Abstract
Background
Psychiatric disorders and hypertension both independently increase risk for heart disease, cardiac events, and healthcare utilization. However, the contribution of specific psychiatric disorders to healthcare utilization in persons with hypertension is unknown.
Objective
To evaluate associations between psychiatric disorders and receipt of hospital care in people with hypertension.
Design
Cross-sectional epidemiologic survey.
Subjects
A total of 8,812 hypertensive individuals drawn from a randomly selected sample of 43,093 US adults.
Main outcomes
Participants were assessed in-person for a range of mental disorders (using the Diagnostic and Statistical Manual of Mental Disorders-IV), hypertension status (self-report), and past-year occurrence of emergency room treatment and overnight hospital stay (self-report).
Results
After controlling for demographics and clinical variables, persons having any lifetime mood, anxiety, or personality disorders had increased likelihood of emergency room treatment [odds ratios (ORs) = 1.26, 1.18, and 1.47, respectively]. Persons having any mood or personality disorder had increased likelihood of overnight hospital stay (ORs = 1.24 and 1.31, respectively). The specific disorders significantly associated with emergency room treatment were lifetime major depression, lifetime manic disorder, past-year major depression, past-year manic disorder, past-year panic disorder without agoraphobia, and paranoid, histrionic, antisocial, obsessive–compulsive personality disorders, with ORs ranging from 1.25 to 2.41. The specific disorders significantly associated with overnight hospital stay were lifetime dysthymia, lifetime manic disorder, past-year major depression, past-year manic disorder, and histrionic, antisocial, and paranoid personality disorders, with ORs ranging from 1.40 to 1.87.
Conclusion
Results suggest that addressing mental health problems in persons with hypertension may decrease healthcare utilization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) is the most common cause of death in industrialized countries. Hypertension is the most frequent treatable CVD risk factor, and it affects 28% of the US population [32]. Psychiatric disorders are also prospectively associated with CVD, with depressive disorders showing the strongest and most consistent relationships [10].
Vascular disease and psychiatric disorders each independently result in considerable healthcare utilization. Recent US data show that circulatory diseases were the most frequent primary diagnosis for short hospital stays [5], accounting for 26% of non-obstetric hospitalizations admitted through the emergency department [4]. Psychiatric disorders were the sixth most frequent accounting for 6% of hospitalizations.
Of the psychiatric disorders, depression is the most widely studied in relation to healthcare utilization and cost. Unutzer [29] found that among patients with one or more chronic medical diseases, depression was associated with approximately the same proportional increase of total costs at all levels of medical morbidity. Moreover, even among those who have high utilization rates, depressed high utilizers have higher medical costs than nondepressed high utilizers [16]. Prospective studies show that healthcare for depressed persons costs approximately twice that of nondepressed persons [28]. While not all studies separated medical healthcare costs from mental healthcare costs, evidence indicates that depression increases costs across every component of healthcare delivery (e.g., pharmacy, primary care, medical inpatient, laboratory). Furthermore, specialty mental health and substance abuse treatment only accounts for a small percentage of the difference in total costs [28].
While the literature is generally consistent in documenting a relationship between psychiatric disorders and healthcare utilization, there are limitations in the literature. First, very little is known about the relationship between personality disorders and healthcare utilization. Given the chronic and pervasive nature of personality disorders, their association with utilization may be important. Second, with very few exceptions, most studies have relied on symptom questionnaires or medical claims data for an indication of mental health problems including depression (cf. [20]). Symptom questionnaires do not allow for a diagnosis per se, and medical claims data are vulnerable to several biases including healthcare provider errors in screening, detection, diagnosis, and recording. Second, only limited epidemiological data exist regarding the associations between healthcare utilization and disorders other than depression, such as anxiety and personality disorders. The Epidemiological Catchment Area (ECA) [20] study has the most relevant data in this regard. In that study, the rate of current psychiatric disorders among medical users was significantly higher than among nonusers (22 vs. 17%). However, the ECA study collapsed all psychiatric diagnoses into four categories, which precludes examination of specific disorders. Further, that study did not account for clinical characteristics such as overweight, smoking, or substance use, which covary with some psychiatric disorders and may confound results.
