Abstract
Despite human healthcare advances, some microorganisms continuously react evolving new survival strategies, choosing between a commensal fitness and a pathogenic attitude. Many opportunistic microbes are becoming an increasing cause of clinically evident infections while several renowned infectious diseases sustain a considerable number of deaths. Besides the primary and extensively investigated role of immune cells, other cell types are involved in the microbe-host interaction during infection. Interestingly, mesenchymal stem cells (MSCs), the current leading players in cell therapy approaches, have been suggested to contribute to tackling pathogens and modulating the host immune response. In this context, this review critically explores MSCs’ role in E. coli, S. aureus, and polymicrobial infections. Summarizing from various studies, in vitro and in vivo results support the mechanistic involvement of MSCs and their derivatives in fighting infection and in contributing to microbial spreading. Our work outlines the double face of MSCs during infection, disease, and sepsis, highlighting potential pitfalls in MSC-based therapy due to the MSCs’ susceptibility to pathogens’ weapons. We also identify potential targets to improve infection treatments, and propose the potential applications of MSCs for vaccine research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Better understanding of stem cell behavior at sites of inflammation appears to be a key strategy in developing new approaches for in situ tissue regeneration [1]. Mesenchymal stem cells (MSCs) are adult stem cells with a broad tissue distribution [2], such as bone marrow [3], adipose tissue [4], and dental pulp [5]. MSCs are able to self-renew and differentiate into mesodermal and non-mesodermal cell lineages contributing to tissue homeostasis and regeneration, thus becoming increasingly interesting for clinical applications [2]. Moreover, their easy availability and broad differentiation potential, together with their low immunogenicity, have greatly increased interest in applying them in cell-based therapy and regenerative approaches. Evidence suggests MSCs contribute to host defense and inflammation, in case of tissue injury or inflammatory diseases. MSCs are considered crucial regulators of tissue regeneration even under such harsh environmental conditions. Indeed, currently, the most attractive feature identifying MSCs as a promising tool for the treatment of immune disease is their immune-modulatory capability [5, 6]. The heterogeneous effects of bacteria on MSCs observed in studies reflect the complexity underlying the interactions between stem cells and bacteria. Although inflammation represents the main host defense against microbial infections, the absence or inhibition of the pro-inflammatory cytokines produced during sepsis (such as TNF-α, IL-1β, IFN-γ, IL-18) improves survival in some experimental models [7], suggesting that excessive inflammation in sepsis could worsen the course of the pathology. An inflammatory environment like sepsis promotes autophagy and apoptosis of MSCs [8]. On the other hand, however, complete immunosuppression of the host has been observed to be equally detrimental. Indeed, lack of a proper immune defense is a common feature in patients affected by sepsis [9, 10], often due to splenocyte deficiency in producing pro-inflammatory cytokines [11] or to immune cell apoptosis [10], which could increase sepsis lethality. Taken together, such evidence suggests that developing immunomodulatory strategies utilizing MSCs could avoid worsening of the pathology and speed up the patient’s recovery. However, several findings have now highlighted MSCs’ susceptibility to microbial infection, potentially questioning their effectiveness in a clinical situation. Most of the available literature is based on preclinical models and in vitro studies, as the clinical applications are still at an early stage. The aim of this review is to summarize the latest findings about the role of MSCs and their derivatives in various models of infectious disease, reporting the effects on the microbes and the final outcome (Tables 1, 2, 3, and 4), highlighting the double involvement of MSCs in infection and sepsis (Fig. 1). Furthermore, we provide an update on the actual potential, and side effects, of this powerful autologous source of treatment so as to pave the way for further developments and initiatives in the field of immunotherapy. A critical analysis of the current findings is indeed urgently needed to guide clinical applications in a bench-to-bedside setting [12]. This review thoroughly describes the state-of-the-art interplay between MSCs and the most common microbes in the clinical setting. The outcomes from different experimental models and different sources of MSCs are described, overall indicating MSCs and their derivatives as a valuable tool to treat infectious diseases, but urging an accurate evaluation of the most effective source of MSCs.
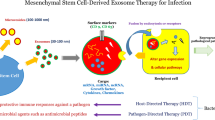
Role of MSCs during infection. The first barrier encountered by bacteria is the epithelium. Microbial components and their associated antigens elicit an immune response in the host. Even though the bacteria-host interaction can result in clinically silent infection like commensalism, the bacteria are characterized by different adhesion and entry machinery to attack mammalian cells. The microbes sharing PAMPs are recognized by the host immune system. Microbes produce many virulent factors able to promote a pathogenic interaction with the host. The immune system can recognize microbes thanks to TLRs. MSCs can help the immune system fighting the infection, by producing antibacterial responses through AMPs (e.g., LL-37, β-defensin, lipocalin, and hepcidin), immunomodulatory/immunosuppressant molecules (e.g., IDO and HLA-G), anti-inflammatory cytokines (e.g., IL10). Some of the molecules mediating the effects of MSCs are often secreted in MVs. MSCs can modulate the ratio of T cells/T-reg and T cells that interacted with MSCs may contribute to infection resolution. Many MSCs’ secreted molecules can influence T cell function. However, inadequate immune response and a pro-inflammatory environment may lead to tissue damages, chronic infections, and sepsis. PAMPs, pathogen-associated molecular patterns; TLR, Toll-like receptors; MSCs, mesenchymal stem cells; AMPs, antimicrobial peptides; LPS, lipopolysaccharide; IDO, indoleamine 2,3-dioxygenase; MVs, microvesicles; TNF-α, tumor necrosis factor alpha; T-reg, regulatory T cell
Functioning features of MSCs
MSC role during infection
The mechanisms underlying microbial pathogenesis differ according to the acquired and individual characteristics of both the host and the microbe, each one giving an opposite but equally important contribution to the course of infection [13]. The human body is the final determinant in whether an infection and possible sepsis set in. Recently, close attention has been paid to host defenses, with the aim of finding potential weapons against the most virulent microbial phenotypes.
In case of infection, MSCs can help the body out through two possible mechanisms: (i) promoting direct bacterial killing, helping the host to clear the pathogen or (ii) indirectly promoting host survival, decreasing the side effects of infection, such as tissue damage, and thus the lethality of sepsis. The evidence supporting the role of MSCs in infection is based on data from various animal and cellular models; considering the range of technical approaches used, it is difficult to compare and consolidate the results (Tables 1, 2, 3, and 4). Moreover, it is not fully understood whether the main weapon is the cell itself or its secretome. In infection onset, progression, and outcome, MSCs’ role may present two sides: on the one hand, they can help the host by immunosuppressing the environment, avoiding exacerbation of pathological symptoms, helping to heal tissue damage, and allowing the establishment of an immune tolerant environment; on the other hand, however, excessive immune suppression, as well as MSCs’ sensitivity to microbial infection, can lead to the opposite effect, hampering the host from fighting the infection and, instead, encouraging microbial effectors to spread.
Pattern recognition receptors
The process by which the innate immune system senses microbial infection is based on the interaction between host pattern recognition receptors (PRRs) and highly shared pathogen-associated molecular patterns (PAMPs) with conserved motifs that the immune system learned to recognize during evolution. Toll-like receptors (TLRs) are probably the best-known membrane-PPRs. TLRs are expressed by immune and non-immune cells and can bind a large series of exogenous and endogenous ligands, including nucleic acids, lipids, and carbohydrates. TLRs activate key signaling transduction pathways [14] involved in the regulation of inflammatory processes and allow the development of immunological memory against the foreign harmful microbes. Different TLR ligands can activate different inflammatory pathways. In particular, stimulation of TLR2, TLR4, and TLR9 is able to activate NF-κB and IRF transcription factors [14].
