Abstract
Objective
To collect information on clinical practice and current management strategies in 22 Italian neurosurgical hospitals for patients with aneurysmal subarachnoid hemorrhage.
Design and setting
Observational 6-month study for prospective data collection.
Patients
350 cases of aneurysmal subarachnoid hemorrhage.
Measurements and results
Each center enrolled from 4–36 patients. Neurological deterioration (24%) was more frequent in patients with higher Fisher classification, and with pretreatment rebleeding and it was associated with an unfavorable outcome (46%, 36/78, vs. 33%, 83/251). Aneurysms were mainly secured by clipping (55%, 191/350). An endovascular approach was utilized in 35% (121/350). The more frequent medical complications were fever, recorded in one-half of cases, pneumonia (18%), sodium disturbances (hyponatremia 22%, hypernatremia 17%), cardiopulmonary events as neurogenic pulmonary edema (4%) and myocardial ischemia (5%). Intracranial hypertension was experienced in one-third of the patients, followed by hydrocephalus (29%) and vasospasm (30%). Cerebral ischemia was found in an about one-quarter of the cohort. To identify the independent predictors of outcome we developed a model in which the dichotomized Glasgow Outcome Scale was tested as function of extracranial and intracranial complications. Only high intracranial pressure and deterioration in neurological status were independent factors related to unfavorable outcome.
Conclusions
Our data confirm that in every step of care there is extreme heterogeneity among centers. These patients are complex, with comorbidities, immediate risk of rebleeding, and delayed risk of intracranial and medical complications. Following SAH early treatment and careful intensive care management requires the careful coordination of the various clinical specialties.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subarachnoid hemorrhage (SAH) is a frequent neurosurgical emergency caused by the extravasation of blood in the subarachnoid space [1]. The leading cause of nontraumatic SAH is intracranial aneurysm rupture accounting for more than 80% of presenting cases. This has a worldwide incidence of about 10.5/100,000 per year, with substantial racial differences [2]. During 2003 in Italy, with a population of 56.3 million, 5,178 patients were discharged from hospital (http://www.ministerosalute.it/programmazione/sdo/ric_informazioni/sceltadia.jsp; accessed 6 January 2007) with a diagnosis of aneurysmal SAH (aSAH), indicating a national incidence of 9.1 hospitalized cases per 100,000 per year. Data on mortality and morbidity of aSAH in Italy are not available. In recent decades the management of aSAH has become increasingly multidisciplinary, involving a team composed of neurosurgeons, neuroradiologists, anesthesiologists, and intensivists. After initial stabilization, aimed at restoring respiratory and cardiovascular function, the main treatment goals are the prevention and treatment of rebleeding, hydrocephalus and vasospasm, and the management of medical and neurological complications. For each of these aims different approaches are available, but there is no evidence to suggest an optimal regime [3, 4].
The aim of this study was to prospectively survey clinical practice and management strategies in 22 neurosurgical Italian hospitals for patients with aneurysmal aSAH. Our hypothesis was that management approaches to SAH are extremely variable and habitually due to local policies rather than to evidence based criteria. Preliminary data were presented at the 2005 ESICM Congress and have been published as abstract [5].
Methods
Patient recruitment started on 1 September 2004 in 22 Italian neurosurgical centers which had previously participated in a data exchange network [6]. The collaborating centers are listed in the acknowledgement section. All 350 patients were included who were admitted to participating hospitals with a diagnosis of aSAH regardless of Hunt and Hess (HH) grade [7] and of age (mean age 57 ± 14 years; 61% women). Cases in which the SAH was not related to the presence of a documented ruptured aneurysm and cases due to other vascular pathologies were excluded. Each center enrolled between 4 and 36 patients. Centers were ranked according to the number of enrolled patients; there were six low-volume centers (0–10 patients, total 40 cases), nine medium-volume centers (11–20 patients, total 131 cases), and seven high-volume centers (> 20 patients, total 179 cases). Admission to the neurosurgical hospital was direct in 127 patients (37%) while in 223 cases (63%) patients were referred from other hospitals without neurosurgical coverage; referrals were more common in high-volume than medium or low-volume centers. Patients were admitted to neurointensive care units (47%), neurosurgical ward (48%), or other units (5%); median HH grade of those admitted to neurointensive care was 3 and that of the remaining patients was 2. A higher percentage of patients were admitted to the ICU in low-medium volume centers than in high volume centers. Enrollment lasted 6 months, and the study was completed with a 6-month follow-up on September 2005.
