Abstract
Purpose
The objective of the current study was to quantify the extent to which Australia’s tertiary students have reported poorer mental health in comparison with the general community between 2001 and 2017.
Methods
Data were derived from the Household, Income and Labour Dynamics in Australia Survey, a longitudinal household-based panel study. There were 29,124 participants who provided at least one observation over the study period. On average, participants provided 7.4 observations. Mental Health was assessed with the SF-36 mental health and vitality subscales.
Results
There was little evidence for differences in mental health and vitality between those studying at tertiary levels and those not in tertiary education. Age-stratified analyses revealed that any differences were reported by older students. Interactions between education level and time revealed that the association between tertiary study and mental health outcomes has been consistent over time.
Conclusion
There were very few differences between those in and those not in tertiary education. The magnitude of any differences was very small and does not necessarily reflect substantial poor mental health outcome. Overall, the most consistent finding was that there was little risk for poor mental health outcomes attributed to tertiary study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most mental illnesses have their genesis in late adolescence and early adulthood [1, 2]. Consequently, particular concern has been raised regarding the risk of poor mental health outcomes for young adults enrolled in tertiary-level education. The mental health of tertiary students is a public health issue that has been receiving increasing attention in Australia and worldwide [3,4,5,6,7,8,9,10,11,12]. Rates of high or very high psychological distress are commonly reported to be 3–5 times higher than the general population [3, 4]. In Australia, the joint Headspace and National University of Student’s (NUS) Wellbeing Survey of 2016 [13], reported that 65% of university student respondents, aged 18–25 years, reported high or very high psychological distress, with slightly lower levels of distress reported by older tertiary students aged 26 + . These estimates far exceeded those expected in the Australian population, estimated at approximately 15.6%, for young adults [14]. Students enrolled in particular disciplines, such as medicine, appear to be at higher risk, with rates of depression, anxiety and general psychological distress ranging from 6 to 96.7% [15, 16]. Increasing demands for university health and counselling services vary between institutions [17,18,19], but is also provided as indirect evidence for increasing mental ill health burden among tertiary students.
In contrast to these findings, there is a growing body of evidence that despite reports of increasing demand for health and counselling services, students may not necessarily be at higher risk of psychological distress in comparison to their non-tertiary peers. In Australia, a cross-sectional analysis of 3 large national surveys [e.g., the 2007 Household, Income and Labour Dynamic in Australia (HILDA) survey, the 2007–2008 National Health Survey (NHS), and the 2007 National Survey of Mental Health and Wellbeing (NSMHWB)] revealed no difference in high distress between tertiary and non-tertiary students whilst differences in prevalence in moderate distress were attenuated when rates were age- and sex-standardized [20] and other studies have concluded that tertiary-level students are either at no increased risk for poorer mental health in comparison to their non-student peers [21] or indeed report better mental health outcomes in contrast to the population [22]. Relatedly, tertiary students are not an increased risk for suicide or self-harm, at least in two higher-status UK tertiary institutions [23, 24].
Inconsistencies in the research findings may be due to methodological limitations of the studies and data available. Often, arguments for the high prevalence of mental health issues amongst tertiary student populations are based on the findings of studies from convenience or self-selecting samples, often at a single institution, which limits appropriate generalisation to the broader student population [8]. Many findings are drawn from cross-sectional studies [8, 10, 12, 15]. In Australia, the 2016 NUS Wellbeing Survey [13] is one of the only dedicated national surveys of mental health and wellbeing of tertiary students in Australia, but the recruitment method involved social media from Headspace (a service provider), and student union representatives at Australian universities and TAFEs who used a combination of posters, events and word-of-mouth to advertise the survey. This resulted in a sample likely not reflective of the broader student population. For example, in addition to the overly high estimates of distress previously mentioned, 26.7% of the sample identified as LGBTQ, a rate far higher than the 3.2% reported in the 2016 survey of the adult population [25]. A further limitation is that much of the existing research is cross-sectional in design and precludes examination of changes in mental health burden within the same individuals over time. While these limitations are often acknowledged, the consequences are reflected by likely inaccurate reflections of the true extent of mental illness burden. Indeed, one study utilised a small sample of young Bachelor students and their age-matched peers from the HILDA study and assessed their trajectories as they entered and left tertiary study; bachelor students typically reported better mental health than their peers although they did appear to report declines as they entered tertiary study [26].
