Abstract
Introduction
Depression is the second most common chronic disorder seen by primary care physicians. Risk factors associated with depression include medical and psychosocial factors. While in Israel, the rate and risk factors for depression are considered similar to those in other Western countries, population-based data are limited. The present study aims to estimate the prevalence of depression among Jews and Muslim Arabs, and to consider possible associations with demographic, socioeconomic, and health factors.
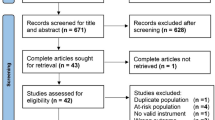
Methods
The study group (N = 872) was equally divided according to ethnicity, gender, and age group. Depression was measured by the Harvard Department of Psychiatry National Depression Screening Day Scale (HANDS).
Results
The rate of depression scores in the likely/very likely range was 2.5 times higher among Arabs than among Jews (24.9 vs. 10.6%; P < 0.001). Women were more likely to express symptoms of depressive episode than were men (22.0 vs. 13.6%; P = 0.001), and the depression rate increased with age, from 11.0% in the youngest group (26–35) to 25.0% in the oldest (P = 0.001). The rate of increase in depression by age was different for the genders, rising more steeply for women than for men. However, the age–gender differential was not identical for the two ethnic groups. The differences in depression prevalence between Arabs and Jews were maintained after controlling for confounding variables, except that when controlling for education, the difference between the ethnic groups was no longer significant. After adjusting for all variables in the analysis, no significant association remained between ethnicity and depression (OR = 0.80; 95% CI = 0.45–1.40).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Depression is the second most common chronic disorder seen by primary care physicians [52], manifesting as a combination of feelings of sadness, loneliness, irritability, worthlessness, hopelessness, agitation and guilt, accompanied by an array of physical symptoms [3]. Hays et al. [26] even suggest that depressed patients have long-lasting impairments in functioning that are at least as severe as do patients with chronic illness. Depression can be treated effectively by psychotherapy and medications [16]. Early identification and proper management can significantly decrease its negative impact in most patients [11].
In developed countries, the lifetime prevalence of major depression in adults is estimated at 7–12% in men and 20–25% in women [50]. General population studies have reported a point prevalence of major depressive disorder of about 5% [7, 43, 51] and rates of depressive symptoms of approximately 15% [14, 35, 36], with the prevalence among patients in primary care settings ranging from 5 to 10% [32].
Population-based data in Israel are limited. A study published in 2003 reported a depressive symptom rate of 21.5% in a representative sample of the adult Jewish population in Israel using the Beck Depression Inventory [27].
Risk factors found to be associated with depression include demographic variables [7, 30, 50, 53], medical conditions [8, 39, 44, 48], psychosocial factors, and measures related to socio-economic status [12, 20, 38, 47].
There is no clear evidence that being a member of an ethnic or racial minority is a risk factor for depression. In the US, Jackson-Triche et al. [29] found that African-Americans and Hispanics had the highest rates of depressive symptoms and Asian-Americans had the lowest, but after adjusting for other variables few statistically significant differences remained. However, large epidemiologic surveys have found that, compared to non-Hispanic whites, blacks have lower lifetime rates of depressive disorder, equivalent or lower rates of 12-month depressive disorder [7, 9, 34, 46], and a higher risk of the persistence of major depressive disorder [54]. The relatively low prevalence rates of depression among minority groups cannot be explained by ethnic differences in response patterns to questions concerning depression [10]. The pattern of race–ethnic differences in risk for psychiatric disorders (including depression) suggests the presence of protective factors that originate in childhood and have generalized effects on internalizing disorders [9]. It has been suggested that even though minority group members are at increased risk for depression (associated with more reporting of problems meeting their basic needs), they also report a higher quality of interpersonal functioning, which may moderate the relationship between ethnicity and depression [45].
