Abstract
Outcomes of patients with hematologic malignancies requiring ICU care for critical illness are suboptimal and represent a major unmet need in this population. We present data from a dedicated haematology oncology setting including 63 patients with a median age of 60 years admitted to the ICU for critical illness with organ dysfunction. The most common underlying diagnosis was multiple myeloma (30%) followed by acute myeloid leukemia (25%). Chemotherapy had been initiated for 90.7% patients before ICU admission. The most common indication for ICU care was respiratory failure (36.5%) and shock (17.5%) patients. Evidence of sepsis was present in 44 (69%) patients. After shifting to ICU, 32 (50%) patients required inotropic support and 18 (28%) required invasive mechanical ventilation. After a median of 5 days of ICU stay, 43.1% patients had died, most commonly due to multiorgan dysfunction. Risk of mortality was higher with involvement of more than two major organs (p = .001), underlying AML (p = .001), need for mechanical ventilation (p = .001) and high inotrope usage (p = .004). Neutropenia was not associated with mortality. Our study indicates high rates of short term mortality and defines prognostic factors which can be used to prognosticate patients and establish goals of care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
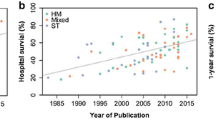
Patients with haematologic malignancies (HMs) requiring admission to intensive care units (ICUs) continue to have suboptimal outcomes, with only modest improvement in survival over the past few decades [1]. Data from the 1990s indicated short term ICU mortality in excess of 75%, which still ranges from 40–50% in current datasets [2]. Recent data from the United States indicates a mortality of 73% for patients with HMs admitted with septic shock, in contrast to approximately 40% for similar patients without cancer [3, 4]. Patients with HMs are at particularly higher risk of death owing to disease and treatment related immunosuppression, translating into a higher risk of invasive fungal infections and bleeding complications [5, 6]. Indeed, patients with HMs exhibit higher mortality compared to patients with solid organ cancers admitted with critical illness [7]. As a result, the utility of ICU admission for critically ill patients with HMs or neutropenia was frequently questioned and discouraged [8].
Survival after ICU admission is inversely correlated with worsening hemodynamic or ventilatory function and is reflected in measures of critical illness severity, including APACHE (Acute Physiology and Chronic Health Evaluation) and SOFA (Sequential Organ Failure Assessment) scores [1, 9, 10]. Unlike previous data, neutropenia is no longer an adverse prognostic factor for survival, indicating an unmet need to identify other factors for selecting patients likely to benefit from ICU admission for critical illness [3]. This has prompted the exploration of newer concepts, such as improved triaging and time limited trials for ICU admission, with an aim to identify patients likely to benefit from ICU admission in this setting.
Patients with haematologic malignancies requiring ICU admissions represent an expanding population. Based on older data, approximately 7% of all patients with haematologic cancers on treatment require critical care [11]. In a large dataset with 86,000 ICU admissions published in 2022, approximately 20% of patients admitted with sepsis had underlying HM [3]. This number is expected to increase over the next few years, as a greater number of patients previously deemed unfit for therapy now receive treatment with curative intent, placing further emphasis on streamlining ICU protocols and identifying suitable candidates for admission to ICU [12,13,14].
This challenge is magnified in resource limited settings such as India, where patients exhibit greater physiological frailty and treatment related complications compared to similarly aged patients in the West [14]. Patients admitted to ICUs in India also display higher rates of infections with gram negative bacilli (GNB) and multidrug resistant (MDR) organisms, translating into higher rates of short term mortality [15, 16]. For context, more than 40% of induction deaths in patients with acute myeloid leukemia in India are attributable to MDR organisms [17].
Given the paucity of published data in the Indian setting, this study was conducted to assess patients with haematologic malignancies (HMs) admitted to intensive care units (ICUs) for critical illness, aiming to determine short-term mortality rates and identify prognostic factors influencing survival. This study included a distinct population of patients with haematologic malignancies alone, and will hopefully enable future research aimed at improving survival in this patient subset.
Methods
Study Design and Setting
This was conducted as a retrospective observational study in the departments of Haematology-Oncology, Medical Oncology and Critical Care in a private unaided tertiary care institution in North India and included patients from May 1, 2019 to May 1, 2022. Patients with acute leukemia, chronic leukemia, multiple myeloma and all subtypes of lymphoma requiring admission to the intensive care unit for critical illness were included in the analysis. All patients were under treatment with the departments of Hematology/Medical Oncology at the time of shifting to ICU. Institutional ethics committee approval was received before starting the study.
