Abstract
Purpose
To evaluate the feasibility of a new protocol, Chest Abdominal-Focused Assessment Sonography for Trauma (CA-FAST), during the primary survey and to estimate its diagnostic accuracy when compared with thoracoabdominal computed tomography (CT) scan.
Methods
A prospective accuracy study was performed from November 2012 to November 2013 at the Emergency Department. Only adult trauma patients who underwent a CA-FAST examination prior to a thoracoabdominal CT scan were enrolled. In addition to standard patterns detected by Extended-FAST (E-FAST) such as pneumothorax (PTX), hemothorax (HTX), pericardial and intraabdominal effusion, CA-FAST protocol also included the research of lung contusions (LCs).
Results
Six hundred and one patients were enrolled. The mean time for protocol execution was 7 ± 3 min. Chest ultrasonography showed the following results (all p < 0.001): LCs sensitivity 59 %, specificity 98 %, positive predictive value (PPV) 92 %, negative predictive value (NPV) 86 %, accuracy 87 %; PTX sensitivity 84 %, specificity 98 %, PPV 93 %, NPV 95 %, accuracy 95 %; HTX sensitivity 82 %, specificity 97 %, PPV 87 %, NPV 95 %, accuracy 94 %. The standard 4-views FAST examination showed a diagnostic accuracy of 91 % with a sensitivity of 75 %, specificity of 96 %, PPV of 81 % and NPV of 94 %.
Conclusion
According to our results CA-FAST protocol proved to be a rapid bedside method, with good accuracy and high NPV in detection of ultrasonographic patterns suggestive of serious injury in trauma patients; moreover, the additional research of LCs did not cause a delay in the diagnosis. Ultrasonography should be used as initial investigation during the primary survey, sending to further diagnostic studies (CT scan) only those patients not clearly classified.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Trauma is the leading cause of death in the developed world in subjects between the ages of 5 and 44 and generates a number of disabling outcomes [1, 2].
In the Emergency Department (ED) trauma patients can rapidly become hemodynamically unstable and need a rapid evaluation (“golden hour”) to identify and treat potential sources of bleeding or other severe injuries in order to reduce complications, length of stay, and overall cost of hospitalization.
Computed tomography (CT) scanning is widely accepted as the investigation of choice in trauma injury, however it might not be appropriate in hemodynamically unstable patients as it is expensive, exposes patients to radiation and usually requires a bolus of intravenous contrast material.
Since 70 s the ultrasonographic evaluation [3–5] has gradually acquired an important role in the rapid evaluation of trauma patients and, as suggested by the advanced trauma life support (ATLS) [2], it is currently performed after the primary survey.
Ultrasonography (US) is a useful initial imaging modality: It is rapid, repeatable and a noninvasive bedside method. In addition it can be performed simultaneously with other resuscitative cares, providing vital information without the time delay caused by the execution and interpretation of radiographs or CT scan [6]. In the literature, Focused Assessment with Sonography for Trauma (FAST) showed an accuracy of 92–97 % [7, 8] in recognizing intraperitoneal and intrapericardial bleeding in unselected trauma patients, and it is nearly 100 % sensitive in hypotensive patients who need an emergency laparotomy and in patients with penetrating trauma and suspicion of cardiac injury [9–12].
A later proposal with the aim of detecting pneumothorax (PNX) and hemotorax (HTX) in addition to intraperitoneal and intrapericardial bleeding became know as Extended-FAST (E-FAST) examination [13–18]. A large number of studies showed that bedside chest US is at least equivalent, if not more accurate than chest radiography (X-ray) for identifying HTX or PTX in trauma patients [13, 14, 19, 20]. Lung contusions (LCs) are a frequent clinical entity in blunt chest trauma and are associated with a 10–25 % mortality rate [21]. Despite its relatively high incidence, it is difficult to identify LCs in the ED as traditional radiology will underestimate its prevalence [22], needing to rely on a more advanced method such as CT. However, some studies have shown that chest US can accurately detect LCs with good accuracy in trauma victims [17, 23, 24].
For this reason we developed a new protocol (CA-FAST, Chest Abdominal FAST) that integrates the detection of LCs in the E-FAST examination which can be performed during the primary survey. The aim of this study was to evaluate the feasibility and the diagnostic performance of CA-FAST examination when compared to the gold standard, thoracoabdominal CT.
Methods
Study design and setting
A prospective accuracy study was performed at the Emergency Department (ED) of an urban academic level I trauma center with an annual census of 120,000 visits. The study, which is consistent with the principles of the Declaration of Helsinki on clinical research involving human subjects, was approved by an Institutional Review Board.
