Abstract
Aims/hypothesis
Diabetes is characterised by progressive loss of functional pancreatic beta cells. None of the therapeutic agents used to treat diabetes arrest this process; preventing beta cell loss remains a major unmet need. We have previously shown that serum from eight young healthy male participants who exercised for 8 weeks protected human islets and insulin-producing EndoC-βH1 cells from apoptosis induced by proinflammatory cytokines or the endoplasmic reticulum (ER) stressor thapsigargin. Whether this protective effect is influenced by sex, age, training modality, ancestry or diabetes is unknown.
Methods
We enrolled 82 individuals, male or female, non-diabetic or diabetic, from different origins, in different supervised training protocols for 8–12 weeks (including training at home during the COVID-19 pandemic). EndoC-βH1 cells were treated with ‘exercised’ serum or with the exerkine clusterin to ascertain cytoprotection from ER stress.
Results
The exercise interventions were effective and improved \( \dot{V}{\mathrm{O}}_{2\mathrm{peak}} \) values in both younger and older, non-obese and obese, non-diabetic and diabetic participants. Serum obtained after training conferred significant beta cell protection (28% to 35% protection after 4 and 8 weeks of training, respectively) from severe ER stress-induced apoptosis. Cytoprotection was not affected by the type of exercise training or participant age, sex, BMI or ancestry, and persisted for up to 2 months after the end of the training programme. Serum from exercised participants with type 1 or type 2 diabetes was similarly protective. Clusterin reproduced the beneficial effects of exercised sera.
Conclusions/interpretation
These data uncover the unexpected potential to preserve beta cell health by exercise training, opening a new avenue to prevent or slow diabetes progression through humoral muscle–beta cell crosstalk.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Loss of functional pancreatic beta cells is key in the development and progression of diabetes [1]. In autoimmune type 1 diabetes, the search for protective therapies has focused on the immune system [2]. The anti-CD3 antibody teplizumab significantly delayed the onset of type 1 diabetes in autoantibody-positive high-risk individuals; half progressed to diabetes nonetheless in an extended follow-up [3, 4]. There is thus a clear need for therapies that directly protect beta cells [2] as an adjuvant to immune modulation in type 1 diabetes. Such a treatment could also be of great value in type 2 diabetes.
Signals of endoplasmic reticulum (ER) stress are present in beta cells of individuals with type 1 [5] and type 2 diabetes [6, 7], and several monogenic forms of diabetes are caused by mutations in genes involved in the response to ER stress (also known as the unfolded protein response) [8]. ER stress contributes to progressive beta cell dysfunction and death in these different forms of diabetes [1]. It can be reproduced in vitro by exposure of human islets to proinflammatory cytokines, palmitate alone or in combination with high glucose, and chemical ER stressors such as thapsigargin [1, 5]. ER stress is defined as the accumulation of mis- or unfolded proteins in the ER lumen, and if severe and unresolved it will lead to beta cell apoptosis [1]. Agents that restore ER homeostasis potentially provide an interesting therapeutic strategy in diabetes. Tauroursodeoxycholic acid (TUDCA) and imatinib have been shown to ameliorate ER stress and protect beta cells in pre-clinical models of diabetes [2, 9,10,11], and they are being tested to delay beta cell loss after the onset of type 1 diabetes [2, 12]. The initial results for imatinib show modest but transient beta cell protection [12] which may be due to the lack of concomitant modulation of the immune system [2].
Physical exercise is an important non-pharmacological component of diabetes therapy. Exercise improves glycaemic control in individuals with type 1 and type 2 diabetes by enhancing insulin sensitivity, stimulating glucose uptake by skeletal muscle cells and reducing body weight; it also decreases circulating lipids, blood pressure and risk of cardiovascular complications [13, 14]. A combination of aerobic and resistance exercise is recommended for diabetic individuals and interval aerobic training might be more effective than continuous aerobic training to improve cardiorespiratory fitness, insulin sensitivity and glycaemic control in type 2 diabetes [15, 16]. In addition, physical training may have direct beneficial effects on pancreatic beta cells via circulating mediators, as evidenced by studies in animal models and human islets [17,18,19]. We have previously shown that serum from eight healthy young male participants who performed moderate-intensity continuous exercise training for 8 weeks was beta cell protective against proinflammatory cytokines and the ER stressor thapsigargin [19]. This protection was observed in primary human islets and the human beta cell line EndoC-βH1 [19]. This study was limited in that it included only a small number of male participants and one type of training. Here we assessed the impact of different exercise modalities on ER stress-induced human beta cell death in a larger cohort of individuals of both sexes with or without diabetes.
Methods
Ethics approval
The exercise intervention protocol was approved by the Erasmus Hospital (Brussels, Belgium) ethical committee (P2018/387 and P2019/591) in accordance with the World Medical Association’s Declaration of Helsinki. All the participants gave written informed consent.