Criteria for Critical Care Admission and Inclusion
Medical records of patients admitted to ICU during the study period were retrieved and evaluated. To ensure that a representative population was included, criteria for organ dysfunction were pre-specified, based on criteria included in the International Consensus definition for Sepsis and Septic Shock [18]. Patients admitted for pre-emptive monitoring and other indications were excluded from the study. Inclusion criteria to define critical illness were:
-
a.
Hypotension: Systolic BP < 90 mmHg
-
b.
Respiratory Failure: SpO2 < 90% or requiring more than 10 L/min of O2 support in the ward, or arterial blood gas (ABG) indicating pO2 < 60 mmHg or pCO2 > 45 mmHg
-
c.
Acute Kidney Injury (AKI): As there is no standard definition of sepsis related AKI (SA-AKI), the presence of AKI according to KDIGO (Kidney Disease Improving Global Outcomes) guidelines along with the presence of Sepsis-3 criteria was used as a pragmatic definition, as described in several guidelines [19, 20]. Thus, an increase in serum creatinine by 0.3 mg/dl, a rise by 1.5 times of baseline, or urine output of < 0.5 ml/kg/hour for more than 6 h was used to define SA-AKI.
-
d.
Altered sensorium: Glasgow Coma Score of < 8/15
-
e.
Major Bleeding: Defined as bleeding associated with a fall in Hemoglobin by ≥ 2 g/dl or requiring blood transfusion support, according to the ISTH (International Society on Thrombosis and Hemostasis) guidelines [21].
-
f.
Cardiac or respiratory arrest
-
g.
Tachyarrhythmia: HR more than 150/min but not sinus tachycardia, or Bradyarrhythmia: HR Less than 60/min requiring cardioversion.
Patients who fulfilled the above criteria and were aged more than 18 years of age at the time of admission were included in the analysis. No other exclusion criteria were specified.
Treatment in ICU
The institutional ICUs follow a semi-closed design, with both the primary team and intensive care team sharing responsibility for the patient. Decisions on ventilatory and hemodynamic support, vascular access or invasive monitoring were primarily made by the intensive care team. Any major decisions involving the addition of further life support or changing the intent of ICU admission (e.g., not to intubate) were made after discussion with the primary team and the patient’s family. To lend context, the approximate cost of ICU care in this center is approximately ₹ 10,000 per day, which can go up to ₹ 25,000/day in case of mechanical ventilation or dialysis support. Neutropenia was defined as an absolute neutrophil count (ANC) of less than 1500/mm3, and institutional protocols based on standard guidelines were followed for the treatment of febrile neutropenia and fungal infections [22].
Briefly, for any patient with a temperature of more than 100.4 F, blood cultures were collected, and intravenous Cefoperazone/Sulbactam and Amikacin were initiated. For patients who were hemodynamically unstable or had previous history of infections with ESBL producing (Extended Spectrum Beta Lactamase) organisms, antibiotics were escalated to Meropenem. A clinical examination was performed to rule out any localizing features of infection and antibiotics were continued for at least 48–72 h before reviewing cultures and modifying the same. For persistent neutropenic fever beyond 72 h, a high resolution CT scan (HRCT) chest was obtained to rule out invasive fungal infection. Antibiotic therapy was modified after mutual discussion between the hematology and critical care teams.
Fungal pneumonia was classified as possible, probable, or proven based on guidelines from the mycoses study group of the EORTC [23]. Administration of inotropic support was determined by the intensive care team, and choice of specific agents was made in accordance with established protocols. Vasoactive inotropic score (VIS) was calculated as previously described [24].
Statistical Analysis
Baseline data and demographics for all patients were obtained from medical records. Chronic co-morbidities, including diabetes mellitus, systemic hypertension, chronic kidney disease, connective tissue disease and coronary artery disease were specifically recorded. Data were described in terms of range; mean ± standard deviation (± SD), median, frequencies (number of cases) and relative frequencies (percentages) as appropriate. To determine whether the data were normally distributed, a Kolmogorov–Smirnov test was used. Comparison of quantitative variables between the study groups was done using Mann Whitney U test for independent samples for non-parametric data. Receiver operator characteristics (ROC) curve was done, and criterion value was estimated depending on the specificity and sensitivity. Area under curve (AUC) was measured. Kaplan–Meier curves for survival were plotted among different variables. For comparing categorical data, Chi square (χ2) test was performed, and Fisher exact test was used when the expected frequency is less than 5. A probability value (p value)less than 0.05 was considered statistically significant. All statistical calculations were done using (Statistical Package for the Social Science)SPSS 21version (SPSS Inc., Chicago, IL, USA)statistical program for Microsoft Windows.
