Abstract
Purpose
Self-rated health is frequently used as an indicator of health and quality of life in epidemiological studies. While the association between self-rated health and negative mental health is well established, associations with indictors of positive wellbeing are less clear. Data from the Dynamic Analyses to Optimise Ageing (DYNOPTA) project were used to compare the effects of vitality and mental health on self-rated health.
Methods
Participants (n = 40,712) provided information on vitality, mental health and self-rated health, were aged 45–95 years at baseline, and were followed between 1 and 10 years (M = 5.6; SD = 2.9).
Results
In comparison with mental health, multi-level modelling indicated between- and within-person change in vitality was more strongly associated with self-rated health. Bivariate dual change score modelling of the cross-lagged associations between vitality and self-rated health indicated vitality to be a stronger predictor of change in self-rated health. Self-rated health was unrelated to change in vitality.
Conclusion
Vitality accounted for most of the mental health effect on self-rated health and was identified as a significant predictor of change in self-rated health over a 10-year period. Promoting wellbeing and psychological functioning may have significant protective effects on negative health outcomes throughout the adult lifespan and into late life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Self-rated heath was introduced into social and medical research as a cost-efficient alternative to clinical assessments of health status [1]. Reflecting respondents’ rating of their general health, self-rated health has become an important component in the measurement of overall health status in both clinical and epidemiological research [2]. Associations between self-rated health and chronic illness, somatization, hypochondriasis, functional disability, and physicians’ health ratings have been reported [3]. Poor self-rated health is a strong predictor of stroke, functional decline, nursing home entry, falls, driving cessation, increased health service utilisation, and mortality [4–10]. Conversely, positive ratings of self-rated health have a protective effect on health outcomes and health behaviours, including higher levels of exercise, and lower levels of smoking and alcohol consumption [11–13]. Self-rated health is also related to social support; socio-economic factors; psychological resources, including coping strategies, perceived control, expectations of health, and self-efficacy; and psychological measures of emotionality, including depression, positive and negative affect, and distress [14–17]. Despite the established association between mental ill-health and poor self-rated health, examination of the associations between self-rated health and dimensions of psychological wellbeing (e.g. vitality, mastery, resilience) is limited. This study explores the concurrent effects of mental health and wellbeing on self-rated health.
Recent definitions of mental health extend beyond the focus on the absence of mental ill-health symptoms and incorporate the presence of positive affect states, healthy psychological functioning, and related behaviours [18, 19]. Recently, Huppert and colleagues [20] proposed a two-factor model of psychological wellbeing that incorporated factors of psychological feeling (e.g. optimism, positive affect) and functioning (e.g. mastery, autonomy) to complement other indices of mental health in a large cross-national population study. Psychological wellbeing has been indicated in a range of outcomes including falls risk and coronary heart disease [21–24]. In this study, we focus on one indicator of psychological wellbeing: the concept of vitality. Vitality reflects feelings of psychological energy and engagement and is a characteristic of fully functioning and psychologically healthy individuals. It is positively related to other wellbeing indicators such as self-actualization, autonomy, and self-esteem, intrinsic motivation, and mindfulness [25–28]. As an indicator of positive mental health, vitality has been demonstrated to be a malleable construct that can be adversely influenced by a range of physical health conditions including cardiovascular and musculoskeletal disorders, respiratory disease and diabetes, hypertension, prostate disease, and mortality [22, 29–31]. Change in vitality has also been associated with better depression outcomes [29]. Its utility as an indicator of positive wellbeing has been demonstrated in large population-based studies [20, 32]. The present study will concurrently examine the longitudinal impact of vitality and mental health on self-rated health from middle adulthood into very old age. First, we will explore whether vitality is associated with level and change in self-rated health, over and above effects for mental health. Second, we will examine the cross-lagged effects of prior self-rated health and wellbeing on change within a bivariate dual change score model (BDCSM) framework.