Maximal incremental test
Maximal exercise capacity was assessed during an incremental cardio-pulmonary exercise test performed on a stationary bike (Ergoselect 100, Ergoline, Bitz, Germany). During the test, participants wore an oral–nasal mask connected to a breath-by-breath analyser (Ergocard, Medisoft, Sorinnes, Belgium) to measure \( \dot{V}{\mathrm{O}}_2 \) and carbon dioxide release. The protocol started with a 3 min warm-up at a load of 20 W for women and 30 W for men. The load then increased by 15 W each minute for women and 20 W for men. The increment kept going until volitional fatigue of the participant. Since a plateau of \( \dot{V}{\mathrm{O}}_2 \) was not observed in all participants, we took the \( \dot{V}{\mathrm{O}}_{2\mathrm{peak}} \) as the highest value of \( \dot{V}{\mathrm{O}}_2 \) reached during the last completed level. The load and heart rate attained during this last level were considered, respectively, as maximal power (Pmax) and maximal heart rate (HRmax). \( \dot{V}{\mathrm{O}}_{2\mathrm{peak}} \), Pmax and HRmax were used to determine intensities during the exercise intervention performed on stationary bikes (see below). Training efficacy is presented in Table 1 and HRmax data are presented in electronic supplementary material (ESM) Table 1.
Exercise interventions with continuous and interval training in healthy participants
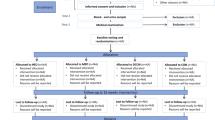
Forty-six healthy participants (26 female and 20 male) were randomly assigned to different exercise training protocols. A stratified randomisation by sex (two strata: male and female) was used to balance the number of male and female participants in each intervention group, and the assignment was made by drawing lots. The intervention groups consisted of stationary bike high-intensity interval training (HIIT), adapted sprint interval training (aSIT) and vigorous-intensity continuous training (VICT) or high-intensity functional training performed at home (HIFT) three times per week over an 8 week period. During the COVID-19 lockdown, all participants were assigned to the home training group. Five additional participants assigned to a no-exercise control group were recommended to continue their usual physical activity habits without additional training. Statistical power analysis using G*Power 3.1 software was performed to assess the sample size. Characteristics of the participants are reported in Table 1.
Stationary bike training protocols
Sessions were performed at the Faculty of Motor Sciences, Université Libre de Bruxelles, on a stationary bike (Ergoselect 100) driven by the Ergoline Rehab System 2 software. Protocols started with a 3 min warm-up and ended with a 3 min cool down at 50 W. The HIIT protocol consisted of six bouts of 2 min at a load equivalent to 90% of \( \dot{V}{\mathrm{O}}_{2\mathrm{peak}} \) interspaced with 2 min of active rest at a load equivalent to 50% of \( \dot{V}{\mathrm{O}}_{2\mathrm{peak}} \). The aSIT protocol consisted of 12 bouts of 30 s at a load equivalent to 125% of \( \dot{V}{\mathrm{O}}_{2\mathrm{peak}} \) interspaced with 2 min of active rest at a load equivalent to 50% of \( \dot{V}{\mathrm{O}}_{2\mathrm{peak}} \). The VICT protocol consisted of 28 min at a load equivalent to 70% of \( \dot{V}{\mathrm{O}}_{2\mathrm{peak}} \). For all protocols, the first four sessions were a familiarisation phase during which the load was a bit lower than the target training load. After this, the load was increased by 2% of Pmax every four sessions to account for improvements during the training period.
Home training
The HIFT home training programme was provided by means of four videos prepared by a professional coach. Training sessions started with a 3 min warm-up followed by four bouts of 30 s of all-out whole-body exercises (squats, lunges, mountain climbers, jumping jacks, modified burpees …) interspaced with 30 s of active rest (walking/jogging on the spot) repeated three (in weeks 1 and 2) to four times (in weeks 3–8). In the videos, exercises were proposed with an easier and more difficult variant. Participants were asked to use each video for 2 weeks, the easier variant during week 1 and the more difficult one during week 2. Exercise difficulty increased from video 1 to video 4. All sessions ended with 5 min of stretching. Heart rate was recorded using a Polar H9 heart rate sensor (Polar, Kempele, Finland) connected to the ‘Polar Beat’ app on the participants’ smartphones.
Exercise intervention to assess impact of diabetes status
To evaluate possible impacts of diabetes and of ancestry and cultural background on the beta cell-protective effects of exercise, 36 individuals, non-diabetic or with type 1 or type 2 diabetes, of Belgian origin (‘European ancestry’ in the text) or Belgians of Moroccan, Turkish or African origin (‘non-European ancestry’), participated in the study. Non-diabetic participants were matched to individuals with type 1 or type 2 diabetes based on age (±5 years) and sex. The prevalence of diabetes in Belgian adults is higher in those of Moroccan and Turkish origin, possibly due to higher obesity rates, lack of physical activity in men and lower educational attainment [20]. They took part three times a week in 12 week training combining stationary bike HIIT and strength training at a fitness centre with the first session supervised by one of the study investigators. Subsequent sessions were carried out autonomously with weekly contacts with the investigators to maintain adherence and motivation. Heart rate was recorded during all sessions using Polar M430 or Polar Ignite trackers. HIIT consisted of a 3 min warm-up followed by eight 2 min bouts at 90% of \( \dot{V}{\mathrm{O}}_{2\mathrm{peak}} \) interspaced with 2 min of active rest at 50% of \( \dot{V}{\mathrm{O}}_{2\mathrm{peak}} \). Strength training consisted of four exercises focusing on the main muscle groups, i.e. chest press for pectoralis major and triceps, lateral pulldown for dorsalis major and biceps, leg press for quadriceps and gluteus and leg curl for hamstrings. Participants performed three sets of ten repetitions at a load equivalent to their 10 RM (10 repetitions maximum) determined during the first session. Statistical power analysis using G*Power 3.1.9.4 software (https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower) was performed to assess the sample size. Participant characteristics are reported in Table 1.
