Abstract
MicroRNAs are single-stranded small non-coding RNA molecules which regulate mammalian cell growth, differentiation, and apoptosis by altering the expression of other genes and play a role in tumor genesis and progression. MiR-106a is upregulated in several types of malignancies and provides a pro-tumorigenic effect. However, its role in glioma is largely unknown. Our findings demonstrate that the low expression of miR-106a in human glioma specimens is significantly correlated with high levels of E2F1 protein and high-grade glioma. Here, we present the first evidence that miR-106a provides a tumor-suppressive effect via suppressing proliferation of and inducing apoptosis in human glioma cells. We further show that E2F1 is a direct functional target of miR-106a, suggesting that the effect of miR-106a on the glioma suppressive effect may result from inhibition of E2F1 via post-transcriptional regulation. In addition, our results reveal that miR-106a can increase p53 expression via E2F1 inhibition, whereas the effect of miR-106a on the proliferation of glioma cells is independent of p53 status. Further investigations will focus on the therapeutic use of miR-106a-mediated antitumor effects in glioma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gliomas are the most common primary brain tumors in adults [1]. High-grade gliomas (WHO grades III and IV) are notoriously difficult to treat and recurrences arise virtually in every case [2]. Despite new biological insights and advances in therapy, the prognosis of patients with gliomas still remains poor in the last four decades [3, 4]. The high recurrence rate and mortality of malignant gliomas motivate us to investigate molecular mechanisms underlying malignant tumor progression and the resistance to treatment, with the aim of developing biologically based and more effective clinical therapies.
MicroRNAs (miRNAs) are a class of endogenous small non-coding RNA molecules that are now believed to regulate the expression of up to 30% of human genes, either by inhibiting mRNA translation or by inducing mRNA degradation [5]. MiRNAs are aberrantly expressed in a wide variety of human cancers and thought to play important roles in tumorigenesis [6, 7]. Recent studies revealed that miR-106a was upregulated in gastrointestinal tract tumors and considered to exert pro-tumorigenic effects [8–10]. However, little is understood with respect to potential regulatory mechanisms of miR-106a in gliomas.
E2F1, a transcription factor, controls cell cycle progression by transactivating a variety of genes involved in chromosomal DNA replication [11]. E2F1 is especially distinct from other E2F family members due to its bimodal effects on cell proliferation and apoptosis. These effects depend on the cell type and the microenvironmental stimulation [12]. Deregulation of E2F1 has been described in various tumor types and correlated with poor patient survival, such as that in malignant gliomas [13–15]. Our aim was to explore the potential biological functions of miR-106a in glioma with a view to its future clinical therapeutic use.
Materials and methods
Human tissue samples
Surgically excised tumor specimens from 14 patients with WHO grade I-IV glioma and normal adjacent tissues (NATs) from three glioma patients were collected in the Department of Neurosurgery, The First Affiliated Hospital of Harbin Medical University, China. Cases included two patients with grade I, four with grade II, four with grade III, and four with grade IV glioma. Histological grading was performed on the basis of the WHO criteria. Collected tissues were immediately snap-frozen in liquid nitrogen and stored at −80°C. This research study was approved by the Institutional Review Board of Harbin Medical University, and the subjects gave informed consent.
Cell culture
The human glioma cell lines T98G, U373, and U87 as well as human embryonic kidney (HEK) 293T cells were obtained from the American Type Culture Collection (ATCC). The human glioma cell lines U251 and SHG44 were obtained from the Cell Bank of the Type Culture Collection of Chinese Academy of Sciences. All cell lines were maintained in Dulbecco's Modified Eagle Medium (Invitrogen, USA) supplemented with 10% fetal bovine serum (Invitrogen, USA).
RNA extraction and quantitative real-time PCR
Total RNA was isolated from cultured cells, human glioma specimens, or NATs using TRIzol® reagent (Invitrogen, USA) according to the manufacturer’s instructions. Quantitative real-time polymerase chain reaction (qRT-PCR) was performed in triplicate in ABI 7500HT fast real-time PCR System (Applied Biosystems) and normalized with U6 and glyceraldehyde 3-phosphate dehydrogenase (GAPDH) endogenous control. Total RNA from NATs was used as a control. MiR-106a levels were measured with the TaqMan microRNA assay kit, and endogenous mRNA levels of E2F1 were detected using SYBR Green PCR Master Mix kit in accordance with the manufacturer’s instructions (Applied Biosystems, USA). The real-time PCR primers for E2F1 and GAPDH were listed in Table 1.
Oligonucleotide synthesis and transfection
MiR-106a mimic, miR-106a inhibitor, E2F1-siRNA, p53-siRNA, and scrambled control oligonucleotides were purchased from GenePharma (Shanghai, China). miRNA and siRNA sequences were described in Table 1. MiRNA, siRNA oligonucleotides, or expression plasmid were transfected into cultured cells using Lipofectamine 2000 reagent (Invitrogen, USA) following manufacturer's instructions.
