for bacterial load assay in blood and peripheral target organs.
Statistical analysis
Mortality rates were compared between groups by using the log-rank test with Kaplan–Meier analysis. Bacterial loads in blood and organs were compared with the χ2 test (with Yates correction if necessary) and BAL fluid culture results with the Mann–Whitney U test. Quantitative parameters were compared using two-way analysis of variance (ANOVA). Post hoc comparisons used the Bonferroni’s test (Version 4.00, Graph Pad Prism, USA). Data are expressed as means ± standard error of the mean (SEM). P values below 0.05 were considered as significant.
Results
Effect of co-instilled heparin on mouse survival
A set of in vitro work demonstrated that heparin inhibits L. pneumophila adhesion to human bronchial and alveolar cell lines [15, 16]. This effect was observed in a concentration-dependent manner with a maximum efficacy at 100 µg of heparin in the medium culture (data not shown). For this reason, this dose only was tested in the study, which was not designed to be an in vivo dose-response study.
Survival was recorded for 7 days after i.t. challenge with non-lethal and lethal doses of L. pneumophila (106 and 108 CFU respectively) (Fig. 1). The survival rate on day 7 was 100% with the non-lethal challenge, regardless of heparin co-instillation. With the lethal challenge, the survival rate on day 7 was 0% without heparin co-instillation and 30% with heparin co-instillation (p < 0.01). Thus, co-instilled heparin improved the survival after L. pneumophila challenge.
Effect of co-instilled heparin on lung and BAL fluid bacterial loads
As previously described with L. pneumophila strain Philadelphia [10], the number of bacteria in the lungs increased exponentially until day 2 and started to decline on day 3 (Fig. 2a). In heparin co-instilled mice, the lung bacterial load tended to be lower than in L. pneumophila-instilled mice on day 1 and the difference reached statistical significance on day 2 (p < 0.001). Lung counts started to decline on day 3 in both groups. Thus, co-instilled heparin increased L. pneumophila clearance from lungs.
Effect of co-instilled heparin on lung and BAL fluid bacterial loads in L. pneumophila pneumonia. a The number of colony-forming units (CFU) in lungs at T0 and days 1, 2 and 3. b CFU were counted on BCYE plates in filtered BAL fluids collected 5 h post-challenge. The data are means ± standard error (SE) (indicated by error bars). N = 5 mice in control groups, n = 8 mice in infected groups. ***p < 0.001 vs. L.p Lens+Hp, **p < 0.01 vs L.p Lens. The data were confirmed in a replicate experiment
To examine whether heparin blocked L. pneumophila primary adhesion to airway epithelial cells, filtered acellular BAL fluid was obtained 5 h after instillation and cultured. Bacterial counts were significantly higher in co-instilled heparin mice than in L. pneumophila-instilled mice (p < 0.05) (Fig. 2b).
Effect of co-instilled heparin on L. pneumophila-related alveolar–capillary barrier injury
A dynamic time-course analysis of the extra-vascular lung water and the protein flux across endothelial barrier was performed from days 1 to 3 post-challenge with L. pneumophila. Pharmacokinetics of heparin instilled into the lungs in a liquid form are not well known, but those of heparin inhaled into the lungs have been published [21, 22]. Therefore, we deduced that the residual amount of 5 µg of heparin in the lungs past 48 h was likely to be negligible and we did not pursue the experiments in the control heparin-instilled mice past this time-point.
In L. pneumophila-instilled groups, the lung W/D weight ratio doubled on day 2 post-challenge and started to decline on day 3 (Fig. 3a). Heparin did not affect this ratio in uninfected mice. In infected mice, however, co-instilled heparin significantly attenuated the increase on day 2 (p< 0.01).
Effect of co-instilled heparin on L. pneumophila-related alveolar–capillary barrier injury at days 1, 2 and 3 post-infection. a evaluation of the wet-to-dry lung weight ratios (W/D). b evaluation of endothelial permeability (EP) of the alveolar–capillary barrier to 125I-labeled bovine serum albumin. The data are means ± SE (indicated by error bars). N = 5 mice in control groups, n = 8 mice in infected groups. **p < 0.01 vs. L.p Lens+Hp, ***p < 0.001 vs. L.p Lens+Hp, *p < 0.05 vs. L.p Lens+Hp. The data were confirmed in a replicate experiment
Endothelial permeability measured after IP injection of 125I-labeled albumin increased threefold in the first 2 days in L. pneumophila-instilled mice and started to decline on day 3 (Fig. 3b). Consistently with former W/D results, co-instilled heparin did not affect endothelial permeability in uninfected mice. In infected mice, however, co-instilled heparin significantly attenuated the increase in endothelial permeability on days 2 and 3 (p < 0.001 and p < 0.05 respectively).