Selection of participants
Consecutive adult trauma patients presenting to the ED from November 2012 to November 2013 that underwent a thoracoabdominal CT scan were enrolled if a CA-FAST examination was previously performed; CT scan was either required or not at discretion of the emergency physician (EP), independently of patient’s participation to the study. Informed verbal consent for study participation was asked to each patient or to next of kin.
Interventions
A CA-FAST examination was performed at ED presentation during the primary survey and before CT scan by 12 physicians (7 senior EPs, 5 residents in emergency medicine). The minimum requirement for the sonographer was to have previously attended a 12-hour course in emergency chest-abdominal US and a hands-on training with execution of at least 25 FAST and 25 chest US scans, as suggested by ACEP guidelines [25]. The multi-probe machines used were the following: two MyLab 30 Gold and one MyLab alpha (Esaote, Genoa, Italy).
CA-FAST protocol consisted of a combined ultrasonographic evaluation of chest and abdomen in order to detect the presence of the following ultrasonographic patterns: PTX, HTX, LCs, pericardial and intraperitoneal effusion. The full examination consisted of 8 chest scans and 4 abdominal scans acquired with the patient in obligated supine position due to spinal boards and cervical collars.
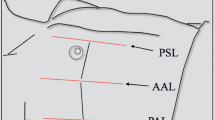
Chest US was performed by a 4- to 8-MHz linear probe or a 3.5- to 5-MHz curved array probe, and as suggested by the international evidence-based recommendation for point-of-care lung ultrasound [26], each hemithorax was divided into 4 areas: 2 anterior and 2 lateral. It was not possible to evaluate posterior chest areas due to the obligated supine position of patients.
A scan for each area (four scans per hemithorax) was obtained in order to detect the presence of specific ultrasound patterns: PTX, HTX and LCs, as described in the recommendations mentioned above [26], and in the literature [16, 17].
The abdominal US was performed by 5-MHz curved array probe using the standard 4-views FAST examination (perihepatic, perisplenic, pelvic and pericardial sub-xiphoid); FAST was considered positive if free fluid was identified in any location [3].
Methods and measurement
In order to compile a written report, the following information was obtained for each patient: personal data, time for completing the CA-FAST examination, ultrasonographic findings and their location. On the base of CT scan results, the Injury Severity Score (ISS) value was calculated.
Data collection and statistical analysis were done by the authors.
Outcomes
The diagnostic performance of the CA-FAST examination, in order to identify pathological patterns considered in the protocol, was assessed considering the CT scan as the gold standard: For chest evaluation due to obligated supine position of patients, we compared only anterior and lateral lung areas. CT scans were performed with AS128 (Siemens, Erlangen, Germany) using contrast medium if not contraindicated and were reviewed by expert radiologists not participating in the present study.
Analysis
Statistical analysis was performed using SPSS Package 21.0 software (SPSS Inc. Chicago, IL, USA). All continuous parameters are reported as means ± standard deviations, and frequency values are written as absolute values and percentages. Dichotomous variables and percentages were compared by Chi-square test. A two-tailed value of p < 0.05 was used to indicate statistical significance. Diagnostic performance of CA-FAST was evaluated by calculating sensitivity, specificity, positive predictive value, negative predictive value, and negative and positive likelihood ratios for each chest pathological findings (PTX, HTX, LCs) and for detection of free fluid in each FAST examination view.
Results
Characteristics of study subjects
Six hundred and one (467, 75 % male) consecutive patients with a mean age of 46 ± 20 years were enrolled in the study. The mean ISS of trauma victims was 16 ± 12; 281 patients had ISS > 15.
At chest CT 440 PTX, 170 HTX and 526 LCs were detected in the anterior and lateral areas; at abdomen CT free fluid was detected in 125 cases, 110 of whom intraperitoneal and 15 intrapericardial.
Main results
The mean time for CA-FAST protocol execution was 7 ± 3 min (4 ± 2 min for chest US and 3 ± 1 min for abdominal US).
Chest US examinations detected 411 PTX, 109 HTX and 293 LCs with an overall accuracy for each chest pathological findings of 95 % (95 % CI 91–97), 94 % (95 % CI 87–95) and 87 % (95 % CI 85–92), respectively. Table 1a reported the diagnostic performance of chest US.
FAST examinations detected free fluid in 116 cases showing an overall accuracy of 91 % (95 % CI 85–93). Considering each single standard view of the FAST examination, the accuracy of perihepatic, perisplenic, pericardial sub-xiphoid and pelvic views was 96, 96, 98 and 95 %, respectively. Table 1b reported the diagnostic performance of FAST examination.
Limitations
Our study was conducted in a single center. The obligated supine position of patients, due to spinal boards and cervical collars during the primary survey, did not allow for posterior chest US scans; therefore, we evaluated and compared only the anterior and lateral chest areas. Radiologists were not blinded to CA-FAST results.