Third, some psychiatric conditions such as depression show long-term associations with emotional and physical well-being, even after diagnostic criteria are no longer met. For example, depression is associated with cellular alterations that remain abnormal even in remission [25, 27]. Other problems associated with depression, which are observable after the depressive episode remits include markers of CVD [1, 18, 31], metabolic alterations [30], physical symptoms [9], and subclinical depressive symptoms [19]. Therefore, investigation of both lifetime and more recent (e.g., past year) psychiatric disorder is critical, yet scant data exist that address the acuity of the psychiatric disorder and its association with healthcare utilization. Finally, some psychiatric disorders are more common in chronic illnesses. However, the vast majority of studies of psychiatric disorders and healthcare utilization do not select, limit analysis to, or control for chronic medical illnesses (cf. [28]). Given the high prevalence and chronic nature of hypertension, and its contribution to CVD risk along with psychiatric disorders, investigation of hypertensive individuals specifically is warranted.
One might expect that in an enriched sample of medically compromised patients, the relationship between psychiatric disorders and healthcare utilization may be weak or nonexistent. We hypothesize that even in this medical sample of individuals who may already have elevated utilization rates by virtue of hypertension, the relationship between psychiatric disorders and utilization is still detectable. We further hypothesize that this relationship will emerge even after controlling for numerous demographic and clinical characteristics that may affect utilization.
The purpose of this study was to replicate and extend results of prior studies examining relationships between psychiatric disorders and healthcare utilization. The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) [14] is the largest psychiatric epidemiology study conducted, and it assessed a wide range of lifetime and past-year Diagnostic and Statistical Manual of Mental Disorders-revision IV (DSM-IV) mood, anxiety, and substance use disorders, as well as seven personality disorders. This dataset provides a unique opportunity to examine the associations between specific psychiatric disorders and healthcare utilization in hypertensives while controlling for important demographic and clinical characteristics.
Method
Sample
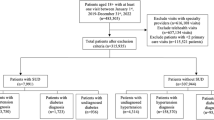
In 2001–2002, the National Institute of Alcohol Abuse and Alcoholism conducted the NESARC, a nationally representative face-to-face survey of 43,093 civilian non-institutionalized adults age 18 and older living in the United States. The response rate was 81%. Young adults (18–24 years) and African-Americans and Hispanics were oversampled. Data were weighted to account for oversampling and design characteristics of the survey, and adjusted based on the 2000 Decennial Census in terms of socioeconomic variables such as age, sex, race-ethnicity, and region of the country [14].
Hypertension assessment
Participants were asked about the presence of a variety of medical conditions. Regarding hypertension, they were asked, “In the past 12 months, have you had high blood pressure or hypertension?” Participants who answered yes were further queried, “Did a doctor or other health professional tell you that you had high blood pressure or hypertension?” Only those responses that endorsed a healthcare provider diagnosis were considered hypertension cases, and 8,812 (21.3%) of participants were classified as such. NESARC was conducted between 2001 and 2002. The Centers for Disease Control (CDC) and Prevention reported that between 1999 and 2002, 28.6% of US adults had hypertension, and 63.4% of them were aware of it, or 18.1% of the US population [2]. Thus, the prevalence of patient-identified hypertension in the sample reported here (21.3%) reasonably approximates the prevalence of patient-identified hypertension in the US population at that time (18.1%). However, it is likely that the NESARC sample underestimated the presence of true hypertension, as the CDC sample did.
DSM-IV psychiatric disorder assessment
The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version (AUDADIS-IV) assessed lifetime and past-year DSM-IV mood and anxiety disorders. Mood disorders included were major depressive episode, dysthymia, manic episode, and hypomanic episode. Anxiety disorders evaluated were generalized anxiety disorder, panic disorder without agoraphobia, panic disorder with agoraphobia, agoraphobia without history of panic disorder, social phobia, and specific phobia. Only primary diagnoses were included in the analyses. Thus, mood and anxiety disorders that were substance-induced or due to a general medical condition or bereavement (about 1% of cases) were not included. Reliability and validity of AUDADIS-IV assessment of mood and anxiety disorders are fair to good [11, 13].