Method
Participants
Data for these analyses were taken from the Dynamic Analyses to Optimize Ageing (DYNOPTA) project [33]. The DYNOPTA project pools data from nine Australian longitudinal studies of ageing. For this study, data were drawn from the Australian Longitudinal Study of Women’s Health (ALSWH; n = 25,148; years = 1996–2005), the Australian Diabetes, Obesity and Lifestyle study (AusDiab; n = 7,241; years = 1999–2005), the Blue Mountains Eye Study (BMES; n = 2,080; years = 1992–2004), and the Household Income and Labour Dynamics in Australia Study (HILDA (n = 5685; years = 2001–2005). The harmonization of existing studies, by pooling data or parallel analysis, is increasingly recognised as an important method that contributes to and addresses the limitations of investment in individual longitudinal studies [34]. Ethical approval was obtained for all individual studies from relevant supervisory bodies (see acknowledgement), while ethical approval for the DYNOPTA project was approved by the Australian National University Human Research Ethics Committee in accordance with National guidelines and the ethical standards laid down in the 1964 Declaration of Helsinki. Overall, there were 50, 652 respondents in the pooled DYNOPTA dataset at baseline, which was collected between 1990 and 2001. Participants (n = 40,712) were included in this study if they had relevant self-rated health, mental health, and vitality scores. Participants were aged 45–95 years (M = 60; SD = 11) at baseline, were predominantly females (80 %), partnered (72 %), and followed for a mean of 6 (SD = 3) years.
Measures
Vitality and mental health
We derived variables from the Short-Form Health Survey-36 (SF-36) [35]. The Vitality and Mental Health sub-scales are two of the subscales that partly comprise the SF-36 Mental Health Component Score. The validation of the SF-36 factor structure in DYNOPTA has previously been reported [36]. Findings from that publication are of relevance for the current study. First, the factor structure of the a-prior SF-36 was confirmed. Second, removing the cross-loadings of the Vitality subscale on the Physical Health Component Score did not significantly lead to a decrement in model fit. Finally, the factor structure was found to be invariant amongst young–old and old–old DYNOPTA participants. For both the Vitality and Mental Health subscales, participants indicated the extent to which they experienced each statement on a 6-point Likert-type scale, ranging from ‘1’ ‘None of the Time’ to ‘6’ ‘All of the Time’ over the preceding four weeks. Vitality and mental health were scaled such that high scores indicated high levels of vitality and mental health (i.e. low levels of mental ill-health). The SF-36 Mental Health Index, including the higher order latent factor Mental Health Component Score, has been validated as a measure of mental health, and specifically depression, in epidemiological studies worldwide [37, 38]. Although moderate cross-sectional bivariate correlations between vitality and mental health, with magnitudes of between r = 0.57 and r = 0.64, were reported over time we concluded that a significant amount of variance in these constructs still remains unexplained and warrants treating these variables as separate indicators of different dimensions of mental health and wellbeing.
Self-rated health
Self-rated health was measured using the global health item from the SF-36 which requires participants to describe their general health on a 5-point rating scale from ‘1’ ‘Excellent’ to ‘5’ ‘Poor’. For ease in interpreting the reported coefficients, self-rated health scores were rescored so that high scores indicated positive self-rated health.
Covariates
Our models adjusted for demographic characteristics including age, education and partner status, and time in study, and included an indicator for each contributing DYNOPTA study. Baseline age was annualised to the nearest chronological year. Education was classified into two levels relating to the extent of school and tertiary education participants reported: no post-high school education (the reference category); and any post-high school (non-tertiary or tertiary) education. Participant partner status was classified into two categories: ‘partnered’ and ‘not partnered’. Time was measured as years since baseline measurement.
Statistical analysis
The key research aims were addressed using the following statistical approaches. First, the relationships between vitality and mental health on self-rated health were examined using multi-level modelling in STATA v10. We examined both between- and within-person change in vitality and mental health and their effects on concurrent level and change in self-rated health. Change in self-rated health was operationalised as a residual change-score whereby current self-rated health is regressed on current wellbeing after adjusting for prior level of self-rated health. Between-person vitality and mental health are reflected as fixed effects that reflect participants’ scores at baseline. Within-person change in both wellbeing and mental health were computed as time-varying variables reflecting individuals’ deviation from their baseline score. Delineating between- and within-person effects in this way is a common approach to longitudinal modelling [39].
