Abstract
Objective
To compare the characteristics and outcome of patients with hematological malignancies referred to the ICU with severe sepsis and septic shock who had or had not received recent intravenous chemotherapy, defined as within 3 weeks prior to ICU admission.
Design and setting
Retrospective observational cohort study on prospectively collected data in a medical ICU of a university hospital.
Patients
186 ICU patients with hematological malignancies with severe sepsis or septic shock (2000–2006).
Measurements and results
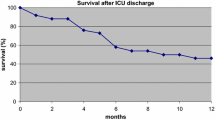
There were 77 patients admitted with severe sepsis and 109 with septic shock; 91 (49%) had received recent intravenous chemotherapy. Patients with recent chemotherapy more often had a high-grade malignancy and were more often neutropenic, less often had pulmonary infiltrates, and less often required mechanical ventilation. ICU, 28-day, in-hospital, and 6-month mortality rates were 33% vs. 48.4%, 40.7% vs. 57.4%, 45.1% vs. 58.9%, and 50.5% vs. 63.2% in patients with and without recent chemotherapy, respectively. Logistic regression identified four variables independently associated with 28-day mortality: SOFA score at ICU admission, pulmonary site of infection, and fungal infection were associated with worse outcome whereas previous intravenous chemotherapy was protective at borderline significance. After adjustment with a propensity score for recent chemotherapy, chemotherapy was not associated with outcome.
Conclusions
Patients referred to the ICU with severe sepsis and septic shock complicating active chemotherapeutic treatment have better prognosis than commonly perceived.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past two decades there has been a tremendous improvement in outcome of cancer patients and more particularly in those with hematological malignancies [1]. This can be attributed to the use of more aggressive chemo- and radiotherapy with or without bone marrow or stem cell rescue, and to advances in supportive care. Unfortunately, these new aggressive treatment modalities may lead to life-threatening complications requiring intensive care unit (ICU) admission. Although admission of these patients remains a matter of debate and controversy [2, 3], several centers over the world have shown that it is possible to achieve meaningful prognosis in these patients [1, 4–10], even in the most severely ill subgroups, such as those requiring mechanical ventilation [6, 7, 11, 12], renal replacement therapy [2, 13–15], or chemotherapy in an urgent setting [14, 16]. Infection is a common and dreaded complication in hemato-oncological patients [8, 17], and developing severe sepsis or septic shock after having received chemotherapy is often considered a worst case scenario in this population [13, 17]. However, only few studies have focused on cancer patients who were referred to the ICU with severe sepsis and septic shock [8,18, 19] and more particularly on the impact of previous chemotherapy in this setting.
The present study examined the characteristics and outcome of patients with hematological malignancies admitted to the ICU with severe sepsis and septic shock and compared patients treated with or without recent intravenous chemotherapy. The findings of this study were presented in part at the 2007 Annual Congress of the European Society of Intensive Care Medicine in Barcelona.
Materials and methods
Setting
The study was conducted at the medical ICU of the 1062-bed Ghent University Hospital. This ICU has 14 beds and admits only adults (> 15 years). Over the study period 186 patients with hematological malignancies were admitted to the ICU with severe sepsis (n = 77) or septic shock (n = 109). Of these, 91 (48.9%) had received intravenous chemotherapy within 3 weeks before referral to the ICU. Admission diagnoses are listed in Table 1. The characteristics of our ICU regarding organization, patient management, and end-of-life policy have been presented elsewhere [16]. In our institution patients who receive cyclic chemotherapy and who are at risk of moderate to severe temporary neutropenia are treated ambulatory and do not receive antimicrobial prophylaxis. Patients such as those with acute myelogenous leukemia, who are at risk of prolonged severe neutropenia, remain in the hospital and receive selective bowel decontamination consisting of colimycin (polymyxin B) and fluconazole prophylaxis. Cotrimoxazole prophylaxis is restricted to patients at risk of Pneumocystis pneumonia, such as those with lymphoblastic malignancies and bone marrow transplant recipients. Acyclovir is restricted for the transplant setting. Neutropenic fever is treated according to international guidelines [17]. All patients in our study were treated according to the guidelines proposed by the Surviving Sepsis Campaign [20]. In our cohort only two patients received activated protein C.
