Abstract
Background
There is growing recognition that mental health is an important public health issue in South Africa. Yet mental health services remain chronically under-resourced. The aim of this study was to document levels of current public sector mental health service provision in South Africa and compare services across provinces, in relation to current national policy and legislation.
Methods
A survey was conducted of public sector mental health service resources and utilisation in South Africa during the 2005 calendar year, using the World Health Organization’s Assessment Instrument for Mental Health Systems (WHO-AIMS) Version 2.2.
Results
South African policy and legislation both advocate for community-based mental health service provision within a human rights framework. Structures are in place at national level and in all nine provinces to implement these provisions. However, there is wide variation between provinces in the level of mental health service resources and provision. Per 100,000 population, there are 2.8 beds (provincial range 0–7.0) in psychiatric inpatient units in general hospitals, 3.6 beds (0–6.4) in community residential facilities, 18 beds (7.1–39.1) in mental hospitals, and 3.5 beds (0–5.5) in forensic facilities. The total personnel working in mental health facilities are 11.95 per 100,000 population. Of these, 0.28 per 100,000 are psychiatrists, 0.45 other medical doctors (not specialised in psychiatry), 10.08 nurses, 0.32 psychologists, 0.40 social workers, 0.13 occupational therapists, and 0.28 other health or mental health workers.
Conclusions
Although there have been important developments in South African mental health policy and legislation, there remains widespread inequality between provinces in the resources available for mental health care; a striking absence of reliable, routinely collected data that can be used to plan services and redress current inequalities; the continued dominance of mental hospitals as a mode of service provision; and evidence of substantial unmet need for mental health care. There is an urgent need to address weak policy implementation at provincial level in South Africa.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
There is growing recognition that mental health is an important public health issue in South Africa. Latest reviews of disease burden in this country rank neuropsychiatric conditions third in their contribution to the burden of disease, after human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS) and other infectious diseases [1]. The first major epidemiological study with a representative sample of South African adults has revealed that 16.5% suffered from a common mental disorder (CMD) (depression, anxiety or substance use disorder) in the previous year [2]. A review of existing studies concluded that about 17% of children and adolescents in the Western Cape suffer from any mental disorder [3]. These studies reported no evidence that there were any differences between socially defined racial groups or cultural groups in the prevalence of mental disorders [2, 3]. The trauma and abuses meted out during the apartheid era have been well documented in the findings of the Truth and Reconciliation Commission [4], as have the effects of these acts on the mental health of victims [5, 6].
More recently, in spite of the political freedoms and human rights advances brought about by the democratically elected government in 1994, there has been a growing trend of increased economic inequality, poverty and unemployment, which has marked the social, economic and political landscape in South Africa. Between 1996 and 2001, the percentage of the population living below the $2 per day poverty line increased from 26 to 28%, an increase that was more prominent amongst black South Africans than other population groups [7]. There is emerging evidence from low- and middle-income countries that mental ill-health is strongly associated with poverty and many aspects of social deprivation associated with poverty [8].
In spite of these disturbing trends and the projected growth in the burden attributable to mental ill-health [9], there is increasing international evidence of the existence of cost-effective interventions. During the last 40 years, anti-psychotic medications have revolutionised the care and treatment of people with schizophrenia and bipolar mood disorder, in a way that allows most people with these conditions to live relatively satisfying lives in the community [10]. Cost-effective generic medications are now available for people suffering from CMDs such as depression and anxiety [11, 12]. Advances in a range of psycho-social interventions have been made and documented [10]. Although many of these psycho-social interventions have been developed in western settings, several have been adapted and found to be effective in low- and middle-income countries, including African countries [13–15]. The development of psycho-social rehabilitation provides new directions for recovery, empowerment and re-integration into communities after periods of mental illness [16].
Like many other low- and middle-income countries, mental health services in South Africa have been chronically under-resourced. Estimates in 1996 were that 2.5% of total health expenditure and 4.2% of hospital expenditure were devoted to mental health [17]. More recent estimates of budget allocations are not routinely available. As part of the colonial legacy and institutional care under apartheid, services remained concentrated in psychiatric institutions up to the late 1990s [18]. There is currently evidence of widespread unmet need for services, with only 28% of people with moderate to severe CMDs receiving mental health care [2].
In the last 12 years, there have been important policy and legislative developments regarding mental health in South Africa. South African health policy has addressed mental health in two important policy documents in 1997 [19, 20]. More recently, there have been reforms in mental health legislation in South Africa, through the adoption of the new Mental Health Care Act (2002), promulgated in late 2004. The act is consistent with international human rights standards [21], and sets in place mechanisms for decentralisation of services, integration of mental health into general health care and the development of community-based care.
A key question is whether progress has been made towards the policy goals set out by the post-apartheid mental health policy, first formalised in 1997 [19, 20], and whether services are responding to the recent change in the legislative environment. The last national review of mental health services was conducted in 1997 [18, 22–25], and there has not yet been a systematic review of public sector mental health service provision using a broad range of input and process indicators, despite the increasing availability of instruments for the assessment of the overall resources and content of mental health service provision [26, 27].
This paper sets out to report on public sector mental health systems in South Africa, focusing on input and process indicators of service provision at the provincial level. South Africa’s nine provinces form the major organisational structure for service delivery, with plans and budget allocations to health (and mental health) services occurring at provincial level. Comparison of service provision between provinces is, therefore, a crucial gauge of the extent to which provincial health departments are implementing nationally developed policy and legislation.