Results
Baseline Data and Setting of ICU shift
A total of 63 patients (M:F = 40:23) with a median age of 60 years (IQR, 40–69) were included in the analysis. The most common underlying diagnosis was multiple myeloma (n = 19, 30%), followed by AML (n = 16, 25%) and chronic lymphocytic leukemia (n = 8, 12.7%). A majority of patients had newly diagnosed disease (n = 49, 77.8%) and treatment for underlying malignancy was initiated for 57 (90.4%) patients before shifting to ICU. The median number of chronic co-morbidities was 1 (IQR, 0–2) with twenty two patients (34.9%) having no prior comorbidities. Baseline echocardiography was available for 34 (54%) patients, and 19 (30%) had LV systolic dysfunction with a median LVEF of 40% (IQR, 30–44). Table 1 shows baseline characteristics of study participants at the time of admission to the ICU and, with frequency of underlying diagnosis displayed in Supplementary Figure 1.
The median neutrophil count at the time of shifting to ICU was 3072/mm3 (IQR, 882–7968) and median creatinine was 1.1 mg/dl (IQR, 0.8 to 2.0). Neutropenia was present in 38.1% (n = 24) patients at the time of admission. In the neutropenic group, the median ANC was 24 cells/mm3 (IQR 0–307), compared to 4620 cells/mm3 (IQR 2898–9240) in the non-neutropenic group. On comparing neutropenic and non-neutropenic patients, the former had a younger median age (46 vs 64 years, p = 0.007) and a greater degree of thrombocytopenia (22,000 vs 96,000/mm3, p = 0.000). Salient differences between the two groups are highlighted in Supplementary Table 1.
The commonest primary indication for shifting to ICU was respiratory failure, present in 23 (36.5%) patients followed by hypotension in 11 (17.5%), acute cardiac event in 9 (14.3%) and altered sensorium in 7 (11.1%) patients. Forty four patients (69.8%) had clinical, radiological, or microbiological evidence of infection at the time of admission, with the most common localization being the lower respiratory tract (n = 23, 52.2%), followed by no specific localization (n = 13, 29.5%). Figure 1a and b show a distribution of primary indication for ICU admission and localization of infection, respectively.
Supportive Care in ICU
A majority of patients had two major organ dysfunction (n = 20, 31.7%), followed by single organ in 16 (25.4%) and three in 15 (23.8%) patients. Out of 102 occurrences of organ dysfunction across the cohort, cardiovascular (CVS) involvement was observed in 37 instances, renal in 29, respiratory in 25, and central nervous system (CNS) involvement in 11 instances. Thirty two patients (50.8%) presented with shock necessitating inotropic support, with a median requirement for 2 inotropic drugs (IQR, 1–3).The median vasoactive score (VIS) was 24 (IQR, 7.3 to 51.5). Respiratory support was required for 43 (68.2%) patients, with a majority of patients requiring non-invasive ventilation with face mask or nasal devices (n = 22, 34.9%) and 3 (4.8%) requiring positive pressure support. Invasive ventilation was required for 18 (28.6%) patients, for a median duration of 2 days (range, 1–9 days). Hemodialysis was performed for nine (14.2%) patients, with five patients receiving continuous renal replacement therapy (CRRT) and four conventional hemodialysis. Dialysis was performed for a median of four days (IQR, 2 to 8.5).
Microbiologic Findings
Of all patients admitted with a diagnosis of sepsis (n = 44, 69.8%), a confirmed microbiologic diagnosis was obtained in 11 patients (25%), with the commonest isolate being GNB in 8 (72%), followed by Gram Positive Cocci, Candida auris and Clostridium Difficile in one patient each. The site of isolation included blood culture in 8 patients, respiratory secretions in 3 and urine in one (one patient had GNB in both blood and sputum). Five of the gram negative bacilli isolated (62%) were carbapenem resistant. None of the patients had proven fungal pneumonia due to lack of biopsy or bronchoscopy during admission. Positive fungal biomarkers were observed in 16 (26%) patients, including galactomannan in 5 (7.9%) and beta glucan in 6 (9.5%) patients. A final diagnosis of possible fungal pneumonia was made in 12 (19%) and probable fungal pneumonia in 11 (17.4%) patients.