Given the inconsistencies and limitations noted, there is a need for further detailed examination to establish (1) the increased risk of poor mental health outcomes for tertiary-level students and (2) whether this purported risk has increased over time. The present study utilises a large representative sample of Australian students drawn from the HILDA study, a nationally representative longitudinal study of Australian households, and currently provides mental health data over a 17-year period to examine the mental health of tertiary students.
Method
Participants
Participants were from the Household, Income and Labour Dynamics in Australia (HILDA) Survey [27]. HILDA is a longitudinal household panel survey that has been conducted annually since 2001. At baseline, there were 7682 sampled households resulting in interviews with 13, 969 individual participants. Participants were identified through a multi-stage area-based sample design which included a random sample of 488 census districts across Australia. Within each district, 25% of private dwellings were invited to participate; 66% of households responded to the invitation to participate [27, 28]. Participants were interviewed in their own homes by trained interviewers. Over time, new participants entered the study as they entered the household or through top-up samples introduced to address attrition. Results in this paper reflect responses of participants (N = 21,280) who provided at least one observation on the relevant measures over the 17 years of data provided by each household member aged 15 and older via both personal interview and self-completion questionnaire.
Measures
Mental health and vitality
Mental Health (Cronbach Alpha = 0.82) and Vitality (Cronbach Alpha = 0.83) were operationalised by the Mental Health Index and Vitality subscales of the Short-Form Health Survey-36 (SF-36) [29] which has been validated in HILDA [30]. The Mental Health Index subscale (MHI-5) has been used in epidemiological studies as an indicator of psychological distress [31,32,33,34] and comprises five items including, ‘Been a nervous person’, ‘Felt so down in the dumps nothing could cheer you up’, ‘Felt calm and Peaceful’, ‘Felt down’, ‘Been a happy person’. The vitality subscale comprises four items including, ‘Feel full of life’, ‘Have a lot of energy’, ‘Felt worn out’, ‘Felt tired’. Vitality has been operationalised as an indicator of positive psychological wellbeing and functioning including self-esteem, intrinsic motivation and mindfulness [35,36,37], and is negatively related to depression, anxiety, and a range of physical health conditions including cardiovascular disease, diabetes, hypertension, falls and mortality risk [38,39,40,41,42,43,44,45,46,47,48]. For both the vitality and mental health subscales, participants reported the extent to which they experienced each statement on a 6-point Likert-type scale, ranging from ‘0’ ‘None of the Time’ to ‘6’ ‘All of the Time’, over the last 4 weeks. Both the vitality and mental health were positively scaled so that higher scores reflected higher levels of vitality and mental health (i.e., low levels of mental ill health).
Tertiary education level
At each wave, level of tertiary education currently being studied was derived from items that asked which qualification respondents were undertaking and coded into ‘Bachelor’, ‘Honours’, ‘Graduate Diploma/Certificate’, ‘Master’, and ‘PhD’ with all other participants grouped into the reference category ‘Not in Tertiary Education.
Covariates
Covariates included current age in years, sex (male/female) and time comprised a binary variable which reflected change over the 17-year study period. All measures were included in all waves of the HILDA.
Statistical analysis
All analyses were undertaken in STATA SE v.15 [49]. Analyses were undertaken with a multi-level linear regression. The analyses derive maximum likelihood estimates and standard error which are adjusted for the clustering of repeated observations within individuals who were followed over time. Due to potential confounding between age and educational level, analyses were re-estimated and stratified by age group categorised as < 26 years and ≥ 26 years. Analyses were estimated with dependent variables in their unstandardized scale, but were then re-estimated with a Z-score standardisation (standardized to each scale’s grand mean) to derive a measure of effect size where the Z-score reflects an effect size in standard deviation terms, where small (d = 0.20), medium (d = 0.40) and large (d = 0.60) effect sizes corresponded with changes of 2 points for small effect sizes, 4 points for medium effect sizes and 8 points for large effect sizes on the mental health measures. In line with recommend practice [50], we report exact significance values and emphasise groups differences in terms of the magnitude of the effect sizes reported.
Results
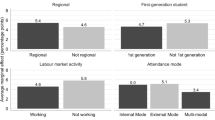
The distribution of socio-demographic and mental health variables of the HILDA sample over the 17 years and stratified by age, are reported in Table 1. These distributions are reported by tertiary level and non-tertiary groups in Table 2 and suggest tertiary students in the HILDA sample are reflective of the general population. For example, the proportion of younger adults engaging with tertiary study is a rate that is consistent with other Australia data.