Discussion
The average time for CA-FAST examination was similar to the traditional E-FAST examination. In the literature, execution time of E-FAST examination was 2.3 ± 2.9 min [27] for chest US and ≤5 min [28] for standard FAST [16, 17]. Therefore, the addition of four supplemental chest scans (2 per hemitorax) to the Extended-FAST scans and the research of LCs in each area considered in the CA-FAST protocol did not cause a significant delay.
Previous studies considered only chest US and did not analyze an integrated chest-abdominal US examination in detecting the three pathological findings (PTX, HTX and LCs) [16, 17]. Results of our study regarding chest US confirmed data already published in the literature, in particular regarding PTX and HTX: Our sensitivities (84 and 82 %) and specificities (98 and 97 %) were similar to previous studies [14–17, 27, 29]. Concerning LCs, CA-FAST showed a specificity of 98 % and a sensitivity of 59 % with a good NPV of 86 %. The sensitivity in our study is lower than values obtained in previous studies reported in the literature, in which, however, we found a large variability (sensitivity for LCs from 61 to 95 %) [17, 23] (Table 2). There are several explanations for this discrepancy. Patients with a different nature of thoracic lesions than that assessed, those with subcutaneous emphysema, or those who required mechanical ventilation were excluded from various former studies [16, 30]. In our study, according to the CT scan, we detected 136 cases in which LCs were associated with subcutaneous emphysema and/or PTX. It is been known for a long time that the first condition compromises the exploration of parietal pleura by thoracic US [16] while, in case of PTX, the presence of air in the pleural space acts as a specular reflector that covers all possible underlying artifacts, like B-Lines as in LCs [31].
In regard to the standard 4-views FAST examination, our study showed an overall accuracy comparable with previous studies [7, 8, 32–37] (Tables 1b, 3). Three of the standard 4-views (perihepatic, perisplenic and pelvic) showed good sensitivity and specificity and overlap between them. Only the pericardial sub-xiphoid view had a lower sensitivity (53 %) although with a high specificity. This result can be explained by the fact that echocardiography appears to be a more accurate imaging technique than CT scan in quantitative assessment of pericardial effusion [38, 39].
Overall, we demonstrated high accuracy of US detecting both thoracic and abdominal patterns, placing this technique as a valuable tool in the process of differential diagnosis.
The reliability of the data has been confirmed by the results of PPV and NPV values, which revealed that the majority of ultrasonographic findings were confirmed by CT.
Particularly, the result of the NPV (PNX 95 %, LCs 86 %, HTX 95 %; FAST 4-views 94 %) is essential in emergency medicine, because it allows to exclude, with reasonable certainty, real-time diagnostic suspects, routing the patient to the most appropriate therapy.
In summary CA-FAST protocol, performed in the emergency setting, showed important advantages: It is a noninvasive, rapid, ionizing radiation-free and an easily repeatable method; in trauma patients it allows to accurately and immediately detect diagnostic information and ultrasonographic patterns of severe injury. Moreover, the addition of four chest scans and the research of LCs did not cause a delay in the diagnosis. In our work, we did not measure the learning curve, because the EPs who performed the US were already experienced operators.
As stated in literature [25, 40, 41], the learning curve of this method is relatively quick; therefore, US evaluation is easily applicable and feasible in emergency setting.
For all these reasons, CA-FAST protocol could represent an integrative tool of traditional CT scan in the management of trauma patients; it should be used as the initial investigation, during the primary survey, sending to further diagnostic studies only patients not clearly classified.
Abbreviations
- FAST:
-
Focused Assessment Sonography for Trauma
- CA-FAST:
-
Chest Abdominal-Focused Assessment Sonography for Trauma
- CT:
-
Computed tomography
- E-FAST:
-
Extended-FAST
- PTX:
-
Pneumothorax
- HTX:
-
Hemothorax
- LCs:
-
Lung contusions
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- ED:
-
Emergency Department
- ATLS:
-
Advanced trauma life support
- US:
-
Ultrasonography
- X-ray:
-
Radiography
- EP:
-
Emergency physician
- ISS:
-
Injury Severity Score
References
World Health Statistics. World Health Organization 1, 45-70. Geneva: WHO Press; 2014.
American College of Surgeons. Advanced trauma life support for doctors. 10th ed. Chicago: American College of Surgeons; 2012.
Scalea TM, Rodriguez A, Chiu WC, Brenneman FD, Fallon WF Jr, Kato K, et al. Focused Assessment with Sonography for Trauma (FAST): results from an international consensus conference. J Trauma. 1999;46(3):466–72.
Rozycki GS, Ochsner MG, Schmidt JA, Frankel HL, Davis TP, Wang D, et al. A prospective study of surgeon-performed ultrasound as the primary adjuvant modality for injured patient assessment. J Trauma. 1995;39(3):492–8.