Outcome of ICU Stay
The overall intent of admission included full support including dialysis and mechanical ventilation for a majority (n = 54, 85%) of patients. Families of six patients (9.5%) opted against intubation, while three patients (4.8%) requested to exclude hemodialysis. The median duration of stay in the ICU was 5 days (IQR, 2 to 8 days). At the end of the ICU stay, 36 (57.1%) patients were shifted out of ICU with clinical improvement. Twenty patents (31.7%) died during the course of ICU stay, and treatment was discontinued by seven patients (11.1%). The latter group was presumed dead for analysis. Cause of death in all patients was progressive multi-organ dysfunction. Median survival in ICU from the date of ICU admission to the last day in ICU was estimated to be 15 days (IQR 8.7 to 21.2). Figure 2 displays Kaplan Meier survival curve for the entire cohort in the ICU.
Statistical Analysis and Predictors of Mortality
Survival was significantly lower for patients with AML (Median, 2 vs. 18 days) compared to those with all other diagnoses (X2 19.4, p = 0.001) and is depicted in Fig. 3a. No difference in survival was observed among neutropenic and non-neutropenic patients, (median, 15 vs 18 days, p = 0.131), as observed in Fig. 3b. Beyond two or more major organ involvement, a significant increase in risk of mortality was observed (X2 = 25.3, p = 0.001), and is depicted in Fig. 3c. A higher risk of mortality was also observed in patients where the primary indication for admission was respiratory failure (X2 = 15.154, p = 0.034) and those who required mechanical ventilation (X2 = 23.79, p = 0.001). A similar effect was noted in patients who had a documented respiratory infection (X2 = 19.47, p = 0.007).
An association between risk of mortality and increasing vasoactive scores (p = 0.004) was also observed. Receiver Operating Characteristic (ROC) curve analysis yielded an Area Under the Curve (AUC) of 0.816 (95% CI, 0.644–0.988, p = 0.004) when utilizing a VIS threshold of 12 to predict excess mortality (Fig. 4).
A comparative analysis to identify baseline differences among survivors and non-survivors revealed significant differences in three parameters, namely, mean baseline platelet count (93,000/mm3 vs 22,000/mm3, Z = -3, p = 0.003), lowest pH on arterial blood gas analysis (7.44 vs 7.06, Z = -2.0, p = 0.043) and mean VIS (13.5 vs 35.3, Z = -2.9, p = 0.004). There was no significant difference between the two groups based on age, baseline counts, ANC, and number of co-morbidities.
Discussion
Our cohort of patients with haematologic malignancies, including 50% admitted with shock and 30% requiring mechanical ventilation offers a broad representation of various aspects of ICU care in this distinct population. Primary findings include an ICU related mortality of 43%, which correlated significantly with an underlying diagnosis of AML and respiratory failure at the time of shifting to ICU. The lack of association between ICU survival and neutropenia or chronic co-morbidities is reassuring, suggesting the possibility of identifying patients who may benefit from ICU admission despite being unfit.
Our finding of ICU-related mortality of 43% is in keeping with rates of 30–50% noted in contemporary studies [25,26,27]. One of the few studies from India evaluating this patient population reported a similar mortality of 48% [28]. It is noteworthy that short term mortality in high income settings also falls in the same range, indicating significant effort required to improve outcomes in this patient subset. As the commonest indication for ICU care in this population is hemodynamic or respiratory support, early identification of clinical deterioration is vital and positively impacts outcomes after ICU admission [29,30,31].
Several early warning systems can be useful in this regard. The modified early warning score (MEWS) serves as a prototype early warning system, incorporating multiple physiological factors which can be assessed easily at the bedside and enables prediction of requirement for ICU care in patients with haematologic malignancies [32]. The predictive value of MEWS can be further enhanced by changing the cutoff score to six [32], or adding serum lactate [33], or the SpO2/FiO2 ratio to baseline assessment [34]. Two other scoring systems including the serially measured Systemic Inflammatory Response Syndrome (SIRS) score [35, 36] and the qSOFA score (RR > 22/min, SBP < 100 mmHg and altered mental status) [37] are easily assessable and have meaningful predictive capabilities.