Immune privilege of MSCs
MSCs are considered immune privileged, as they express several distinctive TLRs (at least TLR1, TLR2, TLR3, TLR4, TLR5, TLR6), but they express only low levels of HLA class I molecules, and totally lack expression of HLA class II, CD40, CD80, and CD86 [15]. This makes MSCs a useful tool for cell therapy applications, allowing the employment of allogeneic-sourced applications in life-threatening conditions, especially when isolation and expansion of autologous MSCs are not feasible [16, 17]. In humans, the expression of some TLRs has been reported in different sources of MSCs. Whether TLR expression can have an effect on proliferation and migration of MSCs is still controversial [18]. In addition, investigation of the role of TLRs on MSC immunomodulation capacity has generated a conflicting idea about the contribution of TLRs to eventual pro-inflammatory or anti-inflammatory MSC-phenotype polarization. The cell response elicited in the MSCs in each specific condition might be dependent not only on the TLR ligand involved but also on the different tissue origin of the MSCs. Thus, the employment of specific molecules mimicking PAMPs could be a useful tool in cell therapy, by way of ex vivo priming of the MSCs before infusing them into the host, in order to pre-determine their in vivo polarization, and finally promote survival/immunosuppression [19]. These properties suggest that MSCs are a useful tool for circumventing graft-versus-host disease (GvHD). Indeed, MSCs have been used to treat GvHD in patients undergoing hematopoietic stem cell transplantation, successfully decreasing GvHD incidence and severity [20, 21]. The low expression of HLA class I, together with the expression of other surface molecules, such as poliovirus receptor (PVR), makes MSCs a natural target for natural killer (NK) cell–mediated killing [22]. On the other hand, MSCs can also strongly alter the NK cell phenotype and suppress cytokine secretion and cytotoxicity against HLA class I–expressing targets. Moreover, MSCs also inhibit NK proliferation, a mechanism where indoleamine 2,3-dioxygenase (IDO) and prostaglandin E2 (PGE2) play a key role [23].
Immunomodulatory action of MSCs
Although differences in the self-renewal and differentiation potential of MSCs deriving from different tissues have been observed [24, 25], the immune modulatory capability seems to be a commonly shared feature. MSCs are activated by inflammatory mediators, such as TNF-α and IFN-γ [26, 27]. They are able in turn to affect several immune cell populations, such as T cells, B cells, and NK cells [28,29,30,31,32], both by cell contact-dependent mechanisms, e.g., by Fas-Fas-L [33] or Notch1 [34], and by releasing a set of soluble factors able to modulate the immune response. MSCs express and release a plethora of immunologically active molecules, mostly with anti-inflammatory properties, namely, TGF-β, granulocyte-macrophage colony–stimulating factor (GMCSF), PGE2, IL-6, IL-10, IL-13, IL17, IL22, IDO, HLA-G, and TNF-α-stimulated gene/protein 6 (TSG-6) [35, 36]. They are also able to release antimicrobial peptides, such as LL-37 β-defensin, lipocalin, IDR-1, and hepcidin. Functional alterations as impaired immunoregulatory and homing ability may occur in MSCs undergoing senescence [37].
MSCs and the immune barrier aid
In the last few decades, our knowledge about the regeneration and repairing mechanisms of human organs has improved substantially, but our ability to utilize this knowledge to establish regeneration strongly depends on the injury location and entity. Stem cells and progenitor cells have been characterized in several tissues, and such reservoirs play a fundamental role in initial immune response and in the tissue healing processes following infection. Mucosae comprise a stromal compartment where the MSCs (i) modulate how the host responds to microbes [38] and/or (ii) directly differentiate contributing to tissue healing and maintenance. The MSCs located in the epithelial niches can already sense the microbial effectors and mediate inflammation, but, in addition, a plethora of signals and cellular events can recruit distant MSCs to the injury site [39, 40]. MSCs also support epithelial sheet proliferation in a paracrine manner [41], enhancing the protecting role of the epithelium as a physical and functional barrier limiting spatial invasion by microbes. Moreover, MSCs increase the frequency of the regulatory T (T-reg) cell compartment, helping to establish a more immunotolerant environment [42].
MSCs and bacteria
The specific interaction between bacteria and MSCs is receiving considerable attention among the scientific community, both because of the now-unraveled interplay between stem cells and microbiome in the physiological state and because of the fundamental role of this interaction during tissue healing. Most of the evidence refers to Escherichia coli (Table 1) and Staphylococcus aureus (Table 2), the widest studied Gram− and Gram+ species, abundant in the environment and well characterized as pathogenic models. For instance, in a recent in vitro study, equine MSCs isolated from the peripheral blood of healthy horses, and their MSC conditioned medium (MSC-CM), demonstrated the ability to inhibit both E. coli and S. aureus growth. In fact, employment of antibodies blocking the antimicrobial peptides (cystatin C, elafin, cathelicidin, and lipocalin-2) reduced that beneficial effect of MSCs-CM on bacterial membrane depolarization [43].
MSCs and E. coli
In C57BL/6 mice, intravenous administration of murine bone marrow–derived MSCs (BM-MSCs) was shown to exert a healing effect on lung inflammation, healing, and edema, after endotoxin intraperitoneal instillation [44]. To the best of our knowledge, the first hypothesis that MSCs might have a specific protective effect on E. coli–induced acute lung injury (ALI) was investigated in a mouse model by Gupta et al. in 2007, where BM-MSCs were isolated from C57BL/6 donor mice, cultured, and administered to C57BL/6 recipients after E. coli endotoxin was delivered intrapulmonarily [45]. Treatment with MSCs derived from C57BL/6J mice also significantly reduced LPS-induced pulmonary inflammation, and, in that context, angiopoietin production was also shown to bolster their beneficial effect [46]. In a simple in vivo model of endotoxemia (cecal ligation and puncture and endotoxin injection), treatment with human adipose–derived MSCs (hAD-MSCs) or murine AD-MSCs (syngeneic from C57Bl/6 mice or allogeneic from Balb/c mice) was shown to increase survival after high-dose lipopolysaccharide (LPS) administration [47]. On the other hand, senescent human BM-MSCs (hBM-MSCs) failed to protect against lethal endotoxemia induced by intraperitoneal LPS injection in a murine model [48]. The therapeutic effect of allogeneic hBM-MSCs on ALI induced by intrabronchial instillation was studied in a model of ex vivo human perfused lung preparation by Lee et al. in 2009: treatment with allogeneic hBM-MSCs, and even hBM-MSC-CM, restored the normal fluid balance [49]. The cells, when pre-treated with a keratinocyte growth factor (KGF) siRNA and instilled, likewise lost their therapeutic benefits, while recombinant KGF partially restored the beneficial effect. A similar perfused model was improved by the same group using live E. coli in order to induce pneumonia: again, hBM-MSCs restored alveolar fluid clearance to a normal level, but also reduced neutrophil influx and bacterial load in the lung by increasing alveolar macrophage phagocytosis [50]. In a different study, intratracheal treatment in ICR mice with human umbilical cord blood–derived MSCs (hUCB-MSCs) attenuated the severity of ALI by down-modulating inflammatory cytokines [51]. In addition, the bacterial colony count was reduced both in vivo (broncho-alveolar lavage (BAL) and blood) and in vitro by the presence of MSCs [51]. Intratracheal transplantation of C57BL/6 mice–derived BM-MSCs in an ALI murine model induced by E. coli obtained similar results: BM-MSCs improved survival by reducing inflammation, and decreased bacterial colony-forming units (CFU) in BAL, effects in part explained by secretion of antimicrobial peptides [52]. Part of the beneficial paracrine effect of the MSCs is thought to reside in secreted microvesicles (MVs) and exosomes (EXs). The protective effect of hBM-MSC-MVs was first described in a model of endotoxin-induced ALI [53]. A better model of pneumonia that was developed by intratracheal instillation of E. coli in mice demonstrated specifically that MSC-MVs (prepared by ultracentrifugation) were as effective as their parent hBM-MSCs in improving survival. The therapeutic effect of the MVs was equivalent to the MSCs in mitigating acute lung injury by reducing neutrophil influx, edema, and wall thickening [54]. The total bacterial load was reduced in vivo both by intravenous and intratracheal administration of MVs. Such improved survival after MV injection was possible partly through a KGF-mediated effect, while the microbial clearance was mediated by enhanced phagocytosis. In this study, CD44 was found critical for vesicle uptake by phagocytes [54]. On the other hand, a similar model was established in rats and hBM-MSCs were administered either intratracheally or intravenously [55]. In particular, intravenous delivery increased antimicrobial peptide (i.e., LL-37) concentrations in alveoli, BAL, and plasma [55]. The monocytes collected from the infected models showed enhanced phagocytic activity, while in vitro the monocytes stimulated with hBM-MSCs were better phagocytes if exposed to E. coli [55]. However, in this study, the paracrine efficacy of hBM-MSCs in reducing the severity of pneumonia was inferior to direct cell treatment, even though animal survival increased [55]. The importance of the capability of the MSCs to enhance phagocytosis was also remarked with neutrophils and their role in infection. Indeed, mouse MSCs, isolated from compact bone, enhanced the ability of peritoneal neutrophils to phagocytize E. coli in vitro and in vivo [56]. Again, LPS-stimulated BM-MSCs induced polymorphonuclear neutrophil granulocyte (NG) chemotaxis and supernatants of LPS-stimulated BM-MSC enhanced the E. coli uptake by NGs [57]. Bacterial preconditioning was sufficient to inhibit the growth of E. coli in vitro by hUCB-MSC supernatants (as well as hUCB-MSCs themselves), while in vivo the hUCB-MSCs attenuated ALI through their microbicidal factors, mainly mediated by beta-defensin 2 secretion, and an anti-inflammatory effect, in which TLR4 seemed critical [58]. Similarly, a more recent study showed that after E. coli injection, neonatal mice receiving intravenously preconditioned hUCB-MSCs increased their survival more than non-conditioned cells [59]. A recent model of E. coli–induced chronic bacterial prostatitis was established in rats; here, the treatment with rat BM-MSCs decreased the inflammation reaction [60]. Worth of note, in a mouse LPS-induced sepsis model, despite the different sources of MSCs, similar survival rates and pro-/anti-inflammatory mechanisms were observed [61]. Furthermore, specific MSC sources, e.g., menstrual MSCs (MenSCs), not only relieved ALI symptoms and showed an anti-inflammatory profile but also brought about a tissue reparative effect [62]. To elucidate the deleterious role of LPS in respect to MSCs, once again in vitro studies were useful: LPS did not alter the immunophenotype but modified the lineage commitment and immunomodulatory capacity of periodontal ligament (PDL) stem cells (PDLSCs) [63]. In addition, LPS treatment in PDLSCs [63] and in BM-MSCs [64] stimulated the expression of the anti-inflammatory factor COX2.
