Abstract
Although surgical techniques pertaining to adult spinal deformity (ASD) have advanced over the last decade, proximal junctional kyphosis (PJK) is still a complication following surgery for ASD that continues to significantly challenge clinicians. This article aimed to report on the prevalence of PJK as well as enhance understanding of surgically modifiable and non-modifiable risk factors of PJK to guide management of this postoperative complication of ASD. As the understanding of the pathogenesis as well as surgical modifications aimed at reducing the incidence of PJK have advanced, so too should clinicians’ ability to implement more patient-specific operative plans and improve outcomes following realignment surgery for ASD.
Zusammenfassung
Obwohl sich die chirurgischen Techniken in Bezug auf die Behandlung von Wirbelsäulendeformitäten des Erwachsenen („adult spinal deformities“, ASD) in den letzten Dekaden weiterentwickelt haben, stellt die proximale junktionale Kyphose (PJK) als Komplikation nach operativer Versorgung der ASD eine große Herausforderung für den Wirbelsäulenchirurgen dar. Ziel dieser Übersichtsarbeit ist es, die Prävalenz der PJK darzustellen und das Verständnis für chirurgisch beeinflussbare sowie chirurgisch nicht beeinflussbare Risikofaktoren der PJK zu erhöhen, damit diese relevante postoperative Komplikation der ASD besser eingeordnet und behandelt werden kann. Da das Verständnis für die Pathogenese der PJK wie auch die chirurgischen Strategien mit dem Ziel, die Häufigkeit der postoperativen PJK zu reduzieren, fortgeschritten sind, muss nun auch die Fähigkeit der Kliniker gefordert werden, die patientenspezifische operative Planung in der Behandlung zu implementieren, um das postoperative Ergebnis nach der Wiederherstellung des sagittalen Profils bei ASD zu verbessern.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical realignment of adult spinal deformity (ASD) has advanced significantly over the last decade [17, 61, 64] but proximal junctional kyphosis (PJK) is a complication that continues to challenge clinicians [17, 59]. Proximal junctional kyphosis impacts health related quality of life and poses a socioeconomic burden, as evidenced by the 3.2 million US$ incurred by a major center, direct costs for revisions due to proximal junctional failure, a more severe and clinically relevant form of PJK [53, 55, 59, 68]. We aim to augment understanding and provide current evidence regarding prevalence and risk factors of PJK to guide clinicians in accounting for this postoperative phenomenon in the setting of ASD.
Epidemiology
Definition
Traditionally, PJK has been defined as a change of at least 10° in the proximal junctional sagittal Cobb angle from the preoperative value (Fig. 1). Most authors have radiographically identified PJK when observing a kyphosis of ≥10° develop between the inferior endplate of the upper instrumented vertebra (UIV) and the superior endplate of the two supra-adjacent vertebrae [32]. Recent efforts by Lafage et al. [40] to redefine the thresholds of proximal junctional pathologies call for expansion of radiographic PJK criteria. By also accounting for sagittal listhesis (from UIV to first supra-adjacent vertebra) and grouping by UIV (T8 and above; T9 and below), the new criteria were able to identify 20% of patients who underwent revision for proximal junctional pathologies (vs. 7% identified by classic criteria), enhancing the utility of radiographic PJK criteria for predicting future revision (Fig. 2; [40]).
Sagittal views of patients with radiographic proximal junctional kyphosis (PJK) at 1 and 2 years (Y; left and right, respectively) postoperatively. a A change in PJK of 3 ° from 1–2 years postoperatively in a patient who underwent revision surgery and was identified by redefined criteria accounting for sagittal listhesis. b A similarly small change in PJK of 2 ° from 1–2 years postoperatively evaluated per traditional criteria. Novel criteria, proposed by Lafage et al. [40], account for proximal junctional (PJ) angle between the UIV and UIV +2 (c) as well as sagittal listhesis (d). The new criteria groups patients into lower thoracic (UIV 3 mm and change in PJ listhesis >3 mm) or upper thoracic (UIV >T8 with PJ listhesis >8 mm and change in PJ listhesis >8 mm)
Incidence and prevalence
The incidence and prevalence rates of PJK are widely variable in the literature. Reported incidence rates range from 5% up to 61%, although many authors reported rates between 20% and 40% [9, 18, 21, 26, 57, 59]. Prevalence has been determined to fall between 29% [58] and 39% [36]. Gupta et al. [20] identified a bimodal incidence and temporal pattern of PJK. Early PJK, which manifests within 6 weeks of surgery, is associated with an increased likelihood of future revision and was found to have an incidence of 40.3%. In contrast, delayed PJK occurs more than 1 year following surgery and was found to have an incidence of 22% ([20]; Fig. 3).