The following information was obtained in all patients and entered into a computerized database: (a) demographic data; (b) HH grade [7], World Federation of Neurosurgical Surgeons scale (WFNS) [8], Fisher scale [9], and aneurysm anatomy; (c) systemic and cerebral monitoring information; (d) systemic and cerebral complications, including intracranial hypertension (defined as intracranial pressure, ICP, > 20 mmHg), hydrocephalus, cerebral ischemia, and swelling (all these three identified by computed tomography, CT), pretreatment rebleeding (clinical and CT) and seizures (deterioration in neurological status was defined as a two-point reduction Glasgow Coma Scale, GCS, or new focal deficits; (e) treatment, i.e., endovascular coiling or neurosurgical clipping, timing, and complications; and (f) discharge and outcome information. To detect early deterioration the HH and WFNS severity scales were recorded twice: upon hospital admission and the worst evaluation before definitive aneurysm treatment. Analysis of changes in neurological evaluation allowed us to characterize pretreatment deterioration, discussed below.
Vasospasm was diagnosed in the presence of clinical deterioration, appearance of new symptoms (cephalalgia, confusion, seizure, or motor deficit), transcranial Doppler mean cerebral blood flow velocities above 120 cm/s (or a daily change in mean transcranial Doppler velocities of > 50 cm/s), or angiographic arterial narrowing [10]. EsaNET software developed by one of the authors (G.C.) was released free to all the participating centers in April 2004 as a run-time version (File Maker Pro SDK, Claris Solution Alliance, Santa Clara, Calif., USA); this works on Windows-based computers. The database captures 32 information items. A brief help manual containing definitions and indications for every field was incorporated in the software and printed as a booklet. A 24-h information hotline based at the coordinating center at the Monza Neurointensive Care Unit was available during the data collection period. Incoming data were carefully reviewed during and after the study period. After a first review, queries were submitted to the centers to clarify information, to overcome inconsistencies, and to obtain missing data. All patient outcomes were collected at discharge and 6 months after aSAH using the Glasgow Outcome Scale (GOS) [11].
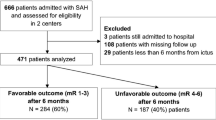
All summary data are expressed as mean ± standard deviation or as median when they were not normally distributed. Mean values were compared by analysis of variance (ANOVA). Differences in proportions were evaluated by the χ2 test. Differences at the level of p < 0.05 were considered statistically significant. The principal endpoint was the dichotomized GOS, with good recovery and moderate disability (GOS 4, 5) classified as favorable outcome and severe disability, vegetative and death (GOS 1–3) classified as unfavorable. Univariate statistical analysis was carried out to identify factors associated with outcome. A logistic regression model was chosen given the dichotomous dependent variables (outcome). All independent variables with p < 0.05 from the univariate analysis were entered into the multivariable model using a guided backward stepwise variable selection procedure. Odds ratios and confidence intervals were obtained for each statistically significant association. All statistical analyses were carried out using the statistical package Datadesk 6 (Data Description) and Statview (SAS Institute).
Results
Diagnosis and aneurysm location
Diagnosis of SAH was made by CT in 98.5% of cases (345/350). Diagnosis of aneurismal rupture was made by cerebral angiography in 71% (236/350) and by CT angiography in 24.3% (81/350). On admission CT 12 patients (3%) were Fisher scale grade 1 (normal scan), 80 (23%) were grade 2 (diffuse deposition of subarachnoid blood, no clots, and no layers of blood greater than 1 mm), 105 (32%) were grade 3 (localized clots and/or vertical layers of blood 1 mm or greater in thickness), and 145 (42%) were grade 4 (diffuse or no subarachnoid blood, but intracerebral or intraventricular clots). Aneurysms were located on the anterior communicating artery (n = 128, 37%), middle cerebral (n = 81, 23%), and internal carotid arteries (n = 52, 15%). Posterior circulation aneurysms were present in fewer than 10% (vertebral/basilar 2%, posterior inferior cerebellar artery 3%, and posterior communicating artery 2%). In 280 patients (83%) the aneurysm was single and in 57 (17%) multiple.