Serum collection
Blood was collected in BD Vacutainer Clot Activator tubes (BD Medical, Franklin Lakes, NJ, USA) prior to the study (week 0) and after 4, 8 and 12 weeks of training, each time 48 h after a training session. For some, an additional sample was drawn 2 months after the end of the training (wash-out). Tubes were kept for 30 min at room temperature before centrifugation at 1700 g for 10 min at 2°C. Serum was collected, aliquoted and stored at −80°C.
Cell culture and treatment
The human beta cell line EndoC-βH1, kindly provided by R. Scharfmann (Cochin Institute, France) [21], was cultured in Matrigel–fibronectin-coated plates as previously described [9]. Cells were free of mycoplasma, as determined monthly using the MycoAlert Mycoplasma Detection kit (Lonza, Basel, Switzerland). EndoC-βH1 cells were pre-cultured for 24 h in medium supplemented with 10% human serum (from week 0, 4, 8 or 12 or wash-out). Cells were then treated with 1 μmol/l thapsigargin (Sigma-Aldrich, St Louis, MO, USA) for 48 h in the presence of serum. One specific EndoC-βH1 cell passage exposed to serum from one participant was considered as an independent experiment.
EndoC-βH1 cells were pre-cultured for 24 h in medium supplemented with 2% FBS plus recombinant clusterin (no. 2937-HS-050, R&D Systems, Minneapolis, MN, USA) at concentrations of 1 and 100 ng/ml. Cells were then treated with 1 μmol/l thapsigargin for 48 h in the presence of clusterin.
Assessment of cell viability
Fluorescence microscopy was used to count apoptotic cells after staining with the DNA-binding dyes Hoechst 33342 and propidium iodide (10 μg/ml, Sigma-Aldrich) as previously described [22]. A minimum of 500 cells was counted in each experimental condition by two independent observers, one of them unaware of sample identity. This method has been extensively used in our laboratory and was previously validated by us and others by comparing it with other methods to measure apoptosis [23,24,25,26].
RNA extraction and quantitative reverse transcription PCR (qRT-PCR)
Polyadenylated mRNA was isolated from cells using Dynabeads mRNA DIRECT purification kit (Invitrogen, Carlsbad, CA, USA) and reverse transcribed using Reverse Transcriptase Core kit (Eurogentec, Liège, Belgium). Quantitative PCR amplification was done with SsoAdvanced Universal SYBR Green Supermix (BIO-RAD, Hercules, CA, USA) and amplicons quantified using a standard curve. Gene expression was corrected by the reference gene ACTB or the geometric mean of ACTB and VAPA [27]. Primers are listed in ESM Table 2.
Statistical analysis
Data are expressed as means of independent experiments (shown as individual data points) ± SEM. A normality test was performed to assess Gaussian distribution. In the case of normality, differences between groups were evaluated using repeated measures one-way ANOVA or linear mixed models in the case of missing values, followed by Bonferroni post hoc test. When the distribution was not normal, the non-parametric Friedman test equivalent to one-way ANOVA was used (GraphPad Prism 9.4.0, Dotmatics, Boston, MA, USA). A multiple linear regression model was generated using SPSS Statistics 27.0 (IBM, Armonk, NY, USA) to determine whether an association existed between the dependent variable cytoprotection and independent variables sex, age, BMI, diabetes status, ancestry and training type. The dependent variable ‘cytoprotection’ was calculated as follows: [(apoptosis week 8 − apoptosis week 0)/apoptosis week 0]×100. A p value less than or equal to 0.05 was considered statistically significant.
Results
Healthy men and women (aged 18–38 years, mean 23.6 years; Table 1) were enrolled in an 8 week exercise study and assigned to one of the four training protocols described in the Methods. Exercise training in these young non-obese individuals was effective, and improved \( \dot{V}{\mathrm{O}}_{2\mathrm{peak}} \) values for all training protocols (Table 1). We evaluated the protective effect of serum collected at week 0 and after 4 and 8 weeks of exercise on human insulin-producing beta cells exposed to thapsigargin. We first evaluated whether some training modalities were particularly beneficial. There was significant protection against thapsigargin-induced beta cell apoptosis already after 4 weeks of exercise for HIIT, aSIP and VICT and after 8 weeks for HIFT (Fig. 1a–d). Since no major differences were observed between the exercise protocols, we pooled the data and reanalysed them according to participant sex. We observed significant exercise-mediated beta cell protection (29–32% decrease in apoptosis in women and 27–40% in men) at 4 and 8 weeks of training (Fig. 1e,f). When pooling all 46 participants (Fig. 1g) there was a 28% to 35% decrease in apoptosis at 4 and 8 weeks. To determine if this protective effect persisted after training was stopped, serum was collected from 13 participants 2 months after the end of training (wash-out). Unexpectedly, the protective effect of serum against thapsigargin remained present 2 months after they had returned to their basal physical activity (Fig. 1h). To assure that the protective effect observed was indeed mediated by training, we collected serum from control participants who remained sedentary for 8 weeks. In contrast to trained sera, sera from these untrained individuals did not confer any protection against thapsigargin (Fig. 1i).