A patient with delayed proximal junctional kyphosis (PJK) requiring multiple revision surgeries. Initial development of radiographic PJK following index surgery for adult spinal deformity (ASD) occurred 1 year postoperatively followed by revision surgery at 3 years postoperatively (from left to right)
Risk factors
While a variety of risk factors have been linked to the development of PJK in the literature, a simple method of stratifying these is by whether they are modifiable or non-modifiable by the surgeon.
Non-Modifiable/Patient-Specific Risk Factors
Age and magnitude of deformity
Older age at time of surgery is a well-documented risk factor associated with PJK and recent data suggest that patients older than 55 years are at increased risk of sustaining PJK [21, 36, 41, 46]; however, Lafage et al. [39] found that PJK in these patients is likely driven by sagittal plane overcorrection. In addition, preoperative presence of substantial sagittal malalignment and magnitude of deformity are also considered risk factors for PJK and proximal junctional failure. High preoperative sagittal vertical axis (SVA) and thoracic kyphosis are parameters of particular note [34, 65]. This emphasizes the necessity for patient-specific treatment, especially for older patients whose age and magnitude of deformity may require different alignment goals than younger patients [39].
Body mass index (BMI) and bone mineral density (BMD)
Strong consensus exists regarding the role of BMI in PJK onset [40, 41]. The underlying mechanism of progression to PJK may be related to the increased biomechanical stress placed on the UIV in patients with high BMIs [32]. At present, no investigation has quantified a BMI cut-off value at which PJK risk increases.
Multiple studies support low bone mineral density as a risk factor for PJK
Multiple studies also support the consideration of low bone mineral density (BMD) as a risk factor for PJK [32, 46]. With respect to bone quality, osteoporotic patients possess a weaker bone-to-screw interface, increasing the risk of screw pull-out post-instrumentation. The risk of adjacent segment disease following spinal fusion due to low BMD is well-documented. Osteoporosis is also associated with muscle atrophy and coupling lower BMD with reduced thoracolumbar musculature has the potential to cause skeletal instability and expedite development of PJK [32, 66].
Neuromuscular envelope
Fatty infiltration of the muscular envelope can contribute to the development of spino-pelvic muscular asymmetry and has been implicated in PJK development [2, 9]. Moal et al. [51] identified how patterns and mechanisms of fatty infiltration vary between muscle groups involved in sagittal posture; the greatest effects were on spine and hip extensors, which may promote sagittal spinopelvic malalignment in the setting of ASD and contribute to the development of PJK [27,28,29, 51]. In addition, Hyun et al. [24] demonstrated that PJK might result from reduced preoperative muscularity and increased fatty degeneration within the thoracolumbar musculature. Their findings strongly encourage spine surgeons to assess thoracolumbar muscularity and degree of fatty degeneration at the junctional area of the UIV of choice.
Comorbidities and risk stratification
The presence of comorbidities is a well-documented risk factor for PJK following ASD realignment surgery [7, 55, 70]. Diebo et al. [10] developed a novel index to quantify collective morbidity risk of ASD realignment surgery, utilizing preoperative comorbidities among several parameters from the Nationwide Inpatient Sample (NIS). Pulmonary circulation and neurological disorders, among others, were identified as contributors to ASD risk. Further study of the roles played by individual comorbidities in development of PJK is warranted. Such indices will help augment preoperative risk stratification for ASD patients. Frailty has also been reported to predispose to PJK. Miller et al. [50] created a deformity-specific frailty index (ASD-FI), clearly demonstrating the increased likelihood of PJK in patients with frailty and severe frailty (0.3–0.5; >0.5, respectively), offering surgeons another useful tool for treatment optimization. Leven et al. [45] showed how higher modified Frailty Index (mFI) scores correlated with increased postoperative complication and re-operation rates (mFI > 0.27, 60% and 15% respectively), validating mFI use for ASD patient risk stratification. Scheer et al. [59] developed a model that predicted either clinically significant PJK or proximal junction failure (PJF) with 86% accuracy. These tools may help surgeons to identify patients at risk for developing PJK/PJF in real-time in order to individualize risk-reduction approaches.
Risk stratification and mitigation of PJK is a top priority of ASD surgeons at present. In light of how the American College of Surgeons utilized the National Surgical Quality Improvement Program (NSQIP) database to generate a risk calculator, the Scoliosis Research Society (SRS) Risk Stratification Task Force is calling for strengthening of current risk stratification tools [16]. The 2016 SRS annual meeting dedicated a full day to a course aimed at identifying outcome predictors to improve care plans and optimizing cost-effectiveness of services provided [1]. Rigorous dual surgeon and multidisciplinary collaborative efforts in ASD during preoperative, perioperative, and postoperative phases has been demonstrated to produce substantial mitigation of perioperative complication rates [62]. The potential for these efforts to reduce PJK rates, enhance PJK prevention, and increase the standard of care appears promising.
Modifiable surgeon-controlled factors
Prevalent risk factors pertaining to surgical intervention include those related to operative approach, magnitude of sagittal realignment correction, and the characteristics of constructs.