Septic shock has been consistently identified as a negative prognostic factor in various studies in haematology/oncology patients in the ICU [38,39,40]. Higher inotrope requirements are reflected in the VIS, which provides a standardized representation of the extent of inotrope usage. We observed that a cutoff of 12 provides a sensitivity and specificity of 81% for predicting a higher risk of mortality, which can provide a signpost for informed discussion about the likelihood of poor outcomes.
We observed a mortality rate of 88% in patients requiring invasive mechanical ventilation (IMV). This subset experiences high mortality in published data, ranging from 65 to 75% in several studies [10, 26]. These poor outcomes had prompted alternate strategies in the past, such as utilizing NIV in the ward to avoid potential intubation. However, trials of NIV in the ward are associated with high rates of failure (45 to 60%) and a subsequent higher mortality in those who fail NIV [28, 41, 42]. Although this was challenged by a recent meta-analysis, the question is still unresolved due to suboptimal quality of the included studies, and is not recommended by current guidelines [43, 44]. Consideration of patient frailty and the reversibility of underlying respiratory failure and haematologic malignancy should be a priority before deciding on intubation and ventilation in this context [45].
A microbiologic etiology was documented in 25% of patients with sepsis, broadly in keeping with culture positivity rates of 20–30% noted in most studies [46]. Concerningly, five out of eight isolated GNBs were carbapenem resistant, which are often observed at rates of 40–60% at tertiary centres in India [47,48,49,50].
In resource limited settings, the process of ICU care must necessarily involve financial discussions, as costs of ICU care are significant and often borne out of pocket [51]. This process goes beyond the initial ICU admission and is necessary to avoid imposing unnecessary financial burden when patients are not likely to improve. Therefore, even after admission to ICU, reappraisal of goals and extent of ICU care is paramount and can be assisted by several prognostic factors identified in this study. Involvement of more than two major organs, high inotropic requirement (indicated by a VIS of ≥ 12) and underlying AML warrants a more critical reassessment and lowering the threshold for changing goals of ICU care.
Neutropenia alone should not be considered a negative prognostic factor in this patient subgroup [44]. A recent study from India demonstrated a higher risk of mortality for neutropenic patients, likely due to a higher representation of acute leukemia and use of IMV in over 60% of patients [28]. We did not observe a similar association, indicating that decisions to change goals of care in ICU should depend on measures of organ severity and not neutropenia alone.
There are several nuances to considering AML as a negative prognostic factor. In India, baseline mortality with AML is significantly higher owing to fungal and gram negative infections, and high rates of treatment discontinuation are noted due to financial reasons [17]. In addition, the effect of age on mortality even without critical illness becomes apparent beyond 50–55 years of age [52]. These differences and the additional cost of ICU care become even more significant, emphasizing their crucial role in the discussing goals of ICU care.
Our study has two limitations which may restrict universal application of these results. First, a higher proportion of patients with myeloma compared to AML is an unexpected finding, and may be a result of patient demographics, regional epidemiology, and referral patterns. We have recently demonstrated financial and social factors leading to significant non initiation of therapy in Indian patients with AML, which may have a greater impact in those requiring ICU care [52]. Secondly, our data from a private academic institution may not be universally applicable. Both these limitations can be potentially overcome by accruing data from several Indian institutions from public and private backgrounds with varying funding.
Conclusions
Our study demonstrates a high rate of short term mortality in patients with haematologic malignancies requiring critical care, and identifies the presence of AML, requirement of mechanical ventilatory support, and high inotropic requirement as negative prognostic factors. Early identification of suitable candidates and daily re-evaluation of prognostic factors can enable improved communication with families can allow well-informed decisions regarding goals of care.
