Abstract
Purpose
To resolve contradictory evidence regarding racial/ethnic differences in perceived need for mental health treatment in the USA using a large and diverse epidemiologic sample.
Methods
Samples from 6 years of a repeated cross-sectional survey of the US civilian non-institutionalized population were combined (N = 232,723). Perceived need was compared across three non-Hispanic groups (whites, blacks and Asian-Americans) and two Hispanic groups (English interviewees and Spanish interviewees). Logistic regression models were used to test for variation across groups in the relationship between severity of mental illness and perceived need for treatment.
Results
Adjusting statistically for demographic and socioeconomic characteristics and for severity of mental illness, perceived need was less common in all racial/ethnic minority groups compared to whites. The prevalence difference (relative to whites) was smallest among Hispanics interviewed in English, −5.8% (95% CI −6.5, −5.2%), and largest among Hispanics interviewed in Spanish, −11.2% (95% CI −12.4, −10.0%). Perceived need was significantly less common among all minority racial/ethnic groups at each level of severity. In particular, among those with serious mental illness, the largest prevalence differences (relative to whites) were among Asian-Americans, −23.3% (95% CI −34.9, −11.7%) and Hispanics interviewed in Spanish, 32.6% (95% CI −48.0, −17.2%).
Conclusions
This study resolves the contradiction in empirical evidence regarding the existence of racial/ethnic differences in perception of need for mental health treatment; differences exist across the range of severity of mental illness and among those with no mental illness. These differences should be taken into account in an effort to reduce mental health-care disparities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Compared with non-Hispanic whites, racial/ethnic minorities in the USA are less likely to receive mental health treatment [1,2,3], particularly those who are immigrants to the USA [4, 5]. Evidence suggests that this disparity in care results from a convergence of social [6] and service system factors [7], which put minorities who seek care at a disadvantage when they seek care [8, 9]. However, with respect to perception of need for mental health treatment, an earlier phase in the help-seeking process [10,11,12], evidence regarding racial/ethnic differences is mixed. Qualitative studies find differences across racial/ethnic groups in the USA, with minorities less likely to consider themselves in need of mental health treatment than non-Hispanic whites [13,14,15]. Such variation is not surprising, given that interpretation of mental health conditions as medical conditions varies widely across cultures and across historical periods [16,17,18,19] as do idioms of distress through which mental health problems are expressed [20, 21].
Large epidemiological studies provide an opportunity to observe whether the findings from qualitative studies, which are based on relatively small non-representative samples, reflect differences across racial/ethnic groups in perception of need for mental health treatment in the general population. To date, epidemiological studies have not confirmed those expectations. Two surveys of the US general population, one conducted in the early 1990s [22] and one in the early 2000s [23], found no associations between racial/ethnicity and the perception of need for mental health treatment. However, those studies had two important limitations that may have led them to underestimate of the extent of variation across racial/ethnic groups.
First, the sample sizes for minority groups in prior studies have been small, particularly for those groups that include large proportions of immigrants, among whom differences from whites in the use of mental health treatment is largest: Hispanics and Asian-Americans [24, 25]. Second, the studies have been restricted by design to respondents who meet criteria for a current (within the past year) mental disorder. However, a large portion of mental health services are used by people without a current mental illness [26], most of whom have some alternative clinically significant justification for treatment [27]. Differences in perception of need may contribute to disparities in utilization of mental health care across the full range of severity of mental illness and among people who do not meet criteria for a mental disorder. In addition, cultural variation across racial/ethnic groups may lead to variation in the relationship between severity of mental illness and perceived need.
In this study, we examine racial/ethnic differences in perceived need for mental health care in a way that addresses the limitations of prior studies. Using data on a large sample of the US population, compiled from multiple years of an annual survey, we investigate differences in perceived need for mental health treatment across the full range of severity of mental illness, from no illness in the past year to serious illness in the past year. The sample includes large numbers of Asian-American and Hispanic respondents, including a subsample that chose to take the interview in Spanish. Resolving the contradictory evidence regarding racial/ethnic differences in perceived need is important for efforts, such as anti-stigma campaigns that aim to improve treatment uptake and reduce disparities in service use.