Neurological deterioration
Before treatment the majority of the patients remained neurologically stable (76.4%). A 1-point increase in HH scale was observed in 51 patients (14.7%), a 2-point increase in 20 (5.7%), and a 3 point or greater increase in 11 (3.2%; Table 1). No differences in gender, age, aneurismal location, referral status, admission unit, or blood pressure on admission were detected between patients who deteriorated and those who did not. Deterioration was more frequent in patients with higher Fisher grade: 12% (11/92) with grade 1 or 2 deteriorated vs. 28% with higher grade (71/253, χ2 p = 0.0019). Neurological deterioration was significantly more common in patients with aneurismal rebleeding (58.6%, 17/29) than in those without rebleeding (20%, 65/320, χ2 p < 0.0001). Patients with deterioration had a poorer outcome than those with no neurological deterioration (unfavorable outcome was 46%, 36/78, vs. 33%, 83/251, χ2 p 0.035).
Rebleeding
Aneurysm rebleeding occurred before treatment in 29 cases (8%). This complication was present in 22 (6.8%) of treated patients (322), with no difference either between early surgery and late surgery or between surgical and endovascular patients. Rebleeding was more frequent in untreated (7/29, 24%) than treated patients (22/321, 7%, p < 0.001). Unfavorable outcomes were significantly more frequent in patients who rebled than in those who did not (57% vs. 34%, p < 0.001).
Repair of aneurysm
Aneurysms were treated with surgical clipping in 191 patients (54%), an endovascular approach in 121 (54%), and a combined endovascular and surgical approach in 9 (2%). These cases are classified as surgical in the following discussion. Twenty-nine patients (8%) with a median HH score of 5 received neither surgical nor endovascular therapy.
Treatments modalities differed significantly by center (p < 0.0001, χ2). Surgery was used in more than 90% of cases in three, in more than 60% in ten, and in fewer than 60% in nine. Four centers limited coiling to less than 30% of the cohort. In five centers (three high-volume and two medium-volume centers) more than 60% of the patients received coiling. However, there was no statistical difference in the rates of surgical therapy between low-volume (65% of cases surgically treated, 26/40), medium-volume (58% of cases surgically treated, 76/131), and high-volume centers (54% of cases surgically treated, 98/179). Endovascular coiling was used in 37% of high-volume centers, 33% of medium-volume, and 25% of low-volume centers; in five centers it was never used (one low-volume and four medium-volume centers).
Treatment was initiated within the first 24 h after symptom onset in 45% of patients (n = 159) in during the 24 to 72-h period in 28% (n = 93). There was no difference in timing of treatment between surgical and endovascular groups. Treatment was delayed (> 72 h) in 60 patients. No association between timing of treatment and outcome was evident (ANOVA).
Patients who underwent surgery were younger than those treated endovascularly (55 ± 12- vs. 59 ± 15 years; p ≤ 0.0001, ANOVA) and and had higher Fisher grades (3–4, 78% vs. 64%; p ≤ 0.005, ANOVA). Patients with higher HH grades received surgical therapy more often even, but this difference was not statistically significant (grades I–III, 58% surgery vs. 39% endovascular, no treatment 3%; IV or V, 56% surgery vs. 26% endovascular, no treatment 18%; ≤ 0.0001, χ2). Surgery was more frequent in patients with aneurysms located in the middle cerebral (90% surgically), posterior communicating (65%), and anterior communicating artery (58%) (p ≤ 0.0001, χ2); it was less common for aneurysms located cerebral anterior (47%), carotid (41%), cerebral posterior artery (40%), posterior inferior cerebellar artery (27%), and basilar artery (0%). Reasons for treatment selection were mainly anatomical (aneurysm morphology 66%, location 61%, and neck conformation 28%); availability of trained personnel, either surgical or endovascular, was the reason 25% and lack of neuroradiologist in 7%. Only 1% of patients expressed a preference for a specific treatment.