Trained serum from healthy participants protects human beta cells from thapsigargin-induced apoptosis independently of sex and type of training. EndoC-βH1 cells were cultured for 24 h in medium containing 10% serum from week 0 (white bars), week 4 (grey bars), week 8 (blue bars) or wash-out (orange bars). Thapsigargin (THAP, 1 μmol/l) was added in the continued presence of serum and apoptosis evaluated after 48 h. The cytoprotective effects of serum following HIIT (a, n=12), aSIT (b, n=11), VICT (c, n=10) and HIFT training (d, n=13) were assessed. Data from (a–d) were pooled and separated by sex (e, f ; female and male, respectively) or not (g). (h) Serum from 13 participants was evaluated for cytoprotection after wash-out, i.e. 2 months after completion of training. (i) Serum from five individuals who remained sedentary for 8 weeks was used as negative control. *p<0.05, **p<0.01 and ***p<0.001 compared with week 0 non-treated (NT); †p<0.05, ††p<0.01 and †††p<0.001 compared with week 0 THAP (ANOVA)
To assess if the beneficial effects of serum from these trained young, non-obese and non-diabetic individuals could be replicated in diabetic patients, individuals with type 1 or type 2 diabetes and age- and sex-matched non-diabetic control individuals performed a 12 week aerobic and strength training protocol. These participants were older (aged 24–69 years, mean 46.7 years), less fit with a lower starting \( \dot{V}{\mathrm{O}}_{2\mathrm{peak}} \), and the type 2 diabetic participants were obese (Table 1). The training was equally effective in improving \( \dot{V}{\mathrm{O}}_{2\mathrm{peak}} \) values, albeit with a non-significant progression (p=0.06) for the type 1 diabetic participants (Table 1). Serum from the older non-diabetic participants significantly protected human beta cells from thapsigargin-induced apoptosis after 4, 8 and 12 weeks of training (Fig. 2a). Interestingly, trained serum from participants with type 1 or type 2 diabetes was also protective, reducing apoptosis by 45% and 26%, respectively, after 12 weeks of training (Fig. 2b,c). To determine if ancestry affected the response, we pooled data from the three groups and split them into European and non-European origins (mostly Moroccan, Turkish and African). Serum conferred significant protection against apoptosis (22%, 28% and 37% in Europeans and 25%, 28% and 31% in non-Europeans, respectively) after 4, 8 and 12 weeks of exercise (Fig. 2d,e). Diabetes and ancestry hence do not influence the protective effects of physical exercise against ER stress-induced beta cell apoptosis.
Trained serum from participants with type 1 or type 2 diabetes protects human beta cells from thapsigargin-induced apoptosis independently of ancestry. EndoC-βH1 cells were cultured for 24 h in medium containing 10% serum from week 0 (white bars), week 4 (grey bars), week 8 (blue bars) or week 12 (red bars). Thapsigargin (THAP, 1 μmol/l) was then added in the continued presence of serum and apoptosis was evaluated after 48 h. Serum from non-diabetic control (a, CTL: n=17), type 1 diabetic (b, T1D: n=8) or type 2 diabetic (c, T2D: n=11) individuals was evaluated for cytoprotective properties. Data from (a–c) were pooled and separated by ancestry (d, e, n=22 and 14, respectively). *p<0.05, **p<0.01 and ***p<0.001 compared with week 0 non-treated (NT); †p<0.05, ††p<0.01 and †††p<0.001 compared with week 0 THAP (ANOVA)
The expression of ER stress and pro-apoptotic genes was evaluated. The cells exposed to serum from exercised participants showed reduced CHOP (also known as DDIT3), XBP1s and DP5 (also known as HRK) mRNA expression, while PUMA (also known as BBC3) was not changed (Fig. 3a–d). Serum did not modify expression of INS and PDX1 in ER-stressed cells, but basal PDX1 expression was lowered by 4 week exercised serum (Fig. 3e,f).
Trained serum from healthy participants modulates expression of ER stress and pro-apoptotic genes. EndoC-βH1 cells were cultured for 24 h in medium containing 10% serum from week 0 (white bars), week 4 (grey bars) or week 8 (blue bars). Thapsigargin (THAP, 1 μmol/l) was added in the continued presence of serum and mRNA extracted after 24 h. Expression of CHOP (a), XBP1s (b), DP5 (c), PUMA (d), INS (e) and PDX1 (f) was analysed by qRT-PCR. Values were corrected for ACTB expression and normalised to the condition week 0 THAP set as 1. Results are mean ± SEM of 12 independent experiments (four sera from HIIT, four from aSIT and four from VICT; since the results were similar, they were pooled). *p<0.05, **p<0.01 and ***p<0.001 compared with week 0 non-treated (NT); ††p<0.01 and †††p<0.001 compared with week 0 THAP (ANOVA)
To further analyse determinants of cytoprotection mediated by trained serum, we carried out multiple linear regression analysis including sex, age, diabetes status, training protocol, ancestry and BMI as independent variables (Table 2). In this regression model, the independent variables explained only 6% of the variability in protection, indicating that there is no significant correlation between exercise-induced beta cell protection and any of the variables studied. In other words, the beta cell protection by exercise occurs independently of sex, age, diabetes status, training type, ancestry and BMI.