Construction of E2F1 3′ untranslated region reporter plasmid and E2F1 expression plasmid
The full-length E2F1-3′-UTR was amplified using the primers listed in Table 1 and cloned into the psiCHECK-2 vector (Promega, USA) at two restriction sites for XhoI and NotI. Mutations were introduced by site-directed mutagenesis into two putative binding sites in the 3′UTR of E2F1 gene for miR-106a using the TaKaRa MutanBEST Kit (Takara, China). Primers used for site-directed mutagenesis were listed in Table 1. To construct E2F1 expression plasmid, the full-length cDNA was first amplified using the primers listed in Table 1 and then cloned into the pcDNA3.1 vectors (Invitrogen, USA) at two restriction sites for BamHI and NotI.
Luciferase assays
HEK 293T cells were co-transfected in 24-well plates by Lipofectamine 2000 reagent (Invitrogen, USA) with 0.5 μg of reporter plasmid and miR-106a mimic or control miRNA at a final concentration of 50 nM. Luciferase assays were performed using the dual-Luciferase Reporter Assay system (Promega, USA) according to the manufacturer’s instructions. All experiments were repeated at least three times with duplicate samples.
Protein extraction and Western blot
Total proteins were extracted from human glioma cells and specimens with RIPA lysis buffer. Lysate was separated by 10% sodium dodecyl sulfate polyacrylamide gel electrophoresis, and the gel was blotted onto PVDF membrane (Millipore, USA). The membrane was blocked in 5% non-fat milk and then incubated with either mouse anti-human E2F1 (1:200, KH95, Santa Cruz, USA), mouse anti-human p53 (1:200, DO-1, Santa Cruz, USA), or mouse anti-human GAPDH antibody (1:1000, Sigma, USA). After washing, the membrane was incubated with the fluorescence-conjugated anti-mouse IgG (1:4000, Invitrogen, USA). The bound secondary antibody was quantified using the Odyssey v1.2 software (LI-COR, USA) by measuring the band intensity (area × optical density) for each group and normalized with GAPDH. The final results are expressed as fold changes by normalizing the data to control values.
Cell viability assays
Cultured cells were seeded on 96-well plates and were transfected as described above. On each of four consecutive days, 20 μl of dimethyl thiazolyl diphenyl tetrazolium (MTT; 0.5 mg/mL, Sigma, USA) was added to each well. The reaction was then stopped by lysing cells with 200 μl of dimethyl sulfoxide. Optical density measurements were obtained at a wavelength of 570 nm using spectrophotometric analysis (Tecan, Switzerland).
Cell cycle analysis
Cell cycle analysis was performed by flow cytometry (FCM; Becton Dickinson, USA). Transfected and control cells were fixed with 75% ethanol. Fixed cells were treated with 25 ug/ml of DNase-free RNase A (Sigma, USA) and stained with 50 ug/ml of propidium iodide (PI; Sigma, USA). Experiments were performed in triplicate.
Apoptosis assay
The apoptosis ratio was analyzed using Annexin V Apoptosis Detection Kit (BD Biosciences, USA) according to the manufacturer's instructions. Apoptotic cells were examined and quantified using by FCM. Tests were repeated in triplicate.
Immunohistochemistry
Paraffin-embedded sections of excised glioma specimens were immunostained for E2F1 protein. Staining was performed with the streptavidin–biotin peroxidase complex method according to the manufacturer’s recommendation (Dako, Denmark). Mouse anti-human E2F1 primary antibody (1:100; KH95, Santa Cruz, USA) was administered, followed by secondary goat anti-mouse IgG (Dako, Denmark). Negative controls were performed throughout the entire immunohistochemistry procedure. Only nuclear E2F1 staining was considered as positive. Slides were scored on the basis of the percentage of positive tumor cells. All of the immunostained sections were reviewed in the blinded fashion by two investigators.
Statistical analysis
Statistical analysis was performed with the SPSS13.0 software. Student’s t test or Chi-square analysis was applied, where appropriate. A probability of <0.05 (*) or <0.001 (**) was considered significant.
Results
MiR-106a expression in human glioma is reversely correlated with WHO grade
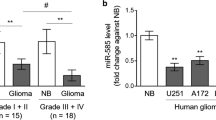
Although a marked downregulation of miR-106a was recently observed in human astrocytoma tissues [16], relatively little is understood with respect to the relevance of miR-106a to glioma tumorigenicity. Therefore, we determined miR-106a expression in specimens of human gliomas of different WHO grades (I-IV) and in malignant human glioma cell lines (T98G, U251, U87, U373, and SHG44) and compared it with that of NATs using TaqMan®-based stem-loop RT-PCR technology. Our results showed that the expression of miR-106a in both glioma specimens and cell lines was significantly lower than that in NATs (Fig. 1). Moreover, miR-106a expression was lower in grade III and grade IV glioma compared with grade I and grade II tumors (Fig. 1a). Therefore, our findings demonstrated that the miR-106a expression in human gliomas was reversely correlated with glioma grade.