Methods
Quantitative data regarding the mental health system in South Africa for the 2005 calendar year were gathered using the World Health Organization’s Assessment Instrument for Mental Health Systems (WHO-AIMS) Version 2.2 [28]. WHO-AIMS consists of six domains (covering the 10 World Health Report 2001 recommendations comprising 28 facets and 156 items). The six domains are interdependent, conceptually interlinked, and somewhat overlapping. The domains include:
-
Domain 1: policy and legislative framework
-
Domain 2: mental health services
-
Domain 3: mental health in primary care
-
Domain 4: human resources
-
Domain 5: public education and links with other sectors
-
Domain 6: monitoring and research
The WHO-AIMS spreadsheets were distributed to the following respondents:
-
9 provincial Departments of Health,
-
17 Mental Health Societies of the South African Federation for Mental Health (SAFMH), a national non-governmental organisation (NGO),
-
professional boards of the Health Professions Council of South Africa (HPCSA) for Psychology, Medicine and Occupational Therapy,
-
the South African Nursing Council, and
-
the South African Council of Social Service Professions.
The purpose of the study was to document all public sector and national NGO mental health service provision in South Africa. For this reason, a comprehensive overview of all mental health services in these sectors was necessary. However, private-for-profit services were not included as they only provide services for a minority of the population, and are seldom utilised by those who live in conditions of poverty [29], a focus of the current study. Mental health services were defined as those providing care to people of all ages with mental disorders, but did not include services for intellectual disability or substance use disorders.
The SAFMH is the only NGO that provides a coordinated national mental health service, and is the largest national mental health service provider in the NGO sector, although other NGOs provide services at a local or provincial level. It is also partially subsidised by government funding. We, therefore, decided to collect data on mental health service provision in the NGO sector from the 17 affiliated societies of the SAFMH.
In the provincial Departments of Health, the Provincial Mental Health Coordinators took responsibility for completion of the spreadsheet, gathering data from regional and district health services, with the assistance of health service managers and senior clinicians. In the SAFMH, the head of each society took responsibility for gathering data relevant to service provision at his/her branch.
The e-mailed spreadsheets were followed up with telephone calls, and (where necessary) faxed versions of the instrument. In many instances, repeated checking of the data submitted by respondents was necessary, with telephone interviews to check each item conducted by one author (SK).
In addition, preliminary findings were presented to a national meeting of Provincial Mental Health Coordinators by two authors (CL, SK). This enabled the researchers to discuss the preliminary findings in detail, and allowed provincial coordinators the opportunity to double check the data that they had submitted. Suggested changes were effected, and a final round of provincial checking of the databases was conducted after the meeting.
The data were entered into 9 separate spreadsheets for each of the provincial Departments of Health, and a further 17 spreadsheets for each of the SAFMH mental health societies. Data for provincial Departments of Health and the provincial SAFMH offices were collated into one spreadsheet to provide a provincial picture. Data from these spreadsheets were then entered into a national spreadsheet, where numeric data were aggregated. Descriptive statistical analyses of relevant items were conducted.
Results
National and provincial policy, structures and plans
As provided for in the White paper on Health [19], mental health policy implementation in South Africa takes place through national, provincial and district structures. A national mental health authority exists which provides advice to the government on mental health policies and legislation, namely the National Directorate: Mental Health and Substance Abuse, in the Department of Health. The Directorate comprises a director, three deputy directors, assistant directors and administrative staff. The implementation of the Mental Health Care Act (2002) has now been prioritised within the National Department of Health’s strategic plan (2004–2009), and is a primary focus of the activities of the National Directorate.
The national mental health authority provides policy direction to the provincial mental health authorities, who are involved in service planning, service management and coordination, and monitoring and quality assessment of mental health care. As directed by the White paper, each province has a structure responsible for mental health and substance abuse. This is either a Directorate or Sub-directorate dedicated to mental health. The seniority of the provincial mental health authority posts varies between provinces. Mental health services are organised in terms of catchment areas in all provinces.
South Africa’s first post-apartheid mental health policy guideline was approved in 1997 by the Meeting of the Health Minister and the 9 provincial Members of Executive Councils (MINMEC), now called the National Health Council, the highest decision-making body for health in South Africa. Although approved for implementation by MINMEC, the policy was not formally published or widely circulated throughout the country, nor followed by the development of implementation guidelines, due to capacity constraints within the national office, and the low priority given to implementation of mental health policy at provincial level [30]. Currently, the National Directorate is in the process of drafting a new policy which is regarded as the first national mental health policy for the country by the current national mental health officials.
Although the National Directorate has an operational plan for its own activities, there is no national mental health plan as plans are devolved to the provinces. Of the nine provinces, one has a separate strategic plan for mental health (KwaZulu-Natal, 2003) and the remaining eight have mental health plans which are integrated within the general health plan for that province. The extent to which mental health is addressed within these general health plans is variable.
A national essential drugs list (EDL) is in place, which includes anti-psychotics, anxiolytics, antidepressants, mood stabilizers and antiepileptic drugs. Psychotropic drugs are most widely available in mental hospitals (100%), followed by psychiatric inpatient units in general hospitals (96%), and then outpatient mental health facilities (88%).
Financing of mental health services
Public sector mental health care is financed through national tax revenue, which is allocated to the National Department of Health. The percentage of national government Health Department expenditure devoted to mental health is not known. All health services and budgets are devolved to the nine provinces, with allocations to mental health services at the discretion of provincial Departments of Health. There is wide variation between provinces in the budget and resources available for mental health care. Only three of the nine provinces were able to report on health expenditure on mental health care: Northern Cape spends 1%, North West 5% and Mpumalanga 8% of its health budget on mental health care.