Overall, there were few associations between tertiary levels and the mental health outcomes (Tables 1, 2). All tertiary students except for PhD students reported lower SF 36 Mental Health (Table 1) although the size of these effects was very small and ranged from a − 0.02 SD (SE = 0.01) to − 0.08 SD (SE = 0.02) for those enrolled in Bachelor and Master degrees, respectively. Lower vitality (Table 2) was reported by those enrolled in Graduate Diploma/Certificate and Master’s degrees, but again, the size of these effects was only of a small magnitude between − 0.05 SD (SE = 0.02) and − 0.06 SD (SE = 0.02).
As age may confound the purported risk of education levels for mental health, the analyses were re-estimated by stratifying the analyses by age groups, dichotomising age into young adulthood (< 26 years) and others (≥ 26 years). Results of these stratified analyses revealed that the risk for low mental health was only reported for those aged ≥ 26 years (see Table 1) and was only reported for those enrolled in Graduate Diploma/Certificate and Master’s degrees. Again, these effects were of only small magnitude ranging in effect size from − 0.06 SD (SE = 0.02) to − 0.07 SD (SE = 0.02), respectively. The lower mental health identified in the overall sample for those in Bachelor and Honours levels was not reflected in either of the age groups and suggests the differences reported in the main analyses reflects the increased power of the main analyses. Therefore, we would emphasise to readers the magnitude of effect sizes which suggests that any differences between groups are only of a very small magnitude. Similar patterns were reported for vitality (see Table 2) with only those aged ≥ 26 years enrolled in Graduate Diploma/Certificates reporting lower vitality, but again the size of effect was of only of a very small magnitude [− 0.06 SD (SE = 0.02)].
Finally, changes in the risk attributed to tertiary education level over time were examined and are reported in a second step in both Tables 3 and 4. Interactions between tertiary level and time revealed no change in the risk attributed to tertiary education levels over the 17 years for both mental health or vitality.
Discussion
The objective of the current study was to examine and quantify differences in mental health and vitality between Australia’s tertiary students and those in the general community not enrolled in tertiary education, and to examine changes over time. The study comprised representative data of the Australian population between 2001 and 2017. Overall, there was little evidence for poorer mental health for those individuals who reported studying at a tertiary level of education in comparison with those who were not. The relative magnitude of any differences was very small. Perhaps the most notable difference reported was on the SF-36 mental health scale for those undertaking Master’s level studies. However, it is important to emphasise that this purported risk reflects only a 1.4-point difference on the SF-36 mental health scale; the corresponding standardized effect size was very small.
Our findings confirm earlier analyses [20, 26]. Analyses of the mental health trajectories of young Bachelor students over the first 11 years of HILDA in comparison with their age-matched peers, revealed that young Bachelor students typically report better mental health [26]. The current study extends these findings and has several advantages over other reports on the mental health of tertiary students, particularly in Australia. First, these findings draw on 17 years of data from the HILDA study which is representative of the Australian population since 2001. Second, the study is itself not specifically a health study. Health is a secondary outcome and unlikely to be biased by self-selection which likely confounds the findings of many existing studies into the mental health of tertiary students. Third, rates of psychological distress in the current study correspond with other national estimates of high or very high psychological distress [14]. As noted above, a criticism of other research on the health of Australia’s tertiary students is that samples are not reflective of the broader student population and are likely biased by self-selection in recruitment methods. Therefore, in contrast to research reporting greater psychological distress and poorer mental health amongst university students in particular [3, 4, 13], the present study offers compelling evidence of comparable mental health outcomes between those in and out of tertiary education and no evidence of increasing mental ill-health burden. We do recognise, however, that these findings are specific to the Australian context since the turn of the 21st Century, and it is important for other national jurisdictions to more closely examine the longitudinal patterns of psychological distress and to quantify the extent to which tertiary students are at comparable, increased or lower risk.