Study design
A retrospective analysis was performed on prospectively collected data of all consecutive patients with hematological malignancies who were admitted to the ICU with either severe sepsis or septic shock from 2000 through 2006. The following variables were collected: age, gender, type of hematological malignancy and disease status, need for mechanical ventilation and duration of ventilation, need for vasopressor drugs, need for renal replacement therapy, presence of infection, site of infection, causative pathogen, use of antimicrobials within 24 h before ICU admission, use of a combination of antibiotic regimens before ICU admission, length of hospitalization before ICU admission and length of stay in the ICU and hospital. Patients were categorized according to whether they had (CHT) or had not received intravenous chemotherapy within 3 weeks prior to ICU admission (nCHT). This cutoff was chosen arbitrarily at the start of data collection with the intention of categorizing all potentially severely immunocompromised patients regardless of the presence or absence of neutropenia at the moment of ICU admission. Severity of illness on the first day of ICU admission was assessed by using the Acute Physiology and Chronic Health Evaluation (APACHE) II score, Sequential Organ Failure Assessment (SOFA) score, and Cancer-Specific Severity of Illness Score (CSSIS) [21]. The latter is a logistic regression model for estimating the probability of hospital mortality and consisting of 16 unambiguous and readily available physiological, laboratory variables, cancer specific variables, and the length of hospitalization before ICU admission. This score is based on prospectively collected data of more than 1,400 patients admitted to four ICUs in the United States and has previously been validated [21]. ICU, 28-day, in-hospital, and 6-month mortality were also recorded.
Until 2004 an independent panel of physicians blinded to patients' outcome categorized the patients according to the severity of infection (sepsis, severe sepsis or septic shock) using the criteria defined by the International Sepsis Definitions Conference in 2001 [22], the diagnostic certainty (documented or clinically suspected), and the site of infection (pulmonary vs. nonpulmonary) as previously described [8]. To be included in the septic shock subgroup patients had to receive vasoactive therapy within 24 h following ICU admission, otherwise they were categorized in the severe sepsis subgroup. Patients were considered to have fungal infection if they fulfilled the criteria of confirmed or probable fungal infection as defined by a recent international consensus meeting [23]. Since 2004 patients have been categorized by at least two senior physicians experienced in the management of cancer patients within 48 h after ICU admission. We found no difference in incidence neither in mortality rates within these subgroups between the two periods (data not shown).
Definitions
The type of hematological malignancy was categorized as (a) high-grade, including acute myelogenous leukemia, acute lymphoblastic leukemia, and high-grade non-Hodgkin lymphoma, and (b) low-grade, including all other types of hematological malignancies and aplastic anemia. Disease status was categorized into active or stable disease. Leukopenia was defined as a total white blood cell count less than 1.0 × 109/l. Mechanical ventilation was defined as the need for noninvasive or invasive respiratory support. The use of vasopressor drugs was defined as any vasopressor (i.e., epinephrine, norepinephrine, dopamine, or vasopressin) or inotropic (i.e., dobutamine or milrinone) therapy administered within 24 h following admission. In our ICU the administration of vasopressor and/or inotropic drugs is restricted to patients with persistent hypotension despite adequate fluid resuscitation, inadequate cardiac output or cardiac failure (confirmed by pulmonary artery monitoring or echocardiography), and distinct signs of sepsis-induced organ dysfunction (i.e., oliguria, renal failure, neurological deterioration, and metabolic acidosis). The study was approved by the Ethics Committee of the Ghent University Hospital.