A reverse correlation exists between miR-106a expression and glioma histological grade. qRT-PCR analysis expression of miR-106a in specimens of human gliomas of different grades (a) and glioma cell lines (b) as compared with that in NATs. U6 small RNA was used as a loading control. NATs indicate normal adjacent tissues, G glioma, **P < 0.001. Data were presented as mean ± SEM for three separate experiments performed in duplicate
Overexpression of miR-106a inhibits cell proliferation and induces apoptosis
To determine the effect of miR-106a on growth and proliferation of glioma cells, we overexpressed or knocked down miR-106a by transfection of miR-106a mimic or miR-106a inhibitory oligonucleotides into glioma cell lines. MMT assay results revealed that miR-106a mimic-transfected cells showed a significant decrease in cell viability in U87 or SHG44 cells as compared with scrambled control-transfected cells (Fig. 2a). At 48 h post-transfection, inhibition of growth in U87 or SHG44 cells transfected with miR-106a mimic was 38.87 ± 7.39% and 33.96 ± 6.29%, respectively, and growth inhibition appeared to reach a maximum. However, we did not observe a significant difference in the rate of growth inhibition between miR-106a inhibitor and scrambled control-transfected U87 or SHG44 cells, although a slightly increasing trend of cell survival rate was seen in SHG44 cells (Fig. 2a).
Overexpression of miR-106a inhibits cellular proliferation and induces apoptosis. a Cell viability was determined by MTT assay in U87 or SHG44 cells transfected with miR-106a mimic, miR-106a inhibitor, or scrambled control for the indicated hours. b Cell cycle analysis was performed by flow cytometry (FCM) in U87 or SHG44 cells 48 h after transfection of miR-106a mimic, miR-106a inhibitor, or scrambled control. c Graphical representation of the FCM analysis in (b). d Cell apoptosis was analyzed by FCM in U87 or SHG44 cells 48 h after transfection of miR-106a mimic, miR-106a inhibitor, or scrambled control. e Graphical representation of the FCM analysis in (d). Data were presented as mean ± SEM for three separate experiments performed in duplicate. *indicates P < 0.05; **P < 0.001
To further examine the potential mechanism underlying decreased cell viability in U87 or SHG44 cells, we used FCM to analyze the cell cycle. FCM analysis demonstrated that at 48 h post-transfection, miR-106a mimic-transfected cells showed an increase in G0/G1-phase cells and a decrease in S-phase compared with control-transfected cells (Fig. 2b, c). Our findings indicated overexpression of miR-106a induced cell cycle arrest in G0/G1 phase in U87 or SHG44 cells. Subsequently, we also determined the effect of miR-106a on apoptosis by Annexin V and PI double staining. MiR-106a mimic-transfected cells had a significant increase in Annexin V-positive apoptotic cells compared with scrambled control-transfected cells (Fig. 2d, e). In contrast, miR-106a inhibitor-transfected U87 or SHG44 cells did not show significant alterations in the cell cycle distribution and apoptosis, although a slightly decreasing trend of both G0/G1 phase cells and apoptotic cells was seen in SHG44 cells (P > 0.05; Fig. 2b–e). These results raise the possibility that there exists a threshold value for miR-106a inhibition. Thus, further inhibition of miR-106a at levels below the threshold could not have any impact on the proliferation of glioma cells [17].
E2F1 is a direct target of miR-106a
Based on the analysis of databases miRanda (http://www.cbio.mskcc.org/mirnaviewer), PicTar (http://www.pictar.bio.nyu.edu), and TargetScan (http://www.targetscan.org), we predicted that E2F1 may be a target gene for miR-106a (Fig. 3a). Thus, miR-106a is likely to function in regulating the E2F1 gene. To test this hypothesis, U87 or SHG44 cells were transfected with miR-106a mimic, inhibitor, or scrambled control, and E2F1 protein levels were evaluated at 48 h post-transfection. As expected, Western blotting analysis showed that miR-106a mimic profoundly decreased E2F1 protein levels in U87 or SHG44 cells (Fig. 3b, c). However, miR-106a inhibitor had no effect on E2F1 protein expression in U87 or SHG44 cells, although a slightly increasing trend of E2F1 protein expression was seen in SHG44 cells (Fig. 3b, c).