Two main messages are worth emphasising. First, it is clear that Australian tertiary students are not necessarily at increased risk for poorer mental health in comparison with the population. Where tertiary students reported poorer outcomes, the magnitude of these effects was much less than other known risk factors, such as the differences reported between sex even in this study. Second, in most instances, there has been no change in the mental health of Australia’s’ tertiary students over the last 17 years. The question then needs to be asked, how are these results to be reconciled with the increase in need for mental health services, reported by both community and university service providers [5]? We would propose that the purported increase in service demand does not necessarily reflect an increase in need in the tertiary student population, but perhaps rather reflects an increase in the willingness and acceptance of the tertiary student population to seek help. We would also hypothesise that whilst a number of reports highlight increased ‘stress’ and ‘low-wellbeing’, this does not necessarily correspond to increases in psychological distress or mental illness. Consequently, we believe it is important for the tertiary sector to recognise that increased need for service provision should not be confused with an increase in burden. Rather there may be simply greater acceptance for those in need to seek support.
If acceptance of help-seeking behaviour is improving, it is vital that appropriate support services are available. As noted, concerns for the increasing demand and capacity of student counselling to meet student need have been raised internationally [17,18,19, 51, 52]. To help alleviate the pressures on existing services, alternative approaches to support mental health should be considered to support students. For example, The World Health Organization World Mental Health International College Student initiative is currently examining evidence-based interventions for the presentation and treatment of mental health concerns amongst tertiary students, with a focus on internet-based approaches [53]. Internet-based interventions for university students are increasing and have found small effects for improving mental health [54]. Supporting diverse avenues for student support also helps to address noted barriers to seeking help for mental health concerns, including issues of affordability and concerns regarding stigma and confidentiality [55, 56].
It is also vital to emphasise the importance of support service provision for students, even if they are for stress and low wellbeing rather than mental illness. It is well known that for many people, psychiatric illness typically has its onset in young adulthood, and higher education providers need to ensure they have sufficient prevention strategies and structures in place should those who are most vulnerable to mental illness have access to support services. However, it is important to emphasise that enrolling in a tertiary-level education program is not a risk in and of itself. It is possible that the demands of tertiary study can act as a catalyst for the development of ill-health in some, but in all likelihood, other contexts could also be a factor in the development of mental health outcomes.
Furthermore, since those not enrolled in tertiary education reported comparable mental health, it does emphasise the need for whole-of-community-based approaches to address the mental health of tertiary and non-tertiary populations. However, perhaps rather than current practice where individual tertiary institutions appear to be developing their own approaches to dealing with mental ill-health, a more effective strategy would be for community health services to be embedded within the tertiary sector to allow for greater ease of access to service provision. This requires greater collaboration between public health and tertiary education sectors. But rather than the development of institution-based services, rather institutions could in themselves act as a conduit for public health services. Certainly, improving links between university services and external mental health provides, and awareness of external support services available to students has been recommended in other recent research [57]. We also recognise that the current study is specific to an Australian context and these recommendations may not necessarily be appropriate to other national jurisdictions.
In conclusion, utilising 17 years of data, we have found no evidence to suggest tertiary students are at an increased risk of poor mental health relative to their community peers, and no indication of increasing mental health issues over time. However, in acknowledgement of the distress reported, and in support of other research highlighting the demand on university counselling services, we emphasise the continued need to ensure the provision of appropriate support services for students. Future research and practice should seek to consider the efficacy of supporting current services with alternative approaches support students in higher education, including online interventions.