It has recently been reported that exercise induces production of the exerkine clusterin, which has anti-inflammatory effects in the brain [28] and may protect rodent beta cells from metabolic stresses [29]. We thus examined whether clusterin could reproduce the beneficial effects of exercised serum in human beta cells. Clusterin reduced thapsigargin-induced cell death by 31–42% at two concentrations (1 and 100 ng/ml; Fig. 4a). The mRNA expression of the pro-apoptotic gene DP5 was significantly reduced at the higher dose of clusterin (Fig. 4b).
Recombinant clusterin protects human beta cells against thapsigargin-induced apoptosis. EndoC-βH1 cells were pretreated for 24 h with 0 (white bars), 1 (grey bars) or 100 ng/ml (purple bars) recombinant clusterin. Medium was then changed, and cells were exposed or not to clusterin and thapsigargin (THAP, 1 μmol/l). Apoptosis (a) and DP5 expression (b) were analysed after 48 h. Gene expression was corrected for the geometric mean of the reference genes ACTB and VAPA and normalised to the condition THAP without clusterin set as 1. Results are mean ± SEM of six independent experiments. **p<0.01 and ***p<0.001 compared with no clusterin/non-treated (NT); ††p<0.01 and †††p<0.001 compared with no clusterin/THAP (ANOVA)
Discussion
The present study demonstrates a beneficial effect of exercise training on the survival of human pancreatic beta cells exposed to a severe ER stress, regardless of training modality, sex, ancestry, diabetes status, age and BMI. This cytoprotection points to a muscle– or multi-organ–beta cell crosstalk, likely mediated by circulating exerkines.
ER stress is a common mediator for beta cell dysfunction and death in type 1 and type 2 diabetes [1, 5,6,7,8]. It is therefore of great interest to identify therapies that restore ER homeostasis and protect beta cells from apoptosis. In a previous study, serum from eight young Brazilian male participants doing moderate-intensity training protected EndoC-βH1 and dispersed human islet cells from proinflammatory cytokines (IFNγ + IL-1β) and thapsigargin [19]. Because the cytoprotection was similar for cytokines or thapsigargin and for human islet or EndoC-βH1 cells, we selected in the present study a single experimental condition, namely thapsigargin-exposed EndoC-βH1 cells, obviating the limited access and variability inherent to human islets. This enabled us to evaluate the putative beneficial effects of serum in a much larger and diverse sample of exercised individuals (82 in total) and test for the impact of individual characteristics—including sex, age, BMI, ancestral background and diabetes status—and training modality. Since part of the study was performed during the COVID-19 pandemic, we introduced a new group of at-home whole-body exercise training. Importantly, there was significant protection by ‘exercised serum’ against ER stress-induced EndoC-βH1 cell apoptosis for all exercise protocols tested, including the at-home version, a relevant finding as it may facilitate and broaden access to exercise. There was no protection by serum from non-exercised individuals sampled at times 0 and 8 weeks, excluding a nonspecific effect of participation in a study.
In the four training protocols, participants spent at least 50% of the time at an intensity superior to 80% of their HRmax as assessed by the Polar tracker (data not shown), corresponding to vigorous intensity according to the American College of Sports Medicine [30]. This indicates that vigorous continuous or interval bicycle protocols and at-home whole-body vigorous interval training are beta cell protective. Whether such protection would also be conferred by mild to moderate exercise programmes, such as brisk walking, remains to be determined.
We investigated the durability of these exercise effects by evaluating cytoprotection of serum collected 2 months after the end of the study and, surprisingly, found that protection persisted. The underlying reason remains to be investigated and could be mediated by epigenetic effects. Exercise training has been shown to remodel the activity of enhancers located in proximity to exercise-regulated genes in skeletal muscle [31]. It is not known whether such changes persist over time, but it is conceivable that exercise-induced epigenetic changes in skeletal muscle cells induce long-term release of myokines that confer beta cell protection, such as IL-6 [19] and other myokines that remain to be determined.
Other organs besides skeletal muscle also secrete exercise-induced factors into the bloodstream, the so-called exerkines [32, 33]. Hepatocytes and cardiomyocytes seem to be the main sources of clusterin [28]. Exercise-induced clusterin release reduces inflammatory gene expression in brain and improves cognition and memory [28]. Here, we demonstrate that clusterin protects human insulin-producing cells from ER stress-induced apoptosis and reduces expression of the pro-apoptotic gene DP5, previously shown by us to play a key role in ER stress-mediated apoptosis [34]. DP5 was also reduced in beta cells exposed to serum from exercised individuals, suggesting a possible role of clusterin in exercise-induced apoptosis protection.
PDX1 gene expression was reduced in beta cells exposed to 4 week trained serum. This is in line with data showing a reduction in insulin secretion [18] and Pdx1 expression [35] in pancreatic islets from trained mice. It suggests a possible role of ‘beta cell rest’ as an additional mechanism of exercise-induced protection.
The progressive loss of beta cells in type 1 and type 2 diabetes has different causes [1], but ER stress is common to both forms of the disease [5,6,7]. Attempts to protect beta cells in type 1 diabetes should be initiated early, ideally at stage 1, i.e. in normoglycaemic individuals who are positive for two or more autoantibodies and who probably retain a large population of viable beta cells [36]. Since many of these individuals are children or adolescents, interventions should be as safe as possible. In people at risk for type 2 diabetes, large-scale intervention studies have shown that lifestyle measures, including physical activity, prevent or delay the development of type 2 diabetes [37, 38]. Fritsche and colleagues recently showed that conventional Diabetes Prevention Program lifestyle intervention was beneficial for low-risk individuals with prediabetes, and intensified lifestyle with doubled exercise volumes was more efficient in high-risk individuals, with increased conversion from impaired to normal glucose tolerance in the latter over 3 year follow-up [39]. Even after type 2 diabetes diagnosis, weight loss and lifestyle interventions improve glycaemic control and prevent or delay chronic complications [40,41,42]. In this context, it is of interest that serum from exercised participants with type 2 diabetes was equally beta cell protective.
