Abstract
Objective
To monitor the use of drotrecogin alfa activated (DrotAA) in Italy and its effects on patients' health.
Design
Prospective pharmaco-surveillance program with a parallel non-randomized control group.
Setting
The Ministry of Health required all intensive care units (ICUs) using DrotAA to participate in the pharmaco-surveillance program. Our control group was formed of patients eligible for treatment with DrotAA but who had not received it.
Patients and participants
The data we collected included basic demographic characteristics, indications, modalities of use, adverse events, and ICU mortality. We identified potentially non-collaborating centres on the basis of data on DrotAA purchasing by hospitals.
Measurements and results
From 2003 to 2006, 668 cases of treatment with DrotAA were reported. We estimate that 79.3% of all patients treated in Italy in this period were recruited. Off-label use was common. Delayed start was the main reason for off-label prescription. Bleeding during infusion occurred in 73 patients (10.9%). The ICU mortality was higher in patients with bleeding (57.5 vs. 44.9%; p = 0.041). Crude ICU mortality was lower in patients receiving DrotAA than in controls (46.4 vs. 54.9%; p = 0.0004); however, multivariate analysis, which adjusted for certain relevant differences, showed that DrotAA treatment was associated with higher mortality after scheduled surgery.
Conclusions
These results question the way in which the drug is used in everyday clinical practice and its efficacy in a selected subgroup, and reinforce the need for a new, independent, confirmatory trial to reassess the risk-to-benefit ratio of DrotAA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Although progress has been made in the treatment of critically ill patients, severe sepsis is still burdened with high morbidity and mortality [1, 2]. On the basis of a single randomized clinical trial [3], in August 2002 the European Medicines Agency (EMEA) approved “under exceptional circumstances” Drotrecogin alfa activated (DrotAA), for adults with severe sepsis associated with multi-organ dysfunction (MOD) [4]. EMEA approval “under exceptional circumstances” is given when comprehensive data on the efficacy and safety of the drug [5] are not available, due to the rarity of the indication, the state of scientific knowledge, or the principles of medical ethics. In these cases, strict monitoring with annual reassessment of safety and efficacy is required. In 2003 the Italian Ministry of Health approved DrotAA use, requiring all users to participate in a pharmaco-surveillance program to evaluate the safety and efficacy of the drug, and the degree of its utilization. Since severe sepsis and septic shock are almost exclusively treated in intensive care units (ICUs), the Italian Medicine Agency of the Ministry of Health (AIFA – “Agenzia Italiana del Farmaco”), which has funded the study, entrusted it to the GiViTI (Italian Group for the Evaluation of Interventions in Intensive Care Medicine), a nationwide network gathering more than half of the Italian ICUs.
Here we present data about patients treated with DrotAA from June 2003 through March 2006. We also compare this treated (exposed) group with a non-treated (unexposed) group of patients with severe sepsis who matched the criteria for treatment with DrotAA.
Methods
Treatment group
All patients who received DrotAA were eligible for treatment with the drug. The case report form (CRF) included basic demographic characteristics, date of ICU admission and discharge, date of the start of treatment, and ICU mortality. Variables needed to compute the severity of infection (sepsis, severe sepsis, and septic shock) [6], the Simplified Acute Physiology Score II (SAPS II) [7], and the Sequential Organ Failure Assessment (SOFA) score [8] were collected at the time of the start of treatment, along with data on the source and characteristics of infections. The SOFA score variables were also collected after drug infusion was finished. Adverse events causing interruption or discontinuation of drug administration were also reported.
Collected data were entered either in an online CRF or in an ad hoc DrotAA form in the Margherita database. This database is maintained by a GiViTI nationwide project for continuous quality-of-care assessment [9], currently witnessing the participation of 180 Italian ICUs. It was designed for easy expansion of the core data collection to fulfil the requirements of specific research projects. Core data included demographics, admission diagnoses, comorbidities, reasons for admission, surgical status, SAPS-II variables, failures and diseases occurring and major procedures/interventions performed during the stay in the ICU, as well as ICU and hospital outcome. Both the CRFs performed several plausibility checks during data entry. Data were further reviewed by the coordinating centre, which contacted individual ICUs to solve problems whenever they occurred (see online supplement). A detailed operating manual specified all the definitions employed.