References
Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustun TB (2007) Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry 20(4):359–364. https://doi.org/10.1097/YCO.0b013e32816ebc8c
Slade T, Johnston A, Oakley Browne MA, Andrews G, Whiteford H (2009) 2007 national survey of mental health and wellbeing: methods and key findings. Aust N Z J Psychiatry 43(7):594–605. https://doi.org/10.1080/00048670902970882
Leahy CM, Peterson RF, Wilson IG, Newbury JW, Tonkin AL, Turnbull D (2010) Distress levels and self-reported treatment rates for medicine, law, psychology and mechanical engineering tertiary students: cross-sectional study. Aust N Z J Psychiatry 44(7):608–615. https://doi.org/10.3109/00048671003649052
Stallman HM (2010) Psychological distress in university students: a comparison with general population data. Aust Psychol 45(4):249–257. https://doi.org/10.1080/00050067.2010.482109
Vivekananda K, Telley A, Trethowan S (2011) A five year study on psychological distress within a university counselling population. J Aust N Z Stud Serv Assoc 37:39–57
Auerbach RP, Alonso J, Axinn WG, Cuijpers P, Ebert DD, Green JG, Hwang I, Kessler RC, Liu H, Mortier P, Nock MK, Pinder-Amaker S, Sampson NA, Aguilar-Gaxiola S, Al-Hamzawi A, Andrade LH, Benjet C, Caldas-de-Almeida JM, Demyttenaere K, Florescu S, de Girolamo G, Gureje O, Haro JM, Karam EG, Kiejna A, Kovess-Masfety V, Lee S, McGrath JJ, O’Neill S, Pennell BE, Scott K, Ten Have M, Torres Y, Zaslavsky AM, Zarkov Z, Bruffaerts R (2016) Mental disorders among college students in the World Health Organization World Mental Health Surveys. Psychol Med 46(14):2955–2970. https://doi.org/10.1017/s0033291716001665
Bayram N, Bilgel N (2008) The prevalence and socio-demographic correlations of depression, anxiety and stress among a group of university students. Soc Psychiatry Psychiatr Epidemiol 43(8):667–672. https://doi.org/10.1007/s00127-008-0345-x
Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C (2013) A systematic review of studies of depression prevalence in university students. J Psychiatr Res 47(3):391–400. https://doi.org/10.1016/j.jpsychires.2012.11.015
Stewart-Brown S, Evans J, Patterson J, Petersen S, Doll H, Balding J, Regis D (2000) The health of students in institutes of higher education: an important and neglected public health problem? J Public Health Med 22(4):492–499
Adewuya AO, Ola BA, Aloba OO, Mapayi BM, Oginni OO (2006) Depression amongst Nigerian university students. Soc Psychiatry Psychiatr Epidemiol 41(8):674–678. https://doi.org/10.1007/s00127-006-0068-9
Tong J, Miao S, Wang J, Yang F, Lai H, Zhang C, Zhang Y, Hsu LK (2014) A two-stage epidemiologic study on prevalence of eating disorders in female university students in Wuhan, China. Soc Psychiatry Psychiatr Epidemiol 49(3):499–505. https://doi.org/10.1007/s00127-013-0694-y
Verger P, Combes J-B, Kovess-Masfety V, Choquet M, Guagliardo V, Rouillon F, Peretti-Wattel P (2009) Psychological distress in first year university students: socioeconomic and academic stressors, mastery and social support in young men and women. Soc Psychiatry Psychiatr Epidemiol 44(8):643–650. https://doi.org/10.1007/s00127-008-0486-y
Rickwood D, Telford N, O’Sullivan S, Crisp D, Magyar R (2017) National tertiary student wellbeing survey 2016. Headspace & National Union of Students
(ABS) ABoS (2015) Psychological distress .4364.0.55.001—national health survey: first results, 2014–15. Commonwealth of Australia, Canberra
Hope V, Henderson M (2014) Medical student depression, anxiety and distress outside North America: a systematic review. Med Educ 48(10):963–979. https://doi.org/10.1111/medu.12512
Mata DA, Ramos MA, Bansal N, Khan R, Guille C, Di Angelantonio E, Sen S (2015) Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. J Am Med Assoc 314(22):2373–2383. https://doi.org/10.1001/jama.2015.15845
Brown J (2018) Student mental health: some answers and more questions AU—Brown, June S. L. J Ment Health 27(3):193–196. https://doi.org/10.1080/09638237.2018.1470319
Eisenberg D, Hunt J, Speer N, Zivin K (2011) Mental health service utilization among college students in the United States. J Nerv Ment Dis 199(5):301–308. https://doi.org/10.1097/NMD.0b013e3182175123
Voelker R (2003) Mounting student depression taxing campus mental health services. J Am Med Assoc 289(16):2055–2056. https://doi.org/10.1001/jama.289.16.2055