Seven personality disorders were also evaluated: antisocial, avoidant, dependent, obsessive–compulsive, paranoid, schizoid, and histrionic. Respondents must have met the required number of DSM-IV criteria and had at least one symptom cause social or occupational dysfunction in order to receive a personality disorder diagnosis. Respondents were instructed to not include times when they were physically ill, depressed, anxious, manic, drinking heavily, using medicine or drugs, or experiencing withdrawal symptoms in considering their responses. Reliability and validity of the AUDADIS-IV personality disorder diagnoses are fair to good [22].
To investigate number of psychiatric disorders, two variables were computed. The first summed any lifetime mood disorder + any lifetime anxiety disorder + any personality disorder (range = 0–3 disorders). The second summed any past-year mood disorder + any past-year anxiety disorder + any personality disorder (range = 0–3).
The AUDADIS-IV also assessed DSM-IV diagnoses of nicotine dependence, and abuse and dependence for alcohol and ten classes of drugs: cannabis, cocaine, heroin, opiates (other than heroin or methadone), stimulants, tranquilizers, sedatives, hallucinogens, inhalants/solvents, and other drugs. Respondents must have met at least one of four abuse criteria in the 12-month period preceding the interview and/or before the 12-month period to receive a past-year or lifetime diagnosis of alcohol or drug abuse. AUDADIS-IV dependence diagnoses required respondents to meet at least three of seven dependence criteria during the past year and/or prior to the past year. All drug use disorders other than nicotine and alcohol were classified into one general category of “any drug use disorder,” because prevalence rates of individual drug use disorders were low. Test–retest reliability and validity of the AUDADIS-IV nicotine, alcohol, and drug use disorders are good to excellent [11, 12, 15].
Healthcare utilization
Participants were asked two questions regarding healthcare utilization. (1) “Not counting hospitalization for delivery of a healthy live-born infant, how many times did you receive medical care or treatment in a hospital emergency room in the past 12 months?” (2) “Not counting hospitalization for delivery of a healthy live-born infant, how many separate times did you stay in a hospital overnight or longer in the past 12 months?” Responses were recoded dichotomously as yes emergency room treatment versus no emergency room treatment, and yes overnight stay versus no overnight stay.
Body mass index
Body mass index was computed from self reported height and weight by dividing weight in kilograms by square of height in meters. Individuals were classified into one of four BMI categories [23]: underweight, BMI < 18.5; normal weight, BMI of 18.5–24.9; overweight, BMI = 25.0–29.9; and obese, BMI > 30.0.
Statistical analyses
The first dependent variable we examined was past-year emergency room treatment. Participants were categorized by emergency room treatment, yes versus no. Differences between these groups in demographics were analyzed using cross-tabulations. Next, a model predicting emergency room treatment from lifetime psychiatric disorders was evaluated. This model included any lifetime mood disorder, any lifetime anxiety disorder, any personality disorder, any lifetime alcohol use disorder, and any lifetime drug use disorder. Next, a model predicting emergency room treatment from past-year psychiatric disorders was evaluated. This model included any past-year mood disorder, any past-year anxiety disorder, any personality disorder, any past-year alcohol use disorder, and any past-year drug use disorder. These two multivariate models controlled for demographics (age, sex, race-ethnicity, education, marital status, income, insurance status, region of the country and urbanicity). They also controlled for clinically relevant characteristics (BMI and lifetime nicotine dependence).
When the overall association for any lifetime or any past-year mood, anxiety, or personality disorder was significant, additional models tested associations between each independent psychiatric disorder, using the same covariates as above. For example, if any lifetime mood disorder significantly predicted emergency room treatment, then all individual lifetime mood disorders were simultaneously entered into a new model predicting emergency room treatment, along with demographic and clinical covariates.
Finally, two models examined the additive effect of multiple psychiatric disorders. A model predicting emergency room treatment from number of lifetime psychiatric disorders was evaluated. Then a model predicting emergency room treatment from number of past-year psychiatric disorders was evaluated. These models controlled for the same demographic and clinical covariates as listed above.