E2F1 is a direct target of miR-106a. a The potential interaction between miR-106a and two putative binding sites in the E2F1-3′-UTR was predicted by miRanda, PicTar, and TargetScan database analysis. The mutant sequences are equivalent to the wild-type ones except mutations at the 3′ end of target site underlined: Mut1 for the putative binding site nts 387–393, Mut2 for nts 980–986, and Mut1+Mut2 for both binding sites. b E2F1 protein expression was determined by Western blot in U87 or SHG44 cells 48 h after transfection of miR-106a mimic, miR-106a inhibitor, or scrambled control. GAPDH was used as a loading control. c Graphical representation of the Western blot analysis in (b). d Luciferase activities were analyzed in 293T cells 48 h after co-transfection of miR-106a mimic and either Mut1, Mut2, or Mut1+Mut2. Data were presented as mean ± SEM for three separate experiments performed in duplicate. *indicates P < 0.05; **P < 0.001
To assess whether there is a direct interaction between miR-106a and E2F1, we constructed the 3′-UTR region of E2F1 gene, which was predicted to interact with miR-106a. The database analysis results revealed that two putative binding sites for miR-106a were harbored in the 3′UTR of E2F1 gene and located at nts 387–393 and 980–986 of the E2F1-3′-UTR, respectively (Fig. 3a). Therefore, three mutated clones of binding sites were constructed, including Mut1 for nts 387–393, Mut2 for nts 980–986, and Mut1+Mut2 for both sites (Fig. 3a). The wild-type or mutant 3′UTR of E2F1 dual-Luciferase reporter plasmid was co-transfected with miR-106a mimic or scrambled control into 293T cells for 48 h, followed by measurement of luciferase activity in transfected cells. Our results showed that the reporter plasmid with wild-type 3′-UTR of E2F1 caused a significant decrease in luciferase activity in cells transfected with miR-106a mimic (Fig. 3d), while neither of Mut1, Mut2, nor Mut1+Mut2 reporter plasmid could produce any change in luciferase activity (Fig. 3d). Our findings showed that, when either of two binding sites in the 3′-UTR of the E2F1 gene was mutated, the regulation of E2F1 by miR-106a was completely eliminated. Taken together, these data confirmed that E2F1 is a direct target of miR-106a.
E2F1 is a functional target of miR-106a
We further assessed the effect of miR-106a on glioma cell growth by E2F1 induction. U87 or SHG44 cells were co-transfected with miR-106a mimic or scrambled control 24 h after transfection with E2F1 expression plasmid. Western blotting results demonstrated the upregulation of E2F1 protein levels was significantly prevented by miR-106a (Fig. 4a, b). Subsequently, the cell proliferation and the cell cycle were assessed in co-transfected U87 or SHG44 cells. Our results showed E2F1 induction can rescue the tumor-suppressive effects of miR-106a overexpression (Fig. 4c–e), indicating that E2F1 is a functional target of miR-106a. Therefore, the tumor-suppressive effects of miR-106a are regulated through the regulation of E2F1.
MiR-106a inhibits glioma cell growth by E2F1 inhibition. a E2F1 protein expression was determined by Western blot in U87 or SHG44 cells transfected with empty vector + scrambled control, E2F1 plasmid + scrambled control, or E2F1 plasmid + miR-106a mimic. b Graphical representation of the Western blot analysis in (a). c Cell viability was determined by MTT assay in U87 or SHG44 cells transfected with empty vector + scrambled control, empty vector + miR-106a mimic, or E2F1 plasmid + miR-106a mimic for the indicated hours. d Cell cycle analysis was performed by FCM in U87 or SHG44 cells transfected with empty vector + scrambled control, empty vector + miR-106a mimic, or E2F1 plasmid + miR-106a mimic. e Graphical representation of the FCM analysis in (d). Data were presented as mean ± SEM for three separate experiments performed in duplicate. *indicates P < 0.05; **P < 0.001
We also examined the protein levels and mRNA expression of E2F1 in human glioma specimens of different WHO grades by immunohistochemistry (Fig. 5), Western blot, and qRT-PCR. Grade III and grade IV gliomas showed a pronounced decrease in miR-106a levels compared with grade I and II gliomas (Fig. 1a). In contrast, a marked increase in the protein expression of E2F1 was observed in grade III and IV gliomas compared with grade I and II gliomas (Fig. 5a, b). Therefore, low expression of miR-106a in human glioma specimens was significantly correlated with high levels of E2F1 protein and high WHO grade. In addition, the levels of nuclear E2F1 protein were higher in glioma tissues than those in NATs, as determined by immunohistochemistry. However, E2F1 mRNA expression was unchanged in glioma tissues, U87, or SHG44 cells (Fig. 6c, d). These indicated that miR-106a controls E2F1 levels by translational suppression rather than by mRNA degradation.