Cvetkovski S, Reavley NJ, Jorm AF (2012) The prevalence and correlates of psychological distress in Australian tertiary students compared to their community peers. Aust N Z J Psychiatry 46(5):457–467. https://doi.org/10.1177/0004867411435290
Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu SM, Olfson M (2008) Mental health of college students and their non-college-attending peers: results from the National Epidemiologic Study on Alcohol and Related Conditions. Arch Gen Psychiatry 65(12):1429–1437. https://doi.org/10.1001/archpsyc.65.12.1429
Sarmento M (2015) A “mental health profile” of higher education students. Proced Soc Behav Sci 191:12–20. https://doi.org/10.1016/j.sbspro.2015.04.606
Hawton K, Bergen H, Mahadevan S, Casey D, Simkin S (2012) Suicide and deliberate self-harm in Oxford University students over a 30-year period. Soc Psychiatry Psychiatr Epidemiol 47(1):43–51. https://doi.org/10.1007/s00127-010-0310-3
Collins IP, Paykel ES (2000) Suicide amongst Cambridge University Students 1970–1996. Soc Psychiatry Psychiatr Epidemiol 35(3):128–132. https://doi.org/10.1007/s001270050195
Wilson T, Shalley F (2018) Estimates of Australia’s non-heterosexual population. Aust Popul Stud 2(1):2018
Cvetkovski S, Jorm AF, Mackinnon AJ (2019) An analysis of the mental health trajectories of university students compared to their community peers using a national longitudinal survey. Stud Higher Educ 44(1):185–200. https://doi.org/10.1080/03075079.2017.1356281
Wooden M, Watson N (2007) The HILDA survey and its contribution to economic and social research (so far). Econ Rec 83(261):208–231. https://doi.org/10.1111/j.1475-4932.2007.00395.x
Wooden M, Warren D (2004) Non-standard employment and job satisfaction: evidence from the Hilda Survey. J Ind Relat 46(3):275–297. https://doi.org/10.1111/j.0022-1856.2004.00142.x
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6):473–483
Butterworth P, Crosier T (2004) The validity of the SF-36 in an Australian National Household Survey: demonstrating the applicability of the Household Income and Labour Dynamics in Australia (HILDA) Survey to examination of health inequalities. BMC Public Health 4:44. https://doi.org/10.1186/1471-2458-4-44
Rumpf HJ, Meyer C, Hapke U, John U (2001) Screening for mental health: validity of the MHI-5 using DSM-IV Axis I psychiatric disorders as gold standard. Psychiatry Res 105(3):243–253
Yamazaki S, Fukuhara S, Green J (2005) Usefulness of five-item and three-item Mental Health Inventories to screen for depressive symptoms in the general population of Japan. Health Qual Life Outcomes 3:48. https://doi.org/10.1186/1477-7525-3-48
Skapinakis P, Lewis G, Araya R, Jones K, Williams G (2005) Mental health inequalities in Wales, UK: multi-level investigation of the effect of area deprivation. Br J Psychiatry 186:417–422
Gill SC, Butterworth P, Rodgers B, Anstey KJ, Villamil E, Melzer D (2006) Mental health and the timing of men’s retirement. Soc Psychiatry Psychiatr Epidemiol 41(7):515–522. https://doi.org/10.1007/s00127-006-0064-0
Huppert FA, Marks N, Clark A, Siegrist J, Stutzer A, Vittersø J, Wahrendorf M (2009) measuring well-being across Europe: description of the ESS well-being module and preliminary findings. Soc Indic Res 91(3):301–315. https://doi.org/10.1007/s11205-008-9346-0
Kasser T, Ryan RM (1996) Further examining the American dream: differential correlates of intrinsic and extrinsic goals. Pers Soc Psychol B 22(3):280–287
Ryan RM, Frederick C (1997) On energy, personality, and health: subjective vitality as a dynamic reflection of well-being. J Pers Soc Psychol 65(3):529–565
Nix GA, Ryan RM, Manly JB, Deci EL (1999) Revitalization through self-regulation: the effects of autonomous and controlled motivation on happiness and vitality. J Exp Soc Psychol 35(3):266–284
Bjorner JB, Wallenstein GV, Martin MC, Lin P, Blaisdell-Gross B, Tak Piech C, Mody SH (2007) Interpreting score differences in the SF-36 Vitality scale: using clinical conditions and functional outcomes to define the minimally important difference. Curr Med Res Opin 23(4):731–739. https://doi.org/10.1185/030079907X178757
Croog SH, Levine S, Testa MA, Brown B, Bulpitt CJ, Jenkins CD, Klerman GL, Williams GH (1986) The effects of antihypertensive therapy on the quality of life. N Engl J Med 314(26):1657–1664. https://doi.org/10.1056/NEJM198606263142602
Fowler FJ Jr, Wennberg JE, Timothy RP, Barry MJ, Mulley AG Jr, Hanley D (1988) Symptom status and quality of life following prostatectomy. JAMA 259(20):3018–3022