Surgical approach
Several cadaver and biomechanical studies suggest that development of PJK is associated with posterior soft tissue and intervertebral elements disruption [34]. The combined anteroposterior approach has also been suggested as a risk factor for PJK [35, 55]; however, Liu et al. [46] have refuted this claim.
Sagittal realignment
Larger magnitude of deformity corrections is also associated with increased PJK incidence [55]. Multiple studies concluded that overcorrection of lumbar lordosis (LL) and SVA both contribute to PJK onset [33, 34, 47, 55]. Dubousset’s cone of economy helps explain this: sagittal alignment overcorrection disrupts the equilibrium between SVA and the natural line of gravity. The body tries to self-correct to an optimal position but is restricted to the remaining unfused segments following extensive fusion. This serves as the probable driving force behind the magnitude of reciprocal change in the proximal unfused thoracic spine, underscoring the importance of operative planning with respect to individual patient profiles [37]. Subsequently, the one-size-fits-all approach to determining realignment goals is ceding ground to patient-specific planning. Lafage et al. [39] adjusted for age and found that all age groups of patients who developed PJK demonstrated global alignment overcorrection, revealing a connection between overcorrection and PJK magnitude. Overcorrection was once favored for older patients to gradually counter alignment degeneration, yet it does not account for age and patient-specific alignment goals. Thus, more comprehensive preoperative planning may mitigate PJK risk and establish patient sustainable realignment [39].
The extent of correction can also modify PJK risk. Gupta et al. [20] found that in contrast to delayed PJK, patients with early PJK had a higher rate of upper lumbar apex corrections, with a lesser extent of caudal correction. Durrani et al. [12] also determined that risk of PJK is best mitigated following implementation of posterior dynamic stabilization at caudal-most levels. Another consideration in realignment surgery is comprehensive evaluation of parameters that contribute to sagittal malalignment [42]. Currently, full spine standing radiographs in the coronal and sagittal planes are the gold standard for assessing spinopelvic parameters and global alignment [3]; however, a significant proportion of the population spends the majority of their time at work in the sitting position [13, 15].
Larger magnitude of deformity corrections is also associated with increased PJK incidence
Therefore, assessment of sagittal trunk alignment cannot be restricted to standing posture only. Posture when sitting activates adaptive mechanisms that are modulated by pelvic incidence (PI) and that modify pelvic tilt (PT) and LL [42]. Endo et al. [13] showed how asymptomatic adults demonstrated nearly 50% reduction in LL angle and 285% increase in PT in the sitting position when compared to standing. Lee et al. [43] showed that not only did LL decrease as subjects went from standing to sitting, but these differences were more prominent in older subjects; specifically, these changes were highly concentrated in the lower lumbar region while sitting. Investigation of postural changes to the lumbar spine by Meakin et al. [48] showed small and non-significant changes in the lumbar spine shape between standing and supine positioning, yet they showed how the effect of positional change was markedly different for various spine shapes. Hey et al. [23] furthered explored this by radiographic evaluation of ROM, via sagittal global and segmental Cobb angles, in six common postures (slump sitting, forward bending, supine, half squatting, standing, and backward bending). They showed that lordosis persisted at L4–L5 and L5–S1 across all postures, and that L4–L5 had the greatest ROM among lumbar spinal functional units. Recently, Patel et al. [56] highlighted the superior performance of preoperative supine radiographs over standing radiographs for predicting alignment changes in unfused segments following thoracolumbar fusion for ASD. Evaluation of sagittal alignment in more than one position may provide a better understanding of the true flexibility of the spine, account for the patient’s daily activities that require positional changes and improve overall outcomes by allowing achievement of a more optimal postoperative alignment.
Junctional zone
The literature consistently reports that UIV selection at the thoracolumbar junction, specifically between T11 and L1, is associated with PJK. This is likely due to the transition from the more inflexible thoracic spine and ribs to the more mobile lumbar spine [32, 55]. Beyond this, in-depth knowledge of the implications of UIV selection is limited. Lafage et al. [38] confirmed a significantly increased rate and risk of PJK in patients with UIV at a lower thoracic level. They also identified another potential risk factor: further review of the UIV zone, while controlling for the compensatory impact of post-PJK increase in PT, revealed that patients who developed PJK demonstrated a more posterior construct inclination, suggesting that risk may decrease with suitable rod contouring [38]. The nature of the construct and instrumentation selected has also been examined. Utilization of hooks over pedicle screws has been associated with lower proximal junctional angle. Metzger et al. [49] concluded that placement of bilateral supralaminar hooks at the UIV was superior to all other hook and/or pedicle screw combinations, producing reduced hypermobility at the supra-adjacent noninstrumented segment. Han et al. [21] investigated spinal construct stiffness and found that cobalt chromium multi-rod constructs (CoCrMRC), in comparison to titanium two-rod constructs (TiTRCs), demonstrated improved rod stiffness, construct stability, and potential to reduce rod-breakage; however, increasing rod stiffness with CoCr MRCs increased the risk of PJK occurrence and impacted the time-frame within which PJK develops. Whereas TiTRC patients developed PJK between 2 and 84 months, all PJK cases related to CoCrMRC occurred within 7 postoperative months [21].