Since the original CRF provided only a rough estimate of appropriateness of prescription and adverse effects, in June 2005 it was replaced by a modified version detailing timing of administration, number and nature of organ dysfunctions, timing of surgery, and severity of adverse events. It is noteworthy that both in the original and the modified form only infusion-period adverse effects, including bleeding events, were reported. To facilitate the completion of the form, the modified CRF was simplified by suppressing the SAPS II and final SOFA fields.
Adherence to the surveillance program
Physicians were required to report every treatment with DrotAA. We used data supplied by the Ministry of Health on drug purchases by single hospitals to estimate the total number of treatable patients in each hospital (see online supplement). In consideration of the high cost of the drug and the relative rarity of its indications, we expected a single hospital to stock no more DrotAA than was required for three complete courses of treatment. All hospitals with a gap greater than 3 between the number of treatable patients and the number of cases actually reported were considered possibly non-compliant and the AIFA sent their directors a reminder. This policy was adopted throughout 2004 and 2005. After receiving the warning, the directors of still possibly non-compliant hospitals were informed that they would be summoned to the Ministry of Health for clarification.
Off-label use
We were able to identify off-label (OL) use of DrotAA with varying degrees of accuracy depending on the version of the CRF used. Administration was defined as OL in the following cases: patients aged less than 18 years (available in both the original and modified CRFs); patients without sepsis-associated MOD, organ dysfunction being defined as SOFA score > 0 (available in both CRFs); when more than 48 h had passed between the onset of the first sepsis-induced organ dysfunction and the beginning of administration for patients treated after January 2005, when thisrestriction was introduced in the Summary of Product Characteristics (SPC, available in the modified CRF only); patients with less than 30,000 platelets per cubic millimeter (available in the modified CRF only). We verified whether OL use was associated with mortality and bleeding, the latter being the most important adverse event ascribed to this drug.
Untreated (control) group
In 2005, 110 Italian ICUs participating in the Margherita project took part in an infection surveillance program. All patients were screened for infections on ICU admission and daily during their stay. Infections were diagnosed by attending physicians according to Centers for Disease Control (CDC) definitions [10] or, for fever of unknown origin, suspected systemic catheter-related infection, pneumonia, and central nervous system infection (ventriculitis), according to the definitions reported in the online supplement. Infections were also classified as community acquired, hospital acquired, or ICU acquired. The severity of infection on admission and the most severe infection-related conditions during the ICU stay were also reported, along with the dates of their occurrence. Severity was defined according to criteria proposed in 1992 [11] and revised in 2001 [6], as: “infection with or without SIRS”, “severe sepsis” and “septic shock”.
On the basis of available data we were able to identify, with good approximation, patients eligible to receive DrotAA. These were adults with severe sepsis or septic shock and MOD at admission or acquired during stay who did not have any contraindication to the drug. Table 1 presents the contraindications listed in the SPC [12] which we were able to identify in our database. The patients eligible for treatment with DrotAA who did not receive it formed the control (unexposed) group. Patients of possibly non-compliant centres were always excluded to avoid misclassification of drug administration (Fig. 1).
Data presentation and statistical analysis
We used proportion as descriptive statistic for categorical variables, and mean, standard deviation, median and interquartile range for continuous variables. We performed bivariate analyses using the t-test for quantitative variables and the chi-square test (or Fisher's exact test, if indicated) for qualitative variables. To identify prognostic factors for ICU mortality we developed a multivariate logistic regression model including all patients eligible for DrotAA treatment from both the unexposed and the exposed groups (OL patients were hence excluded). We tested the assumption that the logit is linear in the quantitative variables by analysing the estimated coefficients of designed variables representing the quartiles of the original variable distribution [13]. Whenever suggested by this analysis, we tested a second-order model or log-transformation of the variable. If these approaches failed to fit the data, we divided the variable into classes and used dummy variables [13]. Independent variables associated with ICU mortality with a conservative criterion (p < 0.3) were entered into a step-by-step backward-forward approach in which different models were selected with a p < 0.05 criterion at the likelihood ratio test. Independent variables tested included gender, age, surgical status, trauma, severity of infection, use of DrotAA and all possible interactions among these categories.