Our data show that serum from non-diabetic and type 1 and type 2 diabetic individuals who underwent an 8–12 week programme of vigorous exercise confers beta cell protection against ER stress. This uncovers the unexpected potential to preserve beta cell health by exercise training, opening a new avenue to prevent or slow diabetes progression through humoral muscle–beta cell crosstalk. Such a humoral crosstalk may be beneficial to other tissues, as suggested by the recent report that exercised plasma reduces brain inflammation and protects neurons [28].
Exercise training should hence be tested as a non-pharmacological intervention in people at risk of developing either type 1 or type 2 diabetes, not only for the benefits on muscle, liver, fat and potentially brain, but also to directly protect pancreatic beta cells. Exercise is a safe approach which may help individuals at the early stages of diabetes to preserve endogenous insulin secretion and beta cell health, in addition to conferring cardiovascular and a plethora of other health benefits.
In the context of type 1 diabetes, exercise could be particularly beneficial in autoantibody-positive and overweight individuals with the dual aim to delay disease until other and more specific protective/regenerative/replacement therapies become available [43, 44] and to serve as an adjuvant beta cell-protective therapy to support other ‘curative’ approaches. It is difficult to know at this stage whether an exercise intervention alone would confer meaningful beta cell protection during a protracted autoimmune assault; only a future clinical trial can answer this question. It is conceivable that exercise, when used at an early stage, may delay the evolution of the disease by increasing beta cell resistance to ER stress and other mediators of immune damage. It will be crucial, however, to attempt in parallel to ‘convince the immune system to forget the beta cells’ and thus avoid the continuous autoimmune assault eventually culminating in clinical diabetes.
Data availability
All the data that support the findings of the present study are available from the corresponding author upon reasonable request.
Abbreviations
- aSIT:
-
Adapted sprint interval training
- ER:
-
Endoplasmic reticulum
- HIFT:
-
High-intensity functional training performed at home
- HIIT:
-
High-intensity interval training
- HRmax:
-
Maximal heart rate
- Pmax:
-
Maximal power
- qRT-PCR:
-
Quantitative reverse transcription PCR
- VICT:
-
Vigorous-intensity continuous training
References
Eizirik DL, Pasquali L, Cnop M (2020) Pancreatic β-cells in type 1 and type 2 diabetes mellitus: different pathways to failure. Nat Rev Endocrinol 16(7):349–362. https://doi.org/10.1038/s41574-020-0355-7
Eizirik DL, Szymczak F, Alvelos MI, Martin F (2021) From pancreatic β-cell gene networks to novel therapies for type 1 diabetes. Diabetes 70(9):1915–1925. https://doi.org/10.2337/dbi20-0046
Herold KC, Bundy BN, Long SA et al (2019) An anti-CD3 antibody, teplizumab, in relatives at risk for type 1 diabetes. N Engl J Med 381(7):603–613. https://doi.org/10.1056/NEJMoa1902226
Sims EK, Bundy BN, Stier K et al (2021) Teplizumab improves and stabilizes beta cell function in antibody-positive high-risk individuals. Sci Transl Med 13(583):eabc8980. https://doi.org/10.1126/scitranslmed.abc8980
Marhfour I, Lopez XM, Lefkaditis D et al (2012) Expression of endoplasmic reticulum stress markers in the islets of patients with type 1 diabetes. Diabetologia 55(9):2417–2420. https://doi.org/10.1007/s00125-012-2604-3
Laybutt DR, Preston AM, Åkerfeldt MC et al (2007) Endoplasmic reticulum stress contributes to beta cell apoptosis in type 2 diabetes. Diabetologia 50(4):752–763. https://doi.org/10.1007/s00125-006-0590-z
Marchetti P, Bugliani M, Lupi R et al (2007) The endoplasmic reticulum in pancreatic beta cells of type 2 diabetes patients. Diabetologia 50(12):2486–2494. https://doi.org/10.1007/s00125-007-0816-8
Cnop M, Toivonen S, Igoillo-Esteve M, Salpea P (2017) Endoplasmic reticulum stress and eIF2α phosphorylation: the Achilles heel of pancreatic β cells. Mol Metab 6(9):1024–1039. https://doi.org/10.1016/j.molmet.2017.06.001
Brozzi F, Nardelli TR, Lopes M et al (2015) Cytokines induce endoplasmic reticulum stress in human, rat and mouse beta cells via different mechanisms. Diabetologia 58(10):2307–2316. https://doi.org/10.1007/s00125-015-3669-6
Morita S, Villalta SA, Feldman HC et al (2017) Targeting ABL-IRE1α signaling spares ER-stressed pancreatic β cells to reverse autoimmune diabetes. Cell Metab 25(4):883–897.e8. https://doi.org/10.1016/j.cmet.2017.03.018
Hägerkvist R, Sandler S, Mokhtari D, Welsh N (2007) Amelioration of diabetes by imatinib mesylate (Gleevec®): role of β-cell NF-KB activation and anti-apoptotic preconditioning. FASEB J 21(2):618–628. https://doi.org/10.1096/fj.06-6910com