Free access to essential psychotropic medicines is available to 80% of the population (provincial range 75–83%). For those that pay out of pocket, the cost of generic anti-psychotic medication (chlorpromazine) is 24 South African cents per day (0.7% of the daily minimum wage) and generic antidepressant medication (amitriptyline) is 15 South African cents per day (0.5% of the daily minimum wage). There are no social health insurance schemes.
Human rights protection
In keeping with the Mental Health Care Act 2002, Review Boards have been established in each province, with the authority to oversee regular inspections in mental health facilities, review involuntary admission and discharge procedures, and review appeals related to these processes. The Review Boards do not have the authority to impose sanctions (e.g., withdraw accreditation, impose penalties, or close facilities that persistently violate human rights). In addition to the Review Boards, the parliamentary Human Rights Commission has occasionally reviewed and produced reports on conditions in mental health facilities, and serves an external watchdog function.
More than half (52%) of mental hospitals and psychiatric inpatient units in general hospitals had at least one review/inspection of human rights protection of service users in 2005, while only 8% of community residential facilities had such a review. Most mental hospitals (78%) have had at least 1 day of training on human rights protection of patients in the last 2 years but only 40% of psychiatric inpatient units in general hospitals and community residential facilities have had such training.
Mental health services
Mental health outpatient facilities
There are 3,460 outpatient facilities which offer mental health services in the country, although these are general health facilities, in which the provision of specific mental health services is not monitored. Of these outpatient facilities, only 1.4% provide services exclusively for children and adolescents. Data on service utilisation were only available from 4 provinces, where these facilities treat 1,660 users per 100,000 general population annually. These services are provided as part of the integrated health service within public health facilities.
Day treatment facilities
There are 80 day treatment facilities available in the country, treating 3.4 users per 100,000 general population. Approximately, half of these facilities are run by the SAFMH. None of the facilities offer services exclusively for children and adolescents.
Of all users treated in day treatment facilities, the SAFMH reports that 41% are female. In the KwaZulu-Natal province, users spend an average of 273 days in day treatment facilities per year. Across five SAFMH facilities in four provinces, users spend an average of 267 days in day treatment facilities. No other provinces or SAFMH facilities reported length of treatment data.
Psychiatric inpatient units in general hospitals
There are 41 psychiatric inpatient units in general hospitals in the country with a total of 2.8 beds per 100,000 population. Only 3.8% of these beds are reserved for children and adolescents. These facilities are provided for and run by the provincial health authorities. The average length of admission is not routinely reported and data were, therefore, not available.
In terms of the provisions of the Mental Health Care Act (2002), general hospitals are required to admit and assess people with psychiatric emergencies for a minimum of 72 h before they may be referred to specialist mental hospitals. This has required the identification of “designated” hospital facilities that are able to provide these services. The intention of this provision is to encourage decentralisation of mental health care and integration into general health services. National Department of Health officials report that 53% of all hospitals (defined as “health establishments” in the Mental Health Care Act) have been designated to provide 72 h assessments of psychiatric emergencies, in keeping with the provisions of the act. This includes 131 of 251 district hospitals, 28 of 59 secondary hospitals, and 14 of 33 tertiary hospitals. Service users are frequently admitted to general wards in these listed facilities as there are as yet no separate psychiatric inpatient units in most of these facilities.
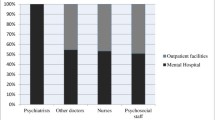
The national distribution of beds across provinces and facility types is provided in Fig. 1.
Community residential facilities
There are 63 community residential facilities available in the country, of which 47% are provided by the SAFMH. These facilities provide a total of 3.6 beds per 100,000 population. The number of these beds that are reserved for children and adolescents is not known.
The number of users in community residential facilities is 2.3 per 100,000 population and the average number of days spent in community residential facilities is unknown, except for three mental health societies in the Eastern Cape, KwaZulu-Natal and Mpumalanga which, respectively, reported average annual lengths of stay of 364, 365 and 365 days. In community residential facilities provided by the SAFMH, 41% of users are female. The Department of Health does not keep a record of gender distribution in these facilities.
Mental hospitals
There are 23 mental hospitals in the country, providing a total of 18 beds per 100,000 population (provincial range 8–39). Seventy-nine percent of these facilities are organisationally integrated with mental health outpatient facilities. Only 1% of the beds in mental hospitals are reserved specifically for children and adolescents.
The number of mental hospital beds decreased by 7.7% between 2000 and 2005. There is wide variability between provinces in this regard, with some provinces slightly increasing bed numbers (e.g., Free State 4%) and some dramatically decreasing bed numbers (Eastern Cape −27%, Limpopo −26%, Western Cape −21%).
Forensic facilities
In addition to beds in mental health facilities, there are 3.5 beds per 100,000 population for people with mental disorders in forensic inpatient units. Based on data from three provinces (Free State, KwaZulu-Natal and North West), 9% of users spend less than 1 year, 25% spend 1–4 years, 62% spend 5–10 years, and 3% spend more than 10 years in forensic inpatient units.
A map summarising the mental health facilities and poverty levels in all provinces is provided in Fig. 2. Poverty levels were reported by the Southern African Regional Poverty Network [31].