All tests were two-tailed, with 0.05 as level of significance. We used SAS software to analyse the data (version 9.02, SAS, Cary, N.C.).
Results
Study participation
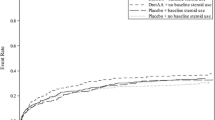
From July 2003 to March 2006, a total of 709 patients from 134 ICUs who had been treated with DrotAA were recruited (see online supplement for description). Some ICUs bought the drug only several months after July 2003, so the average number of treated patients per year per unit was 2.6 (see the online supplement). Since 41 patients (5.8%) were still in the ICU or under examination at the time of our analysis, we discarded them and evaluated only the remaining 668 cases. The data relative to 344 patients were reported in the original CRF form, whereas the modified form was used for the remaining 324 patients. Table 2 illustrates the main features of the sample. The recruitment rate over time is presented in Fig. 2. Relying on our data on DrotAA purchasing by Italian hospitals, if we assumed an average hospital stock of enough DrotAA for two courses of treatment, it could be estimated that our case group included 79.3% of all patients treated in Italy in the period under consideration. The control group was formed of 1181 patients not treated with DrotAA but possibly eligible for treatment, recruited through the infection surveillance program carried out by GiViTI in 2005.
The description of patients who received the drug and potentially eligible patients who did not receive it (unexposed group) is provided in Table 2. Treated patients were significantly younger than untreated ones, more frequently surgical, and more frequently with trauma.
Off-label use was quite frequent: 13.6% before and 27.8% after the introduction of the timing restriction by the EMEA (Table 3).
We regarded 12 more cases reported with the modified CRF as possibly OL since the drug was started on the same day that these patients underwent surgery, whereas the drug should not be administrated within 12 h after surgery [12]. Neither ICU mortality (46.1% in OL patients, 46.5% in the others; p = 0.94), nor bleeding (7.0% in OL, 11.9% in non-OL; p = 0.12) were associated to the off-label use of the drug.
Safety evaluation
Data on completion of the 96-h course of treatment were unavailable in 3 cases. Only 431 of the remaining 665 patients (64.8%) completed the course without any interruption. Seventy-seven (11.6%) patients completed the course with at least one interruption, and in 157 cases (23.6%) infusion was stopped altogether before the 96-h course was over. Causes for interruption are reported in Table 4. Bleeding events during the infusion period occurred in 73 patients (10.9%; sites reported in Table 5). The ICU mortality was higher in patients with bleeding than in patients without bleeding (57.5 vs. 44.9%; OR = 1.66, 95% CI = 1.02–2.72; p = 0.041). This relationship was not statistically different in medical and surgical patients (OR = 1.55 and 1.81, respectively; p of the Breslow–Day test for homogeneity of the ORs = 0.76).
Twenty-nine bleeding events (8.9%) were reported with the modified CRF (324 patients), which called for a detailed evaluation of the severity of bleeding; of these, 15 (4.6%) were classified as severe according to commonly shared definitions (i.e. they resulted in death, were life-threatening, required prolonged hospitalization, caused persistent or significant disability or incapacity, or required more than 2 units of blood transfusion). In 3 cases, haemorrhage due to DrotAA was life-threatening, and in 2 others it was fatal.
Reporting of bleeding events was not available for the unexposed group.
Outcome
Crude ICU mortality was significantly lower in patients receiving DrotAA than in unexposed ones (Table 2); however, there were important differences between treated and untreated patients. Table 6 presents the result of our multivariate logistic regression model, which gives ORs adjusted for possible confounders. Only the 540 in-label cases and all the 1181 unexposed patients were included in this model. Patients treated according to the label did not differ in any respect from treated patients as a whole (data not shown). Age and the occurrence of septic shock were independently associated with ICU mortality. Conversely, DrotAA administration and surgical status (i.e. surgery within 7 days before or 24 h after admission) significantly interacted in influencing the outcome. This means that the association between DrotAA and mortality differed according to surgical status, making it difficult to compute the ORs for DrotAA use [13]. For this reason, Table 6 also provides the ORs for DrotAA, along with the 95% CI for each level of surgical status.