Gitelman SE, Bundy BN, Ferrannini E et al (2021) Imatinib therapy for patients with recent-onset type 1 diabetes: a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Diabetes Endocrinol 9(8):502–514. https://doi.org/10.1016/S2213-8587(21)00139-X
Dela F, Prats C, Helge JW (2014) Exercise interventions to prevent and manage type 2 diabetes: physiological mechanisms. In: Goedecke JH, Ojuka EO (eds) Medicine and sport science. S. Karger AG, Basel, pp 36–47
Tonoli C, Heyman E, Roelands B et al (2012) Effects of different types of acute and chronic (Training) exercise on glycaemic control in type 1 diabetes mellitus: a meta-analysis. Sports Med 42(12):1059–1080. https://doi.org/10.1007/BF03262312
Mitranun W, Deerochanawong C, Tanaka H, Suksom D (2014) Continuous vs interval training on glycemic control and macro- and microvascular reactivity in type 2 diabetic patients: continuous vs interval training. Scand J Med Sci Sports 24(2):e69–e76. https://doi.org/10.1111/sms.12112
American Diabetes Association (2021) 3. Prevention or delay of type 2 diabetes: standards of medical care in diabetes—2021. Diabetes Care 44(Suppl 1):S34–S39. https://doi.org/10.2337/dc21-S003
Curran M, Drayson MT, Andrews RC et al (2020) The benefits of physical exercise for the health of the pancreatic β-cell: a review of the evidence. Exp Physiol 105(4):579–589. https://doi.org/10.1113/EP088220
Paula FMM, Leite NC, Vanzela EC et al (2015) Exercise increases pancreatic β-cell viability in a model of type 1 diabetes through IL-6 signaling. FASEB J 29(5):1805–1816. https://doi.org/10.1096/fj.14-264820
Paula FMM, Leite NC, Borck PC et al (2018) Exercise training protects human and rodent β cells against endoplasmic reticulum stress and apoptosis. FASEB J 32(3):1524–1536. https://doi.org/10.1096/fj.201700710R
Vandenheede H, Deboosere P (2009) Type 2 diabetes in Belgians of Turkish and Moroccan origin. Arch Public Health 67(2):62. https://doi.org/10.1186/0778-7367-67-2-62
Ravassard P, Hazhouz Y, Pechberty S et al (2011) A genetically engineered human pancreatic β cell line exhibiting glucose-inducible insulin secretion. J Clin Invest 121(9):3589–3597. https://doi.org/10.1172/JCI58447
Cunha DA, Hekerman P, Ladrière L et al (2008) Initiation and execution of lipotoxic ER stress in pancreatic β-cells. J Cell Sci 121(14):2308–2318. https://doi.org/10.1242/jcs.026062
Hoorens A, Van de Casteele M, Klöppel G, Pipeleers D (1996) Glucose promotes survival of rat pancreatic beta cells by activating synthesis of proteins which suppress a constitutive apoptotic program. J Clin Invest 98(7):1568–1574. https://doi.org/10.1172/JCI118950
Moore F, Colli ML, Cnop M et al (2009) PTPN2, a candidate gene for type 1 diabetes, modulates interferon-ɣ-induced pancreatic β-cell apoptosis. Diabetes 58(6):1283–1291. https://doi.org/10.2337/db08-1510
Gurzov EN, Ortis F, Cunha DA et al (2009) Signaling by IL-1β+IFN-γ and ER stress converge on DP5/Hrk activation: a novel mechanism for pancreatic β-cell apoptosis. Cell Death Differ 16(11):1539–1550. https://doi.org/10.1038/cdd.2009.99
Moore F, Santin I, Nogueira TC et al (2012) The transcription factor C/EBP delta has anti-apoptotic and anti-inflammatory roles in pancreatic beta cells. PLoS ONE 7(2):e31062. https://doi.org/10.1371/journal.pone.0031062
Alvelos MI, Szymczak F, Castela  et al (2021) A functional genomic approach to identify reference genes for human pancreatic beta cell real-time quantitative RT-PCR analysis. Islets 13(3–4):51–65. https://doi.org/10.1080/19382014.2021.1948282
De Miguel Z, Khoury N, Betley MJ et al (2021) Exercise plasma boosts memory and dampens brain inflammation via clusterin. Nature 600(7889):494–499. https://doi.org/10.1038/s41586-021-04183-x
Hong S-W, Lee J, Kim MJ et al (2020) Clusterin protects lipotoxicity-induced apoptosis via upregulation of autophagy in insulin-secreting cells. Endocrinol Metab 35(4):943–953. https://doi.org/10.3803/EnM.2020.768
American College of Sports Medicine (2014) ACSM’s guidelines for exercise testing and prescription, 9th edn. Wolters Kluwer, Lippincott Williams & Wilkins, Baltimore, MD
Williams K, Carrasquilla GD, Ingerslev LR et al (2021) Epigenetic rewiring of skeletal muscle enhancers after exercise training supports a role in whole-body function and human health. Mol Metab 53:101290. https://doi.org/10.1016/j.molmet.2021.101290
Chow LS, Gerszten RE, Taylor JM et al (2022) Exerkines in health, resilience and disease. Nat Rev Endocrinol 18(5):273–289. https://doi.org/10.1038/s41574-022-00641-2
Sato S, Dyar KA, Treebak JT et al (2022) Atlas of exercise metabolism reveals time-dependent signatures of metabolic homeostasis. Cell Metab 34(2):329–345.e8. https://doi.org/10.1016/j.cmet.2021.12.016