Extracranial and intracranial complications
Intra- and extracranial complications during the hospital stay and their association with outcome are summarized in Table 2. Intracranial complications included intracranial hypertension, experienced by one-third of patients, hydrocephalus (29%), and vasospasm [12] (29%), cerebral ischemia and neurological deterioration, i.e., a GCS reduction of 2 points and/or the appearance of new focal deficits, were described in one-quarter of the cohort. The most frequent medical complications were fever, recorded in one-half of cases, pneumonia (18%), sodium disturbances (hyponatremia 22%, hypernatremia 17%), neurogenic pulmonary edema (NPE, 4%) and myocardial ischemia (5%). As shown in Table 2, there was an association between systemic insults (fever, pneumonia, hypernatremia, and myocardial ischemia) and outcome. Moreover, cerebral insults (intracranial hypertension, hydrocephalus, cerebral ischemia and swelling, pretreatment rebleeding, and seizures) are associated with an increased incidence of unfavorable outcome.
ICP was monitored in 57.3% of the 350 patients, with intraventricular catheters in 45%, followed by intraparenchimal probes (7%) and subdural devices (11%, 3%). Lumbar drainage was inserted in 19 patients (5%). High ICP (> 20 mmHg lasting more than 5 min) was recorded in 121 patients, with a higher incidence seen in more severe patients (proportion of monitored patients presenting high ICP, ranked by HH grade: I, 13.1%; II, 17.3%; III, 29.1%; IV, 50%; V, 65.8%; p ≤ 0.0001, χ2). High ICP was treated with CSF removal (n = 82, 67%), sedation (n = 89, 73%), mannitol (n = 84, 69%), hyperventilation (n = 48, 39%), increasing cerebral perfusion pressure (n = 44, 36%), decompressive craniectomy (n = 26, 21%), hypertonic saline (n = 27, 22%) and barbiturates (n = 24, 19%). Intracranial hypertension was a univariate and multivariate predictor of unfavorable outcomes. Vasospasm was present in 108 patients (30%), with no significant difference between surgical and endovascular patients (30% vs. 28%). The incidence of vasospasm was increased in patients with higher HH grade but without reaching statistical significance (I, 27.1%; II, 28.7%; III, 27.8%; IV, 38%; V, 34.7%).
Vasospasm was treated with hypertension, hemodilution, and hypervolemia (triple-H therapy) [13] in 94 patients (87%) and less frequently with endovascular treatment (pharmacological 11%, n = 12; mechanical, 0.9%, n = 1). The presence of vasospasm was not a predictor of unfavorable outcome; however, patients with vasospasm had a trend to longer hospital stay (28 ± 18 vs. 23 ± 29 days).
Outcome
The GOS was determined at 6 months in 333 of the 350 patients (9.5% lost to follow-up). Outcome was good in 50% (n = 166), moderate disability in 14% (n = 47), and severe disability in 9% (n = 30); 3% were vegetative (n = 10) and 24% dead (n = 80). The location of the aneurysms did not affect outcome or the incidence of complications. Surgical patients had a favorable outcome in 66.7% of cases (n = 120) vs. 72.3% of those with endovascular treatment (n = 81; ns). A simple regression model tested the relationship between GOS and more than 20 variables, both intracranial (HH, WFNS, Fisher, rebleeding, neuroworsening, hydrocephalus, high ICP, vasospasm, seizures) and extracranial (NPE, myocardial ischemia, hypo-/hypernatremia, fever, pneumonia). In a logistic regression model (Table 3) only elevated ICP, neurological deterioration, HH grade, age over 60 years, and seizures were independent predictors of unfavorable outcome. We believe that multivariate analysis, such as the model that we used, better captures the weight of specific features on the final outcome than repeated univariate analyses. Based on the model shown in Table 3 the odds ratio for unfavorable outcome due to the worst HH recorded is 2. There was no statistical difference in outcome between cases treated by surgery and those treated by coils. We also observed no difference in outcome between high-volume and low-volume centers.
Discussion
The aim of this study was to investigate the current treatment of SAH patients in a number of Italian centers. It was our hypothesis that approaches to SAH could be extremely variable and habitually due to local policies rather than to evidence based criteria. The data presented support this hypothesis. In contrast to another recently published paper [14] in which the treating team were asked to provide opinions and information, this research is based on the analysis of clinical cases: 350 patients were enrolled during 6 months in 22 neurosurgical hospitals. Although this number seems remarkable, it should be emphasized that the centers participating in the study, located mainly in the northern part of our country, have a special interest in clinical research and are probably not representative of aSAH management practices nationwide.