Our second aim was to test the lead–lag relationships between wellbeing and self-rated health. This was evaluated using bivariate dual change score modelling (BDCSM) in MPLUS v.7 [40]. BDCSM allows exploration of the cross-domain change in vitality and self-rated health and to examine predominance of lead–lag indicators of change. The BDCSM framework combines elements of latent growth models (LGM) [41] and cross-lagged regression models [42] and estimates latent intercept and slope factors for two variables and their cross-lagged relationships. Our BDCSM used full information maximum likelihood (FIML) estimation whereby all available data build up maximum-likelihood estimates to optimise the model parameters and adjusts for unbalanced data structures and longitudinal selectivity under the assumption that data are missing at random [43].
A graphical representation of our BDCSM is described in Fig. 1. As an example, the diagram comprises manifest and latent variables for two variables of interest, vitality and self-rated health, reflected by the initials ‘v’ and ‘s’. A constant is represented by the triangle, and fixed and random parameters are reflected by the single- and two-headed arrows, respectively. All unlabeled paths are constrained to 1. The intercepts V 0 and S 0 reflect baseline vitality and self-rated health scores while the slope factors V S and S S reflect a linear 12-month change in vitality and self-rated health scores. The vitality and self-rated health latent intercepts and slopes are allowed to vary and covary as indicated by the double-headed paths. The latent vitality and self-rated health scores are reflected by the manifest variables v1 thru v10 and s1 thru s10, which represent the ten measurements of vitality and self-rated health, respectively. Each measure represents a 12-month period between measurement occasions. The BDCSM assumes that the error terms es and ev are normally distributed with a mean of zero and time-invariant variance and are uncorrelated with the other components. As a unique feature of the BDCSM, the difference scores for vitality (∆v [t1 thru 10]) and self-rated health (∆s [t1 thru 10]) are defined by three components. First is the linear component of change for each variable which is reflected by the regression of the latent difference scores ∆v [t] and ∆s [t] on the latent slope factors X S and Y S, respectively. Unlike a typical latent growth model, these parameters are all constrained to 1. Second, the auto-proportion parameters, βv and βs, reflect the prior effect of variable v or s, respectively, at time t − 1 on change in each of the variables. Finally, the cross-lagged parameters ϒvs and ϒsv are estimated and reflect the effect of vitality (ϒvs) at time t − 1 on change in the self-rated health (∆s [t]) or conversely the effect of self-rated health (ϒsv) at time t − 1 on change in vitality (∆v [t]). Examination of the inter-variable coupling parameters allows us to make an empirical comparison of several hypotheses pertaining the associations and lead–lag patterns between vitality and self-rated health. Specifically, the BDCSM allows us to test the following hypotheses: (a) that prior level of self-rated health predicts change in vitality while the effect for prior level of vitality on change in self-rated health is constrained to zero; (b) that prior level of vitality predicts change in self-rated health while the effect for prior level of self-rated health on change in vitality is constrained to zero; (c) that prior level of self-rated health and vitality report similar-sized effects on subsequent change in each other; and (d) that prior level of self-rated health and vitality are unrelated with subsequent change in each other being constrained to zero. Using goodness of fit indices (GFI), these models are compared to a baseline model in which the cross-lagged effects of prior vitality on change self-rated health and prior self-rated health on change in vitality are freely estimated.
In all analyses, we compensated for DYNOPTA’s sample size by only interpreting effects with stringent α values (p < 0.001) and focus on those large effects with small standard error. All reported estimates are residualized for age, sex, time, partner, and education status. To ease interpretation of effects, self-rated health, vitality and mental health variables were transformed into z scores and standardized to baseline.