The second dependent variable examined was past-year overnight hospital stay, using the same sequence of analyses. Participants were categorized by overnight hospital stay, yes versus no. Differences between these groups in demographics were analyzed using cross-tabulations. Next, a model predicting overnight hospital stay from lifetime psychiatric disorders was evaluated. This model included any lifetime mood disorder, any lifetime anxiety disorder, any personality disorder, any lifetime alcohol use disorder, and any lifetime drug use disorder, and the covariates listed above. Next, a model predicting overnight hospital stay from past-year psychiatric disorders was evaluated. This model included any past-year mood disorder, any past-year anxiety disorder, any personality disorder, any past-year alcohol use disorder, any past-year drug use disorder, and the covariates listed above.
When the overall association for any lifetime or any past-year mood, anxiety, or personality disorder was significant, subsequent analysis examined associations between each independent psychiatric disorder, using the same covariates as above. For example, if any lifetime mood disorder significantly predicted overnight hospital stay, then all individual lifetime mood disorders were simultaneously entered into a new model predicting overnight hospital stay, along with demographic and clinical covariates.
Finally, two models examined the additive effect of multiple psychiatric disorders. A model predicting overnight hospital stay from number of lifetime psychiatric disorders was evaluated. Then a model predicting overnight hospital stay from number of past-year psychiatric disorders was evaluated. These models controlled for the same demographic and clinical covariates as listed above.
Odds ratios (ORs) and 95% confidence intervals (CIs) are presented for each independent variable. SUDAAN, a software package that uses Taylor series linearization to adjust for the complex sampling methodology, was used for analyses [26].
Results
DSM-IV psychiatric disorders
Rates of single and multiple psychiatric disorders were computed; 5,577 of the 8,812 respondents (63.4%) had no lifetime psychiatric disorder, 1,878 (21.3%) had one lifetime psychiatric disorder, 889 (10.1%) had two lifetime psychiatric disorders, and 449 (5.2%) had three lifetime psychiatric disorders. The respective rates for past-year psychiatric disorder were 6,360 (72.2%) 1,623 (18.4%), 597 (6.8%), and 223 (2.6%).
Healthcare utilization
Rates of past-year overnight hospitalization and ER visit were computed; 2,561 (29.1%) endorsed past-year emergency room treatment and 1,857 (21.1%) endorsed past-year overnight hospital stay. Past-year overnight hospitalization and ER visit were significantly related. Of those who had a past-year overnight hospitalization, 65.55% were also treated in ER, χ2(1) = 147.07, P < 0.001).
Specific DSM-IV psychiatric disorders and past-year emergency room treatment
Table 1 shows demographic and clinical characteristics of respondents based on past-year emergency room treatment. Several demographics differed by emergency room treatment categories, with emergency room-treated individuals being in lower income brackets, more frequently unmarried, and more likely ethnic minority than the group not treated in the emergency room. African-Americans were more likely to be treated in the emergency room than were Whites.
Table 1 also shows ORs and 95% CIs from logistic regression with past-year emergency room treatment predicted from lifetime psychiatric disorders. Controlling for all demographics and clinical characteristics listed in Table 1, those diagnosed with any lifetime mood disorder or any personality disorder were more likely to report receiving treatment in an emergency room. Those diagnosed with any lifetime anxiety disorder were marginally more likely to report receiving treatment in an emergency room (95% CI 1.00–1.40).
Table 2 shows that controlling for all demographics and clinical characteristics listed in Table 1, those diagnosed with any past-year mood disorder or any past-year anxiety disorder were more likely to report receiving treatment in an emergency room. (Note that the results for any lifetime disorders in Tables 1 and 2 are exactly the same because they reflect the same regressions.) Table 2 also shows that controlling for the same covariates, the following mood disorders were significantly associated with a greater likelihood of emergency room treatment: lifetime major depression, lifetime manic disorder, past-year major depression, past-year manic disorder. The following personality disorders were significantly associated with greater likelihood of emergency room treatment: paranoid, histrionic, antisocial, and obsessive–compulsive personality disorders. Of the anxiety disorders, only lifetime panic disorder without agoraphobia and past-year panic disorder without agoraphobia was associated with greater likelihood of emergency room treatment.