References
Taccone FS, Artigas AA, Sprung CL, Moreno R, Sakr Y, Vincent J-L (2009) Characteristics and outcomes of cancer patients in European ICUs. Crit Care 13(1):R15
Lloyd-Thomas AR, Wright I, Lister TA, Hinds CJ (1988) Prognosis of patients receiving intensive care for lifethreatening medical complications of haematological malignancy. Br Med J (Clin Res Ed) 296(6628):1025–1029
Manjappachar NK, Cuenca JA, Ramírez CM, Hernandez M, Martin P, Reyes MP et al (2022) Outcomes and predictors of 28-day mortality in patients with hematologic malignancies and septic shock defined by sepsis-3 criteria. J Natl Compr Canc Netw 20(1):45–53
Buchman TG, Simpson SQ, Sciarretta KL, Finne KP, Sowers N, Collier M et al (2020) Sepsis among medicare beneficiaries: 1. The burdens of sepsis, 2012-2018. Crit Care Med 48(3):276–88
Hawari FI, Nazer LH, Addassi A, Rimawi D, Jamal K (2016) Predictors of ICU admission in patients with cancer and the related characteristics and outcomes: a 5-year registry-based study. Crit Care Med 44(3):548–553
Kubihal V, Chandrashekhara SH, Triveni GS (2022) Clinical imaging in oncological ICU. In: Kumar V, Gupta N, Mishra S (eds) Onco-critical care: an evidence-based approach. Springer Nature Singapore, Singapore, pp 37–50
Williams MD, Braun LA, Cooper LM, Johnston J, Weiss RV, Qualy RL et al (2004) Hospitalized cancer patients with severe sepsis: analysis of incidence, mortality, and associated costs of care. Crit Care (London, England) 8(5):R291–R298
Brunet F, Lanore JJ, Dhainaut JF, Dreyfus F, Vaxelaire JF, Nouira S et al (1990) Is intensive care justified for patients with haematological malignancies? Intensive Care Med 16(5):291–297
Evison J, Ritz R, Elsasser S (2001) Intensive care unit admission in patients with hematological disease: incidence, outcome and prognostic factors. Swiss Med Wkly 131(4748):681–686
Owczuk R, Wujtewicz MA, Sawicka W, Wadrzyk A, Wujtewicz M (2005) Patients with haematological malignancies requiring invasive mechanical ventilation: differences between survivors and non-survivors in intensive care unit. Support Care Cancer: Off J Multinatl Assoc Support Care Cancer 13(5):332–338
Gordon AC, Oakervee HE, Kaya B, Thomas JM, Barnett MJ, Rohatiner AZ et al (2005) Incidence and outcome of critical illness amongst hospitalised patients with haematological malignancy: a prospective observational study of ward and intensive care unit based care. Anaesthesia 60(4):340–347
Senapati J, Dhawan R, Aggarwal M, Kumar P, Kumar Vishwanathan G, Dass J et al (2021) Venetoclax and azacitidine (VenAZA) combination therapy in young unfit patients with AML: a perspective from a developing country. Leuk Lymphoma 62(6):1514–1517
Jobanputra KN, Nayak L, Jain H, Sengar DM (2021) Diffuse large B-cell lymphoma in the elderly: retrospective analysis from a single tertiary cancer center in India. Blood 138:2515
Shaikh MRMA, Mehta P, Mirgh SP, Halder R, Agrawal N, Khushoo V et al (2021) Individualized AML induction with venetoclax based therapy in unfit treatment naïve patients aged ≤ 60 years: a real world perspective from India. Blood 138:4417
Hammond NE, Kumar A, Kaur P, Tirupakuzhi Vijayaraghavan BK, Ghosh A, Grattan S et al (2022) Estimates of sepsis prevalence and outcomes in adult patients in the ICU in India: a cross-sectional study. Chest 161(6):1543–1554
Chaudhry D, Prajapat B (2017) Intensive care unit bugs in India: How do they differ from the western world? J Assoc Chest Phys 5(1):10–17
Philip C, George B, Ganapule A, Korula A, Jain P, Alex AA et al (2015) Acute myeloid leukaemia: challenges and real world data from India. Br J Haematol 170(1):110–117
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M et al (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8):801–810
Peerapornratana S, Manrique-Caballero CL, Gómez H, Kellum JA (2019) Acute kidney injury from sepsis: current concepts, epidemiology, pathophysiology, prevention and treatment. Kidney Int 96(5):1083–1099
Cheung AK, Chang TI, Cushman WC, Furth SL, Hou FF, Ix JH et al (2021) KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int 99(3):S1–S87