Referral system and case load
In our country there are 116 neurosurgical units, i.e., one for fewer than 500,000 inhabitants. The number of aSAH patients treated annually in the studied centers varied between 8 and 72. In the centers with higher case-load a maximum of 40 endovascular or of 46 surgically treated aSAH patients per year were recorded. At the other extreme there were centers treating fewer than 10 cases per year. It appears difficult, at least in the low-volume centers, to maintain an adequate level of expertise in all the involved specialties, to train new physicians, to offer all the possible therapeutic opportunities (endovascular and/or surgery) and to be cost effective. In aSAH, as in other surgical conditions, a strong relationship has been demonstrated between case-load and outcome, with high-volume centers achieving significantly better results [15–17]. Our data do not confirm these concepts, since we did not observe outcome differences between high- and low-volume centers. For this analysis, however, our sample is clearly underpowered.
More than 50% of patients were referred from primary treatment centers generally without neurosurgical coverage to treatment centers with variable case-loads. There are no specific rules for transferring aSAH patients to designated centers, and this is reflected in our results. Interestingly, all medical and surgical emergencies in our country are managed through a centralized call system which collects calls, dispatches ambulances and helicopters and supervises hospital admission. The system covers a great part of the country but is restricted by the shortage of beds, operating room availability for emergencies, etc. Our data suggest a need to rationalize the triage of neurosurgical emergencies such as aSAH to designated tertiary referral centers with higher case-loads and trained specialists.
Deterioration in aSAH
Using the HH score on admission as a baseline and comparing it with the worst score assessed before treatment detected neurological deterioration in about one-quarter of the population. This deterioration was significantly correlated with an aneurysmal rebleeding and with higher Fisher grade. The link between neurological deterioration, rebleeding, and poor outcomes following aSAH reinforces the need for early aneurysmal repair. Neurological deterioration can also be due to hydrocephalus, vasospasm, and seizures, complications whose prevention and treatment mandate intensive and rigorous monitoring protocols as all may be favorably affected by appropriate medical intervention.
Complications
As documented in other series [18–23], medical and intracranial complications are frequent and have a significant association with negative outcome. We recorded a number of systemic complications including dramatic physiological alterations such as NPE and raised ICP and also disturbances of sodium balance, with hypo- or hypernatremia recorded in a total of 32% of cases, highlighting the importance of careful medical care of these patients. Fever per se can adversely affect ICP and exacerbate cerebral ischemia [24, 25] and is felt to be an independent contributor to worse outcome following aSAH [26]. Our data confirm fever as a frequent complication. Preexisting medical diseases such as cardiorespiratory insufficiency, diabetes, and arterial hypertension are frequent in the aSAH population and may decompensate following aneurismal rupture [27].
Aneurysm repair
Surgical clipping was the most frequent strategy for aneurysm securing, but different strategies are pursued in each center. In some centers surgery was uncommon while in others centers almost all the patients were operated on, often reflecting the nonavailability of endovascular specialists. No statistically significant association between increased propensity for surgery and case-load was detected. Two recent randomized controlled trials and a Cochrane collaboration systematic review [28] demonstrated that endovascular coiling is associated with a better outcomes for patients with ruptured aneurysms of either the anterior or posterior circulation who present in good clinical condition and are suitable for both surgical and endovascular treatment [29, 30]. We observed no significant difference in outcome between surgical and endovascular patients, but this dataset is not sufficiently large for such an analysis, and furthermore any comparison in unselected, nonrandomized patients without adjustment for severity would be inappropriate.
In this series a significant proportion of patients had ICP and/or CSF catheters, a higher proportion than previously reported in a national survey [31], probably reflecting a selection bias towards more specialized neurosurgical centers, many of which have adopted an aggressive therapeutic approach with respect to intracranial hypertension including the administration of barbiturates and decompressive craniectomy. Finally, this study shows that it is feasible to collect a large amount of data through an organization with strong commitment but limited resources. The study was inexpensive, as centers were offered no funding, and its success depended upon the commitment of the participants. Nevertheless the data returned were generally of high quality with regard to completeness of information. More than 90% of potential observations were completed, and data checking revealed few recordings outside specified ranges or showing obvious inconsistencies requiring referral back to the investigator for clarification.
Limitations of the study
The selection of the centers, although this may have only a minor effect on the incidence of complications, could influence the results on quantitative and qualitative outcome. Moreover, a confirmation of the accuracy of the data by comparison with original case records was not possible, as this process is extremely time and labor intensive.