Statistical analysis
Values are presented as mean ± standard deviation, median (with interquartile range), or counts (with percentage) according to the distribution. For comparative tests the Mann–Whitney U test and Fisher's exact test or χ2 test was used as appropriate. Multivariate logistic regression was used to assess the independent impact of previous chemotherapy on 28-day mortality. Three logistic regression models were built; one including only factors present before ICU admission, a second containing factors present before and upon ICU admission, and a third additionally adjusted with propensity score to minimize the effect of potential selection bias [24, 25]. This propensity score reflected a patients' likelihood of having received recent intravenous chemotherapy. Variables associated with a p value of less than 0.25 in univariate analysis between CHT vs. nCHT patients were used to build the propensity score. The following variables were retained for propensity score: age, high-grade malignancy, active disease, diagnosis, remission state, and previous antimicrobial therapy. This propensity score was entered as a continuous variable into the models [24, 25]. Variables with a p value less than 0.25 in univariate analysis were considered for the multivariate analysis on 28-day mortality as well as clinically relevant variables. To reduce the risk of multicollinearity, only variables significantly associated with outcome in the first model were candidate for inclusion in the successive models. To assess the relationship between a continuous variable and outcome and subsequently to analyze whether a continuous variable needed to be transformed or categorized we used a smoothing scatterplot (LOESS) for each model. We tested for potential interactions. All reportedp values are two-tailed, and are considered significant when less than 0.05. Analyses were executed with SPSS 12.0 (SPSS, Chicago, IL, USA).
Results
There was no difference in mortality between documented and clinically suspected bacterial infection (36/80, 45% vs. 22/57, 39%, p = 0.49). In 19 patients (10.2%) the causal pathogen remained unclear. Twelve of them were treated with broad-spectrum antibiotics, in combination with a fungostatic in seven, high-dose cotrimoxazole in six, and acyclovir or ganglicovir in four. Five had a possible diagnosis of invasive fungal infection, two possible candidal pneumonia, and three possible invasive pulmonary aspergillosis (confirmed by autopsy in one). Two patients had possible Pneumocystis pneumonia or viruslike pneumonia. The causal pathogens in patients with documented bacterial infection are summarized in Table 2.
Differences in characteristics between CHT and nCHT patients
CHT patients were younger than nCHT patients(p < 0.001), were more often neutropenic (p < 0.001), had more often a high-grade malignancy (p < 0.001), had a longer duration of hospitalization prior to ICU admission (p = 0.012), and more often received antibiotics within 24 h before ICU admission (p = 0.027; Table 3). Broad-spectrum antibiotics with or without added fungostatics were more often administered in the CHT group (p < 0.001; Table 3). In addition, CHT patients less often had pulmonary infiltrates on chest radiography(p = 0.007), had a higher PaO2/FIO2 (p = 0.022), and were less often mechanically ventilated (p = 0.041) during ICU stay. However, no differences were found between CHT and nCHT groups in severity of illness upon admission as assessed by APACHE II (p = 0.094) or SOFA score(p = 0.231; Table 4).
Impact of recent chemotherapy on 28-days mortality after adjustment for potential confounders and propensity score
Crude ICU and 28-day mortality were lower in CHT patients than nCHT patients (33% vs. 48.4%, p = 0.037 and 40.7% vs. 57.4%, p = 0.027, respectively; Table 4). There was only a trend toward lower hospital mortality (45.1% vs. 58.9%, p = 0.076) between the groups; however, the observed hospital mortality rates were considerably lower than that expected by the CSSIS (77.2% vs.78.6%, p = 0.47). Twenty-eight day mortality rates in patients with severe sepsis and septic shock were 39.0% and 42.0% (p = 0.832) in CHT patients vs. 47.2% and 64.4% (p = 0.134) in nCHT patients, respectively. Twenty-eight day mortality in CHT vs. nCHT patients with invasive fungal infection was 77% and 75% (p = 0.335), and 31.5% and 52.6% (p = 0.02) in those with documented or suspected bacterial infection.
The results of the unadjusted and adjusted effects of recent chemotherapy on 28-day mortality are presented in Table 5. In multivariate logistic analysis with adjustment for variables present before ICU admission active disease (p = 0.026) and the initiation of combination antibiotic regimens before admission (p = 0.011) were independently associated with worse outcome, whereas recent intravenous chemotherapy had a protective effect (p = 0.007). Once adjusted for the site of infection and diagnosis of invasive fungal infection, the “protective effect” of chemotherapy became borderline significant (p = 0.049). In multivariate regression with adjustment for propensity score chemotherapy was no longer significantly associated with better outcome(p = 0.079).