Specific strategies to counteract E. coli infection may reside in antimicrobial peptide production by MSCs.
LL-37 is the unique bioactive form of human cathelicidin derived by cleavage of propeptide human cationic antimicrobial peptide-18 (hCMP18) [65]. LL-37 production is upregulated in hBM-MSCs exposed to E. coli [66]. Human BM-MSCs and their CM reduced E. coli growth and CFU counts during co-incubation; furthermore, they proved antimicrobial in an E. coli–induced pneumonia mouse model where activity was decreased by LL-37 sera [66]. LL-37 was also administered by intratracheal instillation into the lungs and inhibited LPS-induced TNF-α levels by alveolar macrophages [67]. No increase in LL-37 secretion was associated with the preconditioning of MSCs that were delivered intravenously to attenuate E. coli–induced neonatal sepsis in rats, even though plasma levels of the antimicrobial peptide were higher in MSC-treated rats than in saline-treated ones [59].
Iron is an important source for the growth of E. coli. TLR stimulation after E. coli recognition by immune cells is known to increase the levels of lipocalin-2 antimicrobial peptide and sequestrate iron for bacterial growth [68]. Intratracheal instillation of E. coli in wild-type mice augmented the levels of lipocalin-2 by airway epithelia and reduced the number of bacteria in the lungs compared with lipocalin-deficient mice [69]. Another study had previously shown that lipocalin-deficient mice, infected intraperitoneally with E. coli, had a lower survival than the wild type [70]. Again, the neutrophils isolated from the same knockout mice were impaired in bacteriostatic activity [70]. Moreover, mice receiving syngeneic BM-MSC treatment after ALI upregulated lipocalin-2 levels, while anti-lipocalin-2 antibodies reduced the protective antibacterial effect of syngeneic BM-MSCs [52]. Pre-stimulation, for example by LPS, can enhance in vitro MSC lipocalin gene expression and secretion [52].
Other broadly active natural antimicrobial peptides were linked to the antimicrobial activity of MSCs, namely, the hepcidin and β-defensin families.
Mammalian hosts produce hepcidin, an iron-regulatory hormone that exerts control over the trafficking of iron and causes hypoferremia [71, 72]. IL-6 is the main cytokine inducing hepcidin expression [71], while several microbe-derived Toll-like receptor ligands (e.g., PAMP) stimulate hepcidin transcription [73]. Hepcidin plays different roles according to the site of infection caused by extracellular or intracellular bacteria. Hepcidin may have a detrimental effect on infections by intracellular pathogens because of intracellular iron storage in macrophages [73, 74]. Interestingly, treatment of E. coli K88 bacteria with porcine hepcidin (with its limited bactericidal activity) decreased the adherence to epithelial cells by causing bacteria aggregation, thus showing that hepcidin has an iron-independent effect [73]. After peritoneal injection of several E. coli clinical isolates, hepcidin-1 knockout usually potentiated infection. Furthermore, post-infection treatment of knockout mice with a hepcidin agonist prevented sepsis-associated mortality [72]. Consideration of data produced in vitro and structural similarities with the defensin family led to the hypothesis of a direct antimicrobial role by hepcidin in vivo [74].
β-Defensin 2 secreted via TLR4, in particular, was associated with the main antimicrobial activity of UC-MSCs achieved in vitro after E. coli exposure or in vivo against E. coli–induced ALI [58]. The results obtained from E. coli infection models are summarized in Tables 1 and 4.
MSCs and S. aureus
The first experimental study on the interaction between MSCs and S. aureus [75] investigated their intrinsic antimicrobial capacity; a few years back, CD-1 mice–derived adipose tissue–derived MSCs (AD-MSCs) were also conjectured to improve antibiotic treatment of staphylococcal wound infections [76]. Indeed, that study revealed that TLR ligand-activated AD-MSCs were able, in vitro, to reduce S. aureus growth [76]. The hypothesis was later confirmed both in mouse and dog models of chronic biofilm infection [77]. A responsive migration by allogeneic hBM-MSCs was surmised as a consequence of local infection of the epithelial cell line [50], while UCB-MSCs were shown to be able to internalize S. aureus in co-culture experiments [78]. The early hypothesis discussing the potential role of MSCs in supporting antibiotic therapy was again considered when it was shown that preconditioning of hBM-MSCs with a specific antibiotic enhanced the internalization capacity earlier described for S. aureus, while reducing necrosis of hBM-MSCs [79]. Of course, the characteristic of the in vivo model supposedly resembling the disease caused by S. aureus might generate contrasting opinion as to the benefit of MSCs as an antibacterial therapy. Bone hydrogel-based implantation of rat BM-MSCs in a rat ostectomy model aggravates the development of osteomyelitis in infected animals [80] rather than contributing to the clearance of the infection. In the same study, non-significant levels of LL-37 were observed after bacterial challenge in the in vitro setting [80]. In different reports, attentive to the wound healing problem, hBM-MSCs were tested for their migratory ability and resistance to apoptosis after biofilm-conditioned media exposure; such conditioning was found to result in the reduction of both features [81]. New strategies based on co-administration of MSCs and antimicrobial agents are emerging in wound healing models. In particular, the combination of C57BL/6 mouse–derived AD-MSCs with particular proteins, instead of antibiotics, reduced bacterial load and accelerated the wound healing rate [82]. Despite the important contribution of hBM-MSC and hUCB-MSC secretome in the interaction with E. coli, regarding S. aureus, the activity of Wharton’s jelly–derived MSCs (WJ-MSCs) involved in bacterial clearance was recently suggested to be associated with a cell-cell direct MSC-pathogen interaction [79]. However, in an in vivo model of S. aureus infection, LL-37 was described as ameliorating methicillin-resistant Staphylococcus aureus (MRSA)–induced pneumonia by decreasing the anti-inflammatory response [83]. LL-37 levels, on the other hand, were enhanced in BM supernatants stimulated by biofilm-conditioned media derived from S. aureus culture [81]. LL-37 was shown to inhibit LPS-induced osteoclast formation [84]. Recently, beta-defensin overexpression augmented the rat BM-MSC antibacterial effect while promoting the bone healing impaired by S. aureus contamination, in a rat calvarial defect model [85]. Results in models of S. aureus infection are summarized in Table 2.