Mental health in Primary Health Care (PHC)
All provincial services are organised in line with the national policy of integrating mental health into PHC. In two provinces (Gauteng and KwaZulu-Natal), a mean of 5.5% of the training for medical doctors is devoted to mental health. According to the South African Nursing Council, 21% of undergraduate nurse training is devoted to mental health. Some post-qualification refresher training initiatives have been undertaken for PHC nurses, but no data were available on the percentage of PHC doctors and nurses who have received such training in mental health. Only in one province (Northern Cape) it was estimated that 80% of nurses had received such training. In another province (KwaZulu-Natal) nurses had received refresher training, but no records were kept of the numbers of nurses who were trained.
There was wide variability between provinces in the availability of assessment and treatment protocols for key mental health conditions (see Table 1). The general trend suggests wider availability of protocols amongst non-physician-based clinics. Referral guidelines do exist in all provinces, but the extent to which they are adhered to is not known.
There is also wide variation between provinces in the percentage of physician-based PHC doctors who make on average at least one referral per month to a mental health professional. Less than 20% of doctors in the Eastern Cape, 21–50% of doctors in KwaZulu-Natal, Northern Cape and Free State, and over 80% of doctors in the Western Cape and Gauteng make such referrals. The remaining provinces did not provide data. Only four provinces were able to report on the number of non-physician-based PHC clinics that make a referral to a higher level of care. Again there was wide variation, with Gauteng reporting 0%, Western Cape 1–20% and Free State and North West 51–80%. Of the two provinces that reported interactions between PHC doctors and mental health professionals, KwaZulu-Natal reported that 1–20% and the Free State reported that 21–50% of PHC doctors have such interactions in a month.
According to the South African Nursing Council, PHC nurses are allowed to prescribe but with restrictions (e.g., they are not allowed to initiate prescription but are allowed to continue prescription, or they are allowed to prescribe in emergencies only). These practices are dependent on drug schedules. PHC doctors are allowed to prescribe all medications on the EDL.
As for availability of psychotropic medicines, three provinces reported that over 80% of physician-based PHC clinics have at least one psychotropic medicine of each therapeutic category as set out in the EDL, and one province reported that 51–80% of these clinics have such medicines. In non-physician-based clinics, four provinces reported 81–100% availability, three provinces 51–80%, one province 21–50% and one province 0%.
Information systems in mental health services
Information systems are generally weak in most mental health services. In all of the provincial Department of Health services described above, there is no routine reporting of service utilisation by gender, age or diagnosis. If such data are collected, they are entered into users’ folders, and are not used for service planning.
Of the nine provinces, four indicated that there is no formally defined minimum data set of mental health items to be collected by health facilities (Western Cape, KwaZulu-Natal, Northern Cape and Mpumalanga). The remaining five provinces reported that a formally defined list of individual data items exists that ought to be collected by all mental health facilities. The extent of data collection is variable between mental health facilities and provinces (see Table 2).
In the Western Cape, KwaZulu-Natal and Limpopo, 67, 23 and 89% of outpatient facilities transmit data to the provincial Health Department, respectively. All other provincial Health Departments receive data from all mental hospitals, all psychiatric inpatient units in general hospitals, and all mental health outpatient facilities. However, only one of the nine provinces, the North West Province, produced a report from the data transmitted to the provincial Health Department.
Human resources
The total personnel working in mental health facilities are 11.95 per 100,000 population. Of these, 0.28 per 100,000 are psychiatrists, 0.45 other medical doctors (not specialised in psychiatry), 10.08 nurses, 0.32 psychologists, 0.40 social workers, 0.13 occupational therapists, and 0.28 other health or mental health workers (see Table 3).
Very few provinces were able to provide a breakdown of mental health staff by facility type. Those that were able to provide this information could only report on the locations of some staff categories in some locations. Where data are available, the trends are that mental hospitals appear to be better staffed than psychiatric inpatient units in general hospitals. For example, amongst nurses in Mpumalanga and Free State, there is an average of 0.6 nurses per bed in psychiatric inpatient units in general hospitals, in comparison to an average of 1.2 per bed in mental hospitals. For other psycho-social staff (psychologists, social workers and occupational therapists), there are an average of 0.03 per bed for psychiatric inpatient units in general hospitals in Mpumalanga, Free State and Limpopo, and 0.07 per bed in mental hospitals. The exception to this trend is the case of psychiatrists: in KwaZulu-Natal and Free State there is an average of 0.05 psychiatrists per bed in psychiatric inpatient units in general hospitals, in comparison to an average of 0.02 psychiatrists per bed in mental hospitals.
The distribution of human resources between urban and rural areas is disproportionate. Based on data from only two provinces (Free State and North West), the density of psychiatrists in or around the largest city is 3.6 times greater than the density of psychiatrists in the entire province, a trend which is consistent with past research [32] and anecdotal evidence from other provinces. The distribution of nurses between urban and rural areas is not known.
There was a general lack of data regarding either professional training or continuing professional development (CPD) after qualification in all provincial Departments of Health. However, the HPCSA and the South African Nursing Council were able to provide data on the number of new professional registrations in 2005. Per 100,000 population, these include 0.06 psychiatrists, 5.58 other doctors, 5.32 registered nurses, 10.45 enrolled nurses, 12.41 enrolled nursing auxiliaries, 0.8 psychologists, 4.96 nurses with at least 1 year of training in mental health and 0.48 occupational therapists. In KwaZulu-Natal and Free State, it was estimated that up to 20% of psychiatrists emigrate to other countries within 5 years of the completion of their training.