Conclusions
Our data confirm that in every step of care, from transport to ICP monitoring, there is extreme heterogeneity among centers. Subarachnoid hemorrhage remains a great challenge for the treating team. The patients to be treated are complex, with comorbidities, immediate risk of rebleeding, and delayed risk of intracranial and medical complications. SAH requires the combination of various specialties who must coordinate their efforts for early treatment and careful intensive care in the following weeks.
References
Gijn J van, Rinkel GJ (2001) Subarachnoid haemorrhage: diagnosis, causes and management. Brain 124:249–278
Suarez JI, Tarr RW, Selman WR (2006) Aneurysmal subarachnoid hemorrhage. N Engl J Med 354:387–396
Naval NS, Stevens RD, Mirski MA, Bhardwaj A (2006) Controversies in the management of aneurysmal subarachnoid hemorrhage. Crit Care Med 34:511–524
Al-Shahi R, White PM, Davenport RJ, Lindsay KW (2006) Subarachnoid haemorrhage. BMJ 333:235–240
Citerio G, Gallizzi F, Cazzaniga S, Galli D, Patruno A, Sganzerla E (2005) Management Of aneurysmal subarachnoid hemorrhage: time for practical guidelines. Intensive Care Med 31[Suppl 1]:315
Citerio G, Stocchetti N, Cormio M, Beretta L (2000) Neuro-Link, a computer-assisted database for head injury in intensive care. Acta Neurochir (Wien) 142:769–776
Hunt WE, Hess RM (1968) Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg 28:14–20
Drake C (1988) Report of World Federation of Neurological Surgeons Committee on a Universal Subarachnoid Hemorrhage Grading Scale. J Neurosurg 68:985–986
Fisher CM, Kistler JP, Davis JM (1980) Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery 1:1–9
Okada Y, Shima T, Nishida M, Yamane K, Hatayama T, Yamanaka C, Yoshida A (1999) Comparison of transcranial Doppler investigation of aneurysmal vasospasm with digital subtraction angiographic and clinical findings. Neurosurgery 45:443–449
Jennett B, Bond M (1975) Assessment of outcome after severe brain damage. Lancet I:480–484
Janjua N, Mayer SA (2003) Cerebral vasospasm after subarachnoid hemorrhage. Curr Opin Crit Care 9:113–119
Sen J, Belli A, Albon H, Morgan L, Petzold A, Kitchen N (2003) Triple-H therapy in the management of aneurysmal subarachnoid haemorrhage. Lancet Neurol 2:614–621
Sakowitz OW, Raabe A, Vucak D, Kiening KL, Unterberg AW (2006) Contemporary management of aneurysmal subarachnoid hemorrhage in Germany: results of a survey among 100 neurosurgical departments. Neurosurgery 58:137–145
Bardach NS, Zhao S, Gress DR, Lawton MT, Johnston SC (2002) Association between subarachnoid hemorrhage outcomes and number of cases treated at California hospitals. Stroke 33:1851–1856
Cross DT 3rd, Tirschwell DL, Clark MA, Tuden D, Derdeyn CP, Moran CJ, Dacey RG Jr (2003) Mortality rates after subarachnoid hemorrhage: variations according to hospital case volume in 18 states. J Neurosurg 99:810–817
Berman MF, Solomon RA, Mayer SA, Johnston SC, Yung PP (2003) Impact of hospital-related factors on outcome after treatment of cerebral aneurysms. Stroke 34:2200–2207
Diringer MN (2003) Subarachnoid hemorrhage: a multiple-organ system disease. Crit Care Med 31:1884–1885
Solenski NJ, Haley EC Jr, Kassell NF, Kongable G, Germanson T, Truskowski L, Torner JC (1995) Medical complications of aneurysmal subarachnoid hemorrhage: a report of the Multicenter, Cooperative Aneurysm Study. Crit Care Med 23:1007–1017
Gruber A, Reinprecht A, Illievich UM, Fitzgerald R, Dietrich W, Czech T, Richling B (1999) Extracerebral organ dysfunction and neurologic outcome after aneurismal subarachnoid hemorrhage. Crit Care Med 27:505–514
Wartenberg KE, Mayer SA (2006) Medical complications after subarachnoid hemorrhage: new strategies for prevention and management. Curr Opin Crit Care 12:78–84