Disruption of the balance in forces at the junctional area is also thought to play a role in development of PJK. Utilizing finite element analysis, Bess et al. [4] demonstrated that the distribution of forces across and supra-adjacent to the UIV via posterior polyester tethers could allay the risk of PJF. Use of multilevel instrumented constructs with posterior tethers can produce a more gradual progression from instrumented to noninstrumented segments in ROM and forces on pedicle screws and posterior spinal ligaments, potentially mitigating the biomechanical risk of PJK.
Disruption of balance in forces at the junctional area is thought to play a role in PJK
A PJK related to the junctional zone is also frequently associated with vertebral compression fractures [8]. Kebaish et al. [31] demonstrated that a novel method of two-level prophylactic vertebroplasty (UIV + 1) substantially reduced incidence (17%) of vertebral compression fractures in cadaveric models, compared with no (100%) or one-level (67%) vertebroplasty. While cadaveric models preclude direct predictions of clinical PJK incidence, these findings warrant in vivo investigation. Theologis and Burch [67] evaluated two-level cement augmentation (UIV + 1) in patients with ASD, which yielded a significantly reduced revision rate for proximal junctional failure secondary to vertebral compression fracture. Moreover, they found an increased likelihood of revision surgery for PJK in patients undergoing no cement or any non-two-level cement augmentation technique (9.2-fold and 13.1-fold, respectively).
Clinical case presentation
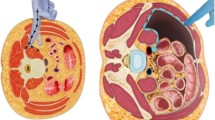
A 69-year-old female patient with osteopenia and 3 previous spinal surgeries was evaluated for PJK, reporting non-radiating back pain and a decline in activities of daily living (Fig. 4).
Preoperatively, the patient had developed a PJK angle of 34°, with evidence of severe sagittal malalignment (thoracic kyphosis [TK] of 25°, SVA of 215 mm, and pelvic incidence minus lumbar lordosis [PI-LL] of 72°). With advanced age and preoperative presence of significant sagittal malalignment, this patient has several risk factors for PJK and PJF (Fig. 5), as well as substantial fatty infiltration of the back musculature (Fig. 6).
Sagittal radiographic evaluation of the 69-year-old woman with radiographic proximal junctional kyphosis (PJK; blue circle) and severe sagittal malalignment (PI-LL = 72°). SVA sagittal vertical axis, TK thoracic kyphosis, LL lumbar lordosis; PI-LL pelvic incidence minus lumbar lordosis, PI pelvic incidence, PT pelvic tilt, SS sacral slope
Accounting for the age-adjusted goals of this older patient (age > 55 years) with severe sagittal malalignment (PI-LL = 72°), osteopenia, previous surgery, PJK (34°), and weak back musculature, she was indicated for a less ambitious, age-specific realignment. The patient underwent Ponte osteotomy at T12-L1 and L1-L2, with pedicle subtraction osteotomy at L3 and fusion from T5-S1 (Fig. 7).
The patient was observed to have no PJK and significant reduction in sagittal malalignment (PI-LL = 26° and SVA = 73 mm) 9 months postoperatively, demonstrating the clinical benefit of utilizing patient-specific planning in the context of PJK (Fig. 8).
Postoperative standing stereoradiography (9 months) of this 69-year-old patient following surgery, demonstrating resolution of proximal junctional kyphosis (PJK) and significant reduction in sagittal malalignment following age-adjusted goals for surgical correction (insert is close up view). SVA sagittal vertical axis, TK thoracic kyphosis, LL lumbar lordosis; PI-LL pelvic incidence minus lumbar lordosis, PI pelvic incidence, PT pelvic tilt, SS sacral slope
Future directions: what is next?
Further investigation into several preoperative dynamic patient factors may provide a novel framework within which surgeons can work with patients to reduce risk of PJK. Innovations in technology have allowed measurement of body kinematics, which previously required specialized equipment and laboratories, via wearable inertia sensors. Stabilometry, which relies on a single triaxial accelerometer, allows assessment of standing balance and has been widely used in patients with Parkinson’s disease. This demonstrated ability to detect postural abnormalities suggests potential for providing biofeedback on ASD patients undergoing realignment surgery [25].