MSCs and polymicrobial protection
Models of polymicrobial infection (Table 3) are useful tools for mimicking clinical conditions such as peritonitis and can be obtained from gut injury, e.g., by cecal ligation and puncture (CLP). Observation of MSCs’ antibacterial effects was initially based on CLP models. Briefly, after cecum perforation, the model treated with AD-MSCs was monitored for survival. Both mouse and human AD-MSCs were protective in the CLP model [47]. Since mice receiving CLP develop into a polymicrobial sepsis model, Mei et al. analyzed CLP-derived ALI [86]. MSC administration not only prevented lung injury but together with antibiotic treatment was able to reduce mortality [86]. Importantly, bacterial clearance, assessed as the number of CFUs from spleen homogenates post-CLP, was augmented in mice with sepsis and then treated with MSCs. Ex vivo phagocytic activity was increased in CD11+ cells isolated from the septic mice, but there was no difference between the mice infected with E. coli and S. aureus [86]. This study described only a moderate phagocytosis capacity on the part of MSCs for both gram-negative and gram-positive bacteria [86]. The opinion in favor of a combined antibiotic-MSC treatment seemed to increase in accordance with data generated both in vitro and in vivo using MenSCs [87]. These MSCs showed a direct antibacterial activity and, synergizing with antibiotics, in vivo greatly improved the survival rate in the CLP mouse model. Moreover, these cells enhanced bacterial clearance in peritoneal fluid and blood and reducing sepsis-mediated organ injury, by decreasing both pro- and anti-inflammatory cytokines without decreasing the T and B cell number. The CM produced by the same cells also demonstrated MenSCs’ indirect antibacterial activity which is enhanced by preconditioning with bacteria in co-culture, whereas in the CLP-sepsis model, the CM inhibited bacterial growth, increasing the effect when in combination with antibiotics. MenSCs showed antibacterial activity in vitro against a fecal bacterial mixture [87].
Unusually, the antibacterial in vitro activity correlated with hepcidin-dependent mechanisms, rather than those of the best-known antimicrobial peptides. In a mouse model, the toxic shock effect of S. aureus enterotoxin A increased in severity when combined with LPS administration, but interestingly, an intraperitoneal injection of AD-MSCs was able to rescue animals from lethality [88]. A recent work showed how human WJ-MSCs minimize multi-organ injury in a CLP model of sepsis in rats [89].
In a rat model of CLP-induced sepsis, hBM-MSC and hWJ-MSC administration was able to both increase the percentage of circulating CD4+CD25+ T-reg cells, increasing the T-reg/T cell ratio, and decrease pro-inflammatory cytokine expression (IL-6 and TNF-α), as compared with the vehicle [90]. Moreover, in the same model, the decrease in immunosuppressive capacity of T-reg cells observed after sepsis was restored by both hBM-MSC and hWJ-MSC administration. In another sepsis model in mice, induced by E. coli and fecal content in the abdominal cavity, treatment with mAD-MSCs reduced mouse mortality to 40% and prevented splenocyte apoptosis and TNF-α increase, while it increased IL-10, as compared with the untreated septic group which had 100% mortality [91]. When mBM-MSCs are transplanted into the inflammatory microenvironment of CLP mice, the inflammatory cytokines (e.g., TNF-α and IFN-γ) are able to activate caspase 3 and start apoptosis events which are enhanced by blocking reactive oxygen species (ROS) generation and ERK activation [8]. Genetic inhibition of autophagy was effective in reducing the apoptosis rate after MSC transplantation [8]. The crucial role of TLRs in human clinical study was investigated in a model of experimental sepsis, where mouse AD-MSCs were unable to modify the mRNA expression of the different TLRs evaluated in various tissues [92]. The results obtained on polymicrobial infection models are summarized in Tables 3 and 4.
Microvesicles and MSC-derived molecules
Despite the variety of types of MSC discovered in different tissue sources, a common feature is their ability to release active molecules within membrane-surrounded vesicles, MVs. There are several types of MV, differing in size, shape, molecular composition, and content. Usually, they are produced as a result of intracellular vesicle sorting. Recent nomenclature describes MVs as being shed from the plasma membrane and of > 200 nm diameter, while exosomes, originating from the endosome/exosome system, are of 50–200 nm diameter. Exosomes are one of the most studied subtypes of MSC-derived MV. MSC-derived exosomes are able to alter the activity of target cells by horizontal transfer [93]. One of the main functions of MVs is to communicate within the tissues, delivering DNA, lipids, and proteins. Their peculiar characteristics make MVs a basic element of data transmission extended to other organisms such as symbiotic or pathogenic communities. The MVs’ content provides cells with strong regulatory information, especially in the context of immune system crosstalk. Bacteria produce MVs to regulate stress response and quorum sensing. Bacterial outer membrane vesicles (OMVs) are specific vesicles that are now part of next-generation vaccines [94]. Changes in the exosome pool are associated with many pathogenic backgrounds [95]. The ability to isolate MVs and use them as a therapeutic tool could be an important step forward in MSC-based therapy advancement, allowing use of MSC-derived active molecules and their beneficial properties but avoiding whole cell administration and the risk associated with their engraftment. Like their “parents,” because of their dual role in physiological homeostasis and pathogenic contribution, MVs may intimidate the scientist when it comes to using them as a natural or artificial carrier of a drug. MVs’ potential has been analyzed in several tissue-injury models, such as tetrachloride-induced liver injury [96]; ischemia/reperfusion-induced myocardial injury [97, 98]; cisplatin-induced [99], gentamicin-induced [100], and ischemia/reperfusion-induced kidney injury [101]; and hypoxia-induced lung hypertension [102]. The high potential of MVs is supported by results, recently summarized by others [103], demonstrating that MV administration in preclinical animal models is safe and that MVs hold at least the same effectiveness as MSC administration, contributing to the amelioration of tissue/organ pathology. MVs are acellular material that have still undefined consent by regulatory agencies. MVs have lower antigenicity than synthetic nanosystems [104], suggesting that using MSC-released molecules, in the form of purified or supernatant surrogates, may revolutionize medical biotechnology in the field of infectious diseases.
Discussion
In this review, we have emphasized how MSC co-delivery/delivery can be efficient in attenuating diseases caused by bacteria. First of all, choosing the source of MSCs in order to treat a bacterial infection will be decisive for the final outcome. Indeed, in this review, we thoroughly cited the source and strain of MSCs in the experimental results as different sources have been shown to exert different patterns of immunomodulatory/antimicrobial activity. However, few papers have compared the immunomodulatory capacity of MSCs from different tissue sources [105]. Our incomplete understanding of the mechanism of MSC-based immunomodulation [106] cautions us to be careful before approaching transplantation, as the outcome may well be dependent on the disease status or the local microenvironment. BM-MSCs are currently the preferred source of MSCs in clinical trials, perhaps because they represent the traditional and best-characterized cell type. However, it is important to highlight that alternative sources of MSCs like adipose tissue and cord blood have shown an even stronger immunosuppressive activity than BM-MSCs [105]. Generally, the most common cell sources used for MSC therapy are bone marrow, adipose tissue, and cord blood [107, 108]. It is also important to note that culture conditions are likely to alter the ex vivo immunomodulatory properties of MSCs. The local environment, including pre-exposition to stimuli, may well affect MSCs’ immunomodulatory function [109], which has to be taken into account, especially when dealing with bacteria with a different tissue tropism. The ability to spread to adjacent tissues and at distant sites of antimicrobial peptides (AMPs) and MVs suggests a promising tool to defeat bacterial infections, as we have described in this review. Unfortunately, no comparative study regarding AMP production among the different sources of MSCs has been found in the literature and secretome differences continue to raise a variety of issues. For example, the secretome of UC-MSCs often differs from MSCs from bone marrow and adipose tissue [110]. In addition, further investigation is required for us to comprehend the mechanisms that underlie the migration of MSCs towards specific tissues and the secretion of anti-inflammatory molecules. Knowing that would be a critical step towards a correct choice of the source of MSCs acting against specific infection.
Both preclinical and humans studies focusing on human diseases other than infections support the hypothesis that several kinds of MSCs derived from allogeneic donors could be utilized in clinical therapy [108, 111]. In the context of antimicrobial activity, we did not note any superiority of allogeneic versus autologous MSCs, despite the fact that autologous MSCs may have an impaired potential for self-MSC deficiencies—secondary or intrinsic to the disease itself. Considering this, MSC-donor differences (inter-variability and intra-variability) become the most relevant uncontrolled aspects of both allo- and autologous cell-based approaches in cell therapies [112].
MSC senescence should be considered in the definition of a treatment, since gene expression and paracrine activity by stem cells are likely to be changed in antibacterial outcomes. The best mediators of MSC secretory activity are MVs. This “stem product factory” may be the ideal candidate for treating inflammation-related pathologies [95]. They could be engineered and delivered, providing further advantages such as avoiding the senescent and damaged DNA of transplanted cells and comprising small-sized “healing” molecules spreading better throughout the body. The results obtained on animal models of sepsis show discrepancies from human clinical trials. However, tissue engineering technologies and 3D cell culture advances have given rise to a new field, called tissue microbiology [113], where microbiologists and cell biologists join hands in exploring the microbial dynamics, observing the ex vivo or intravital response of the host tissue environment when exposed to a pathogen or its effectors.
