Abstract
Aims/hypothesis
In patients with type 1 diabetes and end-stage renal disease (ESRD) we aimed to determine whether long-term normoglycaemia, as achieved by successful simultaneous pancreas and kidney (SPK) transplantation, would preserve kidney graft structure and function better than live donor kidney (LDK) transplantation alone.
Methods
Estimated GFR (eGFR) was calculated in SPK (n = 25) and LDK (n = 17) recipients in a stable phase 3 months after transplantation and annually during follow-up. Kidney graft biopsies were obtained at follow-up for measurement of glomerular volume (light microscopy), glomerular basement membrane (GBM) and podocyte foot process widths and mesangial volume fraction (electron microscopy).
Results
SPK and LDK recipients were similar in age and diabetes duration at engraftment. Donor age was higher in the LDK group. Median follow-up time was 10.1 years. Mean HbA1c levels during follow-up were 5.5 ± 0.4% (37 ± 5 mmol/mol) and 8.3 ± 1.5% (68 ± 16 mmol/mol) in the SPK and LDK group, respectively (p < 0.001). Compared with SPK recipients, LDK recipients had wider GBM (369 ± 109 nm vs 281 ± 57 nm; p = 0.008) and increased mesangial volume fraction (median 0.23 [range 0.13–0.59] vs 0.16 [0.10–0.41]; p = 0.007) at follow-up. Absolute eGFR change from baseline was −11 ± 21 and −23 ± 15 ml min−1 1.73 m−2 (p = 0.060), whereas eGFR slope was −1.1 (95% CI −1.7, −0.5) and −2.6 (95% CI −3.1, −2.1) ml min−1 1.73 m−2 per year in the SPK and LDK group, respectively (p = 0.001).
Conclusions/interpretation
In patients with type 1 diabetes and long-term normoglycaemia after successful SPK transplantation, kidney graft ultrastructure and function were better preserved compared with LDK transplantation alone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The clinical hallmarks for development of diabetic nephropathy are microalbuminuria and subsequent overt proteinuria and declining GFR [1]. As originally described in the Oslo study and later confirmed in the Diabetes Control and Complications Trial (DCCT) and the Epidemiology of Diabetes Interventions and Complications (EDIC) study, intensive insulin therapy delays the onset and slows the progression of diabetic nephropathy [2–4]. Further, it takes more than 5 years for microalbuminuria to develop in patients with type 1 diabetes and more than 10 years for overt proteinuria and clinical nephropathy to develop [1]. However, diabetic structural changes in the kidney can be detected at an earlier stage by morphometric analyses [5–7].
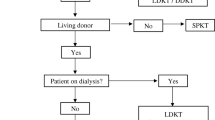
Kidney transplantation is the treatment of choice for patients with end-stage renal disease (ESRD), offering both improved survival and quality of life [8, 9]. In patients with type 1 diabetes and ESRD simultaneous pancreas and kidney (SPK) transplantation has become an established treatment [10–12]. At our centre we promote and prefer, whenever possible, the use of live kidney donors. During recent decades, as an alternative to SPK transplantation, many patients with diabetic ESRD have therefore undergone a kidney transplantation alone (KTA) [13]. Several reports have indicated equal or superior long-term kidney graft survival in patients with type 1 diabetes receiving a KTA from a live donor compared with those receiving an SPK transplant [14–16]. On the other hand, patient survival seems to be slightly better in patients receiving an SPK transplant than in those receiving single kidney allografts from live donors [13]. In this context there is little information on the structural and functional long-term outcome of kidney grafts exposed to hyperglycaemia compared with grafts exposed to normoglycaemia obtained by a simultaneous successful pancreatic transplantation.
In the present study we address the question whether long-term (10.1 year median follow-up) normoglycaemia, as achieved by successful SPK transplantation, would prevent changes in the structure and function of the kidney graft compared with LDK transplantation alone.