The Health Professions Council has implemented a CPD scheme for medical doctors, psychologists and occupational therapists, which covers both private and public sectors. Professionals are required to undertake certain continuing education and supervision activities each year in order to remain registered with the HPCSA. However, no data are kept regarding the amount of CPD training undertaken each year for all registered professionals, as audits are conducted each year on a group of randomly selected professionals.
Quality of care
Because the WHO-AIMS instrument provides only input and process data, it is not possible to thoroughly assess the quality of care received in South African mental health services. However, certain proxy measures such as efficiency, accessibility and coverage may provide indications of service quality. Regarding efficiency, an important indicator is the proportion of financial resources allocated to mental hospitals, as these institutions are commonly acknowledged as making inefficient use of scarce resources [33]. Based on data from four provinces, 86% of mental health expenditure is allocated to mental hospitals. Regarding accessibility, it is widely acknowledged that mental hospitals are geographically inaccessible and frequently stigmatising institutions [10]. Bed distribution between mental hospitals and other facility types is, therefore, an important indicator of accessibility of inpatient care. Across all provinces, a mean of 56% of inpatient beds are located in mental hospitals. Furthermore, the median proportion of beds in or near the largest city in a province was 1.46 (provincial range 0.63–4.78), based on data from seven provinces, indicating difficulty accessing inpatient care, particularly for those in rural areas. This is mirrored in staff distributions, which indicate that there are 3.6 times as many psychiatrists working in urban areas as rural areas, per 100,000 population. These data indicate major rural/urban disparities in access to care. Regarding economic accessibility, as clinic attendance is free for those who are unable to pay, and psychotropic medication costs 0.5% of the daily minimum wage for amitriptyline and 0.7% of the daily minimum wage for chlorpromazine, economic barriers appear to present themselves more in the form of high transport costs than treatment costs. Based on mental health outpatient attendance figures, coverage appears to be very low, with 1.7% annual treated prevalence.
Public education
There is a coordinating body to oversee public education and awareness campaigns on mental health and mental disorders in South Africa, namely the Department of Health. Advocacy and public awareness programmes are being run by the National Department of Health, but are limited by resources. The department is assisted by various NGOs, including the SAFMH, the South African Depression and Anxiety Group and other professional, consumer and advocacy bodies.
Government agencies and NGOs have promoted public education and awareness campaigns in the last 5 years in all provinces. However, only the Western Cape, Free State and Gauteng reported the involvement of professional associations in these campaigns, and only the Western Cape reported the involvement of private trusts, foundations and international agencies. These campaigns have targeted the general population, children, adolescents, women, trauma survivors and other vulnerable or minority groups.
In addition, there have been public education and awareness campaigns targeting professional groups in Gauteng and the Western Cape, including health care providers, complimentary/alternative/traditional healers, teachers, social service staff, leaders and politicians and other professional groups linked to the health sector.
In the Free State, all these groups have been targeted with the exception of social service staff and politicians. In Mpumalanga, these campaigns have been limited to teachers, politicians and other professional groups linked to the health sector. In North West, campaigns have targeted only health professionals. No other provinces have conducted public education and awareness campaigns for mental health.
Discussion
South African mental health services are marked by a number of contradictory elements. On the one hand, mental health care has been included as a priority programme within national health policy; some effort has been directed at integrating basic mental health care into service provision at PHC level; and psychotropic medications are relatively widely available and affordable within existing services. Other important advances have also been made since the election of a democratic government in 1994. Mental health service priorities are clearly defined in the country’s 1997 White paper on health service transformation, a national mental health policy guideline was drafted in 1997, and the Mental Health Care Act (2002) promulgated in 2004 is in keeping with international human rights standards. The latter has introduced a number of reforms such as the establishment of Review Boards to protect human rights of people with mental disorders in health establishments, and the identification of designated mental health facilities, including 72 h observation facilities in general hospitals. In the area of human resources, the HPCSA has introduced a system of CPD to encourage mental health professionals to update their clinical skills and provide ethical, evidence-based services. Steps are also being taken to ensure that health skills are more readily available where needed, e.g., through the introduction of compulsory community service after training for psychologists, doctors and occupational therapists, and the introduction of new categories of health personnel, e.g., a 4-year degree registered counsellor within the psychology profession.
On the other hand, there are several ongoing problems. First, there is widespread inequality between provinces in the resources available for mental health care, including staffing and inpatient beds. This is consistent with previous studies of staff and inpatient bed distributions between provinces [23, 25] and with inequalities in the wider health sector in South Africa [34]. Very little appears to have changed since these studies were conducted 8 years ago, in that under-resourced provinces such as the Eastern Cape, Limpopo, Mpumalanga, North West and the Northern Cape stand in stark contrast to relatively well resourced provinces such as Free State, Gauteng, KwaZulu-Natal and the Western Cape. The findings regarding mental health resource distribution continue to reflect historical legacies of provincial boundaries under apartheid, as reported in previous studies [23]. For example, forensic bed numbers in the three predominantly rural provinces around Gauteng province (North West, Limpopo and Mpumalanga) are negligible compared to Gauteng, and reflect these provinces’ continued reliance on Gauteng for forensic services. These resource distributions reflect the old provincial boundaries of the apartheid era province of the Transvaal. As stated in previous studies, there is an urgent need to improve resource allocations in under-resourced provinces, particularly in rural areas, to improve equity between provinces and improve access to services.