Multivariate analyses were then conducted predicting emergency room treatment from number of lifetime psychiatric disorders along with all covariates. Compared to those with no lifetime psychiatric disorder (reference group), individuals with one disorder (OR = 1.22; 95% CI = 1.05–1.41), two disorders (OR = 1.60; 95% CI = 1.30–1.96), and three disorders (OR = 2.33; 95% CI = 1.73–3.13) were significantly more likely to report emergency room treatment.
Multivariate analyses were then conducted predicting emergency room treatment from number of past-year psychiatric disorders, along with all covariates. Compared to those with no past-year disorder, individuals with one disorder (OR = 1.48; 95% CI = 1.26–1.75), two disorders (OR = 1.93; 95% CI = 1.47–2.52), and three disorders (OR = 2.70; 95% CI = 1.81–4.02) were significantly more likely to report emergency room treatment.
Specific DSM-IV psychiatric disorders and past-year overnight hospital stay
Table 3 shows demographic and clinical characteristics of respondents based on past-year overnight hospital stay. Several demographics differed by overnight hospital stay categories, with hospitalized individuals being older, in lower income brackets, and more frequently unmarried than the nonhospitalized group.
Table 3 also shows ORs and 95% CIs from logistic regressions with past-year overnight hospital stay predicted from lifetime psychiatric disorders. Controlling for all demographics and clinical characteristics listed in Table 3, those diagnosed with any lifetime mood disorders or any personality disorder were more likely to report an overnight hospital stay.
Table 4 shows that controlling for all demographics and clinical characteristics listed in Table 3, those diagnosed with any past-year mood disorder were more likely to report an overnight hospital stay. (Note that the results for any lifetime disorders in Tables 3 and 4 are exactly the same because they reflect the same regressions.) Table 4 also shows that controlling for demographics, the following mood disorders were significantly associated with a greater likelihood of overnight hospital stay: lifetime dysthymia, lifetime manic disorder, past-year major depression, past-year manic disorder. The following personality disorders were also significantly associated with a greater likelihood of overnight hospital stay: histrionic, antisocial, and paranoid personality disorders. Anxiety disorders were not significantly associated with overnight hospital stay.
Multivariate analyses were then conducted predicting overnight hospital stay from number of lifetime psychiatric disorders, along with all covariates. Compared to those with no life time disorder, individuals with two disorders (OR = 1.28; 95% CI = 1.03–1.60) and three disorders (OR = 1.74; 95% CI = 1.24–2.43) were significantly more likely to report an overnight hospital stay. Individuals with no life time disorders and those with one disorder reported similar rates of overnight hospital stay (OR = 1.02; 95% CI = 0.88–1.19).
Multivariate analyses were then conducted predicting overnight hospital stay from number of past-year psychiatric disorders, along with all covariates. Compared to those with no past-year psychiatric disorder, individuals with two disorders (OR = 1.56; 95% CI = 1.22–1.99) and three disorders (OR = 2.04; 95% CI = 1.31–3.17) were significantly more likely to report overnight hospital stay. Individuals with no past-year disorders and with one past-year disorder reported similar rates of overnight hospital stay (OR = 1.05; 95% CI = 0.87–1.26).
Discussion
This study examined the relationship between DSM-IV psychiatric disorders and healthcare utilization in hypertensives drawn from a large, nationally representative sample of adults. The results indicate that even in the setting of hypertension, a chronic condition that already increases healthcare utilization, certain psychiatric disorders are associated with more frequent hospital care. These relationships held after controlling for numerous demographic and clinical characteristics. In general, our findings are consistent with those of previous reports (e.g., 8). This study extends previous findings by examining hypertensives specifically, investigating personality disorders, and considering individual psychiatric disorders separately. At the same time, this study controlled for nicotine, alcohol, and drug use disorders, each of which may independently be associated with healthcare utilization.