Methods
Study sample
Six years of data (2009–2014) on the adult (age 18 years and over) sample from the National Survey of Drug Use and Health (NSDUH) were combined. The NSDUH is an annual survey of a nationally representative sample of the US population. The sample is based on a multi-stage area probability sample of households and group living quarters. Interviews are conducted in respondents’ homes using computer-assisted interviewing methods [28]. Interviews were conducted in English and Spanish. The data are publicly available at: https://www.datafiles.samhsa.gov/. Analysis of publicly accessible data was approved by the RAND Human Subject Protection Committee.
Assessments
Perception of need for treatment
Following Mojtabai [22], respondents were identified as perceiving a need for mental health treatment if they received treatment within the past year or indicated that they needed but did not receive treatment within the past year. The definition was modified to exclude respondents who received treatment, but indicated that they did so because they were legally required to do so. Perceived need was assessed among those who did not receive treatment with the following question: “During the past 12 months, was there any time when you needed mental health treatment or counseling for yourself but did not get it?”
Mental illness
Mild, moderate and serious mental illness are defined using a weighted combination of responses to the K6 [29], a measure of serious psychological distress, and the World Health Organization Disability Scale (WHODAS) [30], a measure of impairment [31]. Weights were developed in a calibration study, in which survey respondents were re-interviewed by psychologists using a structured clinical interview [32]. Mild, moderate and serious mental illnesses, defined according to the clinical interviews, were modeled in the calibration sample as a function of responses to the K6 and WHODAS items. Coefficients from these models were then applied to the K6 and WHODAS scores for the entire NSDUH sample to generate the corresponding mental illness categories.
Race/ethnicity
Respondents are asked to indicate whether they are of Hispanic origin and which racial group or groups they identify with. We focus on five racial/ethnic groups defined using these items, three non-Hispanic and two Hispanic. The non-Hispanic groups are whites, blacks, and Asian-Americans. Hispanics were sub-divided by language of interview into English interview and Spanish interview groups.
Other covariates
Statistical adjustments were made for demographic characteristics (age, sex, marital status, and household size), socioeconomic status (educational attainment, employment status, and income), health insurance coverage, and survey year.
Statistical analysis
Associations between race/ethnicity and perceived need for mental health treatment were estimated in logistic regression models with statistical adjustment for covariates. Results are presented on the prevalence scale using predicted marginals. Heterogeneity of associations between severity of mental illness and perceived need across racial/ethnic groups was also tested on the prevalence scale [33]. The predicted prevalence of perceived need for each racial/ethnic group at each level of severity of mental illness was estimated from a logistic regression model including the statistical interaction between race/ethnicity and severity of mental illness in addition to the following covariates: age, sex, marital status, family size, educational attainment, income, employment status, insurance coverage, severity of mental illness, and survey year. Statistical analyses were conducted using the survey procedures in STATA to account for the complex sample design [34].
Results
Table 1 shows the demographic and socioeconomic status characteristics of the sample, by race/ethnicity. These distributions follow the expected population patterns. Differences are notable for the larger household sizes and high levels of ‘no health insurance’ for Hispanics relative to other groups and for the high levels of educational attainment among Asian-Americans. For ease of presentation, subsequent results are not shown for the other race/ethnicity category, but are available from the author. Table 2 shows the distribution of two key study variables, perceived need and mental illness severity, by race/ethnicity. The prevalence of perceived need is highest among whites (17.9%), about half as high among blacks (9.4%), and about a third as high among Asian-Americans (6.4%). Among Hispanics, there is a threefold difference in the prevalence of perceived need between those who completed the interview in English (11.1%) and those who completed the interview in Spanish (3.4%). There are also large differences in the prevalence of mental illness across racial/ethnic groups. Notably, the prevalence of serious mental illness is higher among whites (4.4%) than among blacks (3.1%) and Asian-Americans (2.2%). Among Hispanics, the difference between the English and Spanish interview groups in prevalence of serious mental illness is almost threefold (4.3 vs. 1.5%).