Discussion
DrotAA is the first anti-inflammatory drug that has been proven to be effective in the treatment of severe septic patients [3]; however, it has also determined an increase in serious bleeding events [3] and, more importantly, subgroup analyses of the PROWESS trial have suggested that its efficacy differed in patients with high or low risk of death [14]. Correspondingly, ADDRESS, a placebo-controlled randomized trial which evaluated DrotAA in severe septic patients with low risk of death, was interrupted for futility when only 2640 patients of the planned 11,444 had been enrolled [15]. A heated debate on the risk-to-benefit ratio of the drug arose [16] and is still ongoing [17]. Independent data on the efficacy and safety of DrotAA have been demanded [16, 17, 18].
As prescribed in cases of EMEA approval “under exceptional circumstances”, AIFA (the Italian Medicine Agency) organized a mandatory pharmaco-surveillance program to monitor the use of DrotAA and its consequences on patients' health in Italy. Adherence to the project was assessed with the assistance of the Ministry of Health. Two features of the recruitment rate over time (Fig. 2) are noteworthy, namely, the increasing use of the drug, and the effectiveness of the personalized reminder letter of the Ministry of Health in promoting participation in the study. This allowed the recruitment into the surveillance program of a very high percentage of the treated cases (between 70 and 100%), an important achievement. Thanks to such an extensive coverage, the study's description of the clinical use of DrotAA is representative and informative. Furthermore, it provides a comparatively unbiased estimate of the occurrence of adverse events, a result which would not have been achievable with spontaneously provided data [19]. The good result obtained indicates that strict monitoring and promotion of participation is feasible and should be enacted whenever possible.
The high percentage of off-label prescriptions (13.6 and 27.8%, respectively, before and after the introduction of the timing restriction mentioned above) is another important finding. It is noteworthy that the number of platelets was not recorded for the 344 patients recruited with the original CRF, so that OL use in those cases is relatively underestimated.
The rate of serious bleeding during the infusion period reported with the modified form was higher compared with data from the PROWESS and the ENHANCE trials (4.6 vs. 2.4 and 3.6%, respectively), probably because of the more rigid criterion adopted in these trials to define serious bleeding in terms of blood transfusion (administration of more than 2 units of packed red cells vs. administration of 3 units on two consecutive days).
The rate of fatal or life-threatening events was worrisome: three life-threatening (0.9, 95% CI 0.3–2.6%) and 2 fatal (0.6%, 95% CI 0.2–2.2%) events were reported with the modified form. The rate of fatal events was 0.2% in PROWESS and ENHANCE, whereas life-threatening bleeding events were not reported [20]. Our finding is comparable to the 0.7% rate of fatal bleeding events reported in a retrospective study which reviewed 274 medical records of patients treated with DrotAA in the United States [21], and questions that the septic populations studied by PROWESS and ENHANCE can be regarded as representative of the population encountered in every-day clinical practice.
Data from trials, which unavoidably recruit a low number of patients compared with the population target of the drug, cannot provide reliable statistics on infrequent and serious adverse events. We believe that surveillance programs should be mandatory after the approval of drugs with this kind of adverse effects, at least until drug use spreads and thousands of patients are treated, and data about safety are hence sufficient to confirm that the benefit-to-risk profile is advantageous.
The ICU mortality rate observed among in-label patients treated with DrotAA (46.5%) was much higher indeed than the 28-day mortality reported in PROWESS (26.5%) and ENHANCE (27.1%) in subgroups with MOD [3, 14, 20]. Since it is difficult to imagine a different degree of aggressiveness or quality of treatment in Italy, it would be tempting to deduce that the populations differ because Italian intensivists save DrotAA for sicker patients; however, this hypothesis is contradicted by the fact that ICU mortality in our untreated group (i.e. patients potentially eligible to DrotAA who did not receive the drug) was higher than the 28-day mortality assessed in the placebo group of PROWESS (54.9 and 34%, respectively). It can be concluded that the population selected in PROWESS is not representative of the Italian ICU population of patients with severe sepsis, who are at higher risk of death. This lack of representativeness of a trial's population compared with available data for current clinical practice is not new, especially for severe sepsis [22], and we believe it should act as an alarm bell for regulatory agencies, particularly when they are going to approve a drug on the basis of a single sponsored trial.