Preconditioning may be an important strategy to trigger the MSCs potential for treating bacterial infection. Selecting the molecule to be used is critical because it must be restricted to positive effects alone. For example, treatment with LPS can induce IDO expression in human PDL cells [114], but this advantage is offset by subsequent modification of the mesodermal differentiation potential [63]. MSCs have been shown to contact host innate immune cells to increase their own antibacterial activity. In this case, preconditioning with TLRs will be an option to investigate. Interestingly, LL-37 increased proliferation, growth factor secretion, and migration in a transwell chamber via formyl peptide receptor-like 1 (FPRL1) from human AD-MSCs [115]. Again, in placenta-derived MSCs, LL-37 caused increased migration during a scratch assay as well as a higher immunosuppressive profile with a remarkable expression of TLR3 [116]. Hence, not only MSCs preconditioning with specific antibiotics but also preconditioning of MSCs with specific cytokines [59] or preconditioning with both antimicrobial peptides and antibiotics can all be strategies to boost the MSCs’ antibacterial effect. In the context of drug-resistant infections, it may be possible to prime the antimicrobial and immunological properties of MSCs ex vivo to enhance their later therapeutic outcome. Perhaps preconditioning will develop our ideas about using autologous MSCs against infection. Lastly, an ongoing research and a better understanding of AMPs, including their interaction with TLRs [117], will be useful to exploit the AMP potential in MSC-based therapy as well. Hepcidin is a peptide hormone regulating iron homeostasis as well as being advocated as an antimicrobial peptide [74]. Hepcidin seems to exert both iron- and non-iron-dependent antimicrobial effects on E. coli [72, 73] while MenSC-derived hepcidin has shown an antimicrobial effect in vitro [87]. Even though the hepatocytes are the main source of hepcidin, upregulation has also been seen in immune cells at the site of bacterial infection [74]. The production of hepcidin by MSCs may be a novel strategy for the treatment of infections with extracellular bacteria.
Since sepsis is a frequent cause of death in hospitalized patients, MSC administration has been seen as an alternative therapy to modulate the deregulated immune system of such patients [118]. Intravenous or intraperitoneal administration of MSCs could be a valuable tool to treat sepsis, especially because of the injuries that sepsis causes to many tissues and organs. Conveniently, MSCs are able to migrate to many injured tissues, such as the liver [119], myocardium [120], kidney [121], lung [122], and brain [111]. Furthermore, regarding the ex vivo modulation occurring in MSCs, genetic or pharmacological inhibition of autophagy might increase MSC survival under sepsis [8] and thus represent a novel immunotherapy approach.
Conclusion
So far, all the data produced have made it possible to start currently ongoing clinical trial studies on MSC treatment for sepsis syndrome, as well as for lung injury [77] [12]. The leap into MSC clinical trials to treat infections seems imminent, but in order to start new human clinical studies, the evaluation of preclinical reports remains an important ongoing task [12].
References
Chatzivasileiou K, Kriebel K, Steinhoff G, Kreikemeyer B, Lang H (2015) Do oral bacteria alter the regenerative potential of stem cells? A concise review. J Cell Mol Med 19:2067–2074
Sheng G (2015) The developmental basis of mesenchymal stem/stromal cells (MSCs). BMC Dev Biol 15:44
Friedenstein AJ, Gorskaja JF, Kulagina NN (1976) Fibroblast precursors in normal and irradiated mouse hematopoietic organs. Exp Hematol 4:267–274
Zuk PA, Zhu M, Ashjian P, de Ugarte DA, Huang JI, Mizuno H, Alfonso ZC, Fraser JK, Benhaim P, Hedrick MH (2002) Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell 13:4279–4295
Gronthos S, Mankani M, Brahim J, Robey PG, Shi S (2000) Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proc Natl Acad Sci U S A 97:13625–13630
Doorn J, Moll G, Le Blanc K et al (2012) Therapeutic applications of mesenchymal stromal cells: paracrine effects and potential improvements. Tissue Eng B Rev 18:101–115
Wiersinga WJ, Leopold SJ, Cranendonk DR, van der Poll T (2014) Host innate immune responses to sepsis. Virulence 5:36–44
Dang S, Yu Z, Zhang C, Zheng J, Li KL, Wu Y, Qian LL, Yang ZY, Li XR, Zhang Y, Wang RX (2015) Autophagy promotes apoptosis of mesenchymal stem cells under inflammatory microenvironment. Stem Cell Res Ther 6:247
van der Poll T, Opal SM (2008) Host-pathogen interactions in sepsis. Lancet Infect Dis 8:32–43
Hotchkiss RS, Monneret G, Payen D (2013) Sepsis-induced immunosuppression: from cellular dysfunctions to immunotherapy. Nat Rev Immunol 13:862–874
Boomer JS, To K, Chang KC et al (2011) Immunosuppression in patients who die of sepsis and multiple organ failure. JAMA 306:2594–2605
Lalu MM, Sullivan KJ, Mei SH et al (2016) Evaluating mesenchymal stem cell therapy for sepsis with preclinical meta-analyses prior to initiating a first-in-human trial. Elife 17:5
Casadevall A, Pirofski LA (2000) Host-pathogen interactions: basic concepts of microbial commensalism, colonization, infection, and disease. Infect Immun 68:6511–6518
Kawasaki T, Kawai T (2014) Toll-like receptor signaling pathways. Front Immunol 5:461
Kahan BD (2003) Timeline: individuality: the barrier to optimal immunosuppression. Nat Rev Immunol 3:831–838
Le Blanc K, Tammik C, Rosendahl K et al (2003) HLA expression and immunologic properties of differentiated and undifferentiated mesenchymal stem cells. Exp Hematol 31:890–896
Mitchell JB, McIntosh K, Zvonic S, Garrett S, Floyd ZE, Kloster A, di Halvorsen Y, Storms RW, Goh B, Kilroy G, Wu X, Gimble JM (2006) Immunophenotype of human adipose-derived cells: temporal changes in stromal-associated and stem cell-associated markers. Stem Cells 24:376–385
DelaRosa O, Dalemans W, Lombardo E (2012) Toll-like receptors as modulators of mesenchymal stem cells. Front Immunol 3:1–8
Sangiorgi B, Panepucci RA (2016) Modulation of immunoregulatory properties of mesenchymal stromal cells by Toll-like receptors: potential applications on GVHD. Stem Cells Int 2016:9434250–9434210
Baron F, Storb R (2012) Mesenchymal stromal cells: a new tool against graft-versus-host disease? Biol Blood Marrow Transplant 18:822–840
Wei X, Yang X, Han Z, Qu FF, Shao L, Shi YF (2013) Mesenchymal stem cells: a new trend for cell therapy. Acta Pharmacol Sin 34:747–754
Spaggiari GM, Capobianco A, Becchetti S, Mingari MC, Moretta L (2006) Mesenchymal stem cell-natural killer cell interactions: evidence that activated NK cells are capable of killing MSCs, whereas MSCs can inhibit IL-2-induced NK-cell proliferation. Blood 107:1484–1490
Spaggiari GM, Capobianco A, Abdelrazik H, Becchetti F, Mingari MC, Moretta L (2008) Mesenchymal stem cells inhibit natural killer-cell proliferation, cytotoxicity, and cytokine production: role of indoleamine 2,3-dioxygenase and prostaglandin E2. Blood 111:1327–1333
Noël D, Caton D, Roche S, Bony C, Lehmann S, Casteilla L, Jorgensen C, Cousin B (2008) Cell specific differences between human adipose-derived and mesenchymal-stromal cells despite similar differentiation potentials. Exp Cell Res 314:1575–1584