Franco L, Becattini C, Beyer-Westendorf J, Vanni S, Nitti C, Re R et al (2020) Definition of major bleeding: prognostic classification. J Thromb Haemost 18(11):2852–2860
Zimmer AJ, Freifeld AG (2019) Optimal management of neutropenic fever in patients with cancer. J Oncol Pract 15(1):19–24
Donnelly JP, Chen SC, Kauffman CA, Steinbach WJ, Baddley JW, Verweij PE et al (2019) Revision and update of the consensus definitions of invasive fungal disease from the European organization for research and treatment of cancer and the mycoses study group education and research consortium. Clin Infect Dis 71(6):1367–1376
Belletti A, Lerose CC, Zangrillo A, Landoni G (2021) Vasoactive-inotropic score: evolution, clinical utility, and pitfalls. J Cardiothorac Vasc Anesth 35(10):3067–3077
Ferreyro BL, Scales DC, Wunsch H, Cheung MC, Gupta V, Saskin R et al (2021) Critical illness in patients with hematologic malignancy: a population-based cohort study. Intensive Care Med 47(10):1104–1114
de Vries VA, Müller MCA, Arbous MS, Biemond BJ, Blijlevens NMA, Kusadasi N et al (2019) Long-term outcome of patients with a hematologic malignancy and multiple organ failure admitted at the intensive care. Crit Care Med 47(2):e120–e128
Tridente A, Dempsey NC, Khalifa M, Goddard J, Shuker K, Hall J et al (2023) Predicting outcomes of hematological malignancy patients admitted to critical care. Front Hematol 2. https://doi.org/10.3389/frhem.2023.1127322
Siddiqui SS, Prabu NR, Chaudhari HK, Narkhede AM, Sarode SV, Dhundi U et al (2021) Epidemiology, clinical characteristics, and prognostic factors in critically ill patients with hematolymphoid malignancy. Indian J Crit Care Med: Peer-reviewed, Off Publ Indian Soc Crit Care Med 25(1):56–61
Moreno-Sanchez F, Gomez-Gomez B (2022) Antibiotic management of patients with hematologic malignancies: from prophylaxis to unusual infections. Curr Oncol Rep 24(7):835–842
Azoulay E, Recher C, Alberti C, Soufir L, Leleu G, Le Gall JR et al (1999) Changing use of intensive care for hematological patients: the example of multiple myeloma. Intensive Care Med 25(12):1395–1401
Hampshire PA, Welch CA, McCrossan LA, Francis K, Harrison DA (2009) Admission factors associated with hospital mortality in patients with haematological malignancy admitted to UK adult, general critical care units: a secondary analysis of the ICNARC case mix programme database. Crit Care (London, England) 13(4):R137
van Mourik N, Oomen JJ, van Vught LA, Biemond BJ, van den Bergh WM, Blijlevens NM et al (2023) The predictive value of the modified early warning score for admission to the intensive care unit in patients with a hematologic malignancy–a multicenter observational study. Intensive Crit Care Nurs 79:103486
Yoo J-W, Lee JR, Jung YK, Choi SH, Son JS, Kang BJ et al (2015) A combination of early warning score and lactate to predict intensive care unit transfer of inpatients with severe sepsis/septic shock. Korean J Intern Med 30(4):471
Lee JR, Jung YK, Kim HJ, Koh Y, Lim CM, Hong SB et al (2020) Derivation and validation of modified early warning score plus SpO2/FiO2 score for predicting acute deterioration of patients with hematological malignancies. Korean J Intern Med 35(6):1477–1488
Mato A, Fuchs BD, Heitjan DF, Mick R, Halpern SD, Shah PD et al (2009) Utility of the systemic inflammatory response syndrome (SIRS) criteria in predicting the onset of septic shock in hospitalized patients with hematologic malignancies. Cancer Biol Ther 8(12):1095–1100
Mato AR, Luger SM, Heitjan DF, Mikkelson ME, Olson E, Ujjani C et al (2010) Elevation in serum lactate at the time of Febrile Neutropenia (FN) in hemodynamically-stable patients with Hematologic Malignancies (HM) is associated with the development of septic shock within 48 hours. Cancer Biol Ther 9(8):585–589
Nathan N, Sculier JP, Ameye L, Paesmans M, Bogdan-Dragos G, Meert AP (2021) Sepsis and septic shock definitions in patients with cancer admitted in ICU. J Intensive Care Med 36(3):255–261