The prevalence of perceived need remains lower in each of the four racial/ethnic minority groups relative to whites after statistical adjustment for age, sex, marital status, family size, educational attainment, income, employment status, urbanicity, insurance coverage, severity of mental illness, and survey year (Table 3). For the entire population, differences are all statistically significant, ranging from −5.8% (95% CI −6.5, −5.2%) among Hispanics interviewed in English to −11.2% (95% CI −12.4, −10.0%) among Hispanics interviewed in Spanish. Statistically significant differences are also found for each racial/ethnic group at each level of mental illness. The differences are smaller among those without mental illness when compared to those with mental illness. However, perceived need is less prevalent among those without mental illness; thus, it is expected that smaller differences in perceived need exist between the groups among those without mental illness. These results provide clear evidence that the differences in perceived need between the racial/ethnic groups occur across mental illness severity groups. Particularly notable are the prevalence differences found in the group with serious mental illness, where compared with whites the prevalence of perceived need is 23.3% (95% CI −34.9, −11.7%) lower among Asian-Americans and 32.6% (95% CI −48.0, −17.2%) lower among Hispanics interviewed in Spanish.
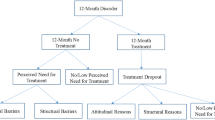
Figure 1 shows the adjusted prevalence of perceived need at each level of mental illness, within each racial/ethnic group. Among all racial/ethnic groups, the prevalence of perceived need rises with increasing severity of mental illness, but the magnitude of these increases differs across racial/ethnic groups (Chi-squared test for differences across racial/ethnic groups: p < 0.001). Among whites, the difference in prevalence of perceived need between the highest and lowest categories of mental illness is 62.5%. The corresponding differences are significantly smaller among the other four race/ethnic groups. Among blacks and Hispanics interviewed in English, the difference in prevalence of perceived need between the highest and lowest severity of mental illness categories is slightly smaller than among whites, at 56.1% (p = 0.016) and 56.7% (p = 0.018), respectively. The difference is much smaller among Asian-Americans at 47.7% (p = 0.012) and Hispanics interviewed in Spanish at 30.6% (p < 0.001). p values correspond to the difference between the race/ethnic groups of the differences in perceived need between the highest and lowest severity of mental illness categories. Similar patterns hold for the other mental illness categories and are statistically significant (results available upon request).
Discussion
The goal of this study was to address contradictory evidence in the literature regarding differences in perceived need for mental health treatment across racial/ethnic groups in the USA. Studies which focus on minority groups, in particular those that focus on immigrant populations, suggest that racial/ethnic minorities are less likely than whites to perceive themselves as in need of mental health treatment [13, 14]. However, data from studies based on large representative samples of the US population have not supported these conclusions [22, 23, 35]. The contradictory evidence might arise from a lack of representativeness of the studies that focus on minority groups or limitations in the population coverage of the epidemiological studies. Results from this study clearly resolve the contradictory evidence in favor of the existence of large differences in perceived need across racial/ethnic groups. This finding has important implications for understanding and responding to racial/ethnic disparities in mental health service use.
Confidence in these results stems from two strengths of this study relative to prior analyses of epidemiological survey data, the large sample size, and the assessment of perceived need in the entire population, across the range of severity of mental illness. The large sample size, made possible by combining multiple years of an annual survey, provided greater statistical power to detect differences and allowed us to break out groups of particular interest that were not examined in prior studies, in particular Hispanics who choose to take the interview in Spanish and Asian-Americans. Inclusion of the entire population allowed us to examine differences in perceived need at varying levels of mental illness, which is important given the large proportion of mental health services that are used by people who do not meet the official criteria for a disorder [27]. In addition, we were able to compare the relationship of perceived need with severity of mental illness across groups, yielding additional insights regarding cultural differences. These differences were sustained after statistical adjustment for demographic and socioeconomic characteristics.