De Ugarte DA, Morizono K, Elbarbary A et al (2003) Comparison of multi-lineage cells from human adipose tissue and bone marrow. Cells Tissues Organs 174:101–109
Krampera M, Cosmi L, Angeli R, Pasini A, Liotta F, Andreini A, Santarlasci V, Mazzinghi B, Pizzolo G, Vinante F, Romagnani P, Maggi E, Romagnani S, Annunziato F (2006) Role for interferon-gamma in the immunomodulatory activity of human bone marrow mesenchymal stem cells. Stem Cells 24:386–398
Prasanna SJ, Gopalakrishnan D, Shankar SR, Vasandan AB (2010) Pro-inflammatory cytokines, IFNgamma and TNFalpha, influence immune properties of human bone marrow and Wharton jelly mesenchymal stem cells differentially. PLoS One 5:e9016. https://doi.org/10.1371/journal.pone.0009016
Di Nicola M, Carlo-Stella C, Magni M et al (2002) Human bone marrow stromal cells suppress T-lymphocyte proliferation induced by cellular or nonspecific mitogenic stimuli. Blood 99:3838–3843
Krampera M, Glennie S, Dyson J et al (2003) Bone marrow mesenchymal stem cells inhibit the response of naive and memory antigen-specific T cells to their cognate peptide. Blood 101:3722–3729
Ghannam S, Pène J, Moquet-Torcy G et al (2010) Mesenchymal stem cells inhibit human Th17 cell differentiation and function and induce a T regulatory cell phenotype. J Immunol 185:302–312
Prigione I, Benvenuto F, Bocca P, Battistini L, Uccelli A, Pistoia V (2009) Reciprocal interactions between human mesenchymal stem cells and gammadelta T cells or invariant natural killer T cells. Stem Cells 27:693–702
Corcione A, Benvenuto F, Ferretti E, Giunti D, Cappiello V, Cazzanti F, Risso M, Gualandi F, Mancardi GL, Pistoia V, Uccelli A (2006) Human mesenchymal stem cells modulate B-cell functions. Blood 107:367–372
Akiyama K, Chen C, Wang D, Xu X, Qu C, Yamaza T, Cai T, Chen WJ, Sun L, Shi S (2012) Mesenchymal-stem-cell-induced immunoregulation involves FAS-ligand-/FAS-mediated T cell apoptosis. Cell Stem Cell 10:544–555
Liotta F, Angeli R, Cosmi L, Filì L, Manuelli C, Frosali F, Mazzinghi B, Maggi L, Pasini A, Lisi V, Santarlasci V, Consoloni L, Angelotti ML, Romagnani P, Parronchi P, Krampera M, Maggi E, Romagnani S, Annunziato F (2008) Toll-like receptors 3 and 4 are expressed by human bone marrow-derived mesenchymal stem cells and can inhibit their T-cell modulatory activity by impairing Notch signaling. Stem Cells 26:279–289
Brun J, Abruzzese T, Rolauffs B, Aicher WK, Hart ML (2016) Choice of xenogenic-free expansion media significantly influences the myogenic differentiation potential of human bone marrow–derived mesenchymal stromal cells. Cytotherapy 18:344–359
Choi H, Lee RH, Bazhanov N, Oh JY, Prockop DJ (2011) Anti-inflammatory protein TSG-6 secreted by activated MSCs attenuates zymosan-induced mouse peritonitis by decreasing TLR2/NF-κB signaling in resident macrophages. Blood 118:330–338
Turinetto V, Vitale E, Giachino C (2016) Senescence in human mesenchymal stem cells: functional changes and implications in stem cell-based therapy. Int J Mol Sci 17:1164
Le Blanc K, Mougiakakos D (2012) Multipotent mesenchymal stromal cells and the innate immune system. Nat Rev Immunol 12:383–396
Shi Y, Su J, Roberts AI, Shou P, Rabson AB, Ren G (2012) How mesenchymal stem cells interact with tissue immune responses. Trends Immunol 33:136–143
Le Blanc K, Davies LC (2015) Mesenchymal stromal cells and the innate immune response. Immunol Lett 168:140–146
Wannemuehler TJ, Manukyan MC, Brewster BD, Rouch J, Poynter JA, Wang Y, Meldrum DR (2012) Advances in mesenchymal stem cell research in sepsis. J Surg Res 173:113–126
Bassi ÊJ, de Almeida DC, Moraes-Vieira PMM, Câmara NOS (2012) Exploring the role of soluble factors associated with immune regulatory properties of mesenchymal stem cells. Stem Cell Rev 8:329–342
Harman RM, Yang S, He MK, Van De Walle GR (2017) Antimicrobial peptides secreted by equine mesenchymal stromal cells inhibit the growth of bacteria commonly found in skin wounds. Stem Cell Res Ther 8:157
Xu J, Woods CR, Mora AL et al (2007) Prevention of endotoxin-induced systemic response by bone marrow-derived mesenchymal stem cells in mice. Am J Physiol Lung Cell Mol Physiol 293:131–141
Gupta N, Su X, Popov B, Lee JW, Serikov V, Matthay MA (2007) Intrapulmonary delivery of bone marrow-derived mesenchymal stem cells improves survival and attenuates endotoxin-induced acute lung injury in mice. J Immunol 179:1855–1863
Mei SHJ, McCarter SD, Deng Y et al (2007) Prevention of LPS-induced acute lung injury in mice by mesenchymal stem cells overexpressing angiopoietin 1. PLoS Med 4:e269. https://doi.org/10.1371/journal.pmed.0040269
Gonzalez-Rey E, Anderson P, Gonzalez MA, Rico L, Buscher D, Delgado M (2009) Human adult stem cells derived from adipose tissue protect against experimental colitis and sepsis. Gut 58:929–939
Sepúlveda JC, Tomé M, Fernández ME et al (2014) Cell senescence abrogates the therapeutic potential of human mesenchymal stem cells in the lethal endotoxemia model. Stem Cells 32:1865–1877
Lee JW, Fang X, Gupta N, Serikov V, Matthay MA (2009) Allogeneic human mesenchymal stem cells for treatment of E. coli endotoxin-induced acute lung injury in the ex vivo perfused human lung. Proc Natl Acad Sci 106:16357–16362
Lee JW, Krasnodembskaya A, McKenna DH et al (2013) Therapeutic effects of human mesenchymal stem cells in ex vivo human lungs injured with live bacteria. Am J Respir Crit Care Med 187:751–760
Kim E, Chang Y, Choi S et al (2011) Intratracheal transplantation of human umbilical cord blood-derived mesenchymal stem cells attenuates Escherichia coli-induced acute lung injury in mice. Respir Res 12:108
Gupta N, Krasnodembskaya A, Kapetanaki M, Mouded M, Tan X, Serikov V, Matthay MA (2012) Mesenchymal stem cells enhance survival and bacterial clearance in murine Escherichia coli pneumonia. Thorax 67:533–539
Zhu Y-G, Feng X-M, Abbott J, Fang XH, Hao Q, Monsel A, Qu JM, Matthay MA, Lee JW (2014) Human mesenchymal stem cell microvesicles for treatment of Escherichia coli endotoxin-induced acute lung injury in mice. Stem Cells 32:116–125
Monsel A, Zhu YG, Gennai S et al (2015) Therapeutic effects of human mesenchymal stem cell-derived microvesicles in severe pneumonia in mice. Am J Respir Crit Care Med 192:1–63
Devaney J, Horie S, Masterson C, Elliman S, Barry F, O’Brien T, Curley GF, O’Toole D, Laffey JG (2015) Human mesenchymal stromal cells decrease the severity of acute lung injury induced by E. coli in the rat. Thorax 70:625–635
Hall SRR, Tsoyi K, Ith B, Padera RF Jr, Lederer JA, Wang Z, Liu X, Perrella MA (2013) Mesenchymal stromal cells improve survival during sepsis in the absence of heme oxygenase-1: the importance of neutrophils. Stem Cells 31:397–407
Brandau S, Jakob M, Bruderek K, Bootz F, Giebel B, Radtke S, Mauel K, Jäger M, Flohé SB, Lang S (2014) Mesenchymal stem cells augment the anti-bacterial activity of neutrophil granulocytes. PLoS One 9:e106903. https://doi.org/10.1371/journal.pone.0106903
Sung DK, Chang YS, Sung SI, Yoo HS, Ahn SY, Park WS (2016) Antibacterial effect of mesenchymal stem cells against Escherichia coli is mediated by secretion of beta- defensin- 2 via toll- like receptor 4 signalling. Cell Microbiol 18:424–436