The results of our study show that the crude mortality rate is lower among treated patients; however, treated and untreated patients were quite different, the latter being presumably more severe than the former (older, more medical, more emergency surgical within surgical, less trauma, higher severity of sepsis). Our multivariate analysis, which adjusts for some relevant features, indicates that ORs for mortality of medical and unscheduled surgical patients were lower than 1, though non-significantly. This means that either there is a reduction of mortality – but subgroups are too small to provide significant results – or that no positive effect on mortality can be ascribed to treatment with DrotAA. Notably, DrotAA treatment was associated with a significant mortality increase among patients with MOD who underwent scheduled surgery (OR = 2.79, 95% CI 1.31–5.97). This finding, which resembles the results of the ADDRESS trial, which suggested a harmful effect of therapy in patients with recent surgery and a single organ failure [15], was of concern, because a subgroup of patients for whom DrotAA was still considered indicated had suffered harm from treatment. It is remarkable that this effect was not observed among unscheduled surgical patients; thus, we can hypothesize that surgery has not much to do with risk of death.
These results suggest, first of all, that the target population of DrotAA is not clearly defined, and that the current definition of high risk-of-death patients eligible for therapy is questionable; and secondly, that the treatment with DrotAA can be harmful for some subsets of patients who match the currently provided indications. Data from available RCTs, as well as from our study, leads us to believe that only a randomized confirmatory trial targeted to patients with sepsis-induced MOD can clarify the issue of indications and the risk-to-benefit profile of DrotAA. We suggest that it not be carried out by researchers who have a conflict of interest (e.g. employees or consultants of the manufacturer or those who share any other kind of financial interest with the manufacturer), and the manufacturer itself should be excluded from the organization and management of the trial, and from result analysis. We believe that if these conditions of independence are fulfilled, it will be possible to avoid disagreement and conflicting opinions on such an important aspect of therapy for severe sepsis.
References
Alberti C, Brun-Buisson C, Burchardi H, Martin C, Goodman S, Artigas A, Sicignano A, Palazzo M, Moreno R, Boulme R, Lepage E, Le Gall R (2002) Epidemiology of sepsis and infection in ICU patients from an international multicentre cohort study. Intensive Care Med 28:108–121
Linde-Zwirble WT, Angus DC (2004) Severe sepsis epidemiology: sampling, selection, and society. Crit Care 8:222–226
Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, Steingrub JS, Garber GE, Helterbrand JD, Ely EW, Fisher CJ Jr (2001) Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 344:699–709
EMEA. European Public Assessment Report. Scientific discussion for the approval of Xigris. Accessed in January 2006 at: http://www.emea.eu.int/humandocs/Humans/EPAR/xigris/Xigris.htm
EMEA. Guideline on procedures for the granting of a marketing authorisation under exceptional circumstances, pursuant to article 14 (8) of regulation (ec) no 726/2004. Accessed in January 2006 at: http://www.emea.eu.int/pdfs/human/euleg/35798105en.pdf
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med 29:530–538
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. J Am Med Assoc 270:2957–2963
Vincent JL, Mendonca A de, Cantraine F, Moreno R, Takala J, Suter PM, Sprung CL, Colardyn F, Blecher S (1998) Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med 26:1793–1800
Boffelli S, Rossi C, Anghileri A, Giardino M, Carnevale L, Messina M, Neri M, Langer M, Bertolini G (2006) Continuous quality improvement in Intensive Care Medicine. The GiViTI Margherita Project: Report 2005. Minerva Anestesiol 72:419–432