Thus, alveolar–capillary barrier injury was roughly halved on day 2 when heparin was co-instilled with L. pneumophila, and no rebound effect was noted.
Effect of co-instilled heparin on extrapulmonary dissemination of L. pneumophila
In L. pneumophila-instilled mice, bacterial translocation from the lungs was detectable on day 1 (Table 1). On day 2, L. pneumophila culture was positive in the liver, kidneys and spleen (87%, 80% and 71% respectively) than in blood and brain (about 50% for both). Heparin co-instillation roughly halved the rates of positive blood cultures and prevented brain infection on day 1. On day 2, in heparin co-instilled mice, blood, liver, kidney spleen and brain culture positivity rates were 4%, 20%, 10%, 30% and 0% respectively, representing a drastic L. pneumophila growth restriction in this group (all p < 0.05 versus L. pneumophila-instilled group).
Effect of co-instilled heparin on lung proinflammatory cytokine levels
On day 2, TNF-α production was significantly higher in L. pneumophila-instilled group than in control heparin and heparin co-instilled groups (p < 0.01 and p < 0.05 respectively) whereas no difference in IL-6 levels was noted (Fig. 4a, b). IFN-γ and IL-12p70 levels increased significantly more from day 1 to 2 in co-instilled heparin groups than in heparin control and L. pneumophila-instilled groups (for both cytokines p < 0.01 and p < 0.05 respectively) (Fig. 4c, d).
Effect of co-instilled heparin on cytokine concentrations (pg/ml) in bronchoalveolar lavage fluid (BALF) on days 1 and 2 of L. pneumophila challenge. a TNF-α levels; b IL-6 levels; c IFN-γ levels; d IL-12p70 levels. The data are means ± SE (indicated by error bars). N = 5 mice in control groups and n = 8 mice in infected groups. #p < 0.05 vs. L.p Lens+Hp, *p < 0.05 vs. L.p Lens, ººp < 0.01 vs. Hp. The data were confirmed in a replicate experiment
Thus, co-instilled heparin led to a dissociated pattern of inflammation from day 1 to 2, with a minor increase in the acute-phase cytokine TNF-α and a major increase in the Th1 cytokines IFN-γ and IL-12p70.
Discussion
In this study, a single intratracheal dose of sulfated heparin co-instilled with a virulent isolate of L. pneumophila in A/J mouse lungs lowered the mortality rate, protected the alveolar–capillary barrier, prevented systemic bacterial dissemination and stimulated Th1 cytokine production.
To characterize the anti-adhesion effect of heparin, we chose a bacterial inoculum of 106 cells per mouse, which mimics fairly mild legionnaires’ disease [10]. A single dose of heparin was instilled along with L. pneumophila as uptake of this pathogen by host cells occurs within minutes after entry into the lung alveoli [23].