Discussion
In our study patients with hematological malignancies who were referred to the ICU because of severe sepsis and septic shock with a history of recent chemotherapy faired better than commonly perceived. Recent chemotherapy was not associated with an increased risk of death after adjusting for differences in baseline characteristics and more particularly for the probability of having received chemotherapy by using a propensity score. This confirms previous results that cancer specific characteristics have no effect on short-term outcome in critically ill cancer patients [26, 27] provided that treatment options and expected long-term outcome are also considered. The presence of a pulmonary site of infection, fungal infection, and organ failure were the only factors associated with mortality in multivariate analysis.
In addition to catheter-related infections, chemotherapy-induced mucositis with subsequent bacterial translocation from the gut into the bloodstream is thought to be the major portal of entry in neutropenic patients [28], while pneumonia is less often diagnosed in this group at least by routine chest radiography [29]. Accordingly, in our study CHT patients were less often admitted with a pulmonary site of infection (49.5% vs. 69.5%, p = 0.007). It has previously been shown that the site of infection and/or portal of entry has a key impact on prognosis in a general ICU population [30, 31] as well as in cancer patients [30, 32]. In a general neutropenic cancer population Carratalàet al. [33] reported a mortality of 10.6% (39/368) in patients with bacteremia from a nonpulmonary focus vs. 55% (22/40) in those with bacteremia from a pulmonary focus, whereas Elting et al. [34] found that bacteremia was associated with a 3.8 odds of death when associated with pneumonia. In a general cancer population with Pseudomonas bacteremia Chatzinikolaou et al. [32] reported a mortality rate in patients without and with pneumonia of 8.1% (12/148) and 37.1% (36/63), respectively. In our study 28-day mortality in patients with a pulmonary site of infection was about 60%, regardless of recent chemotherapy (p = 0.99). This figure can be contrasted with the lower mortality in patients with other sources of sepsis, where prior chemotherapy did have a major impact: 28-day mortality was 21.7% when patients had received chemotherapy and 48.3% when they had not (p = 0.023; Table 2). This strongly suggests that sepsis resulting from (simple) bacterial translocation from the gut during chemotherapy-induced neutropenia is more readily contained by early appropriate antimicrobial therapy, as compared to pneumonia, or any other site of infection with the potential exception of catheter-related infection, in patients not treated with chemotherapy. This is probably related to a rapid achievement of source control in bacterial translocation as less local tissue inflammation or destruction is present [32].
In addition to the site of infection, the reversibility of the admission diagnosis and treatment options should also be taken into account. Mortality was about 75% in patients with invasive fungal and other nonbacterial infections regardless of previous chemotherapy vs. to 31.5% and 52.6% in patients with documented or suspected bacterial infection who did or did not receive chemotherapy, respectively. This is in accordance with our previous studies [5, 6, 8, 13, 16] and several other reports [4, 26, 35], and confirms the finding that nonbacterial infection remains much more difficult to treat than bacterial infection, particularly in critically ill patients [4, 8, 26]. However, with more antifungals with improved safety and efficacy becoming available, the care for nonbacterial infections may improve in the near future [36, 37].
Despite the fact that it is possible to achieve a meaningful survival in critically ill cancer patients, ICU physicians remain reluctant to admit such patients to their ICU for advanced life-supporting therapy [2, 3], particularly when severe infection is present. Our study confirms the finding that ICU physicians should not select patients that should benefit from advanced life-supporting therapy upon the number and severity of failing organs only [1, 2, 4, 5, 7, 8, 16]. The potential reversibility of the admission diagnosis [5, 6, 8], the expected long-term outcome and quality-of-life with regard to underlying malignancy, the patients' and family wishes, but also other factors such as comorbidity and performance status [7, 15], which were not considered in our multivariate analysis, should be taken into account as well. By a policy of timely ICU referral of hematological patients with severe sepsis and by providing advanced and prolonged supportive care to these patients we achieved survival rates that were equivalent to the general ICU patients admitted with severe infection [30], and that were considerably lower as expected by the CSSIS (Table 1). The latter finding might be explained by the fact that the CSISS is less accurate in predicting mortality in cancer patients than initially hoped for [38, 39]. Improvement in the overall management of such patients in the ICU, particularly in the management of severe sepsis and septic shock, might at least partially explain this discrepancy [22].