The finding that all minority groups are less likely to perceive a need for mental health treatment, even after adjusting for mental health status, suggests that differences in perceived need may be a neglected cause of racial/ethnic disparities in mental health-care utilization. The differences in perceived need are similar in magnitude to observed differences across racial/ethnic groups in mental health-care utilization. For instance, according to unadjusted estimates based on the 2008–2012 NSDUH, use of any mental health services was 8.0% less common among blacks relative to whites and 11.7% less common among Asian-Americans relative to whites [36]. The corresponding differences in perceived need, based on Table 2 above, are 8.6% for blacks and 11.5% for Asian-Americans. Both clinical and non-clinical intervention strategies that have commonly been used to address disparities in care could be extended in ways that specifically address perception of need, in addition to traditional goals of increasing uptake of treatment among people with identified conditions. Clinical interventions such as collaborative care for depression in primary care, which has been shown to reduce disparities in care [37], could be augmented with efforts to address the diversity of perceptions of distress among people who screen positive for depression [38]. Non-clinical interventions, such as anti-stigma campaigns [39], could be more culturally targeted with greater emphasis on faith-based [40, 41] and other community-based organizations, such as work being done on public health outreach through barber shops [42]. Programs addressing mental health literacy may also be useful [43, 44]. However, more evidence is needed to guide policy in this area, particularly given the lack of evidence that increasing knowledge of medical models of mental illness is associated with more accepting attitudes toward the mentally ill [45, 46].
Three additional findings emerge with examination of differences in perceived need across levels of mental illness severity. First, differences exist even at the highest level of severity of illness. From a public health perspective, this is perhaps the most important finding, given that this group is most likely to benefit from mental health services. Second, differences in perceived need also exist among the group with the lowest level of need, those who do not appear to have a mental illness based on their reported symptoms and impairment. Differences at this low end of the severity range are more challenging to interpret because we do not have clear criteria for distinguishing overuse of care from unmet need for care in this group. It is therefore unclear whether the appropriate strategy for addressing these differences is to lower perception of need among whites or to increase perception of need among minority groups. However, the issue is highly significant with respect to equal distribution of health-care resources. Although the proportions of individuals in the no disorder group that perceive need for care are low, ranging from 9.9% among whites to 1.8% among Hispanics interviewed in Spanish, the volume of services used by this group is large, due to the large portion of the population with no past year mental illness, which ranges from 80.6% among whites to 89.3% among Hispanics interviewed in Spanish.
Third, among minority racial/ethnic groups the differences in the relationship of severity of mental illness with perceived need follow two distinct patterns. For blacks and Hispanics interviewed in English, the increase in perceived need is smaller than among whites, though consistent throughout the range of severity of mental illness. This finding is consistent with research showing that self-rated mental health is more strongly associated with standardized assessments of mental health in whites than in minority groups [47, 48]. In contrast, for Asian-Americans and Hispanics interviewed in Spanish, the two groups largely comprised immigrants from countries with much lower prevalence of mental health service use [24, 25, 49], and the increase in prevalence of perceived need across levels of mental illness was noticeably smaller. In particular, the gap between Hispanics interviewed in Spanish and the other groups widens across levels of mental illness. The larger gap in perceived need among these groups suggests an even more profound divergence between cultural perceptions of need and clinically defined need among these two groups comprised largely of immigrants than among the two other groups comprised largely of US-born individuals. There is also evidence from prior studies that the relationship between self-rated health and psychiatric diagnoses differ between African-Americans and Caribbean blacks in the USA [50]. These findings confirm at a population level the importance of addressing cultural perceptions of mental health and illness among immigrant groups [21, 51, 52].
One limitation of this study is the lack of interviews in languages other than English and Spanish. While Spanish is by far the most commonly spoken non-English language in the USA, the next three most common languages are Asian languages: Chinese, Tagalog, and Vietnamese. Given evidence that perception of need is more common among more acculturated Asian-Americans [53], it is likely that if speakers of additional Asian languages were included, the prevalence of perceived need in the Asian-American sample would be lower than it is in the current sample.
The large and persistent racial/ethnic disparities in mental health services in the USA are likely a result of a complex mix of factors that influence individuals at many points in the help-seeking process. The evidence from this study suggests that differences in perception of need for treatment across groups, one of the earliest stages in the help-seeking process, may be a large contributor to those differences. Differences in perceived need may be one reason that disparities in utilization of care remain after accounting for differences in access to care and health status [54]. Addressing these differences presents a complex institutional challenge to the health-care system, in particular for tailoring efforts to address perceptions of need to different groups and to different levels of mental illness. However, our ability to improve equity in the distribution of mental health care across race/ethnic groups may be limited without attention to these cultural differences that precede initiation of care.