Secondly, the service platform for mental health continues to be dominated by mental hospitals, in contrast to other health programmes which have more readily been integrated into the PHC model at regional and district levels. As shown in Fig. 1, the predominant form of inpatient mental health service provision continues to be based on mental hospitals. There have been developments in service provision in community residential facilities and psychiatric inpatient units in general hospitals compared to previous studies [25], but this still falls far short of the aims of the 1997 White Paper for Health that calls for a community-based service, integrated into PHC [19]. These challenges are reflective of difficulties in building PHC in wider health sector reform in South Africa [35].
Thirdly, there is a striking absence of reliable, routinely collected data that can be used to plan services and redress current inequalities, as reported in previous studies [22, 24].
The findings of this study also appear to indicate continued unmet need for mental health care in South Africa. For example, mental health outpatient attendance figures indicate an annual treated prevalence of 1.7% of the total population. If this figure is compared to the annual prevalence estimate of 16.5% for CMDs in adults alone [2], this indicates large numbers of people with needs for care who do not receive mental health services. This is confirmed by epidemiological data which indicate that only 28% of people with moderate–severe CMDs received mental health care in the last year [2].
The wide variation in resources between (and within) provinces appears to be at least partially symptomatic of the absence of a nationally accepted mental health policy, with a lack of consensus on the official status of the 1997 policy, and the redrafting of a new policy at an early stage of development. Without clear imperatives from the National Department of Health, provincial departments are free to address mental health according to their own priorities. This results in inconsistent approaches to resource allocation, inconsistent data collection, lack of standardisation of the training of PHC staff in mental health, and a lack of formalised inter-sectoral collaboration with other departments and stakeholders. These problems are reinforced by current financing mechanisms, in which provincial mental health budgets are allocated from national tax-based health budgets. There are few financial incentives for provincial Departments of Health to increase efficiency or resource allocation for mental health services. Thus, while the Mental Health Care Act (2002) has legislated reforms in the form of Review Boards and 72 h assessment facilities at district hospitals, there have been limited budget allocations to community mental health care in a manner advocated by the act. This trend is reflected in broader health sector financing, where calls have been made to link district health funding improvements to performance and efficiency [36].
In comparison to previous South African studies, total bed/population ratios have declined from 48 per 100,000 population in 1997 [25] to 28 per 100,000 population in 2005. There are no indications that this reduction in bed numbers has been accompanied by a substantial increase in community-based services. Furthermore, total staff numbers appear to have declined over this period, with 19.5 total mental health staff, 0.4 psychiatrists and 15.6 nurses reported per 100,000 population in 1997 [23], while this study found 11.95 total mental health staff, 0.3 psychiatrists and 10.1 nurses per 100,000 population in 2005 (Table 3). These findings indicate an overall decline in mental health resources over this period, which is of grave concern. The finding for human resources is consistent with research on wider health sector reform, which indicates that the South African health workforce is substantially weaker now than it was in the mid-1990s [37].
Comparing these findings with other African countries, South Africa fares favourably. Only 50% of African countries have a mental health policy and while 80% have mental health legislation, only 30% of this legislation has been reformed since 1990 [38]. Furthermore, 70% of African countries spend less than 1% of their meagre health budgets on mental health [38]. However, in relation to other middle-income countries, the findings appear comparable. For example, Brazil, India and Mexico spend 2.6, 2.1 and 1% of their health budgets on mental health, respectively; and similarly to South Africa, all three of these countries have mental health policies and legislation in place [39].
There are a number of limitations to this study, which need to be noted. First, there was wide variability between provinces in the number of nurses per 100,000 population (provincial range 1.1–20.6), which may be partially attributed to differing definitions of nurses between provinces, in spite of the clear definition provided in the instrument. This may reflect a broader trend of inconsistent record keeping and/or information systems across the provinces. For example, although provinces were able to provide the numbers of nurses working in specialist mental health facilities, such as mental hospitals, it was more difficult to provide numbers of nurses providing mental health services within integrated general health facilities. Secondly, Gauteng was not able to provide data on the number of psychologists, social workers or occupational therapists. As a highly urbanised province, with a large population, it is likely that there is a higher concentration of these professionals in this province than in other provinces. The resulting underestimation at the national level is, therefore, likely to be greater than would have been the case had the missing data been from a less urbanised province. Thirdly, the study reported input and process indicators, but not outcome indicators. Routine outcome data are not currently available from provincial mental health services in South Africa. It is important that information systems are developed to facilitate the collection and analysis of outcome data in future. Fourthly, no provincial information systems were able to report service utilisation data by diagnosis, which makes it impossible, amongst other things, to calculate the treatment gap by diagnosis. All these limitations reinforce the need to develop reliable routine information systems for monitoring mental health services in South Africa.
The WHO-AIMS instrument provided a useful means of assessing national mental health systems in South Africa, using standardised items that were comparable across provinces and with other countries. The instrument is receiving increasing international recognition and use [26], although some of its limitations have been identified as a neglect of the politics of mental health policy development, underestimation of the role of culture in mental health care utilisation and questionable measurement validity [40]. It is clear that an instrument of this nature is not designed to provide detailed analyses of political and cultural factors, and in the case of South Africa, we have used qualitative methodologies to explore these aspects in other papers [41, 42]. Other methods have been developed for exploring explanatory models and public perceptions in relation to mental health policy, e.g., in Kenya [43]. Measurement validity is a limitation in some items, e.g., assessing the quality of training, or regulatory aspects of medication supply [40], and this could perhaps be improved in future versions of the instrument.