Photomicrographs showing representative results of immunohistochemical analysis of E2F1 expression in specimens of human gliomas of different grades and NATs. a NAT specimen. b, c Grade II glioma specimens. d, e Grade IV glioma specimens. Original magnification ×400. Scale bars were 25 μm. f Graphical representation of the immunohistochemical analysis in (a–e). Data were presented as mean ± SEM. **indicates P < 0.001
E2F1 is regulated by miR-106a via translational suppression. a E2F1 protein expression was detected by Western blot in specimens of human gliomas of different grades and NATs. GAPDH was used as a loading control. b Graphical representation of the Western blot analysis in (a). c E2F1 mRNA expression was detected by qRT-PCR in specimens of human gliomas of different grades and NATs. GAPDH mRNA was used as a loading control. d miR-106a expression was detected by qRT-PCR in U87 or SHG44 cells transfected with miR-106a mimic or scrambled control. NATs indicate normal adjacent tissues, G glioma. Data were presented as mean ± SEM for three separate experiments performed in duplicate
MiR-106a regulates p53 expression via E2F1 inhibition
E2F1, which is present in most human tumors, may modulate p53 expression [12]. Therefore, to test whether p53 expression is regulated by miR-106a via E2F1 inhibition in glioma cells, we first assessed the expression of p53 and E2F1 proteins in five glioma cell lines, as shown in Fig. 1b. Western blotting analysis showed low basal levels of miR-106a expression in T98G or U87 cells correlated with increased expression of E2F1 and decreased expression of p53. In contrast, high levels of miR-106a in U251, U373, or SHG44 cells correlated with decreased expression of E2F1 and increased expression of p53 (Fig. 7a, b). Subsequently, all five glioma cell lines were transfected with miR-106a mimic, inhibitor, or scrambled control, and p53 protein levels were analyzed by Western blot. Our results showed that upregulation of miR-106a can increase p53 protein expression in all five glioma cell lines (Fig. 7c, d). We also examined the p53 expression in all five glioma cells following transfection of E2F1-siRNA. Western blotting results revealed that the cells transfected with E2F1-siRNA had a significant downregulation of E2F1 protein and upregulation of p53 protein, consistent with those transfected with miR-106a mimic (Fig. 7e, f). Therefore, it supported our hypothesis that miR-106a regulates p53 expression via the inhibition of E2F1.
miR-106a upregulates p53 expression via E2F1 inhibition. a p53 protein expression was determined by Western blot in five glioma cell lines. GAPDH was used as a loading control. b Graphical representation of the Western blot analysis in (a). c p53 protein expression was determined by Western blot in five glioma cell lines 48 h after transfection of miR-106a mimic, miR-106a inhibitor, or scrambled control. GAPDH was used as a loading control. d Graphical representation of the Western blot analysis in (c). e Protein levels of E2F1 and p53 were examined by Western blot in five glioma cell lines 48 h after transfection of miR-106a mimic, E2F1-siRNA, or scrambled control. GAPDH was used as a loading control. f Graphical representation of the Western blot analysis in (e). Data were presented as mean ± SEM for three separate experiments performed in duplicate. *Indicates P < 0.05; **P < 0.001
The inhibitory effect of miR-106a on glioma cell growth via inhibition of E2F1 is independent of p53 status
Intriguingly, U87 or SHG44 cells expressing wild-type p53 protein [18, 19] and T98G, U251, or U373 cells which express mutant p53 protein [18] had increased levels of wild-type or mutant p53 protein, respectively (Fig. 7c). Therefore, we further investigated the effect of miR-106a on glioma cell growth in T98G, U251, or U373 which express mutant p53 protein. Our results showed that overexpression of miR-106a could also significantly inhibit cell proliferation, block the cell cycle, and induce apoptosis in T98G, U251, or U373 cells, as evaluated by both MTT and FCM (Fig. 8). Meanwhile, miR106a inhibition provides a significant pro-tumorigenic effect in U373 cells with highest expression of miR106a (Figs. 1b and 8). The inhibition of cell growth by miR-106a in T98G, U251, or U373 cells was consistent with that in U87 or SHG44 cells expressing wild-type p53 protein (Fig. 2b–e). Therefore, our results showed miR-106a could decrease glioma cell proliferation independent of the functional status of the p53 protein.
The effect of miR-106a on glioma cells expressing mutant p53. a Cell viability was determined by MTT assay in T98, U251, or U373 cells transfected with miR-106a mimic, miR-106a inhibitor, or scrambled control for the indicated hours. b Cell cycle analysis was performed by FCM in T98G, U251, or U373 cells 48 h after transfection of miR-106a mimic, miR-106a inhibitor, or scrambled control. c Graphical representation of the FCM analysis in (b). d Cell apoptosis was analyzed by FCM in T98, U251, or U373 cells 48 h after transfection of miR-106a mimic, miR-106a inhibitor, or scrambled control. e Graphical representation of the FCM analysis in (d). Data were presented as mean ± SEM for three separate experiments performed in duplicate. *Indicates P < 0.05; **P < 0.001
To corroborate the above results, we performed co-transfection experiments in U87 or SHG44 cells expressing wild-type p53 protein again. p53-siRNA was first transfected in U87 or SHG44 cells, and Western blotting analysis indicated that p53 protein expression was significantly inhibited (Fig. 9a). Subsequently, U87 or SHG44 cells were co-transfected with miR-106a mimic or scrambled control 24 h after transfection with p53-siRNA. U87 or SHG44 cells co-transfected with p53-siRNA+miR-106a mimic had a significantly reduced proliferation rate (Fig. 9b) and a significant increase in the percentages of cells in the G0/G1 phase of the cell cycle (Fig. 9c, d) compared with those co-transfected with p53-siRNA+scrambled control. Thus, we revealed that the inhibitory effect of miR-106a on the proliferation of glioma cells was not dependent on the functional inactivation of the p53 protein. Taken together, our results suggested that the overexpression of miR-106a could increase p53 expression via inhibition of E2F1 in glioma cells, whereas the anti-proliferative effect of miR-106a on glioma cells was independent of the p53 status.