References
Alegría M et al (2008) Disparity in depression treatment among racial and ethnic minority populations in the US. Psychiatr Serv 59(11):1264–1272
Gonzalez HM et al (2010) Depression care in the US too little for too few. Arch Gen Psychiatry 67(1):37–46
Cook BL et al (2014) Assessing racial/ethnic disparities in treatment across episodes of mental health care. Health Serv Res 49(1):206–229
Orozco R et al (2013) A cross-national study on prevalence of mental disorders, service use, and adequacy of treatment among mexican and mexican american populations. Am J Public Health 103(9):1610–1618
Alegria M et al (2007) Correlates of past-year mental health service use among Latinos: results from the National Latino and Asian American Study. Am J Public Health 97(1):76–83
Dinwiddie GY et al (2013) Residential segregation, geographic proximity and type of services used: evidence for racial/ethnic disparities in mental health. Soc Sci Med 80:67–75
Alegria M et al (2012) The impact of insurance coverage in diminishing racial and ethnic disparities in behavioral health services. Health Serv Res 47(3 Pt 2):1322–1344
Cook BL et al (2016) Assessing the individual, neighborhood, and policy predictors of disparities in mental health care. Med Care Res Rev. doi:10.1177/1077558716646898
Cook BL et al (2016) Trends in racial-ethnic disparities in access to mental health care, 2004–2012. Psychiatr Serv 68(1):9–16
Mechanic D (2002) Removing barriers to care among persons with psychiatric symptoms. Health Aff (Millwood) 21(3):137–147
Edlund MJ, Unützer J, Curran GM (2006) Perceived need for alcohol, drug, and mental health treatment. Soc Psychiatry Psychiatr Epidemiol 41(6):480–487
Andersen RM (1995) Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav 36(1):1–10
Wong YJ et al (2010) Asian Americans’ lay beliefs about depression and professional help seeking. J Clin Psychol 66(3):317–332
Carpenter-Song E et al (2010) Ethno-cultural variations in the experience and meaning of mental illness and treatment: implications for access and utilization. Transcult Psychiatry 47(2):224–251
Apesoa-Varano EC et al (2015) Idioms of distress among depressed white-non-Mexican and Mexican-origin older men. J Cross Cult Gerontol 30(3):305–318
Karasz A (2005) Cultural differences in conceptual models of depression. Soc Sci Med 60(7):1625–1635
Horwitz AV, Wakefield JC (2007) The loss of sadness: how psychiatry transformed normal sorrow into depressive disorder. Oxford University Press, Oxford
Kirmayer LJ, Schwartz L (2014) Culture and global mental health. In: Patel V (ed) Global mental health: principles and practice. Oxford University Press, New York, pp 41–62
Good BJ (1992) Culture, diagnosis and comorbidity. Cult Med Psychiatry 16(4):427–446
Lewis-Fernandez R et al (2002) Comparative phenomenology of ataques de nervios, panic attacks, and panic disorder. Cult Med Psychiatry 26(2):199–223
Lewis-Fernández R et al (2010) Association of trauma-related disorders and dissociation with four idioms of distress among latino psychiatric out-patients. Cult Med Psychiatry 34(2):219–243
Mojtabai R, Olfson M, Mechanic D (2002) Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Arch Gen Psychiatry 59(1):77–84
Mojtabai R et al (2011) Barriers to mental health treatment: results from the National Comorbidity Survey Replication. Psychol Med 41(8):1751–1761
Kim G et al (2011) Limited English proficiency as a barrier to mental health service use: a study of Latino and Asian immigrants with psychiatric disorders. J Psychiatr Res 45(1):104–110
Bauer AM, Chen C-N, Alegría M (2010) English language proficiency and mental health service use among Latino and Asian Americans with mental disorders. Med Care 48(12):1097–1104
Wang PS et al (2005) Twelve-month use of mental health services in the US: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry 62(6):629–640
Druss BG et al (2007) Understanding mental health treatment in persons without mental diagnoses: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry 64(10):1196–1203
Center for Behavioral Health Statistics and Quality (2015) 2014 National survey on drug use and health: methodological summary and definitions. Rockville, Substance Abuse and Mental Health Services Administration
Kessler RC et al (2003) Screening for serious mental illness in the general population. Arch Gen Psychiatry 60(2):184–189