Our study has several potential limitations. First, we cannot exclude selection or treatment bias, even after adjusting for the probability of having received recent chemotherapy by using a propensity score. The latter score can, however, only correct for those variables taken into account. For instance, since we lacked a performance status and a comorbidity score, these parameters were not taken into account into our analysis. However, in our ICU patients were selected only upon their expected long-term outcome and not upon the severity of acute illness, the reason for deterioration, or whether they had recently received chemotherapy. Therefore, we do not think that selection bias was present in such extent to explain the absence of a worse outcome in patients who received prior chemotherapy. Moreover, it is also important to note that the two groups were similar in severity of illness upon admission according to several scoring systems, received similar vasopressor doses, and were well balanced regarding the incidence of active disease; also, there was no difference in the number of end-of-life decisions, nor in time until such a decision was made. Secondly, since we do not use computer tomography on a routine basis, we do not know whether chemotherapy-treated patients developed pulmonary infiltrates less often, or whether pulmonary infiltrates were manifested less obviously. Whether earlier and more accurately detection of pulmonary infiltrates by computed tomography affects outcome in critically ill hematological patients should be addressed in future studies [40, 41]. Finally, as our tertiary center has an experienced ICU staff trained in dealing and taking care of those patients working in good collaboration with the attending hematologists, our results may not be readily generalized.
In conclusion, the findings of this study demonstrate that patients with hematological malignancies admitted to the ICU with severe sepsis or septic shock after having received recent intravenous chemotherapy have a better prognosis than commonly perceived.
References
Brenner H (2002) Long-term survival rates of cancer patients achieved by the end of the 20th century: a period analysis. Lancet 360:1131–1135
Azoulay E, Afessa B (2006) The intensive care support of patients with malignancy: do everything that can be done. Intensive Care Med 32:3–5
Groeger JS, Bach PB (2003) Consider saying yes. Crit Care Med 31:320–321
Azoulay E, Thiery G, Chevret S, Moreau D, Darmon M, Bergeron A, Yang K, Meignin V, Ciroldi M, Le Gall JR, Tazi A, Schlemmer B (2004) The prognosis of acute respiratory failure in critically ill cancer patients. Medicine (Baltimore) 83:360–370
Benoit DD, Vandewoude KH, Decruyenaere JM, Hoste EA, Colardyn FA (2003) Outcome and early prognostic indicators in patients with a hematologic malignancy admitted to the intensive care unit for a life-threatening complication. Crit Care Med 31:104–112
Depuydt PO, Benoit DD, Vandewoude KH, Decruyenaere JM, Colardyn FA (2004) Outcome in noninvasively and invasively ventilated hematologic patients with acute respiratory failure. Chest 126:1299–1306
Soares M, Salluh JI, Spector N, Rocco JR (2005) Characteristics and outcomes of cancer patients requiring mechanical ventilatory support for > 24 hrs. Crit Care Med 33:520–526
Benoit DD, Depuydt PO, Peleman RA, Offner FC, Vandewoude KH, Vogelaers DP, Blot SI, Noens LA, Colardyn FA, Decruyenaere JM (2005) Documented and clinically suspected bacterial infection precipitating intensive care unit admission in patients with hematological malignancies: impact on outcome. Intensive Care Med 31:934–942
Hilbert G, Gruson D, Vargas F, Valentino R, Gbikpi-Benissan G, Dupon M, Reiffers J, Cardinaud JP (2001) Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N Engl J Med 344:481–487