Yeo CD, Kim JW, Kim SC, Kim YK, Kim KH, Kim HJ et al (2012) Prognostic factors in critically ill patients with hematologic malignancies admitted to the intensive care unit. J Crit Care 27(6):739.e1-739.e6
Cetintepe T, Cetintepe L, Solmaz S, Calık S, Ugur MC, Gediz F et al (2021) Determination of the relationship between mortality and SOFA, qSOFA, MASCC scores in febrile neutropenic patients monitored in the intensive care unit. Support Care Cancer 29(7):4089–4094
Al-Zubaidi N, Shehada E, Alshabani K, ZazaDitYafawi J, Kingah P, Soubani AO (2018) Predictors of outcome in patients with hematologic malignancies admitted to the intensive care unit. Hematol Oncol Stem Cell Ther 11(4):206–218
Wang T, Zhang L, Luo K, He J, Ma Y, Li Z et al (2016) Noninvasive versus invasive mechanical ventilation for immunocompromised patients with acute respiratory failure: a systematic review and meta-analysis. BMC Pulm Med 16(1):129
Liu J, Bell C, Campbell V, DeBacker J, Tamberg E, Lee C et al (2019) Noninvasive ventilation in patients with hematologic malignancy: a retrospective study. J Intensive Care Med 34(3):197–203
Amado-Rodríguez L, Bernal T, López-Alonso I, Blázquez-Prieto J, García-Prieto E, Albaiceta GM (2016) Impact of initial ventilatory strategy in hematological patients with acute respiratory failure: a systematic review and meta-analysis. Crit Care Med 44(7):1406–1413
Wise MP, Barnes RA, Baudouin SV, Howell D, Lyttelton M, Marks DI et al (2015) Guidelines on the management and admission to intensive care of critically ill adult patients with haematological malignancy in the UK. Br J Haematol 171(2):179–188
Huaringa AJ, Francis WH (2019) Outcome of invasive mechanical ventilation in cancer patients: Intubate or not to intubate a patient with cancer. J Crit Care 50:87–91
Hakim H, Flynn PM, Knapp KM, Srivastava DK, Gaur A (2009) Etiology and clinical course of febrile neutropenia in children with cancer. J Pediatr Hematol Oncol 31(9):623
Choudhari S, Gawande R, Watchmaker J, Bamnote P, Mishra P, Dwivedi P (2023) Bloodstream infections in cancer patients in central India: trend over five years. Access Microbiol 000673. https://doi.org/10.1099/acmi.0.000673.v1
Kumar K, Subash C, Prabhu D, Pulikkal D, Basker D (2021) Pattern of bacterial infections in Indian bone marrow transplant patients-experience from Chennai India. Blood 138:4855
Chauhan P, Gupta A, Gopinathan M, Sanjeev GA, Khanna S et al (2022) Real-world challenges in the management of acute myeloid leukemia: a single-center experience from North India. Ann Hematol 101(6):1261–73
Ghosh S, Chakraborty M, Samanta S, Sinha N, Saha S, Chattopadhyay A et al (2021) Analysis of blood stream infections, antibiograms and clinical outcomes in haematological patients with febrile neutropenia: data from a tertiary care haematology institute in India. Ann Hematol 100(2):395–403
Peter JV, Thomas K, Jeyaseelan L, Yadav B, Sudarsan TI, Christina J et al (2016) Cost of intensive care in India. Int J Technol Assess Health Care 32(4):241–245
Singh S, Lionel S, Jain H, Nayak L, Selvarajan S, Samuel P et al (2022) Real world data on unique challenges and outcomes of older patients with AML from resource limited settings: Indian acute leukemia research database (INwARD) of the hematology cancer consortium (HCC). Blood 140(Supplement 1):6096–6098
Acknowledgements
SS and VG designed the research study and protocols. SS, RS and GK performed the research and data entry. SS, JS and KJ performed literature search and statistical analysis. SS and PG analyzed and verified the data. SS, JS and PG wrote the paper and reviewed the final version. The authors thank Ms Namita Bansal for performing statistical analysis for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singh, S., Sharma, R., Singh, J. et al. Clinical Outcomes and Determinants of Survival in Patients with Hematologic Malignancies Admitted to Intensive Care Units with Critical Illness. Indian J Hematol Blood Transfus 40, 423–431 (2024). https://doi.org/10.1007/s12288-024-01757-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-024-01757-3