Cunha DA, Igoillo-Esteve M, Gurzov EN et al (2012) Death protein 5 and p53-upregulated modulator of apoptosis mediate the endoplasmic reticulum stress–mitochondrial dialog triggering lipotoxic rodent and human β-Cell apoptosis. Diabetes 61(11):2763–2775. https://doi.org/10.2337/db12-0123
Bronczek GA, Soares GM, de Barros JF et al (2021) Resistance exercise training improves glucose homeostasis by enhancing insulin secretion in C57BL/6 mice. Sci Rep 11(1):8574. https://doi.org/10.1038/s41598-021-88105-x
Insel RA, Dunne JL, Atkinson MA et al (2015) Staging presymptomatic type 1 diabetes: a scientific statement of JDRF, the Endocrine Society, and the American Diabetes Association. Diabetes Care 38(10):1964–1974. https://doi.org/10.2337/dc15-1419
Tuomilehto J, Lindström J, Eriksson JG et al (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344(18):1343–1350. https://doi.org/10.1056/NEJM200105033441801
Knowler WC, Barrett-Connor E, Fowler SE et al (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346(6):393–403. https://doi.org/10.1056/NEJMoa012512
Fritsche A, Wagner R, Heni M et al (2021) Different effects of lifestyle intervention in high- and low-risk prediabetes: results of the randomized controlled prediabetes lifestyle intervention study (PLIS). Diabetes 70(12):2785–2795. https://doi.org/10.2337/db21-0526
Chudyk A, Petrella RJ (2011) Effects of exercise on cardiovascular risk factors in type 2 diabetes: a meta-analysis. Diabetes Care 34(5):1228–1237. https://doi.org/10.2337/dc10-1881
Schwingshackl L, Missbach B, Dias S, König J, Hoffmann G (2014) Impact of different training modalities on glycaemic control and blood lipids in patients with type 2 diabetes: a systematic review and network meta-analysis. Diabetologia 57(9):1789–1797. https://doi.org/10.1007/s00125-014-3303-z
Davies MJ, D’Alessio DA, Fradkin J et al (2018) Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 61(12):2461–2498. https://doi.org/10.1007/s00125-018-4729-5
Brusko TM, Russ HA, Stabler CL (2021) Strategies for durable β cell replacement in type 1 diabetes. Science 373(6554):516–522. https://doi.org/10.1126/science.abh1657
Bluestone JA, Buckner JH, Herold KC (2021) Immunotherapy: building a bridge to a cure for type 1 diabetes. Science 373(6554):510–516. https://doi.org/10.1126/science.abh1654
Acknowledgements
The authors are grateful to the study participants and to the study nurses A. Hamouda and D. Oger (Division of Endocrinology, Erasmus Hospital, Université Libre de Bruxelles, Brussels, Belgium).
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
ACdB contributed to the design and performance of the experiments, investigation and formal analysis, and wrote, revised and edited the manuscript. AEM, JMC-J and AC performed experiments and revised the article. CS, JC, VF, MC and MK contributed to create the training protocols; recruited, screened and randomised participants; performed maximal incremental tests; monitored training sessions; organised blood sampling; and revised the article. VF, MK, MC and DLE contributed to the original idea and the design, supervision and interpretation of the experiments. DLE wrote and revised the manuscript and MC edited it. All authors have read and approved the final version of the manuscript. ACdB is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
DLE is funded by the Walloon Region, Belgium, through the Welbio/FRFS project no. WELBIO-CR-(2019-CGR-X400120F) and by the Dutch Diabetes Research Foundation (project Innovate2CureType1, DDRF; no. 2018.10.002). VF, MK, MC and DLE are funded by the Brussels Region (INNOVIRIS BRIDGE grant DiaType); DLE and MC are supported by the Innovative Medicines Initiative 2 Joint Undertaking under grant agreements 115797 (INNODIA) and 945268 (INNODIA HARVEST). This Joint Undertaking receives support from the European Union’s Horizon 2020 research and innovation programme and the European Federation of Pharmaceutical Industries and Associations, JDRF and The Leona M. and Harry B. Helmsley Charitable Trust; MC is funded by the Fonds National de la Recherche Scientifique, the Walloon Region SPW-EERWin2Wal project BetaSource, Belgium, the Francophone Foundation for Diabetes Research (sponsored by the French Diabetes Federation, Abbott, Eli Lilly, Merck Sharp & Dohme and Novo Nordisk) and the European Foundation for the Study of Diabetes/Boehringer Ingelheim European Research Programme on ‘Multi-System Challenges in Diabetes’.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM
(PDF 106 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Coomans de Brachène, A., Scoubeau, C., Musuaya, A.E. et al. Exercise as a non-pharmacological intervention to protect pancreatic beta cells in individuals with type 1 and type 2 diabetes. Diabetologia 66, 450–460 (2023). https://doi.org/10.1007/s00125-022-05837-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-022-05837-9