Methods
Patients
All patients with type 1 diabetes (n = 268) who were recipients of combined grafts (SPK, n = 147) or kidney grafts from live donors (LDK, n = 121) due to end-stage diabetic nephropathy in the period 21 June 1983 to 10 August 2003 were potential candidates to be included. Patients were included and examined between 9 October 2007 and 26 March 2012. In the SPK group 106 patients were no longer candidates either due to graft loss (pancreas, n = 56; kidney, n = 32) or death (n = 18) and 98 LDK recipients were no longer eligible either due to kidney graft loss (n = 37), pancreatic islets after kidney transplantation (n = 7), pancreas after kidney transplantation (n = 1) or death (n = 53), whichever came first. A total of 64 recipients (SPK, n = 41; LDK, n = 23) were contacted and asked to participate. Of these a total of 22 patients (SPK, n = 16; LDK, n = 6) were not studied further either due to refusal to participate or failure to be examined because of logistical problems. This left 42 patients with type 1 diabetes and ESRD who were either SPK (n = 25) or LDK (n = 17) recipients. Study participants gave their written informed consent. The study was approved by the Regional Committee for Medical and Health Research Ethics.
Glomerular structures in the kidney graft
Ultrasound guided percutaneous 18G kidney graft core needle biopsies were performed at follow-up. For light microscopy the biopsies were fixed in 4% (wt/vol.) formaldehyde (formalin) and embedded in paraffin. Tissue sections cut at 2 μm were stained with haematoxylin–eosin–saffron, periodic acid-Schiff and trichrome, respectively. For electron microscopy the biopsies were fixed in a 0.1 mol/l phosphate-buffered mixture of 2% (wt/vol.) paraformaldehyde and 0.5% (wt/vol.) glutaraldehyde and embedded in the non-polar methacrylate resin Lowicryl HM23 at low temperature. Light microscopy with semiquantitative estimation of kidney graft pathology was performed according to the Banff scheme and subsequent use of the chronic allograft damage index (CADI) [17, 18]. Morphometric measurements (AnalySIS Pro; Digital Soft Imaging System, Münster, Germany) of glomerular structures were performed by a single investigator who was blinded to the patient’s identity and clinical information. As a control the blinded procedure was performed twice by the same investigator in half of the patients. In addition a second investigator performed a quality check-up to ensure reproducibility and consistency of the estimates used in this study.
Glomerular area measurement was performed by tracing the outline of the glomerular visceral epithelium layer (Fig. 1a). Measurements were performed on central sections through intact glomeruli (excluding globally sclerotic glomeruli) at a magnification of ×190 according to the maximal profile area (MPA) method [19]. Glomerular volumes were determined by identifying the largest profile from a glomerulus and generating a radius from its area assuming the glomerular profile to be a circle. Glomerular volume was then calculated assuming the glomerulus to be a sphere. Measurements of glomerular basement membrane (GBM) width were performed on electron micrographs at a magnification of ×13,000, using the same interactive image analysis program as above, measuring the distance of a line orthogonal from the edge of the endothelial side to the edge of the epithelial side (Fig. 1b). The mean of five measurements was used from each of ten glomerular capillaries in two different glomeruli. The sample size (number of glomeruli, capillaries and measurements per capillary) was determined from a series of pilot experiments using cumulative mean plots for evaluation [20]. Electron micrographs at a magnification of ×890 were used to estimate the volume fraction of glomerular mesangium (Fig. 1c) by point counting [21]. Using the image analysis program with a superimposed square grid, the number of intersections falling on the mesangium, defined as the sum of the mesangial cells, mesangial matrix and mesangial glomerular basement membranes (GBMs), was counted and compared with the total number of intersections falling on the glomerular tuft. Estimation of per cent podocyte coverage of the capillary GBM was performed by intersection counting using the same micrographs as for measurement of GBM width but with a sample of parallel test lines superimposed in random directions (Fig. 1d) according to stereological principles [21]. Thus the number of intersections between the outer basement membrane surfaces covered by foot processes and a test line relative to the total number of intersections between a test line and the outer surface of the GBM was registered using the interactive image analysis program. The width of podocyte foot processes was measured by the method described by Deegens et al and recently advocated by Liu et al using the same sample of micrographs at ×13,000 magnification as above and the interactive image analyser for measuring the length of the basement membranes [22, 23].