This study highlights the need for further research, including epidemiological studies that examine treated prevalence; mental health services research that includes more sophisticated methods of sampling representative geographical areas [44] in circumstances of limited information systems; and intervention studies that evaluate the development of mental health systems, e.g., national policy development, information systems and the integration of mental health into PHC.
Conclusion
In comparison to many other low- and middle-income countries, South Africa is an interesting case study for mental health systems. Unlike many other low- and middle-income countries, particularly those in Africa [39], legislation and some level of policy commitment are in place to advocate for the development of community-based care and the protection of human rights for those with mental disabilities. However, there remain major challenges of policy implementation and widespread inequalities in available mental health service resources.
In this light, a number of policy and service development initiatives are required. First, there is a need for stronger national leadership to develop a national mental health policy which provides a clear framework for public mental health service development. Such national policy should recommend levels of provision for provinces, facilitate systems to monitor the implementation of national policy, and harness political will and administrative investment in mental health on par with other health programmes. Secondly, capacity needs to be built for mental health programme managers and other officials involved in planning and monitoring of mental health services at provincial and district level. Thirdly, a nationally agreed minimum data set needs to be put in place and an information system established, in order to consistently monitor mental health service delivery and outcomes at provincial and district level.
References
Bradshaw D, Norman R, Schneider M (2007) A clarion call for action based on refined DALY estimates for South Africa. Editorial. S Afr Med J 97:438–440
Williams DR, Herman A, Stein DJ, Heeringa SG, Jackson PB, Moomal H, Kessler RC (2007) Prevalence, service use and demographic correlates of 12-month psychiatric disorders in South Africa: the South African Stress and Health Study. Psychol Med 38:211–220
Kleintjes S, Flisher A, Fick M, Railon A, Lund C, Molteno C, Robertson B (2006) The prevalence of mental disorders among children, adolescents and adults in the Western Cape, South Africa. S Afr Psychiatr Rev 9:157–160
Truth and Reconciliation Commission (2000) Report of the Truth and Reconciliation Commission of South Africa. McMillan, London
Kaminer D, Stein DJ, Mbanga I, Zungu-Dirwayi N (2001) The Truth and Reconciliation Commission in South Africa: relation to psychiatric status and forgiveness among survivors of human rights abuses. Br J Psychiatry 178:373–377
Stein DJ (1998) Psychiatric aspects of the truth and reconciliation commission in South Africa. Br J Psychiatry 173:455–457
Bhorat H, Kanbur R (2005) Poverty and well-being in post-apartheid South Africa: an overview of data, outcomes and policy. Development Policy Research Unit, University of Cape Town, Cape Town
Patel V, Kleinman A (2003) Poverty and common mental disorders in developing countries. Bull World Health Organ 81:609–615
Lopez DA, Mathers DC, Ezzati M, Jamison TD, Murray JLC (2006) Global burden of disease and risk factors. Oxford University Press and The World Bank, New York
WHO (2001) World Health Report 2001, mental health: new understanding, new hope. WHO, Geneva
Patel V, Chisholm D, Rabe-Hesketh S, Dias-Saxena F, Andrew G, Mann A (2003) The efficacy and cost-effectiveness of a drug and psychological treatment for common mental disorders in general health care in Goa, India: a randomised controlled trial. Lancet 361:33–39
Patel V, Araya R, Bolton P (2004) Editorial: treating depression in the developing world. Trop Med Int Health 9:539–541
Bolton P, Bass J, Neugebauer R, Verdeli H, Clougherty KF, Wickramaratne P, Speelman L, Ndogoni L, Weissman M (2003) Group interpersonal psychotherapy for depression in rural Uganda: a randomized controlled trial. J Am Med Assoc 289:3117–3124
Siskind D, Bolton P, Kim J (2007) Country contextualization of cost-effectiveness analysis of treatments for depression in Chile and Uganda using a Markov model. J Mental Health Policy Econ 10:S40–S41
Patel V, Araya R, Chatterjee S, Chisholm D, Cohen A, De Silva M, Hosman C, McGuire H, Rojas G, Van Ommeren M (2007) Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet 370:991–1005
WHO (1996) Psychosocial rehabilitation: a consensus statement. WHO, Geneva
Department of National Health (1996) Restructuring the national health system for universal primary health care. Department of National Health, Pretoria
Lund C, Flisher AJ (2003) Community/hospital indicators in South African public sector mental health services. J Mental Health Policy Econ 6:181–187
Department of Health (1997) White paper for the transformation of the health system in South Africa. Government Gazette, Pretoria
Department of Health (1997) National health policy guidelines for improved mental health in South Africa. Department of Health, Pretoria
WHO (2005) WHO resource book on mental health, human rights and legislation. WHO, Geneva
Lund C, Flisher AJ (2001) South African mental health process indicators. J Mental Health Policy Econ 4:9–16
Lund C, Flisher AJ (2002) Staff/population ratios in South African public sector mental health services. S Afr Med J 92:161–164
Lund C, Flisher AJ (2002) Staff/bed and staff/patient ratios in South African public sector mental health services. S Afr Med J 92:157–161