Zhu Y, Xu L, Collins JJP et al (2017) Human umbilical cord mesenchymal stromal cells improve survival and bacterial clearance in neonatal sepsis in rats. Stem Cells Dev. https://doi.org/10.1089/scd.2016.0329
Yi S, Han G, Shang Y, Liu C, Cui D, Yu S, Liao B, Ao X, Li G, Li L (2016) Microbubble-mediated ultrasound promotes accumulation of bone marrow mesenchymal stem cell to the prostate for treating chronic bacterial prostatitis in rats. Sci Rep 6:19745
Ou H, Zhao S, Peng Y, Xiao X, Wang Q, Liu H, Xiao X, Yang M (2016) Comparison of bone marrow tissue- and adipose tissue-derived mesenchymal stem cells in the treatment of sepsis in a murine model of lipopolysaccharide-induced sepsis. Mol Med Rep 14:3862–3870
Xiang B, Chen L, Wang X, Zhao Y, Wang Y, Xiang C (2017) Transplantation of menstrual blood-derived mesenchymal stem cells promotes the repair of LPS-induced acute lung injury. Int J Mol Sci 18. doi: https://doi.org/10.3390/ijms18040689
Kukolj T, Trivanović D, Djordjević IO, Mojsilović S, Krstić J, Obradović H, Janković S, Santibanez JF, Jauković A, Bugarski D (2018) Lipopolysaccharide can modify differentiation and immunomodulatory potential of periodontal ligament stem cells via ERK1,2 signaling. J Cell Physiol 233:447–462
Németh K, Leelahavanichkul A, Yuen PST, Mayer B, Parmelee A, Doi K, Robey PG, Leelahavanichkul K, Koller BH, Brown JM, Hu X, Jelinek I, Star RA, Mezey É (2009) Bone marrow stromal cells attenuate sepsis via prostaglandin E2–dependent reprogramming of host macrophages to increase their interleukin-10 production. Nat Med 15:42–49
Dürr UHN, Sudheendra US, Ramamoorthy A (2006) LL-37, the only human member of the cathelicidin family of antimicrobial peptides. Biochim Biophys Acta Biomembr 1758:1408–1425
Krasnodembskaya A, Song Y, Fang X et al (2012) Antibacterial effect of human mesenchymal stem cells is mediated in part from secretion of the antimicrobial peptide LL-37. Stem Cells 28:2229–2238
Brown KL, Poon GFT, Birkenhead D, Pena OM, Falsafi R, Dahlgren C, Karlsson A, Bylund J, Hancock REW, Johnson P (2011) Host defense peptide LL-37 selectively reduces proinflammatory macrophage responses. J Immunol 186:5497–5505
Flo TH, Smith KD, Sato S, Rodriguez DJ, Holmes MA, Strong RK, Akira S, Aderem A (2004) Lipocalin 2 mediates an innate immune response to bacterial infection by sequestrating iron. Nature 432:917–921
Wu H, Santoni-Rugiu E, Ralfkiaer E, Porse BT, Moser C, Høiby N, Borregaard N, Cowland JB (2010) Lipocalin 2 is protective against E. coli pneumonia. Respir Res 11:96
Berger T, Togawa A, Duncan GS, Elia AJ, You-ten A, Wakeham A, Fong HEH, Cheung CC, Mak TW (2006) Lipocalin 2-deficient mice exhibit increased sensitivity to Escherichia coli infection but not to ischemia-reperfusion injury. Proc Natl Acad Sci U S A 103:1834–1839
Nairz M, Dichtl S, Schroll A, Haschka D, Tymoszuk P, Theurl I, Weiss G (2018) Iron and innate antimicrobial immunity—depriving the pathogen, defending the host. J Trace Elem Med Biol 48:118–133
Stefanova D, Raychev A, Deville J, Humphries R, Campeau S, Ruchala P, Nemeth E, Ganz T, Bulut Y (2018) Hepcidin protects against lethal Escherichia coli sepsis in mice inoculated with isolates from septic patients. Infect Immun 86:e00253–e00218
Liu D, Gan Z-S, Ma W, Xiong HT, Li YQ, Wang YZ, du HH (2017) Synthetic porcine hepcidin exhibits different roles in Escherichia coli and Salmonella infections. Antimicrob Agents Chemother 61. https://doi.org/10.1128/AAC.02638-16
Michels K, Nemeth E, Ganz T, Mehrad B (2015) Hepcidin and host defense against infectious diseases. PLoS Pathog 11:e1004998. https://doi.org/10.1371/journal.ppat.1004998
Krasnodembskaya A, Song Y, Fang X, Gupta N, Serikov V, Lee JW, Matthay MA (2010) Antibacterial effect of human mesenchymal stem cells is mediated in part from secretion of the antimicrobial peptide LL-37. Stem Cells 28:2229–2238
Johnson V, Webb T, Dow S (2013) Activated mesenchymal stem cells amplify antibiotic activity against chronic Staphylococcus aureus infection (P5056). J Immunol 190:180.11
Johnson V, Webb T, Norman A, Coy J, Kurihara J, Regan D, Dow S (2017) Activated mesenchymal stem cells interact with antibiotics and host innate immune responses to control chronic bacterial infections. Sci Rep 7:9575
Josse J, Velard F, Mechiche Alami S, Brun V, Guillaume C, Kerdjoudj H, Lamkhioued B, Gangloff SC (2014) Increased internalization of Staphylococcus aureus and cytokine expression in human Wharton’s jelly mesenchymal stem cells. Biomed Mater Eng 24:27–35
Guerra AD, Rose WE, Hematti P, Kao WJ (2017) Minocycline modulates NFκB phosphorylation and enhances antimicrobial activity against Staphylococcus aureus in mesenchymal stromal/stem cells. Stem Cell Res Ther 8:171
Seebach E, Holschbach J, Buchta N, Bitsch RG, Kleinschmidt K, Richter W (2015) Mesenchymal stromal cell implantation for stimulation of long bone healing aggravates Staphylococcus aureus induced osteomyelitis. Acta Biomater 21:165–177
Ward CL, Sanchez CJ, Pollot BE et al (2015) Soluble factors from biofilms of wound pathogens modulate human bone marrow-derived stromal cell differentiation, migration, angiogenesis, and cytokine secretion. BMC Microbiol 15:75
Mot YY, Othman I, Sharifah SH (2017) Synergistic antibacterial effect of co-administering adipose-derived mesenchymal stromal cells and Ophiophagus hannah l-amino acid oxidase in a mouse model of methicillin-resistant Staphylococcus aureus-infected wounds. Stem Cell Res Ther 8:5
Hou M, Zhang N, Yang J, Meng X, Yang R, Li J, Sun T (2013) Antimicrobial peptide LL-37 and IDR-1 ameliorate MRSA pneumonia in vivo. Cell Physiol Biochem 32:614–623
Liu Z, Yuan X, Liu M et al (2018) Antimicrobial peptide combined with BMP2 modified mesenchymal stem cells promotes calvarial repair in mouse inflammatory calvarial osteolytic model. Mol Ther 26:199–207
Lee P-H, Chen M-Y, Lai Y-L et al (2017) Human beta-defensin-2 and -3 mitigate the negative effects of bacterial contamination on bone healing in rat calvarial defect. Tissue Eng A. https://doi.org/10.1089/ten.tea.2017.0219
Mei SHJ, Haitsma JJ, Dos Santos CC, Deng Y, Lai PFH, Slutsky AS, Liles WC, Stewart DJ (2010) Mesenchymal stem cells reduce inflammation while enhancing bacterial clearance and improving survival in sepsis. Am J Respir Crit Care Med 182:1047–1057
Alcayaga-Miranda F, Cuenca J, Martin A, Contreras L, Figueroa FE, Khoury M (2015) Combination therapy of menstrual derived mesenchymal stem cells and antibiotics ameliorates survival in sepsis. Stem Cell Res Ther 6:199
Asano K, Yoshimura S, Nakane A (2015) Adipose tissue-derived mesenchymal stem cells attenuate staphylococcal enterotoxin A-induced toxic shock. Infect Immun 83:3490–3496
Cóndor JM, Rodrigues CE, de Sousa Moreira R, Canale D, Volpini RA, Shimizu MHM, Camara NOS, Noronha IL, Andrade L (2016) Treatment with human Wharton’s jelly-derived mesenchymal stem cells attenuates sepsis-induced kidney injury, liver injury, and endothelial dysfunction. Stem Cells Transl Med 5:1048–1057
Chao Y-H, Wu H-P, Wu K-H, Tsai YG, Peng CT, Lin KC, Chao WR, Lee MS, Fu YC (2014) An increase in CD3+CD4+CD25+ regulatory T cells after administration of umbilical cord-derived mesenchymal stem cells during sepsis. PLoS One 9:e110338. https://doi.org/10.1371/journal.pone.0110338