Studies reporting depression among Muslim Arabs have identified specific risk groups (women, middle-age) in a primary health care sample in the United Arab Emirates [16–18] and in a community survey of adults in Al-Ain city [13]. A higher rate was found among divorced Israeli Bedouin-Arab women in the Negev [2], as well as among young women, students, and non-married in Bahraini adults [42]. An association of depression with specific morbidity, e.g. hypertension, has also been reported in a Qatari population [6].
The current study aims to estimate the prevalence of depression among Jews and Muslim Arabs in Israel, the latter being a minority group and of generally lower socioeconomic status (SES), and to identify demographic, socioeconomic, and health status factors which can explain prevalence rates in both population groups.
Methods
Design
This is a population-based, cross-sectional study.
Subjects
The study participants were derived from a random sample of the general urban population of the Hadera District in Israel. The district population (about 300,000 residents), mostly urban, includes about 60% Jews and 40% Arabs, living in separate towns. The study sample (N = 880) was stratified into groups of equal size, according to ethnicity (Arab or Jewish), gender, and four age groups (overall age range: 25–67 years). Eight individuals of the original sample, from very small population groups, were excluded. The overall response rate to the interviews in the original sample was 79%; 90% among Arabs and 68% among Jews (P < 0.001). Non-responders (who could not be traced or refused participation) were on average 3 years younger than participants (P = 0.07). The proportion of men among non-responders was 44% compared to 51% among participants (P = 0.08). Non-responders were substituted by others drawn from a random sample, matched by gender, age, ethnicity, and town of residence [31].
Variables and instruments
A structured interview questionnaire was prepared for the study protocol. The questionnaire was translated into Hebrew and Arabic, and translation and back-translation ensured reliability across languages. Ethnicity (Arab or Jewish), was determined by self-report and validated by the participant’s town of residence. Demographic parameters included gender, age, and marital status. Age groups were clustered into four 10-year age groups, according to age quartiles at time of interview, as follows: 26–35, 36–45, 46–55; 56–67. Socioeconomic parameters included housing density (number of people living in the home divided by the number of rooms), years of education, employment status, self-reported religious identification, and professional prestige. Professional prestige was determined according to the 10-group ordinal scale of the Israel Bureau of Statistics grading, with the score chosen being the highest prestige level of the subject or his/her spouse. Health status was defined as the number of chronic diseases (e.g. diabetes, hypertension) reported, and grouped as follows: 0, 1, and 2+.
Depression was measured using the Harvard Department of Psychiatry National Depression Screening Day Scale (HANDS) [25], following permission received for its translation and use. The HANDS is a ten-question screening instrument for assessing depression symptoms over the previous 2 weeks, developed and tested in a community population of depressed and non-depressed adults. Scores range from 0 (the symptom occurring none or a little of the time) to 3 (occurring all of the time), for total scores ranging from 0 to 30. Internal consistency was demonstrated by an Alpha coefficient of 0.87. Validation in the general population suggested that a cutoff score of >9 had a sensitivity of 0.95 and a specificity of 0.94, for meeting DSM-IV criteria for major depressive episode [3]. Further distinction regarding severity is as follows: 0–8 indicates that the presence of a major depressive episode is unlikely; 9–16 indicates that the presence of a major depressive episode is likely; 17–30 indicates that the presence of a major depressive episode is very likely [4]. The authors recommend that those with a score of ≥9 undergo a complete mental health evaluation to determine whether a diagnosis of clinical depression is indicated. Since there were very few scores at the extremes of the scoring range, for the current analysis, the HANDS score was divided dichotomously into two groups: ‘not likely’ to be suffering from depression (<9) and ‘likely/very likely’ to be suffering from depression (9–30).
Procedure
Interviews and completion of the HANDS were conducted in the participants’ homes by trained Arabic- or Hebrew-speaking personnel. Data were collected from January 2002 to May 2006. The study protocol was approved by the ethics committee of the Sheba Medical Center and all participants provided written informed consent form before participation in the study.