Somatosensory, visual, and vestibular systems play a role in impacting erect postural alignment. Older adults with ASD have an impaired perception of upright vertical alignment that worsens with age-related impairment of proprioceptive and vibratory input from the lower extremities. Assessment of these impairments prior to surgical realignment procedures for ASD may provide a deeper understanding of patient needs and ability to maintain the new alignment [6, 19, 30, 60]. A practical method of assessing balance and sensory input in the setting of ASD is the new Dubousset Functional Test. Completing this series of four simple timed tests (5 min walk: from a sitting position, stand, walk 5 m forward and backward, and return to a seated position; Stairs: climb up and down 3 stairs; Squat: squat up and down; Telephone: walk while speaking on the phone) was found to be feasible and safe for ASD patients [69]. Lemay et al. [44] reported similar findings in patients with spinal cord injury utilizing the Mini-Balance Evaluation Systems Test (Mini BESTest), a 14-item shortened clinical outcome score used to assess dynamic balance. This assessment method includes items evaluating sensory inputs, underscoring their role in maintaining static postural balance. Other such studies have been carried out to evaluate the utility of performance-based tests in assessing changes in balance, posture, or sensory function and their impact on postural alignment. Dugailly et al. [11] demonstrated the utility of the head repositioning test (HRT) in tracking management and progression of proprioceptive cervical deficits in patients with and without neck pain. In comparing patients with and without chronic lower back pain, da Silva et al. [63] validated the use of balance assessment during one-legged and semi-tandem stance in identifying deficiency in postural control in patients with chronic lower back pain, potentially revealing a tool to guide balance re-training for clinicians. Gautschi et al. [14] and Hartmann et al. [22] used the Timed Up and Go (TUG) test in patients with lumbar degenerative disc disease, showing that the TUG test was a more sensitive and accurate tool for assessing the preoperative status and postoperative course than patient-reported outcomes, including the Visual Analog Scale (VAS) and EuroQol5D (EQ5D). Preoperative TUG test scores have been shown to predict the necessity of an assistive device 6 months following total hip arthroplasty [52], emphasizing the potential that such assessments may have in optimizing postoperative outcomes for patients with ASD. Moreover, current preoperative assessment and planning with respect to surgery for ASD is based on static radiographic imaging [5]. Lacking from the literature is a three-dimensional gait assessment of ASD patients preoperatively and postoperatively to identify dynamic factors related to the development of PJK. The kinematic and temporospatial data obtained could improve our understanding of the role of dynamic forces in the development of PJK and other complications following realignment surgery.
Conclusion
While surgical realignment for ASD has undergone significant advancement and improvement over the last decade, PJK remains a significant postoperative complication that challenges surgeons. In reviewing the literature, we have covered evidence-based discussion of prevalence and risk factors, both non-modifiable and surgeon-controlled. With an augmented understanding of all of the relevant factors in play, clinicians should be able to account for this phenomenon better and implement more patient-specific operative plans to optimize outcomes following realignment surgery for ASD.
Abbreviations
- ASD:
-
Adult spinal deformity
- ASD-FI:
-
Adult spinal deformity frailty index
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- CoCrMRC:
-
Cobalt chromium multi-rod construct
- HRT:
-
Head repositioning test
- LL:
-
Lumbar lordosis
- mFI:
-
Modified frailty index
- miniBESTest:
-
Mini-balance evaluation systems test
- NIS:
-
Nationwide Inpatient Sample
- NSQIP:
-
National surgical quality improvement program
- PI:
-
Pelvic incidence
- PI-LL:
-
Pelvic incidence minus lumbar lordosis
- PJF:
-
Proximal junction failure
- PJK:
-
Proximal junctional kyphosis
- PT:
-
Pelvic tilt
- ROM:
-
Range of motion
- SRA:
-
Scoliosis Research Society
- SVA:
-
Sagittal vertical axis
- TiTRC:
-
Titanium two-rod construct
- TK:
-
Thoracic kyphosis
- TUG test:
-
Timed Up and Go test
- UIV:
-
Upper instrumented vertebra
- VAS:
-
Visual analog scale
References
Scoliosis Research Society (2016) Final program. Scoliosis Research Society 51st Annual Meeting. Scoliosis Research Society, Prague