A preliminary in vitro study showed differences in the ability of some L. pneumophila mutants to attach to macrophages and respiratory epithelial cells, indicating that some of the mechanisms of attachment are different [5]. The molecular mechanisms underlying L. pneumophila invasion of respiratory epithelial cells, which constitute more than 95% of the surface area of the alveolar surface area, are poorly known, including the nature of the host receptor involved in a non-complement-mediated uptake. Many microorganisms express adhesins that bind sulfated glycosaminoglycans (GAGs) borne by proteoglycans (PGs) at the surface of host epithelial cells. Bacterial interaction with PGs facilitates epithelial cell invasion by Neisseria gonorrhoeae and systemic dissemination of Mycobacterium tuberculosis [24, 25]. L. pneumophila shares many traits with M. tuberculosis, such as initial pulmonary infection, spread to other tissues, and the use of professional alveolar phagocytes as a major site of replication. Interactions with non-phagocytic cells may also have an important role in the pathogenesis of legionnaires’ disease. M. tuberculosis complex strains produce at their surface a protein named heparin-binding hemagglutinin adhesin (HBHA) [26]. Binding of M. tuberculosis to epithelial cells, but not to macrophages, can be inhibited by anti-HBHA antibodies and by competition with heparin, which is a highly acidic mucopolysaccharide with sulfaminic bridges, suggesting that HBHA-mediated adherence is specific for non-phagocytic cells [26]. In vitro, heparin inhibited the adhesion of L. pneumophila to human bronchial and alveolar cell lines by 93% and 60% respectively [15, 16]. These percentages suggest that more than half of the epithelial cells receptors involved in L. pneumophila attachment are heparan sulfate molecules. The main consequence of the anti-adhesion effect of sulfated heparin may be the trapping of “free” heparin-coated forms of L. pneumophila unable to adhere to airway epithelial cells in the alveolar spaces. Two findings favor this hypothesis: first, filtered BAL fluids cultures collected 5 h post-infection contained a larger number of cultivable bacteria when heparin was co-instilled. The 5-h time point was too early for L. pneumophila replication to have occurred in alveolar macrophages. Second, the amount of L. pneumophila released in the lungs during the first 48 h was lower in heparin co-instilled mice than in L. pneumophila-instilled mice. This could explain the limited alveolar–capillary barrier damages in the presence of heparin, as shown by a 50% decrease in extravascular lung water and in endothelial permeability to radiolabeled albumin. Heparin inhibition of L. pneumophila epithelial adhesion might also explain the lower systemic spread measured by blood and organ culture. Finally, the larger amounts of IFN-γ and IL-12p70 in BAL fluid on day 2 may be related to the increased numbers of non-adherent “free” forms of bacteria in the alveolar spaces of heparin-treated animals. Indeed, IFN-γ and IL-12p70 are two Th1 cytokines involved in the host response to pathogens, and particularly in restriction of bacterial growth and clearance from infected sites [27–29]. The conjunction of all these factors would tend to limit L. pneumophila pathogenicity and dissemination, ultimately leading to improved animal survival.
Although there are no studies in the specific context of L. pneumophila pneumonia, ALI leads to systemic and local lung imbalances in coagulant factors, resulting in fibrin deposition [30]. In addition, levels of natural anticoagulants such as activated protein C (APC), antithrombin (AT) and tissue factor pathway inhibitor (TFPI) decline during sepsis, owing both to decreased production and to enhanced breakdown [31]. As heparin is not inert with respect to coagulation, and possibly inflammation too, the effect of heparin observed in this study at the very beginning of the infectious process could also be due in part to these effects. However, heparin effects on both coagulation and inflammation are controversial. In human healthy volunteers, inhaled heparin reduced the level of inflammatory mediators such as histamine and increased TFPI release in blood [32]. These data were not confirmed in a smoke inhalation-induced lung injury model, which could reduce neither lung dysfunction nor leukocyte accumulation [33]. In fact, exogenous heparin exhibits paradoxical in vitro functioning, since it is an acceleratory cofactor for anticoagulant AT but can also induce its inactivation in pathologic conditions reinforcing procoagulant activity [34, 35]. Thus, the in vivo ability of heparin to block fibrin deposition in the lung and thereby to improve lung function is uncertain [36]. This is why attempts to prevent fibrin deposition in human pneumosepsis have evolved toward natural anticoagulant systemic supply, such as APC [37, 38].
In the setting of L. pneumophila-related ALI, a strategy capable of preventing primary bacterial attachment to airway epithelial cells might limit the pulmonary pathogenicity of this microorganism. The protective effect of heparin in vivo indirectly supports the evidence of a bacterial mechanism of attachment operating through the binding to pneumocyte surface GAGs. Attempts are underway to identify L. pneumophila GAG-binding adhesin(s). This would provide the possibility of developing new specific anti-adhesive therapy that might be a potential alternative to conventional antimicrobial chemotherapy.