(a) Glomerular area measurement was performed by tracing the outline (blue) of the glomerular visceral epithelium layer (scale bar, 100 μm). (b) Measurement of GBM width was performed on electron micrographs (scale bar, 2 μm), measuring the distance of a line (red) orthogonal from the edge of its endothelial to its epithelial side. (c) Electron micrographs (scale bar, 20 μm) were used to estimate the mesangial volume fraction. Using a superimposed square grid, the number of intersections (blue circles) falling on the mesangium, defined as the sum of the mesangial cells, mesangial matrix and mesangial GBMs, was counted and compared with the total number of intersections (sum of green and blue circles) falling on the glomerular tuft. (d) Estimation of per cent podocyte coverage of the capillary GBM was performed by intersection counting. Using a sample of parallel test lines superimposed in random directions, the number of intersections (green circles) between the outer basement membrane surfaces covered by foot processes and a test line relative to the total number of intersections (sum of green and blue circles) between a test line and the outer surface of the GBM were registered (scale bar, 2 μm)
Kidney graft function
Serum creatinine concentrations were measured in a stable phase 3 months post transplant and annually during follow-up. Estimated GFR (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [24]. Creatinine values obtained with the old non-isotope dilution mass spectrophotometry (IDMS)-standardised assay (all measurements performed before 26 June 2003) were converted to the new IDMS-traceable creatinine value. Kidney graft loss was defined as need for dialysis treatment or kidney re-transplantation.
Glycaemic control
HbA1c data were determined according to the DCCT standard and had been reported annually to the Norwegian Renal Registry since 1997 and were used for a more precise assessment of glycaemic control in SPK recipients and surveillance of conventional diabetes therapy in LDK recipients during follow-up. Pancreas graft loss was defined as need for insulin treatment or HbA1c ≥ 6.5% (48 mmol/mol). Diabetes in donor kidneys was ruled out by the pre-transplant work-up including OGTT in live donors before acceptance for donor nephrectomy. Absence of diabetes was a prerequisite for an individual to be considered for pancreas donation. Baseline (at the time of transplantation) biopsies of the kidney grafts were not routinely performed.
Statistical analyses
Demographic data were summarised and grouped by mode of treatment. Continuous variables are reported as the mean ± SD or median (range) depending on normality fit. Categorical data are described using frequencies. Student’s t test for independent samples or the Mann–Whitney U (Wilcoxon) test were used to compare continuous variables as appropriate. The χ 2 test was used to compare categorical variables. Spearman’s correlations were calculated between structural and functional variables. Simple linear regression analyses were used to determine the rate of decline in eGFR for each group, using all measured eGFR values during follow-up. All reported p values were two-tailed, and p values < 0.05 were considered significant. Statistical analyses were conducted using IBM SPSS Statistics for Windows, version 21 (IBM, Armonk, NY, USA).
Results
Patient characteristics
The demographics of the study population are shown in Table 1. For all participants, the median duration of follow-up after transplantation was 10.1 (7.2–20.5) years. There were no significant differences between SPK and LDK recipients in terms of sex, age at transplantation, diabetes duration prior to transplantation, age at follow-up, length of follow-up, zero HLA mismatch, kidney graft rejection episodes, basic immunosuppression or use of antihypertensive agents or statins. All patients received a calcineurin-based (CNI) regimen, either with ciclosporin or tacrolimus. In the LDK recipients the donor age was significantly higher (p < 0.001) and more patients tended to receive angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocker (ARB) therapy at follow-up compared with SPK recipients (p = 0.067).
Laboratory results
Data are presented in Table 2. In LDK recipients the HbA1c and triacylglycerol levels were significantly higher than in SPK recipients (p < 0.001 and p = 0.003, respectively), whereas no significant differences were seen between SPK and LDK recipients for ciclosporin or tacrolimus trough levels during follow-up or for total cholesterol, LDL-cholesterol, HDL-cholesterol, alanine transaminase or urinary protein/creatinine ratio at follow-up (at time of kidney graft biopsy).