Statistical analysis
Data entry and analyses were performed using the 9.13 release of SAS PC computer software. Differences in demographic and clinical characteristics between the Arabs and Jewish participants were tested using binary and ordered logistic regressions, adjusted for gender and age. The difference between the two populations in years of education was tested using analysis of covariance, adjusted for gender and age. Differences between the two population groups in the prevalence of depression, adjusted for each of the demographic and health characteristics were tested using the Cochran Mantel–Haenszel test.
A multiple logistic regression with depression as the dependent variable was applied using logistic procedure. The process of building the multiple regression model began by conducting univariate analysis for each explanatory variable: participants’ age, gender, ethnicity, years of education, marital and employment status, religious identification, professional prestige, housing density (persons per room) and number of chronic diseases. Explanatory variables found significant at a 20% level were entered into a backward elimination procedure, except for gender and ethnicity, which were forced into the multivariate model. By this procedure, the least significant variables were eliminated sequentially until all remaining variables were significant at a 6% level. Interactions between ethnicity gender or age and any of the other explanatory variables were then tested. This constituted the final multiple regression.
Results
Subjects
The two main study groups, Jews and Arabs, had almost identical age and gender distributions, as per sampling design. When compared with Arabs, Jews rated significantly better on all socio-economic indicators. No difference in the number of chronic diseases was observed (Table 1).
Depression
The distribution of HANDS scores was: 82.2% (N = 717) not likely to be suffering a major depressive episode (score < 9), 15.4% reporting symptoms indicating likelihood of an episode (score 9–16) and 2.4% very likely to be suffering an episode (score ≥ 17). The rate of scores in the likely/very likely range was 2.4 times higher among Arabs than among Jews (24.9 vs. 10.6%; P < 0.001).
Arabs were more likely to report depression than were Jews in almost every strata of the variables associated with depression (e.g. age, gender, number of chronic diseases) (Table 2). The only exceptions were that there was no difference in the depression rate among Arabs and Jews, among those employed; among those in the highest professional prestige tertile; among those with at least 13 years of education (for whom the rate was even lower among Arabs than Jews, 1.4 vs. 7.7%, respectively).
Women in the study group were more likely to express symptoms of depressive episode than were men (22.0 vs. 13.6%, respectively; P = 0.001), and the rate of HANDS score >9 increased with age, from 11.0% in the youngest group to 25.0% in the oldest (P = 0.001). The rate of increase in depression by age was different for the genders, rising more steeply for women than for men: 18.3–30.0%, respectively. However, the age–gender differential was not identical for the two ethnic groups (Figs. 1, 2). While in all age groups, Arabs had higher rates than did Jews, for the men, this distinction was particularly noticeable from the 46 to 55-year-old group to the 56–67 group; whereas the rate for Arab men rose from 16.1 to 24.6%, the Jewish men dropped from 12.5 to 7.1%. On the other hand, the rate among Arab women rose steadily with age, from 14.0 to 51.7%, while among Jewish women, the rate rose from 7.7% in the youngest group and peaked at 19% among the 46 to 55-year-old.
The differences in depression prevalence between Arabs and Jews were maintained after controlling for each potential confounding variable separately, except when adjusting for years of education (P = 0.77).
Multivariate analysis indicated that subjects of older age, married, more educated, and employed (each adjusted for the others) were less likely to suffer from depression. On the other hand, housing density and number of chronic diseases were significantly positively associated with depression (Table 3). After adjusting for all other variables in the analysis, no significant association remained between ethnicity and depression (OR = 0.80; 95% CI = 0.45–1.40). There were no significant interactions between age, gender, or ethnicity and any of the other variables.