Results
Delineating within and between-person effects of mental health and vitality on self-rated health
Intercept-only models established the Intraclass Correlation Coefficients (ICC) for vitality (ICC = 0.62), mental health (ICC = 0.57) and self-rated health (ICC = 0.61), indicating most of the variance was accounted for at the intercept. Significant declines in vitality [β = −0.005 (SE = 0.001); p < 0.001], mental health [β = −0.007 (SE = 0.001); p < 0.001], and self-rated health [β = −0.016 (SE = 0.001); p < 0.001] were also reported, warranting an examination of the effects of intra-individual vitality and mental health on the changes in self-rated health. These results are reported in Table 1. First, higher levels of within-person change in mental health (β = 0.263) and baseline mental health (β = 0.440) scores were associated with higher levels of self-rated health over time. However, much of the between- and within-person effects for mental health on self-rated health in Model 1 were accounted for by the inclusion of between- and within-person vitality effects in Model 2. Within-person change in vitality (β = 0.396) was associated with increases in self-rated health while higher levels of baseline vitality (β = 0.571) were associated with higher levels of self-rated health. As mental health and vitality were z scored, a direct comparison of the effect sizes clearly demonstrates that vitality was more strongly associated with self-rated health than mental health. Finally, we extended our analyses to estimate the effects of change in mental health and vitality on change in self-rated health (Model 3). Results (Table 1) indicated that the effects of mental health on self-rated health were accounted for by both level and change in vitality with change in vitality (β = 0.324; SE = 0.004; p < 0.001) the most significant driver of change in self-rated health. This suggests that between-occasion change in vitality is a significant predictor of change in self-rated health.
Given DYNOPTA is a study with particular focus on the determinants of ageing and late-life health, we did consider the impact of ageing effects. However, non-substantive age effects were reported, with only a reported 0.006 SD decline in self-rated health for each year a person aged. Investigation of interaction effects between age and both the between- and within-person mental health and vitality variables identified these effects as mostly failing to reach statistical significance. One exception was an age interaction for the between-person effect of vitality; a small increment in self-rated health was found for each year above 45 for those who reported an increase in vitality (β = 0.003; SE = 0.000; p < 0.001). However, since the variables were z scored, the size of this effect is far from substantive. Even when comparing age in broader 10-year age groupings this reflected only a 0.03 SD increase in self-rated health per decade for those who reported increases in vitality. Since the effects of vitality and mental health were far more substantial than the effects for age, and the effects of vitality and mental health appear to be consistent across age levels, we concluded that further investigation of age effects was not warranted. Other statistically significant demographic effects were also of much smaller magnitude in comparison with the wellbeing and mental health effects and are not reported here as they are not related to our aims.
Evaluation of the lead–lag effects of vitality and mental health on self-rated health
Since vitality was identified as a stronger predictor of self-rated health than was mental health, we supplemented our multi-level analysis with a BDCSM [40] to test our second aim: an examination of the auto-regressive relationships between vitality and self-rated health to determine dominance of effect between self-rated health and vitality. Table 2 reports GFI used to compare five nested models, each adjusted for baseline chronological age, gender, education, and partner status. The baseline model freely estimated both cross-lagged coupling parameters for prior level of vitality on change in self-rated health and for prior level of self-rated health on change in vitality. Four other models were nested under this baseline model. A uni-directional model constrained the vitality on self-rated health parameter to zero while the self-rated health on vitality parameter was freely estimated. Conversely, a third model, also a uni-directional model, constrained the self-rated health on vitality parameter to zero while the vitality on self-rated health parameter was freely estimated. A fourth model, an equal-coupling model, estimated both cross-lagged parameters (effect of prior self-rated health on level of vitality and effect of prior vitality on level of self-rated health) constraining them to be of equal size. The fifth model constrained these parameters to zero and reflects a no-coupling model, whereby neither vitality not self-rated health influences each other.