Wartenberg KE, Schmidt JM, Claassen J, Temes RE, Frontera JA, Ostapkovich N, Parra A, Connolly ES, Mayer SA (2006) Impact of medical complications on outcome after subarachnoid hemorrhage. Crit Care Med 34:617–623
Vespa P (2006) The three tenors of subarachnoid hemorrhage: fever, anemia, and hyperglycemia. Crit Care Med 34:897–898
Sminia P, Van Der Zee J, Wondergem J, Haveman J (1994) Effect of hyperthermia on the central nervous system: a review. Int J Hyperthermia 10:1–30
Corbett D, Thornhill J (2000) Temperature modulation (hypothermic and hyperthermic conditions) and its influence on histological and behavioral outcomes following cerebral ischemia. Brain Pathol 10:145–152
Diringer MN, Reaven NL, Funk SE, Uman GC (2004) Elevated body temperature independently contributes to increased length of stay in neurologic intensive care unit patients. Crit Care Med 32:1489–1495
Kochanek PM, Yonas H (1999) Subarachnoid hemorrhage, systemic immune response syndrome, and MODS: is there cross-talk between the injured brain and the extra-cerebral organ systems? Multiple organ dysfunction syndrome. Crit Care Med 27:454–455
Schaaf I van der, Algra A, Wermer M, Molyneux A, Clarke M, van Gijn J, Rinkel G (2005) Endovascular coiling versus neurosurgical clipping for patients with aneurysmal subarachnoid haemorrhage. Cochrane Database Syst Rev 19 Oct (4):CD003085
Rl Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, Holman (2002) International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. Lancet 360:1267–1274
Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, Sandercock P (2005) International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet 366:809–817
Stocchetti N, Longhi L, Magnoni S, Roncati Zanier E, Canavesi K (2003) Head injury, subarachnoid hemorrhage and intracranial pressure monitoring in Italy. Acta Neurochir (Wien) 145:761–765
Acknowledgements
The authors thank Dr. Robert D. Stevens (Division of Neurosciences Critical Care, Johns Hopkins University School of Medicine, Baltimore, USA) for his extensive editing of the manuscript and for his expert advice. The authors are indebted to the clinical research associates who participated in the data collection: Dr. R. Trigliani, M. Scerrati (Ancona Torrette); Dr.ssa P. Ceccarelli, Dr. M. Mergoni (Azienda Ospedaliera di Parma); Dr. S. Chibbaro (Cattinara Trieste); Dr. F. Tartara, Dr. P. Versari (Civile Alessandria); Dr.ssa MM. Archilli (CTO Torino); Dr. R. Potenza, Dr. CA. Castioni (G. Bosco Torino); Dr. A. Cardia (Galeazzi Milano); Dr. V. Valeriani (Galliera Genova); Dr. L. Arnaboldi (Gravedona); Dr. F. Lusenti, Dr. E. Crestan (Lecco); Dr.ssal. Cancelliere, Dott. GL. Vignazia (Maggiore Novara); Dr. F. Procaccio. Dott.ssa E. Basso (Azienda Ospedaliera di Verona); Dr. A. Caricato, Dr. E. Marchese (Policlinico A. Gemelli, Roma); Dr. L. Longhi, Dr. F. Acerbi (Policlinico Milano); Dr. R. Pugliese, Dr. R. Imberti (Policlinico San Matteo, Pavia); Dr.ssa F. Gallizzi; Dr.ssa M. Crespi (San Gerardo Monza); Dr. M. Berardino, Dr. C. Carlino (San Giovanni Battista Torino); Dr. M. Cenzato (San Raffaele Milano); Dr. D. Vidili, Dr. G. Profili (Sassari); Dr. A. Perin, Dr. M. Tripodi (Treviso); Dr. S. Peron (Varese); Dr.ssa S. Rossi (Vicenza). We gratefully acknowledge Sara Cazzaniga, PhD, for the careful review of collected the study data during and after period.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Citerio, G., Gaini, S.M., Tomei, G. et al. Management of 350 aneurysmal subarachnoid hemorrhages in 22 Italian neurosurgical centers. Intensive Care Med 33, 1580–1586 (2007). https://doi.org/10.1007/s00134-007-0700-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0700-5