Lund C, Flisher AJ, Lee T, Porteus KA (2002) Bed/population ratios in South African public sector mental health services. Social Psychiatry Psychiatr Epidemiol 37:346–349
Saxena S, Lora A, Van Ommeren M, Barrett T, Morris J, Saraceno B (2007) WHO’s Assessment Instrument for Mental Health Systems: collecting essential information for policy and service delivery. Psychiatr Serv 58:816–821
Lloyd-Evans B, Johnson S, Slade M (2007) Assessing the content of mental health services: a review of measures. Social Psychiatry Psychiatr Epidemiol 42:673–682
WHO (2005) WHO Assessment Instrument for Mental Health Systems (AIMS) Version 2.1. WHO, Geneva
Lund C, Flisher AJ (2006) Norms for mental health services in South Africa. Social Psychiatry Psychiatr Epidemiol 41:587–594
Lund C, Kleintjes S, Campbell-Hall V, Mjadu S, Petersen I, Bhana A, Kakuma R, Mlanjeni B, Bird P, Drew N, Faydi E, Funk M, Green A, Omar M, Flisher AJ (2008) Mental health policy development and implementation in South Africa. Phase 1 Country Report. Mental Health and Poverty Project, University of Cape Town, Cape Town
Southern African Regional Poverty Network (2004) Fact sheet: poverty in South Africa. Southern African Regional Poverty Network, Pretoria
Flisher AJ, Riccitelli G, Jhetam N, Robertson BA (1997) A survey of professional activities of psychiatrists in South Africa. Psychiatr Serv 48:707–709
Saxena S, Thornicroft G, Knapp M, Whiteford HA (2007) Resources for mental health: scarcity, inequity and inefficiency. Lancet 370:878–889
Day C, Gray A (2008) Health and related indicators. In: Barron P, Roma-Reardon J (eds) South African health review 2008. Health Systems Trust, Durban, pp 239–396
Kautzky K, Tollman SM (2008) A perspective on Primary Health Care in South Africa. In: Barron P, Roma-Reardon J (eds) South African health review 2008. Health Systems Trust, Durban, pp 17–30
Blecher M, Day C, Dove S, Cairns R (2008) Financing in the public sector. In: Barron P, Roma-Reardon J (eds) South African health review 2008. Health Systems Trust, Durban, pp 179–194
Lehmann U (2008) Strengthening human resources for primary health care. In: Barron P, Roma-Reardon J (eds) South African health review 2008. Health Systems Trust, Durban, pp 163–178
WHO (2005) Atlas: mental health resources in the world. WHO, Geneva
Jacob KS, Sharan P, Mirza I, Garrido-Cumbrera M, Seedat S, Mari JJ, Sreenivas V, Saxena S (2007) Mental health systems in countries: where are we now? Lancet 370:1061–1077
Hamid H, Abanilla K, Bauta B, Huang KY (2008) Evaluating the WHO Assessment Instrument for Mental Health Systems by comparing mental health policies in four countries. Bull World Health Organ 86:467–473
Draper C, Lund C, Kleintjes S, Funk M, Omar M, Flisher AJ, the MHaPP Research Programme Consortium (2009) Mental health policy in South Africa: development process and content. Health Policy Plan. doi:10.1093/heapol/czp027
Petersen I, Bhana A, Campbell-Hall V, Mjadu S, Lund C, Kleintjes S, Hosegood V, Flisher AJ, the Mental Health and Poverty Research Programme Consortium (2009) Planning for district mental health services in South Africa. A situational analysis of a district site. Health Policy Plan. doi:10.1093/heapol/czn049
Muga F, Jenkins R (2008) Public perceptions, explanatory models and service utilisation regarding mental illness and mental health care in Kenya. Social Psychiatry Psychiatr Epidemiol 43:469–476
Priebe S, Saidi M, Kennedy J, Glover G (2008) How to select representative geographical areas in mental health service research. Social Psychiatry Psychiatr Epidemiol 43:1004–1007
Acknowledgments
This study was made possible by funding provided by the Department for International Development (DfID) for a Research Programme Consortium entitled “The Mental Health and Poverty Project (MHaPP): Mental health policy development and implementation in four African countries” (DfID contract number: RPC HD6 2005–2010). The views expressed are those of the authors and not necessarily those of DfID. We would like to thank Dr Shekhar Saxena and Dr Jodi Morris of the Department of Mental Health and Substance Abuse, WHO for their assistance in reviewing the WHO-AIMS data for this study; our national and provincial government and NGO partners for their assistance in gathering the data; and Mr Luis Eduardo Sevilla for design of the map.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The Mental Health and Poverty Project (MHaPP) is a Research Programme Consortium (RPC) funded by the UK Department for International Development (DfID) (RPC HD6 2005–2010) for the benefit of developing countries. The views expressed are not necessarily those of DfID. RPC members include Alan J. Flisher (director) and Crick Lund (coordinator) [University of Cape Town, Republic of South Africa (RSA)]; Therese Agossou, Natalie Drew, Edwige Faydi and Michelle Funk (World Health Organization); Arvin Bhana (Human Sciences Research Council, RSA); Victor Doku (Kintampo Health Research Centre, Ghana); Andrew Green and Mayeh Omar (University of Leeds, UK); Fred Kigozi (Butabika Hospital, Uganda); Martin Knapp (University of London, UK); John Mayeya (Ministry of Health, Zambia); Eva N. Mulutsi (Department of Health, RSA); Sheila Zaramba Ndyanabangi (Ministry of Health, Uganda); Angela Ofori-Atta (University of Ghana); Akwasi Osei (Ghana Health Service); and Inge Petersen (University of KwaZulu-Natal, RSA).
Rights and permissions
About this article
Cite this article
Lund, C., Kleintjes, S., Kakuma, R. et al. Public sector mental health systems in South Africa: inter-provincial comparisons and policy implications. Soc Psychiat Epidemiol 45, 393–404 (2010). https://doi.org/10.1007/s00127-009-0078-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-009-0078-5