Statistically significant differences in χ 2 statistics indicate a loss in fit for all models in comparison with the baseline model, though it should be noted that since χ 2 is susceptible to large sample sizes, comparisons between models with other GFI is warranted. For instance, the RMSEA confidence intervals and CFI revealed comparable fit between all models. Comparison of the difference in χ 2 scores between Models 2–4 indicated Model 3, where the parameter reflecting the effect of self-rated health on vitality was constrained to zero, as a better fitting model than the other models (p < 0.001). Nested model comparisons would, therefore, suggest that we cannot reject the hypothesis that vitality and self-rated health influence each other. Hypotheses proposing a lead from self-rated health, equality of coupling parameters, and the lack of coupling effects could be rejected. However, given the performance of Model 3 in comparison with the other models, we believe there is an argument for not rejecting the hypothesis that vitality precedes change in self-rated health.
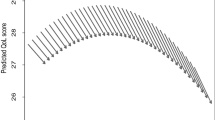
The estimates for Model 1 are reported in Table 3. In contrast to the multi-level models, declines in SRH were accounted for while a small increase in vitality was reported. However, significant random effects for the slopes in both vitality and self-rated health were reported and indicated individual level variability in change. Of particular emphasis for these analyses are the coupling effects between self-rated health and vitality. Clearly the effect of vitality on self-rated health is substantial. In contrast, the coupling of self-rated health on vitality failed to reach statistical significance. To more clearly demonstrate the importance of vitality in predicting self-rated health, we provide a graphical illustration (Fig. 2a, b) to compare the magnitude of the vitality and self-rated health coupling parameters. We modelled their effects over time using estimates derived from the full-coupling BDCSM and are used to describe the implications of varying the initial sample mean for one variable by one standard deviation keeping values for the other variable constant. The top panel (Fig. 2a) indicates the change in self-rated health values over time for three hypothetical individuals who scored the mean level of self-rated health at baseline, but who reported three different vitality scores: mean vitality and 1 standard deviation above and below the mean vitality score. The top line represents a higher self-rated health score for an individual with a vitality score 1SD above the vitality mean, the middle line represents self-rated health when reporting mean vitality, and the bottom line represents a lower self-rated health score for an individual who reports a vitality score 1SD below the vitality mean. In contrast, the bottom panel (Fig. 2b) indicates the change in vitality for three individuals who report the same vitality value at baseline, but who report three different self-rated health scores: mean self-rated health and 1 standard deviation above and below the mean self-rated health score. As with the previous diagram, the top line represents a higher vitality score for an individual with an self-rated health score 1SD above the self-rated health mean, the middle line represents vitality when reporting mean self-rated health, and the bottom line represents a lower vitality score for an individual who reports an self-rated health score 1SD below the vitality mean. This figure clearly demonstrates that the magnitude is greater for the parameter reflecting the effect of prior vitality on self-rated health since there is almost a whole standard deviation difference in self-rated health score between the individual with higher vitality and the individual with lower vitality. In contrast, the difference in the plots of the three vitality scores for those with high, average, and low self-rated health is negligible.
Plotting the effects of self-rated health and vitality on each other based on estimates from age-adjusted bivariate dual change score models. Solid lines reflect self-rated health and the dotted lines vitality; a indicates the effects of vitality (+1SD, mean, −1SD) on self-rated health score over 10 years for participants who report the same level of self-rated health at baseline; b indicates the effects of self-rated health (+1SD, mean, −1SD) on vitality score over 10 years for participants who report the same level of vitality at baseline
Discussion
The central objective of this study was to examine whether vitality, a positive dimension of wellbeing, is as strongly related to self-rated health as is mental health. In a large population sample of middle- and older-aged adults, we demonstrated that the effects of between- and within-person vitality were the most important drivers of level and change in self-rated health, a finding that was consistent across age. The inclusion of age, gender, education, and partner status failed to account for these effects. While these results indicate vitality as a stronger predictor of self-rated health than mental health, it might well be argued that mental health or vitality be regressed on self-rated health. Indeed, an alternative, but equally defensible hypothesis would be that wellbeing and mental health are the outcome of prior self-rated health. Further analysis extended our findings to determine the lead–lag dominance of vitality over self-rated health or self-rated health over vitality. Analysis within a BDCSM framework allowed us to formally compare competing hypotheses relating to the auto-regressive relationships by delineating intra and inter-construct dynamics [44] between self-rated health and vitality. Overall, vitality was a strong driver in change in self-rated health, whereas self-rated health was not associated with change in vitality.