Garner J, Jarvis W, Emori T, Horan T, Hughes J (1996) CDC definitions for nosocomial infections. In: Olmsted R (ed) APIC infection control and applied epidemiology: principles and practice. Mosby, St. Louis, pp A1–A20
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101:1644–1655
EMEA. Xigris: Product information. Accessed in November 2006 at: http://www.emea.eu.int/humandocs/PDFs/EPAR/xigris/H-396-PI-en.pdf
Hosmer D, Lemeshow S (1989) Applied logistic regression. Wiley, New York
Dhainaut JF, Laterre PF, Janes JM, Bernard GR, Artigas A, Bakker J, Riess H, Basson BR, Charpentier J, Utterback BG, Vincent JL (2003) Drotrecogin alfa (activated) in the treatment of severe sepsis patients with multiple-organ dysfunction: data from the PROWESS trial. Intensive Care Med 29:894–903
Abraham E, Laterre PF, Garg R, Levy H, Talwar D, Trzaskoma BL, Francois B, Guy JS, Bruckmann M, Rea-Neto A, Rossaint R, Perrotin D, Sablotzki A, Arkins N, Utterback BG, Macias WL (2005) Drotrecogin alfa (activated) for adults with severe sepsis and a low risk of death. N Engl J Med 353:1332–1341
Mackenzie AF (2005) Activated protein C: Do more survive? Intensive Care Med 31:1624–1626
Carlet J (2006) Prescribing indications based on successful clinical trials in sepsis: a difficult exercise. Crit Care Med 34:525–529
Eichacker PQ, Danner RL, Suffredini AF, Cui X, Natanson C (2005) Reassessing recombinant human activated protein C for sepsis: time for a new randomized controlled trial. Crit Care Med 33:2426–2428
Hazell L, Shakir SAW (2006) Under-reporting of adverse drug reactions: a systematic review. Drug Safety 29:385–396
Vincent JL, Bernard GR, Beale R, Doig C, Putensen C, Dhainaut JF, Artigas A, Fumagalli R, Macias W, Wright T, Wong K, Sundin DP, Turlo MA, Janes J (2005) Drotrecogin alfa (activated) treatment in severe sepsis from the global open-label trial ENHANCE: further evidence for survival and safety and implications for early treatment. Crit Care Med 33:2266–2277
Steingrub J, Sanchez P, Zeckel M, Bates B, Qualy R (2003) Safety of drotrecogin alfa (activated): results of MERCURY, a retrospective multicenter observational study. Crit Care Med 31 (12 Suppl):A117
Cohen J, Guyatt G, Bernard GR, Calandra T, Cook D, Elbourne D, Marshall J, Nunn A, Opal S (2001) New strategies for clinical trials in patients with sepsis and septic shock. Crit Care Med 29:880–886
Acknowledgements
This study was funded by the Italian Medicines Agency of the Ministry of Health (AIFA – “Agenzia Italiana del Farmaco”) and carried out in collaboration with AIFA and the “Gruppo Italiano per la Valutazione degli Interventi in Terapia Intensiva” (GiViTI). GiViTI is the recipient of unconditioned grants from AstraZeneca Italy, Sanofi-Aventis Italy and Draeger Italia, none of which were involved in this study in any way. The authors substantially contributed to: conception and design (G. B., S. L., A. Ad., D. P.), analysis (G. B., C. R.) and interpretation (all authors) of data, the drafting (G. B., D. P.) or critical revision (C. R., S. L., A. Ad., A. Am.) of the article. All of them approved the final version of the manuscript. The full list of participating centres is given in the online supplement. G. Bertolini had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. GiViTI Steering Committee: N. Latronico, Brescia; M. Tavola, Lecco; D. Radrizzani, Legnano (MI); D. Giudici, M. Langer, A. Sicignano, Milan; M. Messina, Olbia; R. Tetamo, Palermo; P. Malacarne, Pisa; G. Bertolini, Ranica (BG); G. Nardi, Rome; S. Livigni, Torino; E. Nascimben, Treviso.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-007-0556-8
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Bertolini, G., Rossi, C., Anghileri, A. et al. Use of Drotrecogin alfa (activated) in Italian intensive care units: the results of a nationwide survey. Intensive Care Med 33, 426–434 (2007). https://doi.org/10.1007/s00134-007-0554-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0554-x