Burns RA, Byles J, Mitchell P, Anstey KJ (2012) Positive components of mental health provide significant protection against likelihood of falling in older women over a 13-year period. Int Psychogeriatr 24(9):1419–1428
Burns R, Sargent-Cox K, Mitchell P, Anstey K (2014) An examination of the effects of intra and inter-individual changes in wellbeing and mental health on self-rated health in a population study of middle and older-aged adults. Soc Psychiatry Psychiatr Epidemiol 49(11):1849–1858. https://doi.org/10.1007/s00127-014-0864-6
Burns RA, Browning CJ, Kendig HL (2015) Examining the 16-year trajectories of mental health and wellbeing through the transition into widowhood. Int Psychogeriatr 27(12):1979–1986. https://doi.org/10.1017/S1041610215000472
Burns RA, Butterworth P, Browning C, Byles J, Luszcz M, Mitchell P, Shaw J, Anstey KJ (2014) Examination of the association between mental health, morbidity, and mortality in late life: findings from longitudinal community surveys. Int Psychogeriatr. https://doi.org/10.1017/s1041610214002051
Burns RA, Byles J, Magliano DJ, Mitchell P, Anstey KJ (2015) The utility of estimating population-level trajectories of terminal wellbeing decline within a growth mixture modelling framework. Soc Psychiatry Psychiatr Epidemiol 50(3):479–487. https://doi.org/10.1007/s00127-014-0948-3
Burns RA, Byles J, Mitchell P, Anstey KJ (2012) Positive components of mental health provide significant protection against likelihood of falling in older women over a 13-year period. Int Psychogeriatr 24(9):1419–1428. https://doi.org/10.1017/S1041610212000154
Burns RA, Mitchell P, Shaw J, Anstey K (2014) Trajectories of terminal decline in the wellbeing of older women: the DYNOPTA project. Psychol Aging 29(1):44–56
StataCorp (2015) Stata statistical software: release 14. StataCorp LP, College Station
Wasserstein RL, Schirm AL, Lazar NA (2019) Moving to a world beyond “p < 0.05”. Am Stat 73(sup1):1–19. https://doi.org/10.1080/00031305.2019.1583913
McAllister M, Wynaden D, Happell B, Flynn T, Walters V, Duggan R, Byrne L, Heslop L, Gaskin C Staff experiences of providing support to students who are managing mental health challenges: a qualitative study from two Australian universities
Thorley C (2017) Not by degrees: improving student health in the UK’s universities. Institute of Public Policy Research
Cuijpers P, Auerbach RP, Benjet C, Bruffaerts R, Ebert D, Karyotaki E, Kessler RC (2019) The World Health Organization World Mental Health International College Student initiative: an overview. Int J Methods Psychiatr Res 28(2):e1761. https://doi.org/10.1002/mpr.1761
Harrer M, Adam SH, Baumeister H, Cuijpers P, Karyotaki E, Auerbach RP, Kessler RC, Bruffaerts R, Berking M, Ebert DD (2019) Internet interventions for mental health in university students: a systematic review and meta-analysis. Int J Methods Psychiatr Res 28(2):e1759. https://doi.org/10.1002/mpr.1759
Lungu A, Sun M (2016) Time for a change: college students’ preference for technology-mediated versus face-to-face help for emotional distress. Telemed J E Health 22(12):991–1000. https://doi.org/10.1089/tmj.2015.0214
Chan JK, Farrer LM, Gulliver A, Bennett K, Griffiths KM (2016) University students’ views on the perceived benefits and drawbacks of seeking help for mental health problems on the internet: a qualitative study. JMIR Hum Factors 3(1):e3. https://doi.org/10.2196/humanfactors.4765
Storrie K, Ahern K, Tuckett A (2010) A systematic review: students with mental health problems—a growing problem. Int J Nurs Pract 16(1):1–6. https://doi.org/10.1111/j.1440-172X.2009.01813.x
Acknowledgements
The research in this paper uses unit record data from the Household, Income and Labour Dynamics in Australia (HILDA) Survey. HILDA is funded by the Australian Government Department of Families, Housing, Community Services and Indigenous Affairs (FaHCSIA) and managed by the Melbourne Institute of Applied Economic and Social Research (Melbourne Institute). The findings and view reported in this paper are those of the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, Richard A. Burns states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Burns, R.A., Crisp, D.A. The long-term mental health of Australia’s tertiary students. Soc Psychiatry Psychiatr Epidemiol 55, 1223–1230 (2020). https://doi.org/10.1007/s00127-019-01806-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-019-01806-7