There are a number of important implications to be considered from these findings. Wellbeing appears to be more strongly implicated in the perceptions of self-rated health than is mental health. In contrast to focusing on measures of clinically related mental health outcomes or psychological distress, this suggests that public health policy should recognise the importance of national accounts of wellbeing to assess social reform and economic policies that impact on the quality of life and wellbeing of their citizens, not just on their mental health [45]. This raises questions about the extent to which population-level interventions can be introduced to improve population wellbeing. There is evidence that interventions can elicit positive wellbeing [46–49]. For example, a recent meta-analysis identified medium effect sizes for the efficacy of positive psychology programmes for increasing wellbeing indices, including vitality (r = 0.29; 95 % CI 0.21; 0.37) and for decreasing depression symptoms (r = 0.31; 95 % CI 0.17; 0.43) [48]. Engagement in these activities elicited both positive functioning and feeling in adults the benefits of which include increased healthy outcomes, community engagement, and increased workforce participation.
DYNOPTA is essentially an observational study and the findings need to be interpreted in this light. For instance, no experimental manipulation of variables is possible. However, large longitudinal surveys provide a significant opportunity to determine the importance of psychological functioning at the population level, with the additional power and increased number of observations to address limitations of smaller experimental designs into the role of positive psychological functioning over a long temporal period. We believe that the findings from this longitudinal study support smaller scale experimental work which emphasise the importance of positive psychological functioning over and above negative dimensions of mental health and highlight positive wellbeing as a significant precursor of quality of life and general wellbeing [48]. We also believe there remain several important wellbeing questions that remain to be answered. Other interesting areas of investigation could relate to applying a mixture modelling approach to identify classes of mental health and wellbeing trajectories in relation to changes in self-rated health, recognising that individuals may differ in their trajectories and not follow a population trajectory.
To conclude, the role of positive wellbeing dimensions in contributing to healthy ageing, independently of negative mental health states, is increasingly recognised [18]. In this study, we have demonstrated that vitality accounted for most of the effect for mental health on self-rated health in a large population sample of middle-aged and older adults, who were followed for up to 10 years. Further, we identified that changes in vitality significantly contributed to change in self-rated health. While the role of negative physical and mental health on self-rated health is well understood, considering the robustness of our findings, it is clear that further research into the role of positive dimensions of wellbeing and flourishing on self-rated health is warranted.
References
Maddox GL (1999) Commentary on the self-reported health symposium. Res Aging 21:501–506
Benyamini Y, Idler EL (1999) Community studies reporting association between self-rated health and mortality: additional studies, 1995 to 1998. Res Aging 21:392–401
Barsky AJ, Cleary PD, Klerman GL (1992) Determinants for perceived health status of medical outpatients. Soc Sci Med 34:1147–1154
Emmelin M et al (2003) Self-rated ill-health strengthens the effect of biomedical risk factors in predicting stroke, especially for men—an incident case referent study. J Hypertens 21:887–896
Lee Y, Shinkai S (2003) A comparison of correlates of self-rated health and functional disability of older persons in the Far East: Japan and Korea. Arch Gerontol Geriatr 37(1):63–76
Roos NP et al (1988) Using administrative data to predict important health outcomes: entry to hospital, nursing home, and death. Med Care 26(3):221–239
Anstey KJ, von Sanden C, Luszcz MA (2006) An 8-year prospective study of the relationship between cognitive performance and falling in very old adults. J Am Geriatr Soc 54:1169–1176