Thiery G, Azoulay E, Darmon M, Ciroldi M, De Miranda S, Levy V, Fieux F, Moreau D, Le Gall JR, Schlemmer B (2005) Outcome of cancer patients considered for intensive care unit admission: a hospital-wide prospective study. J Clin Oncol 23:4406–4413
Azoulay E, Alberti C, Bornstain C, Leleu G, Moreau D, Recher C, Chevret S, Le Gall JR, Brochard L, Schlemmer B (2001) Improved survival in cancer patients requiring mechanical ventilatory support: impact of noninvasive mechanical ventilatory support. Crit Care Med 29:519–525
Lecuyer L, Chevret S, Thiery G, Darmon M, Schlemmer B, Azoulay E (2007) The ICU trial: a new admission policy for cancer patients requiring mechanical ventilation. Crit Care Med 35:808–814
Benoit DD, Hoste EA, Depuydt PO, Offner FC, Lameire NH, Vandewoude KH, Dhondt AW, Noens LA, Decruyenaere JM (2005) Outcome in critically ill medical patients treated with renal replacement therapy for acute renal failure: comparison between patients with and those without haematological malignancies. Nephrol Dial Transplant 20:552–558
Darmon M, Thiery G, Ciroldi M, de Miranda S, Galicier L, Raffoux E, Le Gall JR, Schlemmer B, Azoulay E (2005) Intensive care in patients with newly diagnosed malignancies and a need for cancer chemotherapy. Crit Care Med 33:2488–2493
Soares M, Salluh JI, Carvalho MS, Darmon M, Rocco JR, Spector N (2006) Prognosis of critically ill patients with cancer and acute renal dysfunction. J Clin Oncol 24:4003–4010
Benoit DD, Depuydt PO, Vandewoude KH, Offner FC, Boterberg T, De Cock CA, Noens LA, Janssens AM, Decruyenaere JM (2006) Outcome in severely ill patients with hematological malignancies who received intravenous chemotherapy in the intensive care unit. Intensive Care Med 32:93–99
Hughes WT, Armstrong D, Bodey GP, Bow EJ, Brown AE, Calandra T, Feld R, Pizzo PA, Rolston KV, Shenep JL, Young LS (2002) 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis 34:730–751
Larche J, Azoulay E, Fieux F, Mesnard L, Moreau D, Thiery G, Darmon M, Le Gall JR, Schlemmer B (2003) Improved survival of critically ill cancer patients with septic shock. Intensive Care Med 29:1688–1695
Regazzoni CJ, Irrazabal C, Luna CM, Poderoso JJ (2004) Cancer patients with septic shock: mortality predictors and neutropenia. Support Care Cancer 12:833–839
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, Gea-Banacloche J, Keh D, Marshall JC, Parker MM, Ramsay G, Zimmerman JL, Vincent JL, Levy MM (2004) Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Intensive Care Med 30:536–555
Groeger JS, Lemeshow S, Price K, Nierman DM, White P Jr, Klar J, Granovsky S, Horak D, Kish SK (1998) Multicenter outcome study of cancer patients admitted to the intensive care unit: a probability of mortality model. J Clin Oncol 16:761–770
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31:1250–1256
Ascioglu S, Rex JH, de Pauw B, Bennett JE, Bille J, Crokaert F, Denning DW, Donnelly JP, Edwards JE, Erjavec Z, Fiere D, Lortholary O, Maertens J, Meis JF, Patterson TF, Ritter J, Selleslag D, Shah PM, Stevens DA, Walsh TJ (2002) Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin Infect Dis 34:7–14
Marshall JM, Rosenbaum PR (1999) Propensity scores. Am J Epidemiol 150:327–333
Rosenbaum PR, Rubin DB (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 70:41–55
Massion PB, Dive AM, Doyen C, Bulpa P, Jamart J, Bosly A, Installe E (2002) Prognosis of hematologic malignancies does not predict intensive care unit mortality. Crit Care Med 30:2260–2270
Sculier JP, Paesmans M, Markiewicz E, Berghmans T (2000) Scoring systems in cancer patients admitted for an acute complication in a medical intensive care unit. Crit Care Med 28:2786–2792