Discussion
The current study explored the rates of depression and risk factors among Israeli Jewish and Arab populations in Israel. The depression rate of the Arab minority was almost three times that of the Jews and it remained significantly higher in most demographic and socioeconomic strata. These findings are in agreement with other studies recently conducted in Israel. The Israeli National Health Interview Survey 2003–2004, which included a single question about “feeling depressed most or all of the time during the past 4 weeks,” found that Arab men’s age-adjusted rate of positive responses was 1.5 times greater than that of Jewish men, and Arab women’s rate was 1.7 times higher than Jewish women’s rate [28]. The National Health Survey of 2003–2004 [37] found more expressions of emotional distress among Arabs, compared to Jews, according to the General Health Questionnaire, with rates of affective disorders (symptoms during the preceding 12 months) also higher, albeit of borderline significance. Despite the fact that the prevalence of depressive symptoms in the findings of the current study are similar, in this study multivariate analysis indicates that Arab ethnicity in itself did not enter as an independent significant factor, but the differences between the ethnic groups were better explained by disparity in their educational level and health status. The data for this study were collected between January 2002 and December 2005, during which time there were intense waves of terrorism in Israel. Two surveys of Israeli residents exposed to ongoing and widespread terrorism [21, 49], both of which found that the higher risk for depression among Israeli Arabs remained significant even after controlling for sociodemographic characteristics. Our finding that after adjusting for all other variables in the analysis, no significant association remained between ethnicity and depression, contradicts those findings. Although the differences in methodology of those surveys and the current one (sample design, timing and manner of data collection, depression instrument) might explain some disparity in the findings, it may also be likely that controlling for chronic diseases as included in our study could significantly contribute to the differences that we found.
Regarding the issue of the relationship of age and gender with depression, the current findings can contribute to the ongoing discourse. While studies have generally reported higher prevalence rates among women than men [30, 50], the relationship of gender with age seems to be more complex. This may account for the contradictory reports on the association between depression rates and increasing age [7, 36, 43]. In reviewing published studies on age-specific gender differences in depression, Jorm [30] concluded that the broad claim that depression is more common among women than men is an oversimplification, and an inverted U-shape of the age curve of the female/male depression ratios best fits the data, with the difference between male and female rates being rather small at younger ages, increasing toward mid-life and decreasing thereafter. More recent studies confirm this finding [5, 33, 53]. In the British National Survey, Meltzer et al. [40] reported that while the prevalence rate of depression is higher among women than men up to age 55, after that the ratio changes and the rate is higher for men. The current analysis indicates that the age–gender pattern differed for Arabs and Jews. Among the Jews, both men and women, the depression rate increased with age but showed a drop in the 56+ age group as reported in the literature. Among the Arabs, however, no such a drop was found in the older age group; on the contrary, the rise in depression rates with increasing age was very steep among women, rising sharply in the 56+ age group, while and among the Arab men, the rate was stable from age 25–55, and rose only in the 56+ age group. Another aspect of the differential effect of gender and age in the two ethnic groups was also noted. On the one hand, in the youngest age group, the difference between male and female rates among Jews was not small and the women had a higher rate, as Jorm claims [30], while on the other hand, the youngest Arab women had a lower rate than the Arabs males (this was the only instance of a lower rate among women vs. men).
Interestingly, in this study, multivariate analysis indicated that age was negatively associated with depression when controlling for other factors. A prime reason for this finding might be the fact that health status (number of chronic diseases) was controlled for in the model. One explanation may be found in the fact that the healthy elderly are even more appreciative of the fact of their good health—i.e. do not take it for granted—than are younger persons, and this affects their mood. Additionally, they may have gained from the benefit of their life experience, better-developed modes of coping, etc., which provide a degree of resilience to depressive episodes.