Kidney graft structure
Data are given in Table 3, together with measurements performed on normal kidneys by other groups [22, 25, 26]. A light micrograph illustrating histological changes and an electron micrograph illustrating ultrastructural glomerular changes are shown in Fig. 2. Electron microscopy data could not be analysed in one patient in the SPK group because the biopsy was erroneously embedded in paraffin. One patient in the LDK group refused to have a kidney biopsy but undertook all the other examinations. Morphometric variables could not be evaluated in all patients due to a lack of representative glomeruli or arteries. Data on GBM and podocyte foot process widths, mesangial volume fraction and per cent podocyte coverage of the capillary GBM were available in 24 SPK and 16 LDK recipients, arteriolar hyalinosis score and the degree of fibrosis were available in 23 SPK and 15 LDK recipients and glomerular volume and CADI score were available in 20 SPK and 14 and 12 LDK recipients, respectively. In the LDK recipients the GBM width was significantly wider (p = 0.008) and the mesangial volume fraction was significantly higher (p = 0.007) than in SPK recipients at follow-up. There were no statistical differences in glomerular volume (p = 0.064), podocyte foot process width (p = 0.12), per cent podocyte coverage of the capillary GBM (p = 0.95), CADI score (p = 0.056), arteriolar hyalinosis score (p = 0.14) or in the degree of fibrosis (p = 0.23) between SPK and LDK recipients at follow-up.
(a) Light micrograph illustrating histological changes (scale bar, 100 μm). The glomeruli show increased amounts of mesangial matrix (arrows) and thickened capillary walls (arrowhead). The arterioles show hyaline thickening (short-tailed arrows). In addition, there is slight tubular atrophy and interstitial fibrosis (upper left). (b) Electron micrograph illustrating ultrastructural glomerular changes (scale bar, 5 μm). The basement membranes of the capillaries (C) are thickened, particularly in the lamina densa. In addition, the mesangium areas (M) are widened with increased amounts of matrix
We found a relationship between mesangial volume fraction and proteinuria (r = 0.48; p = 0.018) in the SPK group but not the LDK group (r = 0.22; p = 0.42). On the other hand, we found a relationship between GBM width and proteinuria in the LDK group (r = 0.51; p = 0.046) but not the SPK group (r = 0.22; p = 0.31).
Kidney graft function, blood pressure control and BMI
Data are given in Table 4. In a stable phase 3 months after transplantation there was no significant difference in serum creatinine between the SPK and LDK group (p = 0.23). The eGFR was 78 ± 17 and 69 ± 13 ml min−1 1.73 m−2 in SPK and LDK recipients, respectively (p = 0.059). From baseline to follow-up serum creatinine in the LDK group increased by 36 (−7 to 103) μmol/l compared with 14 (−29 to 86) μmol/l in the SPK recipients (p = 0.032). The eGFR significantly differed between the SPK and LDK recipients at follow-up (67 ± 24 vs 46 ± 14 ml min−1 1.73 m−2; p = 0.002) but the absolute fall in eGFR (ΔeGFR from baseline to follow-up) was not statistically different (p = 0.060). Linear regression analysis was performed to evaluate the rate of decline in eGFR from baseline in both groups. The slope of eGFR over the actual observation periods was −1.1 ml min−1 1.73 m−2 per year in SPK recipients, which was significantly better than −2.6 ml min−1 1.73 m−2 per year in the LDK group (p = 0.001). A subgroup analysis comparing the SPK and LDK recipients who were not on ACE inhibitor or ARB therapy showed that the SPK group declined 9 ± 22 ml min−1 1.73 m−2 and the LDK group 29 ± 17 ml min−1 1.73 m−2 from baseline to follow-up (p = 0.060). For those who were on ACE inhibitor or ARB therapy, the decline was 15 ± 22 and 19 ± 14 ml min−1 1.73 m−2 in the SPK and LDK group, respectively (p = 0.55). At baseline (3 months post transplant) and at follow-up there was no difference in blood pressure when comparing the SPK and LDK groups. At follow-up LDK recipients had gained a 7% increase in BMI from baseline compared with SPK recipients who did not develop any change in BMI (p = 0.051).
Discussion
The major finding in this single-centre long-term follow-up study of organ recipients with type 1 diabetes was that normoglycaemia, as achieved by successful SPK transplantation, was associated with better preserved GBM width and mesangial volume fraction in the kidney graft together with a reduced slope of eGFR when compared with LDK transplantation alone.
Development of biopsy-proven interstitial fibrosis is an important factor in the progression of kidney disease, including hyperglycaemia and CNI-induced nephropathy [27]. The degree of fibrosis was similar in the SPK and LDK groups at follow-up. All participants received CNI therapy, which is known to cause graft fibrosis in the long term [28, 29]. Arteriolar hyalinosis, common to diabetic nephropathy, did not differ between the SPK and LDK recipients. The reason for this may be that the fibrosis seen in our patients was primarily driven by CNI-induced nephrotoxicity rather than being an effect of hyperglycaemia [28, 30, 31].