The inhibitory effect of miR-106a on the growth ability of glioma cells via the inhibition of E2F1 is independent of p53 status. a p53 protein expression was detected by Western blot in U87 or SHG44 cells transfected with p53-siRNA or negative control-siRNA. GAPDH was used as a loading control. b Cell viability was determined by MTT assay in U87 or SHG44 cells transfected with p53-siRNA+miR-106a mimic or p53-siRNA+scrambled control for the indicated hours. c Cell cycle analysis was performed by FCM in U87 or SHG44 cells transfected with p53-siRNA+miR-106a mimic or p53-siRNA+scrambled control. d Graphical representation of the FCM analysis in (c). Data were presented as mean ± SEM for three separate experiments performed in duplicate. *Indicates P < 0.05; **P < 0.001
Discussion
Most cellular processes are likely to be regulated by miRNAs, and an aberrant miRNA expression signature is probably one of the hallmarks of cancer [20]. Deregulation of miR-106a has been demonstrated in several tumors. However, the underlying functional mechanisms remain largely unknown. In this study, we revealed that miR-106a was downregulated in specimens of human gliomas of different grades and in glioma cell lines, and low levels of miR-106a in human glioma specimens were significantly correlated with high levels of E2F1 protein and high histological grade. Here, we presented the first evidence that overexpression of miR-106a could suppress proliferation of and induce apoptosis in glioma cells by E2F1 inhibition. In addition, our results suggested that miR-106a overexpression could increase p53 expression via inhibition of E2F1 in glioma cells, whereas the anti-proliferative effect of miR-106a on glioma cells was independent of p53 functional status.
Expression of miRNAs is regulated in a cell and tissue-type specific manner, and closely correlated with cell differentiation and development [20]. For instance, miR-181b expression level was increased in hepatocellular carcinoma [21], multiple myeloma [22], and colon tumors [23] but decreased in gliomas [16, 24] and chronic lymphocytic leukemia [25]. These observations probably suggest that miR-181b could provide a pro-tumorigenic or tumor-suppressive effect, depending on the cellular context. Therefore, different types of neoplasms may have individual miRNA profiles. In spite of the fact that miR-106a is upregulated in gastrointestinal tract tumors and considered to exert a pro-tumorigenic effect [8–10], our results clearly demonstrated miR-106a was downregulated in gliomas and induced apoptosis and anti-proliferation in glioma cells by E2F1 inhibition via post-transcriptional regulation. To delineate why miR-106a was downregulated in gliomas, we performed DNA sequence analysis of the chromosomal region Xq26.2 in glioma tissues that miR-106a is located at. Our results did not reveal any genetic change (data not shown). Thus, epigenetic changes such as miR-106a promoter methylation may be a potential mechanism of its downregulation [26, 27]. It remains still unclear why miR-106a is downregulated in gliomas but upregulated in other types of malignancies.
Aberrations in the cell cycle are essential steps in the carcinogenesis [28]. The transcription factor E2F1 is known to be able to regulate the cell cycle progression by coordinating a large group of genes involved in the G1/S-phase transition. Overexpressed E2F1 was shown to be pro-tumorigenic, predisposing cells to neoplastic transformation [29]. As p53 and E2F1 are pivotal regulators of cell proliferation and apoptosis [30], their expression and functional activities are tightly connected. E2F1 can have an impact on the expression and activity of p53 through regulation of numerous factors, for example ARF, p21, and ATM [12]. Our results showed that E2F1 may provide a pro-tumorigenic effect in the context of miR-106a regulation in glioma. High levels of E2F1 protein expression were not only associated with glioma cell proliferation but also associated with high histological grade in human gliomas. Our results suggested miR-106a could increase p53 expression via E2F1 inhibition and do so independent of the p53 functional status. It could potentially increase the spectrum of gliomas that might be therapeutically targeted with miR-106a-directed interventions.
Temozolomide (TMZ) has been adopted as the first-line treatment in patients with high-grade gliomas [31]. However, high levels of the O6-methylguanine-DNA methyltransferase (MGMT) activity in gliomas create a resistant phenotype by blunting the therapeutic effect of TMZ and may be an important determinant of treatment failure [32]. p53 induction attenuates MGMT expression and enhances the sensitivity of glioblastoma cells to TMZ [33, 34]. Since miR-106a can increase p53 expression, it is likely that the combinational application of miR-106a and TMZ could sensitize resistant glioma cells to TMZ.