In addition, in this context, it may be important to consider the varying ethnic-specific emphases on social roles, e.g. marital and employment status (with concurrent altered social status) which also change over the life cycle, as Mirowsky has pointed out [41]. Thus, interpreting the impact of age is complex, since it may influence the risk of depression both by biological and by psychosocial mechanisms. This was also the conclusion of Gutiérrez-Lobos’ study, based on admissions to psychiatric in-patient treatment in Vienna [23], showing that the female/male ratio in first admissions of depressed patients was age-dependent and that there was a complicated interaction with marital and employment status. While the authors state that they cannot be sure whether their findings are relevant to the etiology of depression, or only reflect referral peculiarities, it is suggested that incidence studies be carried out in unselected community populations considering gender, age, marital and employment status simultaneously. They state that only by doing so might it be possible to narrow down the number of possible psychosocial and biological explanations of the gender gap in depression. It may be suggested that in the present study population, the excess of depression among the older Arab women—as compared to older Jewish women, and both Arab and Jewish men—is related to the extreme primacy of the homemaking role in their lives, and the loss of this central role with advancing age and the ‘empty nest’ syndrome. Since the data are cross-sectional, the age group differences might also reflect cohort rather than aging effects.
In this study, chronic diseases, marital status, and SES were also found related to depression rates. The major impact of chronic diseases, regardless of ethnic group, age, or gender on depression has been reported by others, who found significantly higher rates among persons with certain medical conditions, including obesity, diabetes mellitus, cancer, and a history of myocardial infarction [8, 39, 44, 48]. In a study based on 1,794 adults with diabetes from the 1999 US National Health Interview Survey, Egede [15] found that the odds of major depression were significantly increased in the presence of two or more chronic conditions. The Canadian Community Health Survey [12] reported that the proportion of respondents meeting criteria for major depression varied significantly according to age group and that in all age categories, the rate of depression was higher among individuals with chronic medical conditions, as well as those who were not married and had fewer academic degrees.
Depression rates have also been found by others to increase with worsening socio-economic circumstances. In a prospective cohort study using the annual Belgian Household Panel Survey, an inverse relationship was found between socio-economic circumstances and depression [38]. A recent study in New York City reported over twice the incidence of depression among those living in low SES neighborhoods, independent of individual SES and other individual covariates [20]. Iancu et al. [27] studied a representative sample of the adult Jewish population in Israel (N = 937) and found significantly higher depression scores among women, those more than age of 60, immigrants, those with fewer years of education, manual workers, and those with low income. The authors concluded that the rate and the risk factors were similar to those reported in other Western countries.
The findings of the current study highlight the complexity of the task in analyzing population groups in order to identify risk and target groups for intervention and not just as a statistical exercise. The potential findings are affected by which groups are compared and along what variables the comparison is conducted. A direct comparison of populations’ crude rates, even when living in the same society, would make such a comparison totally irrelevant if there are differences in basic characteristics between the groups. However, the usual adjusted rates for age and gender can mask important findings, such as the identification in this study of the older Arab women as a risk group, only evident in the ethnic–gender–age analysis. The risk factors for depression were generally more prevalent among the Arabs but even within each stratum, the depression rates were consistently higher among Arabs, with the exception of education. Educational level was the only variable in the analysis for which, when controlled for, the difference in depression rates between the ethnic groups became non-significant. Finally, multivariate analysis indicates that the risk of depression was greater among women, those with low SES indicators and those with multiple chronic diseases––independent of ethnic group. Thus, when controlling for all of these factors, there was no significant difference in the prevalence of depression between Arabs and Jews. Furthermore, there were no significant interactions between ethnicity and other explanatory variables, i.e. the association between these variables and depression did not differ in the two ethnic groups. Despite the fact that controlling for increasing number of variables will almost certainly eliminate the differences between groups, not all the variables, i.e. risk factors, have the same relevance for policy makers. There are those that may be subject to change in a relatively short time span, others might not be expected to change even over a generation, while there are risk factors that are difficult to change but their effect may be ameliorated by policy changes.
The current findings may hold relevance for identifying risk groups and setting priorities. Evidently, some target groups for intervention can be defined from our findings; for example, women of low SES, or persons with multiple chronic diseases. However, the Arab population in Israel must be a priority target group for intervention since, whatever the explanation for the disparities between the groups, there is almost three times the rate of depression among Arabs than among Jews in Israel.