Anstey KJ et al (2006) Predicting driving cessation over 5 years in older adults: psychological well-being and cognitive competence are stronger predictors than physical health. J Am Geriatr Soc 54:121–126
Blaum CS, Liang J, Liu X (1994) The relationship of chronic diseases and health status to the health service utilization of older Americans. J Am Geriatr Soc 42:1087–1093
Mohan R et al (2011) Self-rated health as a tool for estimating health-adjusted life expectancy among patients newly diagnosed with localized prostate cancer: a preliminary study. Qual Life Res: Int J Qual Life Aspects Treat Care Rehabil 20(5):713–721
Mossey JM, Shapiro E (1982) Self-rated health: a predictor of mortality among the elderly. Am J Public Health 72(8):800–808
Settersten L, Lauver DR (2004) Critical thinking, perceived health status, and participation in health behaviors. Nurs Res 53(1):11–18
Sargent-Cox K et al (2014) The effect of health behaviour change on self-rated health across the adult life course: a longitudinal cohort study. Prev Med 58:75–80
Bisconti TL, Bergeman CS (1999) Perceived social control as a mediator of the relationships among social support, psychological well-being, and perceived health. Gerontologist 39:94
Franks P, Gold MR, Fiscella K (2003) Sociodemographics, self-rated health, and mortality in the US. Soc Sci Med 56:2505–2514
Barsky AJ (1988) The paradox of health. N Engl J Med 318:414–418
Kaplan GA, Camacho T (1983) Perceived health and mortality: a nine-year follow-up of the Human Population Laboratory cohort. Am J Epidemiol 117(3):292–304
Huppert FA, Keverne B, Bayliss N (2004) The science of well-being, integrating neurobiology, psychology and social science. Proc Royal Soc Sci Discuss Meet 359(1449):1447–1451
Keyes CL (2002) The mental health continuum: from languishing to flourishing in life. J Health Soc Behav 43(2):207–222
Huppert FA et al (2009) Measuring well-being across Europe: description of the ESS Well-being module and preliminary findings. Soc Indic Res 91(3):301–315
Burns RA et al (2012) Positive components of mental health provide significant protection against likelihood of falling in older women over a 13-year period. Int Psychogeriatr 24(9):1419–1428
Boehm JK et al (2011) A prospective study of positive psychological well-being and coronary heart disease. Health Psychol 30(3):259–267
Burns RA, Machin MA (2010) Identifying gender differences in the independent effects of personality and psychological well-being on two broad affect components of subjective well-being. Personal Individ Differ 48(1):22–27
Burns RA, Machin MA (2012) Moving beyond the pleasure principle: within and between-occasion effects of employee eudaimonia within a school organizational climate context. J Vocat Behav 80(1):118–128
Ryan RM, Frederick C (1997) On energy, personality, and health: subjective vitality as a dynamic reflection of well-being. J Personal 65(3):529–565
Kasser T, Ryan RM (1996) Further examining the American dream: differential correlates of intrinsic and extrinsic goals. Personal Soc Psychol Bull 22(3):280–287
Brown KW, Ryan RM (2003) The benefits of being present: mindfulness and its role in psychological well-being. J Personal Soc Psychol 84(4):822–848
Nix GA et al (1999) Revitalization through self-regulation: the effects of autonomous and controlled motivation on happiness and vitality. J Exp Soc Psychol 35(3):266–284
Bjorner JB et al (2007) Interpreting score differences in the SF-36 vitality scale: using clinical conditions and functional outcomes to define the minimally important difference. Curr Med Res Opin 23(4):731–739
Croog SH et al (1986) The effects of antihypertensive therapy on the quality of life. N Engl J Med 314(26):1657–1664
Fowler FJ Jr et al (1988) Symptom status and quality of life following prostatectomy. J Am Med Assoc 259(20):3018–3022
Foundation NE (2009) National accounts of well-being: bringing real wealth onto the balance sheet. N.E. Foundation (ed). New Economics Foundation, London
Anstey KJ et al (2010) Cohort profile: the dynamic analyses to optimize ageing (DYNOPTA) project. Int J Epidemiol 39(1):44–51
Noale M et al (2005) Predictors of mortality: an international comparison of socio-demographic and health characteristics from six longitudinal studies on aging: the CLESA project. Exp Gerontol 40:89–99