Values for glomerular morphometric variables have quite a wide range in healthy individuals and also differ between kidneys from deceased and living donors [25, 26]. Caramori et al have reported data derived from living kidney donor tissues on glomerular volume, GBM width and mesangial volume fraction in healthy individuals (Table 3) [25]. Our data cannot easily be compared with those presented by Caramori et al, first of all due to different fixation and embedding methods and, second, due to different methods for measuring glomerular variables. In addition, the MPA method, as used in our study, tends to overestimate glomerular volume when compared with the Cavalieri method, which was used by Caramori et al [19, 25].
There was no significant difference in mean podocyte foot process width between the two groups. Unfortunately, the SD was quite large and more so among the LDK recipients. A contributing factor to this was the fact that two of the LDK recipients showed podocyte foot process widths in the order of 1,200 nm, indicating foot process effacement. Such a change was not observed among the pancreas transplant patients. Interestingly, despite differences in tissue preparation, the measured podocyte foot process width in our series was comparable with the values measured by Deegens et al and Liu et al in their healthy control patients [22, 23].
Previous studies have shown that survival is superior in SPK patients even when compared with LDK recipients [13, 15]. On the other hand, only a limited number of studies have addressed whether successful SPK transplantation, with long-term normoglycaemia, prevents recurrence of diabetic glomerulopathy in the kidney graft [32–35]. Shortcomings of these studies have been small patient groups, suboptimal normalisation of plasma glucose and short follow-up (often less than 5 years). Some ultrastructural signs of diabetic nephropathy have been observed as early as 2 years after diagnosis of type 1 diabetes [36, 37]. Furthermore, recurrent diabetic glomerular lesions have been found in the transplanted kidneys as early as 2 years post transplant in KTA recipients [38–40]. However, it takes several years for glomerulosclerosis with impairment of renal function to develop. Also after successful pancreatic transplantation it can take more than 5 years to reverse diabetic lesions in native kidneys [41].
Our study also assessed kidney graft function. The eGFR tended to be somewhat better preserved in the SPK group compared with LDK recipients, although the difference did not reach statistical significance when looking at absolute eGFR change from baseline (p = 0.060). However, when all measurements over the actual observation periods were taken into consideration the negative slopes of eGFR in the SPK group were less than half those for LDK recipients, a difference that was highly significant in favour of SPK recipients (p = 0.001). Such a difference may obviously be of clinical significance. Confounding effects from rejection episodes of the transplanted kidneys are less likely since the frequency of rejections was similar in the SPK and LDK group and all acute rejections, except for one, occurred <3 months after transplantation. Moreover, there were no differences in blood pressure either at baseline or at follow-up. However, more patients in the LDK group tended to use ACE inhibitors or ARBs. One would assume that long-term use of these drugs would help preserve normotension and tend to stabilise renal function rather than cause deterioration. However, we acknowledge the potential confounding effects of ACE inhibitor or ARB therapy on eGFR. Donor age was substantially lower in SPK recipients and this may explain a superior eGFR in the SPK group at baseline. Donor age may also have influenced the course of eGFR during follow-up.
Albuminuria is a hallmark of diabetic glomerulopathy. Despite the differences in kidney graft structure between the two groups, there was no difference in proteinuria at follow-up. Again, recipients of LDK tended to receive more antihypertensive agents including ACE inhibitors and ARBs. This could have blurred a possible difference in proteinuria between the two groups. Proteinuria may also be due to causes other than hyperglycaemia in kidney-transplanted patients with diabetes (e.g. toxic effects of CNIs, which were used equally in the two groups).
There are strong relationships between glomerular structure and renal function across the spectrum of proteinuria [42]. The relationships between glomerular structures and proteinuria in our study differed between SPK and LDK recipients: in the SPK group there was a relationship with mesangial volume fraction and in the LDK group there was a relationship with GBM width. We have no explanation for the difference between the SPK and LDK group in our study concerning the relationship between ultrastructural measures and proteinuria. The difference may be due to the fact that there is considerable structural overlap among the degree of proteinuria and the patient numbers are also small for evaluation of such associations.