A limitation of the current study is that the HANDS questionnaire was not validated specifically on the study population. Since screening tests, especially mental health instruments, may be culture-dependent, one might speculate that the gap between Arabs and Jews is an artificial difference. However, the HANDS, developed by the Harvard Department of Psychiatry, was validated and used in a multi-ethnic/cultural population [4, 25]. The variation in depression rates within the Arab population itself, across the age, gender, and socio-economic sub-groups, was similar to that observed among the Jewish participants, reducing the likelihood that ethnic difference is an artifact of misclassification induced by the study instrument. Other standardized depression screening scales, such as the Beck Depression Inventory, the Hamilton Depression Rating Scales, the Hospital Anxiety and Depression Scale, and the Center for Epidemiological Studies Depression Scale have been validated in various Arab populations [1, 19, 22, 24], lending credence to the validity of the HANDS, which is similar in content to these scales.
Conclusion
The findings of the current study highlight several issues, which may serve to focus attention on the mental health of patients in primary care settings. First, it seems apparent that in Israel, Arabs in every category of demographic, socioeconomic, and health variables are more likely to report depressive symptoms than are Jews. Despite this, the seemingly protective aspect of higher education and professional attainment among Arabs is a recurrent finding in almost all health-related research, but not enough is known about how the effect of education occurs. More in-depth research on the effect of education on health in general and on depression in particular is needed.
Second, it was found that over half of the older Arab women (aged ≥ 56) were likely to suffer depressive symptoms, thus attention should be given to the mental health needs of this risk group, for example, by screening and early intervention within the primary healthcare framework. The fact that the rates of depression rise among the older Arabs while dropping among older Jews should prompt further research into the social and cultural mechanisms that could explain this rise specifically in this age group. Finally, the fact that the presence of coexisting chronic diseases was found to impact depression rate, even when controlling for other factors, suggests the importance of further study of the inter-relation of mental and physical health factors for the well-being of the population.
References
Abdel-Khalek AM (1998) Internal consistency of an Arabic adaptation of the Beck Depression Inventory in four Arab countries. Psychol Rep 82:264–266
Al-Krenawi A, Graham JR (2004) Somatization among Bedouin-Arab women: differentiated by marital status. J Divorce Remarriage 42:131–143
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders: DSM-IV-TR, 4th edn. American Psychiatric Association, Washington, DC (text rev)
Baer L, Jacobs DG, Meszler-Reizes J et al (2000) Development of a brief screening instrument: the HANDS. Psycother Psychosom 69:35–41
Bebbington PE, Dunn G, Jenkins R et al (1998) The influence of age and gender on the prevalence of depressive conditions: report from the National Survey of Psychiatry Morbidity. Psychol Med 28:9–19
Bener A, Kamal A, Fares A, Sabuncuoglu O (2004) A retrospective study of the relationship between anxiety, depression, stress and hypertension. Arab J Psychiatry 15:131–136
Blazer DG, Kessler RC, McGonagle KA, Swartz MS (1994) The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. Am J Psychiatry 151:979–986
Bottomley A (1998) Depression in cancer patients: a literature review. Eur J Cancer Care 7:181–191
Breslau J, Aguilar-Gaxiola S, Kendler KS, Su M, Williams D, Kessler RC (2006) Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychol Med 36(1):57–68