To our knowledge, these are the first data regarding healthcare utilization among individuals with personality disorders. Results indicate that several personality disorders are associated with increased likelihood of hospital care among hypertensives including paranoid, histrionic, antisocial, avoidant, and obsessive–compulsive disorders. Histrionic personality disorder is characterized by excessive emotionality and attention seeking. Thus, the features of this diagnosis may directly increase treatment-seeking behavior including hospital care. All the personality disorders are characterized by impaired interpersonal relationships. Social networks of inadequate size or poor quality may fail to provide emotional and instrumental support, thereby indirectly increasing the likelihood that such individuals will seek care in the hospital. Some research suggests that certain personality traits are associated with poor patient–provider collaboration and primary care clinic nonattendance [6]. Lack of routine care may increase the need for emergent hospital care in patients with personality disorders.
Any past-year or lifetime mood disorder was associated with increased likelihood of both emergency room treatment and overnight hospital stay. Our findings for past-year mood disorders suggest a close temporal association between mood disturbance and hospital care. The relationship between lifetime depression and increased healthcare utilization also suggests more distal associations. These temporally remote associations complement data that show that depressive disorders are prospectively associated with onset of medical illnesses. These conditions may involve hospital care such as heart disease and diabetes [3, 10], as well as symptom exacerbation of existing conditions such as diabetes and rheumatoid arthritis [9, 30]. When both lifetime and past-year mood disorders were entered simultaneously, the effects for hospital care were better accounted for by past-year mood disorder (data not shown).
The results for mood disorders are remarkably similar between emergency room treatment and overnight hospital stay. While we cannot determine whether the emergency room treatment and the overnight hospital stay were linked, these findings may suggest that mood disordered individuals who arrive at the emergency room are evaluated and determined to be at sufficient risk to warrant an overnight stay. This finding is in contrast to anxiety disorders, which were significantly associated only with emergency room treatment. Anxious individuals may present at the emergency room but may be determined not to be at sufficient risk to warrant an overnight stay. Given that anxiety symptoms can mimic cardiac, thyroid, and hypoglycemia symptoms, this finding may reflect patients’ vigilance for somatic changes, misinterpretation of or overreaction to their physical complaints, or a general tendency to somaticize. It should be noted that the overall association between any lifetime anxiety disorder and emergency room treatment was only marginally significant in this very conservative model, so the significant finding for lifetime panic disorder without agoraphobia specifically should be interpreted with caution.
The odds ratios for each given psychiatric disorder are modest, and in some cases smaller than previously reported [17]. This may be because the statistical models tested here are very conservative. In order to isolate the association of a particular psychiatric disorder, each model controlled for every other psychiatric disorder, as well as numerous demographic characteristics, health insurance status, and clinical characteristics including obesity, smoking, and substance use disorders. Yet even under these rigorous constraints, many psychiatric disorders were associated with increased healthcare utilization. In this context, alcohol and drug use disorders were not significantly, independently associated with increased hospital care.
The focus on emergency room treatment and overnight hospital stay is particularly important for two reasons. First, the Agency for Healthcare Quality and Research found that hypertension and depression were two of the most frequent comorbidities among hospitalized patients. Second, emergency room treatment and hospital stays are extremely costly. According to the Medical Expenditure Panel Survey (MEPS) [21], the average cost of an emergency room visit in 2003 was $560. Over one-third of all hospital admissions are through the emergency department [Healthcare Utilization Project (HCUP)] [8]. Once admitted, the average length of stay is 5 days, costing over $17,000. Indeed, MEPS found that inpatient hospital care accounts for $3 of every $10 spent on health care [22]. The data presented in this study do not address cost or length of stay. However, given the MEPS and HCUP figures, the increased cost of hospitalization associated with psychiatric disorders in persons with hypertension is likely to be high. A recent systematic review showed that for depressed medical patients, psychotherapy alone, care management alone, and psychotherapy plus care management all had lower costs per quality-adjusted life year than usual care [24]. Treatment for mental health issues in patients with hypertension has the potential to decrease healthcare utilization, although rigorous studies have yet to clearly demonstrate cost savings for other psychiatric conditions.