To our knowledge, our report represents one of the largest single-centre studies on the effect of kidney transplant structure and function after establishment of normoglycaemia with SPK transplantation. Compared with other similar studies, our study also has the longest follow-up, which is of major importance when studying changes in both renal structure and function. Bohman et al reported that kidney graft biopsies from two SPK recipients were devoid of diabetic changes 2 years post transplant, when compared with six diabetic patients each transplanted with a single kidney [32]. They concluded that combined transplantation appeared to prevent recurrence of diabetic nephropathy. However, the study is limited by a small number of included patients, a short follow-up time and poor metabolic control in the KTA group. Wilczek et al presented a larger cohort of 20 SPK and 30 KTA recipients (18 deceased donors and 12 LDKs) in which kidney graft biopsies were taken 1.0–6.5 and 1.0–6.8 years, respectively, after transplantation [33]. They concluded that a functioning pancreatic graft prevents development of diabetic nephropathy. Somewhat in contrast to these findings, Nyberg et al found that despite a successful SPK transplantation, recurrence of early diabetic glomerular changes could be seen after 2–4 years follow-up in 11 recipients of a combined segmental pancreas and kidney graft [34]. However, these recipients (SPK) had impaired glucose control with a mean HbA1c of 7.2% (55 mmol/mol) and only two out of 11 SPK recipients were categorised with normal glycaemic control.
Bilous et al reported data from 12 recipients who underwent pancreas after kidney (PAK) transplantation [35]. Pancreatic transplantation was performed 1.0–7.2 years (a mean of 4.2 years) after KTA in this study. Renal biopsies were performed prior to successful pancreatic transplantation (PAK) and at mean follow-up time 4.4 years post transplant. These biopsies were compared with biopsies obtained after similar follow-up time in KTA recipients. Mesangial volume fraction was lower in the PAK than in the KTA recipients although GBM thickness was not significantly different possibly due to the relatively short follow-up time. One must also remember that these transplanted kidneys had been exposed to 1.0–7.2 years of hyperglycaemia prior to PAK and this may have contributed to the aborted effect of subsequent normoglycaemia.
The advantages of our study are that it represents a homogenous single-centre study and has a long-term follow-up. Limitations of the present study include its retrospective and non-randomised design and the fact that baseline (at the time of transplantation) biopsies of the kidney grafts were not performed. Data from baseline biopsies would have added relevant information. However, we have no reason to believe that there were systematic differences between the two groups of donor kidneys at the time of transplantation regarding the estimated morphometric variables. Long-term success of SPK transplantation is the exception, as indicated by the large number of ineligible individuals. Those diabetic patients who are uraemic are at high risk of cardiovascular complications and premature death. This is reflected by the high number of patients ineligible for study due to death. Also, the extrapolation of our data to non-white individuals may be questioned.
The evidence up until now suggests, however, that successful pancreatic transplantation ameliorates the development of diabetic glomerulopathy in the transplanted kidneys. The major finding in our study in this context is that normoglycaemia (mean HbA1c value of 5.5% [37 mmol/mol] during follow-up), as compared with moderate hyperglycaemia (mean HbA1c value of 8.3% [68 mmol/mol] during follow-up), protects the transplanted kidney grafts against overt diabetic changes with increased basement membrane width and increased glomerular mesangial volume fraction when assessed after a median follow-up time of 10.1 years post transplant.
In conclusion, in patients with type 1 diabetes and ESRD, long-term normoglycaemia after successful SPK transplantation resulted in better preservation of kidney graft ultrastructure and function compared with LDK transplantation alone.