In summary, our results suggest that miR-106a induced apoptosis and anti-proliferation in glioma cells. We further show that E2F1 is a direct functional target of miR-106a by post-transcriptional regulation. In addition, miR-106a can increase p53 expression via E2F1 inhibition, whereas the effect of miR-106a on proliferation is independent of p53 functional status. These data raise the possibility that miR-106a may serve as a potential therapeutic target for gliomas.
References
Jansen M, Yip S, Louis DN (2010) Molecular pathology in adult gliomas: diagnostic, prognostic, and predictive markers. Lancet Neurol 9:717–726. doi:10.1016/S1474-4422(10)70105-8
Wen PY, Kesari S (2008) Malignant gliomas in adults. N Engl J Med 359:492–507. doi:10.1056/NEJMra0708126
Hadjipanayis CG, Van Meir EG (2009) Tumor initiating cells in malignant gliomas: biology and implications for therapy. J Mol Med 87:363–374. doi:10.1007/s00109-009-0440-9
Purow B, Schiff D (2009) Advances in the genetics of glioblastoma: are we reaching critical mass? Nat Rev Neurol 5:419–426. doi:10.1038/nrneurol.2009.96
Gu S, Jin L, Zhang F, Sarnow P, Kay MA (2009) Biological basis for restriction of microRNA targets to the 3′ untranslated region in mammalian mRNAs. Nat Struct Mol Biol 16:144–150. doi:10.1038/nsmb.1552
Suzuki HI, Miyazono K (2010) Dynamics of microRNA biogenesis: crosstalk between p53 network and microRNA processing pathway. J Mol Med 88:1085–1094. doi:10.1007/s00109-010-0650-1
Ryan BM, Robles AI, Harris CC (2010) Genetic variation in microRNA networks: the implications for cancer research. Nat Rev Cancer 10:389–402. doi:10.1038/nrc2867
Volinia S, Calin GA, Liu CG, Ambs S, Cimmino A, Petrocca F, Visone R, Iorio M, Roldo C, Ferracin M et al (2006) A microRNA expression signature of human solid tumors defines cancer gene targets. Proc Natl Acad Sci USA 103:2257–2261. doi:10.1073/pnas.0510565103
Schetter AJ, Leung SY, Sohn JJ, Zanetti KA, Bowman ED, Yanaihara N, Yuen ST, Chan TL, Kwong DL, Au GK et al (2008) MicroRNA expression profiles associated with prognosis and therapeutic outcome in colon adenocarcinoma. JAMA 299:425–436. doi:10.1001/jama.299.4.425
Zhou H, Guo JM, Lou YR, Zhang XJ, Zhong FD, Jiang Z, Cheng J, Xiao BX (2010) Detection of circulating tumor cells in peripheral blood from patients with gastric cancer using microRNA as a marker. J Mol Med 88:709–717. doi::10.1007/s00109-010-0617-2
Polager S, Ginsberg D (2008) E2F—at the crossroads of life and death. Trends Cell Biol 18:528–535. doi:10.1016/j.tcb.2008.08.003
Polager S, Ginsberg D (2009) p53 and E2f: partners in life and death. Nat Rev Cancer 9:738–748. doi:10.1038/nrc2718
Alonso MM, Fueyo J, Shay JW, Aldape KD, Jiang H, Lee OH, Johnson DG, Xu J, Kondo Y, Kanzawa T et al (2005) Expression of transcription factor E2F1 and telomerase in glioblastomas: mechanistic linkage and prognostic significance. J Natl Cancer Inst 97:1589–1600. doi:10.1093/jnci/dji340
Alla V, Engelmann D, Niemetz A, Pahnke J, Schmidt A, Kunz M, Emmrich S, Steder M, Koczan D, Putzer BM (2010) E2F1 in melanoma progression and metastasis. J Natl Cancer Inst 102:127–133. doi:10.1093/jnci/djp458
Lee JS, Leem SH, Lee SY, Kim SC, Park ES, Kim SB, Kim SK, Kim YJ, Kim WJ, Chu IS (2010) Expression signature of E2F1 and its associated genes predict superficial to invasive progression of bladder tumors. J Clin Oncol 28:2660–2667. doi:10.1200/JCO.2009.25.0977
Zhi F, Chen X, Wang S, Xia X, Shi Y, Guan W, Shao N, Qu H, Yang C, Zhang Y, Wang Q et al (2010) The use of hsa-miR-21, hsa-miR-181b and hsa-miR-106a as prognostic indicators of astrocytoma. Eur J Cancer 46:1640–1649. doi:10.1016/j.ejca.2010.02.003
Keck K, Volper EM, Spengler RM, Long DD, Chan CY, Ding Y, McCaffrey AP (2009) Rational design leads to more potent RNA interference against hepatitis B virus: factors effecting silencing efficiency. Mol Ther 17:538–547. doi:10.1038/mt.2008.273