Breslau J, Javaras KN, Blacker D, Murphy JM, Normand SL (2008) Differential item functioning between ethnic groups in the epidemiological assessment of depression. J Nerv Ment Dis 196(4):297–306
Coulehan JL, Schulberg HC, Block MR, Madonia MJ, Rodriguez E (1997) Treating depressed primary care patients improves their physical, mental, and social functioning. Arch Intern Med 157:1113–1120
Crabb R, Hunsley J (2006) Utilization of mental health care services among older adults with depression. J Clin Psychol 62:299–312
Daradkeh TK, Ghubash R, Abou-Saleh MT (2002) Al Ain community survey of psychiatric morbidity. II: sex differences in the prevalence of depressive disorders. J Affect Disord 72:167–176
Eaton WW, Kessler LG (1981) Rates of symptoms of depression in a national sample. Am J Epidemiol 114:528–538
Egede LE (2005) Effect of comorbid chronic diseases on prevalence and odds of depression in adults with diabetes. Psychosom Med 67:46–51
Elkin I, Shea MT, Watkins JT et al (1989) National Institute of Mental Health Treatment of Depression Collaborative Research Program: general effectiveness of treatments. Arch Gen Psychiatry 46:971–982
El-Rufaie OEF, Absood GH (1994) Depression in primary health care. Arab J Psychiatry 5:39–47
El-Rufaie OEF, Absood GH (1993) Minor psychiatric morbidity in primary health care: prevalence, nature and severity. Int J Soc Psychiatry 39:159–166
El-Rufaie OEF, Absood GH (1995) Retesting the validity of the Arabic version of the hospital anxiety and depression scale in primary health care. Soc Psychiatry Psychiatr Epidemiol 30:26–31
Galea S, Ahern J, Nandi A, Tracy M, Beard J, Vlahov D (2007) Urban neighborhood poverty and the incidence of depression in a population-based cohort study. Ann Epidemiol 17:171–179
Gelkopf M, Solomon Z, Berger R, Bleich A (2008) The mental health impact of terrorism on the Arab minority in Israel. A repeat cross-sectional study of Arabs and Jews. Acta Psychiatr Scand 117:269–380
Ghubash R, Daradkey TK, Al-Naseri KS, Al-Bloushi N, Al-Daheri AM (2000) The performance of the Center for Epidemiologic Study Depression Scales (CES-D) in an Arab female community. Int J Soc Psychiatry 46:241–249
Gutiérrez-Lobos K, Scherer M, Anderer P, Katschnig H (2002) The influence of age on the female/male ratio of treated incidence rates in depression. BMC Psychiatry 2:3
Hamdi E, Amin Y, Abou-Saleh MT (1997) Performance of the Hamilton depression rating scale in depressed patients in the United Arab Emirates. Acta Psychiatr Scand 96:416–423
Harvard Department of Psychiatry and the National Mental Illness Screening Project (1998) HANDS: National depression screening day scale manual. Harvard Department of Psychiatry, Wellesley Hills
Hays RD, Wells KB, Sherbourne CD, Rogers W, Spritzer K (1995) Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Arch Gen Psychiatry 52:11–19
Iancu I, Horesh N, Lepkifker E, Drory Y (2003) An epidemiological study of depressive symptomology among Israeli adults: prevalence of depressive symptoms and demographic risk factors. Isr J Psychiatry Relat Sci 40:82–89
Israel Center for Disease Control (2006) Israeli National Health Interview Survey (INHIS-1): selected findings. ICDC, Ramat Gan. Publication 249
Jackson-Triche ME, Greer Sullivan JG, Wells KB, Rogers W, Camp P, Mazel R (2000) Depression and health-related quality of life in ethnic minorities seeking care in general medical settings. J Affect Disord 58:89–97
Jorm AF (1987) Gender and age differences in depression: a quantitative synthesis of published research. ANZ J Psychiatry 21:46–53
Kalter-Leibovici O, Atamna A, Lubin F et al (2007) Obesity among Arabs and Jews in Israel: population based study. Isr Med Assoc J 9:525–530
Katon W, Schulberg H (1992) Epidemiology of depression in primary care. Gen Hosp Psychiatry 14:237–247
Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson C (1993) Gender and depression in the National Comorbidity Survey I: lifetime prevalence, chronicity and recurrence. J Aff Dis 29:85–96