Tsuji E, Hiki N, Nomura S, Fukushima R, Kojima J, Ogawa T, Mafune K, Mimura Y, Kaminishi M (2003) Simultaneous onset of acute inflammatory response, sepsis-like symptoms and intestinal mucosal injury after cancer chemotherapy. Int J Cancer 107:303–308
Azoulay E, Darmon M, Delclaux C, Fieux F, Bornstain C, Moreau D, Attalah H, Le Gall JR, Schlemmer B (2002) Deterioration of previous acute lung injury during neutropenia recovery. Crit Care Med 30:781–786
Alberti C, Brun-Buisson C, Burchardi H, Martin C, Goodman S, Artigas A, Sicignano A, Palazzo M, Moreno R, Boulme R, Lepage E, Le Gall R (2002) Epidemiology of sepsis and infection in ICU patients from an international multicentre cohort study. Intensive Care Med 28:108–121
Vandijck DM, Decruyenaere JM, Blot SI (2006) The value of sepsis definitions in daily ICU-practice. Acta Clin Belg 61:220–226
Chatzinikolaou I, Abi-Said D, Bodey GP, Rolston KV, Tarrand JJ, Samonis G (2000) Recent experience with Pseudomonas aeruginosa bacteremia in patients with cancer: retrospective analysis of 245 episodes. Arch Intern Med 160:501–509
Carratala J, Roson B, Fernandez-Sevilla A, Alcaide F, Gudiol F (1998) Bacteremic pneumonia in neutropenic patients with cancer: causes, empirical antibiotic therapy, and outcome. Arch Intern Med 158:868–872
Elting LS, Rubenstein EB, Rolston KV, Bodey GP (1997) Outcomes of bacteremia in patients with cancer and neutropenia: observations from two decades of epidemiological and clinical trials. Clin Infect Dis 25:247–259
Gruson D, Vargas F, Hilbert G, Bui N, Maillot T, Mayet T, Pillet O, Chene G, Gbikpi-Benissan G (2004) Predictive factors of intensive care unit admission in patients with haematological malignancies and pneumonia. Intensive Care Med 30:965–971
Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, Kern WV, Marr KA, Ribaud P, Lortholary O, Sylvester R, Rubin RH, Wingard JR, Stark P, Durand C, Caillot D, Thiel E, Chandrasekar PH, Hodges MR, Schlamm HT, Troke PF, de Pauw B (2002) Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med 347:408–415
Rubin MA, Carroll KC, Cahill BC (2002) Caspofungin in combination with itraconazole for the treatment of invasive aspergillosis in humans. Clin Infect Dis 34:1160–1161
Soares M, Fontes F, Dantas J, Gadelha D, Cariello P, Nardes F, Amorim C, Toscano L, Rocco JR (2004) Performance of six severity-of-illness scores in cancer patients requiring admission to the intensive care unit: a prospective observational study. Crit Care 8:R194–R203
Benoit DD, Vandijck DM, Depuydt PO, Offner FC, Roosens CD, Noens LA, Decruyenaere JM (2006) Outcome in septic shock patients with hematological malignancies: impact of previous chemotherapy. Intensive Care Med 32 [Suppl 1]:S341, 91
Horger M, Hebart H, Einsele H, Lengerke C, Claussen CD, Vonthein R, Pfannenberg C (2005) Initial CT manifestations of invasive pulmonary aspergillosis in 45 non-HIV immunocompromised patients: association with patient outcome? Eur J Radiol 55:437–444
Heussel CP, Kauczor HU, Heussel G, Fischer B, Mildenberger P, Thelen M (1997) Early detection of pneumonia in febrile neutropenic patients: use of thin-section CT. AJR Am J Roentgenol 169:1347–1353
Acknowledgements
D.V. is financially supported by a Doctoral Grant from the Special Scientific Research Fund of the Ghent University. None of the authors have financial or other potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-008-1003-1.
Rights and permissions
About this article
Cite this article
Vandijck, D.M., Benoit, D.D., Depuydt, P.O. et al. Impact of recent intravenous chemotherapy on outcome in severe sepsis and septic shock patients with hematological malignancies. Intensive Care Med 34, 847–855 (2008). https://doi.org/10.1007/s00134-008-1002-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1002-2