Amabile C, Moal B, Chtara OA et al (2016) Estimation of spinopelvic muscles’ volumes in young asymptomatic subjects: a quantitative analysis. Surg Radiol Anat 39:1–11
Bernstein P, Hentschel S, Platzek I et al (2012) The assessment of the postoperative spinal alignment: MRI adds up on accuracy. Eur Spine J 21:733–738
Bess S, Harris JE, Turner AWL et al (2016) The effect of posterior polyester tethers on the biomechanics of proximal junctional kyphosis: a finite element analysis. J Neurosurg Spine 26(1):125–133. https://doi.org/10.3171/2016.6.SPINE151477
Bess S, Protopsaltis TS, Lafage V et al (2016) Clinical and radiographic evaluation of adult spinal deformity. Clin Spine Surg 29:6–16
Bhagat S, Vozar V, Lutchman L et al (2013) Morbidity and mortality in adult spinal deformity surgery: Norwich Spinal Unit experience. Eur Spine J 22(Suppl 1):S42–S46
Cammarata M, Aubin C‑É, Wang X, Mac-Thiong J‑M (2014) Biomechanical risk factors for proximal junctional kyphosis: a detailed numerical analysis of surgical instrumentation variables. Spine (Phila Pa 1976) 39:E500–E507
DeWald CJ, Stanley T (2006) Instrumentation-related complications of multilevel fusions for adult spinal deformity patients over age 65: surgical considerations and treatment options in patients with poor bone quality. Spine (Phila Pa 1976) 31:S144–S151
Diebo BG, Henry J, Lafage V, Berjano P (2015) Sagittal deformities of the spine: factors influencing the outcomes and complications. Eur Spine J 24:3–15
Diebo BG, Jalai CM, Challier V et al (2017) Novel index to quantify the risk of surgery in the setting of adult spinal deformity: a study on 10,912 patients from the Nationwide Inpatient Sample. Clin Spine Surg 30(7):E993–E999. https://doi.org/10.1097/BSD.0000000000000509
Dugailly P‑M, De Santis R, Tits M et al (2015) Head repositioning accuracy in patients with neck pain and asymptomatic subjects: concurrent validity, influence of motion speed, motion direction and target distance. Eur Spine J 24:2885–2891
Durrani A, Jain V, Desai R et al (2012) Could junctional problems at the end of a long construct be addressed by providing a graduated reduction in stiffness? Spine (Phila Pa 1976) 37:E16–E22
Endo K, Suzuki H, Nishimura H et al (2012) Sagittal lumbar and pelvic alignment in the standing and sitting positions. J Orthop Sci 17:682–686
Gautschi OP, Corniola MV, Joswig H et al (2015) The timed up and go test for lumbar degenerative disc disease. J Clin Neurosci 22:1943–1948
Gelb DE, Lenke LG, Bridwell KH et al (1995) An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine (Phila Pa 1976) 20:1351–1358
Glassman SD (2016) Risk Stratification Task Force update. https://www.srs.org/newsletter/issues/march-2016/risk-stratification-task-force-update/full-article. Accessed 28 Apr 2017
Glassman SD, Coseo MP, Carreon LY (2016) Sagittal balance is more than just alignment: why PJK remains an unresolved problem. Scoliosis Spinal Disord 11:1. https://doi.org/10.1186/s13013-016-0064-0
Glattes RC, Bridwell KH, Lenke LG et al (2005) Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 30:1643–1649
Good CR, Auerbach JD, O’Leary PT, Schuler TC (2011) Adult spine deformity. Curr Rev Musculoskelet Med 4:159–167
Gupta MC, Diebo BG, Protopsaltis TS et al (2016) Bimodal incidence and causes of Proximal Junctional Kyphosis (PJK) in Adult Spinal Deformity (ASD). Spine J 16:327
Han S, Hyun S‑J, Kim K‑J et al (2017) Rod stiffness as a risk factor of proximal junctional kyphosis after adult spinal deformity surgery: comparative study between cobalt chrome multiple-rod constructs and titanium alloy two-rod constructs. Spine J 17(7):962–968
Hartmann S, Hegewald AA, Tschugg A et al (2016) Analysis of a performance-based functional test in comparison with the visual analog scale for postoperative outcome assessment after lumbar spondylodesis. Eur Spine J 25:1620–1626
Hey HWD, Lau ET-C, Tan K‑A et al (2017) Lumbar spine alignment in six common postures: an ROM analysis with implications for deformity correction. Spine (Phila Pa 1976) 42:1447–1455
Hyun S‑J, Kim YJ, Rhim S‑C (2016) Patients with proximal junctional kyphosis after stopping at thoracolumbar junction have lower muscularity, fatty degeneration at the thoracolumbar area. Spine J 16:1095–1101
Iosa M, Picerno P, Paolucci S, Morone G (2016) Wearable inertial sensors for human movement analysis. Expert Rev Med Devices 13:641–659
Jain A, Naef F, Lenke LG et al (2016) Incidence of proximal junctional kyphosis in patients with adult spinal deformity fused to the pelvis: analysis of 198 patients. Spine J 16:311–312
Jolivet E (2007) Modélisation biomécanique de la hanche dans le risque de fracture du fémur proximal. Arts et Métiers ParisTech, Paris (NNT: 2007ENAM0019)
Jolivet E, Daguet E, Pomero V et al (2008) Volumic patient-specific reconstruction of muscular system based on a reduced dataset of medical images. Comput Methods Biomech Biomed Engin 11:281–290