Limitations
While results of this study suggest that DSM-IV psychiatric disorders are associated with healthcare utilization in hypertensives, a number of methodological limitations must be noted. First, hypertension status was based upon self-report. The rates of false positive reports for self-reports of other chronic illnesses are low (e.g., diabetes [7]). However, due to the asymptomatic nature of elevated blood pressure, persons may have hypertension and not know it. Nevertheless, the proportions of patient-reported hypertension in this sample are consistent with epidemiological data during the time-period of the survey. Similarly, hospital care was per self-report, and like all such indicators, it is vulnerable to participant deception, bias, and recall problems. BMI was also per self-report and tends to be underestimated. However, events such as visiting an emergency room or an overnight hospital stay are likely to be sufficiently salient to avoid recall problems.
Second, the full range of DSM-IV disorders was not assessed, so it is unclear whether other psychiatric disorders are also related to healthcare utilization. For example, psychotic disorders were not evaluated, yet persons with these conditions are at very high risk for hospitalization. Third, it is unknown whether care was sought for medical or mental health issues. Costs for psychiatric admissions can rival or even exceed costs for medical admissions, so this is a potentially important limitation. However, previous reports indicate that differences in healthcare utilization remain even after controlling for mental health services. Fourth, due to the cross-sectional nature of the NESARC, causal relationships between past year psychiatric disorders and past year healthcare utilization cannot be determined. Psychiatric disorders, particularly mood and anxiety disorders, may precede or follow hospital care or the medical crisis that necessitated it.
Finally, the NESARC interview did not assess hospital visits in such a way that allows determination whether the emergency room visits and the overnight hospital stays were related events. Past-year overnight hospitalization and ER visit were in fact significantly related. However, the differing patterns of results for each outcome variable suggest that they were not always related.
Despite these limitations, methodological strengths of this study include the large, randomly selected, nationally representative sample of adults, high response rate, administration of face-to-face interviews, and use of systematic psychiatric diagnostic tools. Demographic variables that may confound relationships between psychiatric disorders and utilization were carefully measured and controlled. The unique focus on a large sample of hypertensives is also a strength.
Conclusions
In summary, results of this study indicate psychiatric disorders are associated with healthcare utilization, even in the setting of a chronic medical condition that may itself increase utilization. Although we cannot establish causality, these results provide some epidemiological support for expanding mental health treatment for hypertensives with psychiatric problems. Healthcare providers who treat people with hypertension are encouraged to screen, treat, or refer for treatment patients with psychiatric disorders to diminish the healthcare utilization associated with these disorders.
References
Agatisa PK, Matthews KA, Bromberger JT et al (2005) Coronary and aortic calcification in women with a history of major depression. Arch Intern Med 165:1229–1236
CDC (2005) Racial/ethnic disparities in prevalence, treatment, and control of hypertension—United States, 1999–2002. MMWR 54:7–9
Carnethon MR, Biggs ML, Barzilay JI et al (2007) Longitudinal association between depressive symptoms and incident type 2 diabetes mellitus in older adults: the cardiovascular health study. Arch Intern Med 167:802–807
Agency for Healthcare Research Quality, Center for Delivery, Organization, and Markets, Healthcare utilization Project, Nationwide Inpatient Sample (2003)
Kozak LJ, Owings MF, Hall MJ (2005) National hospital discharge summary: 2002 annual summary with detailed diagnosis and procedure data. National Center for Health Statistics. Vital Health Stat 2005;13(158)
Ciechanowski P, Russo J, Katon W et al (2006) Where is the patient? The association of psychosocial factors and missed primary care appointments in patients with diabetes. Gen Hosp Psychiatr 28:9–17
Cowie C, Harris M (1997) Ambulatory medical care for non-Hispanic Whites, African Americans and Mexican Americans in the US. Diabetes Care 20:142–147