References
Benin AL, Benson RF, Besser RE (2002) Trends in Legionnaire's disease, 1980–1998: declining mortality and new patterns of diagnosis. Clin Infect Dis 35:1039–1046
Fields BC (2002) Legionella and Legionnaires'disease: 25 years of investigation. Clin Microbiol Rev 15:506–526
Molofski AB, Swanson MS (2004) Differentiate to thrive: lessons from the Legionella pneumophila life cycle. Mol Microbiol 53:29–40
Mody CH, Paine R IIId, Shahrabadi MS, Simon RH, Pearlman E, Eiser BI, Toews GB (1993) Legionella pneumophila replicates within rat alveolar epithelium. J Infect Dis 167:1138–1145
Gao LY, Stone BJ, Brieland JK, Abu Kwaik Y (1998) Different fates of Legionella pneumophila pmi and mil mutants within macrophages and alveolar epithelial cells. Microb Pathog 25:291–306
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R (1994) The American-European consensus conference on ARDS. Definitions, mechanisms, relevant outcomes and clinical trial coordination. Am J Crit Care Med 149:818–824
Ware LB, Matthay MA (2000) The acute respiratory distress syndrome. N Engl J Med 342:1334–1349
Parker JC, Townsley MI (2004) Evaluation of lung injury in rats and mice. Am J Physiol Lung Cell Mol Physiol 286:L231–L246
Wiener-Kronish JP, Franck D, Sawa T (2001) In: Wong HR, Shanley TP (eds) Molecular biology of acute lung injury. Kluwer Academic, Boston, pp 149–161
Brieland J, Freeman P, Kunkel R, Chrisp C, Hurley M, Fantone J, Engleberg C (1994) Replicative lung infection in intratracheal inoculated A/J mice. A murine model of human Legionnaires' disease. Am J Pathol 145:1537–1546
Newton C, McHugh S, Widen R, Nakachi N, Klein T, Friedman H (2000) Induction of interleukin-4 (IL-4) by Legionella pneumophila infection in BALB/c mice and regulation of tumor necrosis factor alpha, IL-6, and IL-1β. Infect Immun 68:5234–5240
Susa M, Ticac B, Rukavina T, Doric M, Marre R (1998) Legionella pneumophila infection in intratracheally inoculated T cell-depleted or -nondepleted A/J mice. J Immunol 160:316–321
Tateda K, Matsumoto T, Ishii Y, Furuya N, Onho A, Miyazaki S, Yamaguchi K (1998) Serum cytokines in patients with Legionella pneumophila: relative predominance of Th1-type cytokines. Clin Diag Lab Immunol 5:401–403
Brieland JK, Freeman DG, Hurley DC, Fantone JC, Engleberg NC (1995) In vivo regulation of replicative Legionella pneumophila lung infection by endogenous tumor necrosis factor alpha and nitric oxide. Infect Immun 63:3253–3258
Thomas RJ, Brooks TJ (2004) Oligosaccharide receptor mimics inhibit Legionella pneumophila attachment to human respiratory epithelial cells. Microb Pathog 36:83–92
Yaradou DF, Raze D, Ginevra C, Ader F, Doléans A, Vandenesch F, Menozzi FD, Etienne J, Jarraud S (2007) Zinc dependent cytoadherence of Legionella pneumophila on human alveolar epithelial cells. Microb Pathog 43:234–242
Menozzi FD, Pethe K, Bifani P, Soncin F, Brennan MJ, Locht C (2002) Enhanced bacterial virulence through exploitation of host glycosaminoglycans. Mol Microbiol 43:1379–1386
Cazalet C, Rusniok C, Brüggemann H, Zidane N, Magnier N, Ma L, Tichit M, Jarraud S, Bouchier C, Vandenesch F, Kunst F, Etienne J, Glaser P, Buchrieser C (2004) Evidence in the Legionella pneumophila genome for exploitation of host cell functions and high genome plasticity. Nat Gen 36:1165–1173
Nguyen TMN, Ilef D, Jarraud S, Rouil L, Campese C, Che D, Haeghebaert S, Ganiayre F, Marcel F, Etienne J, Desenclos JC (2006) A community-wide outbreak of Legionnaires disease linked to industrial cooling towers. How far can contaminated aerosols spread? J Infect Dis 193:102–111
Jayr C, Garat C, Meignan M, Pittet JF, Zelter M, Matthay MA (1994) Alveolar liquid and protein clearance in anesthetized ventilated rats. J Appl Physiol 76:2636–2642
Garrigo J, Danta I, Ahmed T (1996) Time course of the protective effect of inhaled heparin on exercise-induced asthma. Am J Respir Crit Care Med 153:1702–1707
Bendstrup KE, Chambers CB, Jensen JI, Newhouse MT (1999) Lung deposition and clearance of inhaled 99mTc-heparin in healthy volunteers. Am J Respir Crit Care Med 160:1653–1658