Jolivet E, Dion E, Rouch P et al (2014) Skeletal muscle segmentation from MRI dataset using a model-based approach. Comput Methods Biomech Biomed Eng Imaging Vis 2:138–145
Katzman WB, Wanek L, Shepherd JA, Sellmeyer DE (2010) Age-related hyperkyphosis: its causes, consequences, and management. J Orthop Sports Phys Ther 40:352–360
Kebaish KM, Martin CT, O’Brien JR et al (2013) Use of vertebroplasty to prevent proximal junctional fractures in adult deformity surgery: a biomechanical cadaveric study. Spine J 13:1897–1903
Kim DYK, Kim JY, Kim DYK et al (2017) Risk factors of proximal junctional kyphosis after multilevel fusion surgery: more than 2 years follow-up data. J Korean Neurosurg Soc 60:174–180
Kim HJ, Bridwell KH, Lenke LG et al (2014) Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine (Phila Pa 1976) 39:E576–E580
Kim HJ, Iyer S (2016) Proximal junctional kyphosis. J Am Acad Orthop Surg 24:318–326
Kim HJ, Yagi M, Nyugen J et al (2012) Combined anterior-posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis. Clin Orthop Relat Res 470:1633–1639
Kim YJ, Bridwell KH, Lenke LG et al (2008) Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976) 33:2179–2184
Lafage R, Bess S, Glassman S et al (2017) Virtual modeling of postoperative alignment after adult spinal deformity surgery helps predict associations between compensatory spinopelvic alignment changes, overcorrection, and proximal junctional kyphosis. Spine (Phila Pa 1976) 42:E1119–E1125
Lafage R, Line B, Liabaud B et al (2016) Orientation of the upper instrumented segment influences proximal junctional disease following Adult Spinal Deformity (ASD) surgery. Scoliosis Res. Soc, Prague, 21.–24.09.2016 Elsevier, Prague, p S356
Lafage R, Schwab F, Glassman S et al (2017) Age-adjusted alignment goals have the potential to reduce PJK. Spine (Phila Pa 1976) 42:1275–1282
Lafage R, Schwab FJ, Bess S et al (2015) Redefining radiographic thresholds for junctional kyphosis pathologies. Spine J 15:216
Lau D, Clark AJ, Scheer JK et al (2014) Proximal junctional kyphosis and failure following spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976) 39:2093–2102
Lazennec JY, Brusson A, Rousseau MA (2013) Lumbar-pelvic-femoral balance on sitting and standing lateral radiographs. Orthop Traumatol Surg Res 99:S87–S103
Lee ES, Ko CW, Suh SW et al (2014) The effect of age on sagittal plane profile of the lumbar spine according to standing, supine, and various sitting positions. J Orthop Surg Res 9:11. https://doi.org/10.1186/1749-799X-9-11
Lemay J‑F, Gagnon D, Duclos C et al (2013) Influence of visual inputs on quasi-static standing postural steadiness in individuals with spinal cord injury. Gait Posture 38:357–360
Leven DM, Lee NJ, Kothari P et al (2016) Frailty index is a significant predictor of complications and mortality after surgery for adult spinal deformity. Spine (Phila Pa 1976) 41:E1394–E1401
Liu F‑Y, Wang T, Yang S‑D et al (2016) Incidence and risk factors for proximal junctional kyphosis: a meta-analysis. Eur Spine J 25:2376–2383
Maruo K, Ha Y, Inoue S et al (2013) Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976) 38:E1469–E1476
Meakin JR, Gregory JS, Aspden RM et al (2009) The intrinsic shape of the human lumbar spine in the supine, standing and sitting postures: characterization using an active shape model. J Anat 215:206–211
Metzger MF, Robinson ST, Svet MT et al (2016) Biomechanical analysis of the proximal adjacent segment after multilevel instrumentation of the thoracic spine: do hooks ease the transition? Global Spine J 6:335–343
Miller E, Jain A, Daniels AH et al (2016) Assessment of a novel Adult Spinal Deformity (ASD) Frailty Index (ASD-FI) to assist with risk stratification for ASD surgery. Spine J 16:365
Moal B, Bronsard N, Raya JG et al (2015) Volume and fat infiltration of spino-pelvic musculature in adults with spinal deformity. World J Orthop 6:727–737
Nankaku M, Tsuboyama T, Akiyama H et al (2013) Preoperative prediction of ambulatory status at 6 months after total hip arthroplasty. Phys Ther 93:88–93
Nguyen NLM, Kong CY, Hart RA (2016) Proximal junctional kyphosis and failure—diagnosis, prevention, and treatment. Curr Rev Musculoskelet Med 9:299–308
O’Leary PT, Bridwell KH, Lenke LG et al (2009) Risk factors and outcomes for catastrophic failures at the top of long pedicle screw constructs: a matched cohort analysis performed at a single center. Spine (Phila Pa 1976) 34:2134–2139
Park S‑J, Lee C‑S, Chung S‑S et al (2017) Different risk factors of proximal junctional kyphosis and proximal junctional failure following long instrumented fusion to the sacrum for adult spinal deformity: survivorship analysis of 160 patients. Neurosurgery 80:279–286