Novak SP et al (2010) Development of a brief mental health impairment scale using a nationally representative sample in the USA. Int J Methods Psychiatr Res 19(Suppl 1):49–60
Colpe LJ et al (2010) The national survey on drug use and health mental health surveillance study: calibration study design and field procedures. Int J Methods Psychiatr Res 19(Suppl 1):36–48
Aldworth J et al (2010) The national survey on drug use and health mental health surveillance study: calibration analysis. Int J Methods Psychiatr Res 19(Suppl 1):61–87
Greenland S, Lash T, Rothman KJ (2008) Concepts of interaction. In: Rothman KJ, Greenland S, Lash T (eds) Modern epidemiology, 3rd edn. Philadelphia, Lippincott Williams & Wilkins
StataCorp (2015) Stata Statistical Software, Release 13. 2015. College Station, StataCorp LP
Ault-Brutus A, M Alegria (2016) Racial/ethnic differences in perceived need for mental health care and disparities in use of care among those with perceived need in 1990–1992 and 2001–2003. Ethn Health: 1–16
Substance Abuse and Mental Health Services Administration (2015) Racial/ethnic differences in mental health service use among adult. Rockville, Substance Abuse and Mental Health Services Administration
Miranda J et al (2004) Effects of primary care depression treatment on minority patients’ clinical status and employment. Arch Gen Psychiatry 61(8):827–834
Epstein RM et al (2010) “I didn’t know what was wrong”: how people with undiagnosed depression recognize, name and explain their distress. J Gen Intern Med 25(9):954–961
Stuart H (2016) Reducing the stigma of mental illness. Glob Ment Health 3:e17. doi:10.1017/gmh.2016.11
Taylor RJ et al (2000) Mental health services in faith communities: the role of clergy in black churches. Soc Work 45(1):73–87
Dempsey K, Butler SK, Gaither L (2016) Black churches and mental health professionals: can this collaboration work? J Black Stud 47(1):73–87
Luque JS, Ross L, Gwede CK (2014) Qualitative systematic review of barber-administered health education, promotion, screening and outreach programs in African-American communities. J Community Health 39(1):181–190
Jorm AF (2012) Mental health literacy: empowering the community to take action for better mental health. Am Psychol 67(3):231–243
Morawska A et al (2013) Evaluation of mental health first aid training in a diverse community setting. Int J Ment Health Nurs 22(1):85–92
Pescosolido BA et al (2010) “A disease like any other”? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. Am J Psychiatry 167(11):1321–1330
Schomerus G et al (2012) Evolution of public attitudes about mental illness: a systematic review and meta-analysis. Acta Psychiatr Scand 125(6):440–452
Zuvekas SH, Fleishman JA (2008) Self-rated mental health and racial/ethnic disparities in mental health service use. Med Care 46(9):915–923
Kim G et al (2011) Associations between self-rated mental health and psychiatric disorders among older adults: do racial/ethnic differences exist? Am J Geriatr Psychiatry 19(5):416–422
Wang PS et al (2007) Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet 370(9590):841–850
Assari S, Dejman M, Neighbors HW (2016) Ethnic differences in separate and additive effects of anxiety and depression on self-rated mental health among blacks. J Racial Ethn Health Disparities 3(3):423–430
Guarnaccia PJ et al (2010) Ataque de nervios as a marker of social and psychiatric vulnerability: results from the NLAAS. Int J Soc Psychiatry 56(3):298–309
Abe-Kim J et al (2007) Use of mental health-related services among immigrant and US-born Asian Americans: results from the National Latino and Asian American Study. Am J Public Health 97(1):91–98
Leong FT, Lau AS (2001) Barriers to providing effective mental health services to Asian Americans. Ment Health Serv Res 3(4):201–214
Fiscella K et al (2002) Disparities in health care by race, ethnicity, and language among the insured: findings from a national sample. Med Care 40(1):52–59
Acknowledgements
This work was supported by Grants from the National Institute on Minority Health and Health Disparities (R01 MD010274) and the National Institute of Mental Health (R01 MH104381).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Breslau, J., Cefalu, M., Wong, E. et al. Racial/ethnic differences in perception of need for mental health treatment in a US national sample. Soc Psychiatry Psychiatr Epidemiol 52, 929–937 (2017). https://doi.org/10.1007/s00127-017-1400-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-017-1400-2