Molmeret M, Bitar DM, Han L, Abu Kwaik Y (2004) Cell biology of the intracellular infection by Legionella pneumophila. Microbes Infection 6:129–139
Freissler E, Meyer auf der Heyde A, David G, Meyer TF, Dehio C (2000) Syndecan-1 and syndecan-4 can mediate the invasion of OpaHSPG-expressing Neisseria gonorrhoeae into epithelial cells. Cell Microbiol 2:69–82
Pethe K, Alonso S, Blet F, Delogu G, Brennan MJ, Locht C, Menozzi FD (2001) The heparin-binding haemagglutinin of M. tuberculosis is required for extrapulmonary dissemination. Nature 412:190–194
Menozzi FD, Rouse JH, Alavi M, Laude-Sharp M, Muller J, Bischoff R, Brennan MJ, Locht C (1996) Identification of a heparin-binding hemagglutinin present in mycobacteria. J Exp Med 184:993–1001
Gebran SJ, Yamamoto Y, Newton C, Klein TW, Friedman H (1994) Inhibition of Legionella pneumophila growth by gamma interferon in permissive A/J mouse macrophages: role of reactive oxygen species, nitric oxide, tryptophan, and iron III. Infect Immun 62:3197–3205
Brieland JK, Remick DG, LeGendre ML, Engleberg NC, Fantone JC (1998) In vivo regulation of replicative Legionella pneumophila lung infection by endogenous interleukin-12. Infect Immun 66:65–69
Deng JC, Tateda K, Zeng X, Standiford TJ (2001) Transient transgenic expression of gamma interferon promotes Legionella pneumophila clearance in immunocompetent hosts. Infect Immun 69:6382–6390
Levi M, Ten Cate H (1999) Disseminated intravascular coagulation. N Engl J Med 34:586–592
Fourrier F, Chopin C, Goudemand J, Hendrycs S, Caron C, Rime A, Marey A, Lestavel P (1992) Septic shock, multiple organ failure, and disseminated intravascular coagulation. Compared patterns of antithrombin III, protein C, and protein S deficiencies. Chest 101:816–823
Bendstrup KE, Gram J, Jensen JI (2002) Effect of inhaled heparin on lung function and coagulation in healthy volunteers. Eur Respir J 19:606–610
Tasaki O, Mozingo DW, Dubick MA, Goodwin CW, Yantis LD, Pruitt BA (2002) Effects of heparin and lisofylline on pulmonary function after smoke inhalation injury in an ovine model. Crit Care Med 30:637–643
Jordan RE, Nelson RM, Kilpatrick J, Newgren JO, Esmon PC, Fournel MA (1989) Antithrombin inactivation by neutrophil elastase requires heparin. Am J Med 87:19S–22S
Rao LV, Nordfang O, Hoang AD, Pendurthi UR (1995) Mechanism of antithrombin III inhibition of factor VIIa/tissue factor activity on cell surfaces. Comparison with tissue factor pathway inhibitor/factor Xa-induced inhibition of factor VIIa/tissue factor activity. Blood 85:121–129
Laterre PF, Wittebole X, Dhainaut JF (2003) Anticoagulant therapy in acute lung injury. Crit Care Med 31:S329–S336
Laterre PF, Garber G, Levy H, Wunderink R, Kinasewitz GT, Sollet JP, Maki DG, Bates B, Yan SC, Dhainaut JF; PROWESS Clinical Evaluation Committee (2005). Severe community-acquired pneumonia as a cause of severe sepsis: data from the PROWESS study. Crit Care Med 33:952–961
Schultz MJ, Haitsma JJ, Zhang H, Slutsky AS (2006) Pulmonary coagulopathy as a new target in therapeutic studies of acute lung injury or pneumonia. A review. Crit Care Med 34:871–877
Acknowledgements
This study was supported by grants from Collège français des universitaires de Maladies Infectieuses et Tropicales (CMIT) and by Agence française de sécurité sanitaire de l’environnement et du travail (Afsset). The authors thank Dr. Bruno Cardinaud and Dr. Elizabeth Pradel for substantial assistance with work relevant to the study and David Young for editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Franco Dante Menozzi has died since this study was conducted.
Rights and permissions
About this article
Cite this article
Ader, F., Le Berre, R., Fackeure, R. et al. In vivo effect of adhesion inhibitor heparin on Legionella pneumophila pathogenesis in a murine pneumonia model. Intensive Care Med 34, 1511–1519 (2008). https://doi.org/10.1007/s00134-008-1063-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1063-2