Kessler RC, Berglund P, Demier O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS (2003) National Comorbidity Survey Replication. The epidemiology of major depressive disorder. JAMA 289:3095–3105
Knight RG, Waal-Manning HJ, Spears GF (1983) Some norms and reliability data for the state-trait anxiety inventory and the Zung self-rating depression scale. Br J Clin Psychol 22:245–249
Knight RG (1984) Some general population norms for the short form of Beck Depression Inventory. J Clin Psychol 40:751–753
Levav I, Al-Krenawi A, Ifrach A et al (2007) Common mental disorders among Arab-Israelis: findings from the Israel National Health Survey. Isr J Psychiatry Relat Sci 44:104–113
Lorant V, Ch Croux, Weich S, Deliege D, Mackenbach J, Ansseau M (2007) Depression and socio-economic risk factors: 7-year longitudinal population study. Br J Psychiatry 190:293–298
Mayou RA, Gill D, Thompson DR et al (2000) Depression and anxiety as predictors of outcome after myocardial infarction. Psychosom Med 62:212–219
Meltzer H, Gill B, Petticrew M, Hinds K (1995) The prevalence of psychiatric morbidity among adults living in private households. OPCS Survey of Psychiatric Morbidity in Great Britain. Report 1. HMSO, London
Mirowsky J (1996) Age and the gender gap in depression. J Health Soc Behav 37:362–380
Mosalum LMJ (1999) Psychological health and well-being in a community sample of Bahraini adults. Diss Int Sci Eng 59(9-B):4723
Murphy JM, Laird NM, Monson RR, Sobol AM, Leighton AH (2000) A 40-year perspective on the prevalence of depression: the Stirling County Study. Arch Gen Psychiatry 57:209–215
Peyrot M, Rubin RR (1997) Levels and risks of depression and anxiety symptomology among diabetic adults. Diabetes Care 20:585–590
Plant EA, Sachs-Ericson N (2004) Racial and ethnic differences in depression: the roles of social support and meeting basic needs. J Consult Clinl Psychol 72:41–52
Robins LN, Regier DA (1991) Psychiatric Disorders in America: the Epidemiologic Catchment Area Study. Free Press, New York
Smith KLW, Matheson FI, Moineddin R, Glazier RH (2007) Gender, income and immigration differences in depression in Canadian urban centres. Can J Public Health 98:149–153
Spitzer RL, Kroenke K, Williams JB (1999) Patient Health Questionnaire Primary Care Study Group. Validation and utility of a self-report version of PRIMEMD: the PHQ Primary Care Study. JAMA 282:1737–1744
Tracy M, Hobfoll SE, Canetti-Nisim D, Galea S (2008) Predictors of depressive symptoms among Israeli Jews and Arabs during the Al Aqsa Intifada: a population-based cohort study. Ann Epidemiol 18:447–457
US Dept. of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research (1993) Depression in primary care, vol 1. Detection and diagnosis. Government Printing Office, Rockville, AHCPR publication no. 93-0550/1
Weissman MM, Bland RC, Canino GJ et al (1996) Cross-national epidemiology of major depression and bipolar disorder. JAMA 276:293–299
Wells KB (1996) Caring for depression. Harvard University Press, Cambridge
Wilhelm K, Parker G, Hadzi-Pavlovic D (1997) Fifteen years on: evolving ideas in researching gender differences in depression. Psychol Med 27:875–883
Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, Jackson JS (2007) Arch Gen Psychiatry 64:305–315
Acknowledgments
This study was partially supported by the Israel National Institute for Health Policy and Health Services Research, the Israeli Association for the Study of Diabetes and the Israel Heart Fund. The funding sources had no involvement in the study design, the data collection, analysis and interpretation. The authors wish to thank Flora Lubin, Daphna Gopher, Valentina Boyko, Esther Polak and Alex Zibenber for their valuable professional assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kaplan, G., Glasser, S., Murad, H. et al. Depression among Arabs and Jews in Israel: a population-based study. Soc Psychiat Epidemiol 45, 931–939 (2010). https://doi.org/10.1007/s00127-009-0142-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-009-0142-1