Pedrazza L, Lunardelli A, Luft C, Cruz CU, de Mesquita FC, Bitencourt S, Nunes FB, de Oliveira JR (2014) Mesenchymal stem cells decrease splenocytes apoptosis in a sepsis experimental model. Inflamm Res 63:719–728
Pedrazza L, Pereira TCB, Abujamra AL, Nunes FB, Bogo MR, de Oliveira JR (2017) Mesenchymal stem cells cannot affect mRNA expression of toll-like receptors in different tissues during sepsis. Inflamm Res 66:547–551
Phinney DG, Pittenger MF (2017) Concise review: MSC-derived exosomes for cell-free therapy. Stem Cells 35:851–858
van der Pol L, Stork M, van der Ley P (2015) Outer membrane vesicles as platform vaccine technology. Biotechnol J 10:1689–1706
Prattichizzo F, Micolucci L, Cricca M, de Carolis S, Mensà E, Ceriello A, Procopio AD, Bonafè M, Olivieri F (2017) Exosome-based immunomodulation during aging: a nano-perspective on inflamm-aging. Mech Ageing Dev 168:44–53
Li T, Yan Y, Wang B, Qian H, Zhang X, Shen L, Wang M, Zhou Y, Zhu W, Li W, Xu W (2013) Exosomes derived from human umbilical cord mesenchymal stem cells alleviate liver fibrosis. Stem Cells Dev 22:845–854
Lai RC, Arslan F, Lee MM, Sze NSK, Choo A, Chen TS, Salto-Tellez M, Timmers L, Lee CN, el Oakley RM, Pasterkamp G, de Kleijn DPV, Lim SK (2010) Exosome secreted by MSC reduces myocardial ischemia/reperfusion injury. Stem Cell Res 4:214–222
Arslan F, Lai RC, Smeets MB, Akeroyd L, Choo A, Aguor ENE, Timmers L, van Rijen HV, Doevendans PA, Pasterkamp G, Lim SK, de Kleijn DP (2013) Mesenchymal stem cell-derived exosomes increase ATP levels, decrease oxidative stress and activate PI3K/Akt pathway to enhance myocardial viability and prevent adverse remodeling after myocardial ischemia/reperfusion injury. Stem Cell Res 10:301–312
Zhou Y, Xu H, Xu W, Wang B, Wu H, Tao Y, Zhang B, Wang M, Mao F, Yan Y, Gao S, Gu H, Zhu W, Qian H (2013) Exosomes released by human umbilical cord mesenchymal stem cells protect against cisplatin-induced renal oxidative stress and apoptosis in vivo and in vitro. Stem Cell Res Ther 4:34
Reis LA, Borges FT, Simões MJ, Borges AA, Sinigaglia-Coimbra R, Schor N (2012) Bone marrow-derived mesenchymal stem cells repaired but did not prevent gentamicin-induced acute kidney injury through paracrine effects in rats. PLoS One 7:e44092. https://doi.org/10.1371/journal.pone.0044092
Gatti S, Bruno S, Deregibus MC, Sordi A, Cantaluppi V, Tetta C, Camussi G (2011) Microvesicles derived from human adult mesenchymal stem cells protect against ischaemia-reperfusion-induced acute and chronic kidney injury. Nephrol Dial Transplant 26:1474–1483
Lee C, Mitsialis SA, Aslam M, Vitali SH, Vergadi E, Konstantinou G, Sdrimas K, Fernandez-Gonzalez A, Kourembanas S (2012) Exosomes mediate the cytoprotective action of mesenchymal stromal cells on hypoxia-induced pulmonary hypertension. Circulation 126:2601–2611
Akyurekli C, Le Y, Richardson RB et al (2015) A systematic review of preclinical studies on the therapeutic potential of mesenchymal stromal cell-derived microvesicles. Stem Cell Rev Reports 11:150–160
Crivelli B, Chlapanidas T, Perteghella S, Lucarelli E, Pascucci L, Brini AT, Ferrero I, Marazzi M, Pessina A, Torre ML, Italian Mesenchymal Stem Cell Group (GISM) (2017) Mesenchymal stem/stromal cell extracellular vesicles: from active principle to next generation drug delivery system. J Control Release 262:104–117
Mattar P, Bieback K (2015) Comparing the immunomodulatory properties of bone marrow, adipose tissue, and birth-associated tissue mesenchymal stromal cells. Front Immunol 6:560
Gao F, Chiu SM, Motan DAL, Zhang Z, Chen L, Ji HL, Tse HF, Fu QL, Lian Q (2016) Mesenchymal stem cells and immunomodulation: current status and future prospects. Cell Death Dis 7:e2062. https://doi.org/10.1038/cddis.2015.327
Galderisi U, Giordano A (2014) The gap between the physiological and therapeutic roles of mesenchymal stem cells. Med Res Rev 34:1100–1126
Hass R, Kasper C, Böhm S, Jacobs R (2011) Different populations and sources of human mesenchymal stem cells (MSC): a comparison of adult and neonatal tissue-derived MSC. Cell Commun Signal 9:12
Wang Q, Yang Q, Wang Z, Tong H, Ma L, Zhang Y, Shan F, Meng Y, Yuan Z (2016) Comparative analysis of human mesenchymal stem cells from fetal-bone marrow, adipose tissue, and Warton’s jelly as sources of cell immunomodulatory therapy. Hum Vaccin Immunother 12:85–96
Arutyunyan I, Elchaninov A, Makarov A, Fatkhudinov T (2016) Umbilical cord as prospective source for mesenchymal stem cell-based therapy. Stem Cells Int 2016:1–17
Mahmood A, Lu D, Lu M, Chopp M (2003) Treatment of traumatic brain injury in adult rats with intravenous administration of human bone marrow stromal cells. Neurosurgery 53:697–703
Xiong C, Mao Y, Wu T, Kang N, Zhao M, di R, Li X, Ji X, Liu Y (2018) Optimized expression and characterization of a novel fully human bispecific single-chain diabody targeting vascular endothelial growth factor165 and programmed death-1 in Pichia pastoris and evaluation of antitumor activity in vivo. Int J Mol Sci 19:2900
Richter-Dahlfors A, Rhen M, Udekwu K (2012) Tissue microbiology provides a coherent picture of infection. Curr Opin Microbiol 15:15–22
Moon JS, Cheong NR, Yang SY, Kim IS, Chung HJ, Jeong YW, Park JC, Kim MS, Kim SH, Ko HM (2013) Lipopolysaccharide-induced indoleamine 2,3-dioxygenase expression in the periodontal ligament. J Periodontal Res 48:733–739
Yang Y, Choi H, Seon M, et al (2016) LL-37 stimulates the functions of adipose- derived stromal / stem cells via early growth response 1 and the MAPK pathway. Stem Cell Res Ther 1–12. doi: https://doi.org/10.1186/s13287-016-0313-4
Oliveira-Bravo M, Sangiorgi BB, dos Santos Schiavinato JL et al (2016) LL-37 boosts immunosuppressive function of placenta-derived mesenchymal stromal cells. Stem Cell Res Ther 7:189
Lee EY, Lee MW, Wong GCL (2018) Modulation of toll-like receptor signaling by antimicrobial peptides. Semin Cell Dev Biol 2:12
Lombardo E (2015) Mesenchymal stem cells as a therapeutic tool to treat sepsis. World J Stem Cells 7:368–379
Li Z, Liao W, Cui X, Zhao Q, Liu M, Chen YH, Liu TS, Liu NL, Wang F, Yi Y, Shao NS (2011) Intravenous transplantation of allogeneic bone marrow mesenchymal stem cells and its directional migration to the necrotic femoral head. Int J Med Sci 8:74–83
Weil BR, Herrmann JL, Abarbanell AM, Manukyan MC, Poynter JA, Meldrum DR (2011) Intravenous infusion of mesenchymal stem cells is associated with improved myocardial function during endotoxemia. Shock 36:235–241
Hauger O, Frost EE, van Heeswijk R, Deminière C, Xue R, Delmas Y, Combe C, Moonen CTW, Grenier N, Bulte JWM (2006) MR evaluation of the glomerular homing of magnetically labeled mesenchymal stem cells in a rat model of nephropathy. Radiology 238:200–210
Ortiz LA, Dutreil M, Fattman C et al (2007) Interleukin 1 receptor antagonist mediates the antiinflammatory and antifibrotic effect of mesenchymal stem cells during lung injury. Proc Natl Acad Sci U S A 104:11002–11007
Acknowledgments
We thank Dr. Neil Slaven for checking the manuscript and linguistic revision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marrazzo, P., Crupi, A.N., Alviano, F. et al. Exploring the roles of MSCs in infections: focus on bacterial diseases. J Mol Med 97, 437–450 (2019). https://doi.org/10.1007/s00109-019-01752-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-019-01752-6