Abbreviations
- ACE:
-
Angiotensin-converting enzyme
- ARB:
-
Angiotensin receptor blocker
- CADI:
-
Chronic allograft damage index
- CNI:
-
Calcineurin inhibitor
- DCCT:
-
Diabetes Control and Complications Trial
- eGFR:
-
Estimated glomerular filtration rate
- ESRD:
-
End-stage renal disease
- GBM:
-
Glomerular basement membrane
- KTA:
-
Kidney transplantation alone
- LDK:
-
Live donor kidney
- MPA:
-
Maximal profile area
- PAK:
-
Pancreas after kidney
- SPK:
-
Simultaneous pancreas and kidney
References
Selby JV, FitzSimmons SC, Newman JM, Katz PP, Sepe S, Showstack J (1990) The natural history and epidemiology of diabetic nephropathy. Implications for prevention and control. JAMA 263:1954–1960
Dahl-Jørgensen K, Hanssen KF, Kierulf P, Bjoro T, Sandvik L, Aagenaes O (1988) Reduction of urinary albumin excretion after 4 years of continuous subcutaneous insulin infusion in insulin-dependent diabetes mellitus. The Oslo Study. Acta Endocrinol (Copenh) 117:19–25
The Diabetes Control and Complications Trial (DCCT) Research Group (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 329:977–986
The Epidemiology of Diabetes Interventions and Complications (EDIC) study (2003) Sustained effect of intensive treatment of type 1 diabetes mellitus on development and progression of diabetic nephropathy. JAMA 290:2159–2167
Østerby R (1974) Early phases in the development of diabetic glomerulopathy. Acta Med Scand Suppl 574:3–82
Steffes MW, Ellis EN, Mauer SM (1986) Complications of diabetes mellitus and factors affecting their progression. Clin Chem 32:B54–B61
Mauer SM, Steffes MW, Ellis EN, Sutherland DE, Brown DM, Goetz FC (1984) Structural-functional relationships in diabetic nephropathy. J Clin Invest 74:1143–1155
Wolfe RA, Ashby VB, Milford EL et al (1999) Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med 341:1725–1730
Evans RW, Manninen DL, Garrison LP Jr et al (1985) The quality of life of patients with end-stage renal disease. N Engl J Med 312:553–559
Gruessner AC (2011) 2011 update on pancreas transplantation: comprehensive trend analysis of 25,000 cases followed up over the course of twenty-four years at the International Pancreas Transplant Registry (IPTR). Rev Diabet Stud 8:6–16
Sollinger HW, Odorico JS, Becker YT, D’Alessandro AM, Pirsch JD (2009) One thousand simultaneous pancreas-kidney transplants at a single center with 22-year follow-up. Ann Surg 250:618–630
Sutherland DE, Gruessner RW, Dunn DL et al (2001) Lessons learned from more than 1,000 pancreas transplants at a single institution. Ann Surg 233:463–501
Lindahl JP, Hartmann A, Horneland R et al (2013) Improved patient survival with simultaneous pancreas and kidney transplantation in recipients with diabetic end-stage renal disease. Diabetologia 56:1364–1371
Rayhill SC, D’Alessandro AM, Odorico JS et al (2000) Simultaneous pancreas-kidney transplantation and living related donor renal transplantation in patients with diabetes: is there a difference in survival? Ann Surg 231:417–423
Morath C, Zeier M, Dohler B, Schmidt J, Nawroth PP, Opelz G (2008) Metabolic control improves long-term renal allograft and patient survival in type 1 diabetes. J Am Soc Nephrol 19:1557–1563
Young BY, Gill J, Huang E et al (2009) Living donor kidney versus simultaneous pancreas-kidney transplant in type I diabetics: an analysis of the OPTN/UNOS database. Clin J Am Soc Nephrol 4:845–852
Racusen LC, Solez K, Colvin RB et al (1999) The Banff 97 working classification of renal allograft pathology. Kidney Int 55:713–723
Isoniemi H, Taskinen E, Hayry P (1994) Histological chronic allograft damage index accurately predicts chronic renal allograft rejection. Transplantation 58:1195–1198
Lane PH, Steffes MW, Mauer SM (1992) Estimation of glomerular volume: a comparison of four methods. Kidney Int 41:1085–1089
Bolender RP (1978) Correlation of morphometry and stereology with biochemical analysis of cell fractions. Int Rev Cytol 55:247–289
Weibel ER (1979) Stereological methods. Vol. 1: Practical methods for biological morphometry. Academic, London
Deegens JK, Dijkman HB, Borm GF et al (2008) Podocyte foot process effacement as a diagnostic tool in focal segmental glomerulosclerosis. Kidney Int 74:1568–1576