Ware JE Jr et al (1998) The factor structure of the SF-36 health survey in 10 countries: results from the IQOLA Project. International quality of life assessment. J Clin Epidemiol 51(11):1159–1165
Bartsch LJ et al (2011) Examining the SF-36 in an older population: analysis of data and presentation of Australian adult reference scores from the dynamic analyses to optimise ageing (DYNOPTA) project. Qual Life Res 20(8):1227–1236
Skapinakis P et al (2005) Mental health inequalities in Wales, UK: multi-level investigation of the effect of area deprivation. Br J Psychiatry 186:417–422
Gill SC et al (2006) Mental health and the timing of men’s retirement. Soc Psychiatry Psychiatr Epidemiol 41(7):515–522
Singer JD, Willett JB (2003) Applied longitudinal data analysis : modeling change and event occurrence. Oxford University Press, Oxford, New York, pp xx, 644
McArdle JJ, Hamagami F (2001) Latent difference score structural models for linear dynamic analyses with incomplete longitudinal data. In: Sayer LMCAG (ed) New methods for the analysis of change. American Psychological Association, Washington, DC, pp 137–176
Meredith W, Tisak J (1990) Latent curve analysis. Psychometrika 55:107–122
Rogosa D (1980) A critique of cross-lagged correlation. Psychol Bull 88:245–258
Gerstorf D et al (2009) Dynamic links of cognitive functioning among married couples: longitudinal evidence from the Australian longitudinal study of ageing. Psychol Aging 24(2):296–309
Lovden M et al (2005) Studying individual aging in an interindividual context: typical paths of age-related, dementia-related, and mortality-related cognitive development in old age. Psychol Aging 20(2):303–316
Beddington J et al (2008) The mental wealth of nations. Nature 455(7216):1057–1060
Boehm JK, Lyubomirsky S, KM Sheldon (2011) A longitudinal experimental study comparing the effectiveness of happiness-enhancing strategies in Anglo Americans and Asian Americans. Cognit Emot 25(7):1263–1272
Lyubomirsky S (2011) Hedonic adaptation to positive and negative experiences. In: The Oxford handbook of stress, health, and coping. Oxford University Press, New York, pp 200–224
Sin NL, Lyubomirsky S (2009) Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J Clin Psychol 65(5):467–487
Fava GA, Tomba E (2009) Increasing psychological well-being and resilience by psychotherapeutic methods. J Personal 77(6):1903–1934
Acknowledgments
The data on which this research is based were drawn from several Australian longitudinal studies including the Australian Longitudinal Study of Ageing (ALSA), the Australian Longitudinal Study of Women’s Health (ALSWH), the Australian Diabetes, Obesity and Lifestyle Study (AusDiab), the Blue Mountain Eye Study (BMES), the Canberra Longitudinal Study of Ageing (CLS), the Household, Income and Labour Dynamics in Australia study (HILDA), the Melbourne Longitudinal Studies on Healthy Ageing (MELSHA), the Personality And Total Health Through Life Study (PATH), and the Sydney Older Persons Study (SOPS). These studies were pooled and harmonized for the Dynamic Analyses to Optimise Ageing (DYNOPTA) project. DYNOPTA was funded by the National Health and Medical Research Council (NHMRC grant # 410215). All studies would like to thank the participants for volunteering their time to be involved in the respective studies. Details of all studies contributing data to DYNOPTA, including individual study leaders and funding sources, are available on the DYNOPTA website (http://dynopta.anu.edu.au). The findings and views reported in this paper are those of the author(s) and not those of the original studies or their respective funding agencies. Burns and Sargent-Cox are supported by the Australian Research Council Centre of Excellence in Population Ageing Research (project #: CE110001029). Anstey is supported by an NHMRC Research Fellowship (No. 366756).
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Burns, R.A., Sargent-Cox, K., Mitchell, P. et al. An examination of the effects of intra and inter-individual changes in wellbeing and mental health on self-rated health in a population study of middle and older-aged adults. Soc Psychiatry Psychiatr Epidemiol 49, 1849–1858 (2014). https://doi.org/10.1007/s00127-014-0864-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-014-0864-6