Patel A, Varghese J, Liabaud B et al (2016) Supine radiographs outperform standing radiographs in predicting postoperative alignment of unfused thoracic segments. Spine J 16:370–371
Paternostre F, Charles YP, Sauleau EA, Steib J‑P (2017) Cervical sagittal alignment in adult hyperkyphosis treated by posterior instrumentation and in situ bending. Orthop Traumatol Surg Res 103:53–59
Protopsaltis T, Bronsard N, Soroceanu A et al (2017) Cervical sagittal deformity develops after PJK in adult thoracolumbar deformity correction: radiographic analysis utilizing a novel global sagittal angular parameter, the CTPA. Eur Spine J 26:1111–1120
Scheer JK, Osorio JA, Smith JS et al (2016) Development of validated computer based pre-operative predictive model for Proximal Junction Failure (PJF) or clinically significant PJK with 86 % accuracy based on 510 ASD patients with 2‑year follow-up. Spine (Phila Pa 1976) 41:1–10
Schwab FJ, Hawkinson N, Lafage V et al (2012) Risk factors for major peri-operative complications in adult spinal deformity surgery: a multi-center review of 953 consecutive patients. Eur Spine J 21:2603–2610
Schwab FJ, Lafage V, Farcy JP et al (2008) Predicting outcome and complications in the surgical treatment of adult scoliosis. Spine (Phila Pa 1976) 33:2243–2247
Sethi RK, Pong RP, Leveque J‑C et al (2014) The Seattle Spine Team approach to adult deformity surgery: a systems-based approach to perioperative care and subsequent reduction in perioperative complication rates. Spine Deform 2:95–103
da Silva RA, Vieira ER, Fernandes KBP et al (2017) People with chronic low back pain have poorer balance than controls in challenging tasks. Disabil Rehabil 10:1–7. https://doi.org/10.1080/09638288.2017.1294627
Smith JS, Shaffrey CI, Berven S et al (2009) Operative versus nonoperative treatment of leg pain in adults with scoliosis: a retrospective review of a prospective multicenter database with two-year follow-up. Spine (Phila Pa 1976) 34:1693–1698
Smith MW, Annis P, Lawrence BD et al (2013) Early proximal junctional failure in patients with preoperative sagittal imbalance. Evid Based Spine Care J 4:163–164
Terracciano C, Celi M, Lecce D et al (2013) Differential features of muscle fiber atrophy in osteoporosis and osteoarthritis. Osteoporos Int 24:1095–1100
Theologis AA, Burch S (2015) Prevention of acute proximal junctional fractures after long thoracolumbar posterior fusions for adult spinal deformity using 2‑level cement augmentation at the upper instrumented vertebra and the vertebra 1 level proximal to the upper instrumented verteb. Spine (Phila Pa 1976) 40:1516–1526
Theologis AA, Miller L, Callahan M et al (2016) The economic impact of revision surgery for proximal junctional failure after adult spinal deformity surgery. Spine (Phila Pa 1976) 41(16):E964–72
Challier V, Boissiere L, Diebo BG, Lafage V, Lafage R, Castelain JE, Ghailane S, Bouloussa, Obeid I, Gille O (2017) The Dubousset Functional Test: Introducing a new Assessment to Evaluate multi-modal Balance in the setting of Adult Spine Deformity. Unpubl. Data
Watanabe K, Lenke LG, Bridwell KH et al (2010) Proximal junctional vertebral fracture in adults after spinal deformity surgery using pedicle screw constructs: analysis of morphological features. Spine (Phila Pa 1976) 35:138–145
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C.B. Paulino is a paid presenter or speaker for DePuy, A Johnson & Johnson Company. F.J. Schwab receives research support from DePuy, is a paid consultant, presenter or speaker for K2M, Medicrea, Medtronic, Medtronic Sofamor Danek, Nuvasive, and Zimmer, owns stock or stock options in Nemaris INC, and is a board or committee member of the Scoliosis Research Society, Spine Deformity, and International Spine Society Group (Vice President). V. Lafage is a paid presenter or speaker for DePuy and Medtronic, receives research support from DePuy, is a board or committee member of the International Spine Study Group, Scoliosis Research Society, and Nemaris INC, and owns stock or stock options in Nemaris INC. B.G. Diebo, N.V. Shah and S.G. Stroud declare that they have no competing interests.
This article represents a review of the literature, including original studies of human or animal subjects performed by their respective authors, in order to complete this article. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Where applicable, informed consent was obtained from all individual participants included in the respective studies.
Rights and permissions
About this article
Cite this article
Diebo, B.G., Shah, N.V., Stroud, S.G. et al. Realignment surgery in adult spinal deformity. Orthopäde 47, 301–309 (2018). https://doi.org/10.1007/s00132-018-3536-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00132-018-3536-5