Liu XJ, Zhang YM, Wang SX, Liu G (2014) Ultrastructural changes of podocyte foot processes during the remission phase of minimal change disease of human kidney. Nephrology (Carlton) 19:392–397
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Caramori ML, Basgen JM, Mauer M (2003) Glomerular structure in the normal human kidney: differences between living and cadaver donors. J Am Soc Nephrol 14:1901–1903
Toyoda M, Najafian B, Kim Y, Caramori ML, Mauer M (2007) Podocyte detachment and reduced glomerular capillary endothelial fenestration in human type 1 diabetic nephropathy. Diabetes 56:2155–2160
Nath KA (1992) Tubulointerstitial changes as a major determinant in the progression of renal damage. Am J Kidney Dis 20:1–17
Myers BD, Ross J, Newton L, Luetscher J, Perlroth M (1984) Cyclosporine-associated chronic nephropathy. N Engl J Med 311:699–705
Nankivell BJ, Borrows RJ, Fung CL, O’Connell PJ, Allen RD, Chapman JR (2003) The natural history of chronic allograft nephropathy. N Engl J Med 349:2326–2333
Harris RD, Steffes MW, Bilous RW, Sutherland DE, Mauer SM (1991) Global glomerular sclerosis and glomerular arteriolar hyalinosis in insulin dependent diabetes. Kidney Int 40:107–114
Mihatsch MJ, Antonovych T, Bohman SO et al (1994) Cyclosporin A nephropathy: standardization of the evaluation of kidney biopsies. Clin Nephrol 41:23–32
Bohman SO, Tydén G, Wilczek H et al (1985) Prevention of kidney graft diabetic nephropathy by pancreas transplantation in man. Diabetes 34:306–308
Wilczek HE, Jaremko G, Tyden G, Groth CG (1995) Evolution of diabetic nephropathy in kidney grafts. Evidence that a simultaneously transplanted pancreas exerts a protective effect. Transplantation 59:51–57
Nyberg G, Holdaas H, Brekke IB et al (1996) Glomerular ultrastructure in kidneys transplanted simultaneously with a segmental pancreas to patients with type 1 diabetes. Nephrol Dial Transplant 11:1029–1033
Bilous RW, Mauer SM, Sutherland DE, Najarian JS, Goetz FC, Steffes MW (1989) The effects of pancreas transplantation on the glomerular structure of renal allografts in patients with insulin-dependent diabetes. N Engl J Med 321:80–85
Mauer M, Drummond K (2002) The early natural history of nephropathy in type 1 diabetes: I. Study design and baseline characteristics of the study participants. Diabetes 51:1572–1579
Drummond K, Mauer M (2002) The early natural history of nephropathy in type 1 diabetes: II. Early renal structural changes in type 1 diabetes. Diabetes 51:1580–1587
Mauer SM, Steffes MW, Connett J, Najarian JS, Sutherland DE, Barbosa J (1983) The development of lesions in the glomerular basement membrane and mesangium after transplantation of normal kidneys to diabetic patients. Diabetes 32:948–952
Østerby R, Nyberg G, Hedman L, Karlberg I, Persson H, Svalander C (1991) Kidney transplantation in type 1 (insulin-dependent) diabetic patients. Early glomerulopathy. Diabetologia 34:668–674
Hariharan S, Smith RD, Viero R, First MR (1996) Diabetic nephropathy after renal transplantation. Clinical and pathologic features. Transplantation 62:632–635
Fioretto P, Steffes MW, Sutherland DE, Goetz FC, Mauer M (1998) Reversal of lesions of diabetic nephropathy after pancreas transplantation. N Engl J Med 339:69–75
Caramori ML, Kim Y, Huang C et al (2002) Cellular basis of diabetic nephropathy: 1. Study design and renal structural-functional relationships in patients with long-standing type 1 diabetes. Diabetes 51:506–513
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
JPL, FPR, AH and TJ designed the study, analysed and interpreted the data and wrote the manuscript. IAE, KM, HH, LTD, TMR, SOK, RH, OØ and KB participated in the design of the study, interpreted the data and edited the manuscript. All authors read, commented on and approved the final version of the manuscript to be published. JPL, AH and TJ are responsible for the integrity of the work as a whole.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lindahl, J.P., Reinholt, F.P., Eide, I.A. et al. In patients with type 1 diabetes simultaneous pancreas and kidney transplantation preserves long-term kidney graft ultrastructure and function better than transplantation of kidney alone. Diabetologia 57, 2357–2365 (2014). https://doi.org/10.1007/s00125-014-3353-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-014-3353-2