Komata T, Kondo Y, Koga S, Ko SC, Chung LW, Kondo S (2000) Combination therapy of malignant glioma cells with 2-5A-antisense telomerase RNA and recombinant adenovirus p53. Gene Ther 7:2071–2079. doi:10.1038/sj.gt.3301327
Luan S, Sun L, Huang F (2010) MicroRNA-34a: a novel tumor suppressor in p53-mutant glioma cell line U251. Arch Med Res 41:67–74. doi:10.1016/j.arcmed.2010.02.007
Iorio MV, Croce CM (2009) MicroRNAs in cancer: small molecules with a huge impact. J Clin Oncol 27:5848–5856. doi:10.1200/JCO.2009.24.0317
Wang B, Hsu SH, Majumder S, Kutay H, Huang W, Jacob ST, Ghoshal K (2010) TGFbeta-mediated upregulation of hepatic miR-181b promotes hepatocarcinogenesis by targeting TIMP3. Oncogene 29:1787–1797. doi:10.1038/onc.2009.468
Pichiorri F, Suh SS, Ladetto M, Kuehl M, Palumbo T, Drandi D, Taccioli C, Zanesi N, Alder H, Hagan JP et al (2008) MicroRNAs regulate critical genes associated with multiple myeloma pathogenesis. Proc Natl Acad Sci USA 105:12885–12890. doi:10.1073/pnas.0806202105
Nakajima G, Hayashi K, Xi Y, Kudo K, Uchida K, Takasaki K, Yamamoto M, Ju J (2006) Non-coding microRNAs hsa-let-7g and hsa-miR-181b are associated with chemoresponse to S-1 in colon cancer. CANCER GENOMICS PROTEOMICS 3:317–324
Shi L, Cheng Z, Zhang J, Li R, Zhao P, Fu Z, You Y (2008) hsa-mir-181a and hsa-mir-181b function as tumor suppressors in human glioma cells. Brain Res 1236:185–193. doi:10.1016/j.brainres.2008.07.085
Pekarsky Y, Santanam U, Cimmino A, Palamarchuk A, Efanov A, Maximov V, Volinia S, Alder H, Liu CG, Rassenti L et al (2006) Tcl1 expression in chronic lymphocytic leukemia is regulated by miR-29 and miR-181. Cancer Res 66:11590–11593. doi:10.1158/0008-5472.CAN-06-3613
Pavicic W, Perkio E, Kaur S, Peltomaki P (2011) Altered methylation at microRNA-associated CPG islands in hereditary and sporadic carcinomas: MS-MLPAa-based approach. Mol Med
Gao XN, Lin J, Li YH, Gao L, Wang XR, Wang W et al (2011) MicroRNA-193a represses c-kit expression and functions as a methylation-silenced tumor suppressor in acute myeloid leukemia. Oncogene
Malumbres M, Barbacid M (2001) To cycle or not to cycle: a critical decision in cancer. Nat Rev Cancer 1:222–231. doi:10.1038/35106065
Pierce AM, Schneider-Broussard R, Gimenez-Conti IB, Russell JL, Conti CJ, Johnson DG (1999) E2F1 has both oncogenic and tumor-suppressive properties in a transgenic model. Mol Cell Biol 19:6408–6414
Vilborg A, Wilhelm MT, Wiman KG (2010) Regulation of tumor suppressor p53 at the RNA level. J Mol Med 88:645–652. doi:10.1007/s00109-010-0609-2
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996. doi:10.1056/NEJMoa043330
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani L et al (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352:997–1003. doi:10.1056/NEJMoa043331
Harris LC, Remack JS, Houghton PJ, Brent TP (1996) Wild-type p53 suppresses transcription of the human O6-methylguanine-DNA methyltransferase gene. Cancer Res 56:2029–2032
Natsume A, Ishii D, Wakabayashi T, Tsuno T, Hatano H, Mizuno M, Yoshida J (2005) IFN-beta down-regulates the expression of DNA repair gene MGMT and sensitizes resistant glioma cells to temozolomide. Cancer Res 65:7573–7579. doi:10.1158/0008-5472.CAN-05-0036
Acknowledgments
This study was supported by Special Prophase Project of National Basic Research Program of China (2009cb526404 to ZS) and National Natural Science Foundations of China (30772239 and 30973078 to ZS).
Disclosure statement
The authors declare no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guang Yang, Ruyou Zhang, and Xiaofeng Chen contributed equally to this work.
Rights and permissions
About this article
Cite this article
Yang, G., Zhang, R., Chen, X. et al. MiR-106a inhibits glioma cell growth by targeting E2F1 independent of p53 status. J Mol Med 89, 1037–1050 (2011). https://doi.org/10.1007/s00109-011-0775-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-011-0775-x