Merrill CT, Elixhauser A (2005) Hospitalization in the United States, 2002: HCUP Fact Book No. 6. AHRQ Publication No. 05-0056, June 2005. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/data/hcup/factbk6/
Fifield J, Tennen H, Reisine S et al (1998) Depression and the long-term risk of pain, fatigue, and disability in patients with rheumatoid arthritis. Arthritis Rheum 41:1851–1857
Frasure-Smith N, Lesperance F (2005) Reflections on depression as a cardiac risk factor. Psychosom Med 67(suppl 1):S19–S25
Grant BF, Dawson DA, Stinson FS et al (2003) the alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend 71:7–16
Grant BF, Harford TC, Dawson DA et al (1995) The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend 39:37–44
Grant BF, Hasin DS (1991) The alcohol use disorders and associated disabilities interview schedule (AUDADIS). National Institute on Alcohol Abuse and Alcoholism, Rockville
Grant BF, Moore TC, Kaplan K (2003) Source and accuracy statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). National Institute on Alcohol Abuse and Alcoholism, Bethesda
Hasin D, Carpenter KM, McCloud S et al (1997) The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend 44:133–141
Henk HJ, Katzelnikc DJ, Kobak KA et al (1996) Medical costs attributed to depression among patients with a history of high medical expenses in a health maintenance organization. Arch Gen Psychiatr l53:899–904
Himelhoch S, Weller WE, Wu AW et al (2004) Chronic medical illness, depression, and use of acute medical services among medicare beneficiaries. Med Care 42:512–521
Jones DJ, Bromberger JT, Sutton-Tyrrell K et al (2003) Lifetime history of depression and carotid atherosclerosis in middle-aged women. Arch Gen Psychiatry 60(2):153–160
Kennedy N, Paykel ES (2004) Residual symptoms at remission from depression: impact on long term outcome. J Affect Disord 80:135–144
Kessler LG, Burns B, Shapiro S et al (1987) Psychiatric diagnoses of medical service users: evidence from the Epidemiological Catchment Area program. AJPH 77:18–24
Machlin SR (2006) Expenses for a hospital emergency room visit, 2003. Statistical brief #111 (Agency for Healthcare Research and Quality website). Available at: http://www.meps.ahrq.gov/papers/st111/stat111.pdf. Accessed June 26, 2007
Machlin SR, Carper K (2007) Expenses for inpatient hospital stays, 2004. Statistical brief #164 (Agency for Healthcare Research and Quality website). Available at: http://www.meps.ahrq.gov/mepsweb/data_files/publications/st164/stat164.pdf. Accessed June 26, 2007
National Heart Lung and Blood Institute (1998) Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. National Institutes of Health. Obes Res 6(suppl 2):51S–209S
Pirraglia PA, Rosen AB, Hermann RC et al (2004) Cost-utility analysis studies of depression management: a systematic review. Am J Psychiatr 161:2155–2162
Post R (1992) Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. Am J Psychiatry 149:999–1010
Research Triangle Institute (2003) Software for survey data analysis (SUDAAN). Research Triangle Institute, Research Triangle Park
Sheline YI, Sanghavi M, Mintun MA et al (1999) Depression duration but not age predicts hippocampal volume loss in medically healthy women with recurrent major depressive depression. J Neurosci 19:5034–5043
Simon G, VonKorff M, Barlow W (1995) Healthcare costs of primary care patients with recognized depression. Arch Gen Psychiatr 52:850–856
Unutzer J, Patrick D, Simon G et al (1997) Depressive symptoms and the cost of health services in HMO patients aged 65 years and older: a 4-year prospective study. JAMA 277:1618–1623
Wagner J, Tennen H (2007) History of major depressive disorder and diabetes outcomes among diet and tablet treated postmenopausal women: a case control study. Diabet Med 24: 211–216
Wagner J, Tennen H, Mansoor G et al (2006) History of depression and endothelial function in post-menopausal women. Psychosom Med 68: 80–86
Wolf-Maier K, Cooper RS, Banegas J et al (2003) Hypertension prevalence and blood pressure in 6 European countries, Canada, and the United States. JAMA 289:2363–2369
Acknowledgments
Preparation of this report was supported in part by NIH grants R01-MH60417, R01-MH60417-Supp, R01-DA13444, R01-DA018883, R01-DA14618, R01-DA016855, P50-AA03510, P50-DA09241, R21-DK074468, and grants from the American Heart Association and the American Diabetes Association. We thank NIAAA and the U.S. Census Bureau field representatives who administered the NESARC interview.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wagner, J.A., Pietrzak, R.H. & Petry, N.M. Psychiatric disorders are associated with hospital care utilization in persons with hypertension. Soc Psychiat Epidemiol 43, 878–888 (2008). https://doi.org/10.1007/s00127-008-0377-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-008-0377-2