Jehle D, Davis E, Evans T, Harchelroad F, Martin M, Zaiser K, et al. Emergency department sonography by emergency physicians. Am J Emerg Med. 1989;7(6):605–11.
Arrillaga A, Graham R, York JW, Miller RS. Increased efficiency and cost-effectiveness in the evaluation of the blunt abdominal trauma patient with the use of ultrasound. Am Surg. 1999;65(1):31–5.
Miller MT, Pasquale MD, Bromberg WJ, Wasser TE, Cox J. Not so FAST. J Trauma. 2003;54(1):52–9.
Tsui CL, Fung HT, Chung KL, Kam CW. Focused abdominal sonography for trauma in the emergency department for blunt abdominal trauma. Int J Emerg Med. 2008;1(3):183–7.
Rozycki GS, Ballard RB, Feliciano DV, Schmidt JA, Pennington SD. Surgeon-performed ultrasound for the assessment of truncal injuries: lessons learned from 1540 patients. Ann Surg. 1998;228(4):557–67.
Wherrett LJ, Boulanger BR, McLellan BA, Brenneman FD, Rizoli SB, Culhane J, et al. Hypotension after blunt abdominal trauma: the role of emergent abdominal sonography in surgical triage. J Trauma. 1996;41(5):815–20.
Rozycki GS, Feliciano DV, Ochsner MG, Knudson MM, Hoyt DB, Davis F, et al. The role of ultrasound in patients with possible penetrating cardiac wounds: a prospective multicenter study. J Trauma. 1999;46(4):543–51.
Plummer D, Brunette D, Asinger R, Ruiz E. Emergency department echocardiography improves outcome in penetrating cardiac injury. Ann Emerg Med. 1992;21(6):709–12.
Ianniello S, Di G, Sessa B, Miele V. First-line sonographic diagnosis of pneumothorax in major trauma: accuracy of e-FAST and comparison with multidetector computed tomography. Radiol Med. 2014;119(9):674–80.
Kirkpatrick AW, Sirois M, Laupland KB, Liu D, Rowan K, Ball CG, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the Extended Focused Assessment with Sonography for Trauma (EFAST). J Trauma. 2004;57(2):288–95.
Lichtenstein DA, Meziere G, Lascols N, Biderman P, Courret JP, Gepner A, et al. Ultrasound diagnosis of occult pneumothorax. Crit Care Med. 2005;33(6):1231–8.
Soldati G, Testa A, Sher S, Pignataro G, La SM, Silveri NG. Occult traumatic pneumothorax: diagnostic accuracy of lung ultrasonography in the emergency department. Chest. 2008;133(1):204–11.
Hyacinthe AC, Broux C, Francony G, Genty C, Bouzat P, Jacquot C, et al. Diagnostic accuracy of ultrasonography in the acute assessment of common thoracic lesions after trauma. Chest. 2012;141(5):1177–83.
Montoya J, Stawicki SP, Evans DC, Bahner DP, Sparks S, Sharpe RP, Cipolla J. From FAST to E-FAST: an overview of the evolution of ultrasound-based traumatic injury assessment. Eur J Trauma Emerg Surg. 2015. [Epub ahead of print].
Ma OJ, Mateer JR. Trauma ultrasound examination versus chest radiography in the detection of hemothorax. Ann Emerg Med. 1997;29(3):312–5.
Sisley AC, Rozycki GS, Ballard RB, Namias N, Salomone JP, Feliciano DV. Rapid detection of traumatic effusion using surgeon-performed ultrasonography. J Trauma. 1998;44(2):291–6.
Hoff SJ, Shotts SD, Eddy VA, Morris JA Jr. Outcome of isolated pulmonary contusion in blunt trauma patients. Am Surg. 1994;60(2):138–42.
Guerrero-Lopez F, Vazquez-Mata G, Alcazar-Romero PP, Fernandez-Mondejar E, Aguayo-Hoyos E, Linde-Valverde CM. Evaluation of the utility of computed tomography in the initial assessment of the critical care patient with chest trauma. Crit Care Med. 2000;28(5):1370–5.
Soldati G, Testa A, Silva FR, Carbone L, Portale G, Silveri NG. Chest ultrasonography in lung contusion. Chest. 2006;130(2):533–8.
Stone MB, Secko MA. Bedside ultrasound diagnosis of pulmonary contusion. Pediatr Emerg Care. 2009;25(12):854–5.
American College of Emergency Physicians. Emergency ultrasound guidelines. Irvig: American College of Emergency Physicians; 2008.
Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38(4):577–91.
Zhang M, Liu ZH, Yang JX, Gan JX, Xu SW, You XD, et al. Rapid detection of pneumothorax by ultrasonography in patients with multiple trauma. Crit Care. 2006;10(4):R112.
Korner M, Krotz MM, Degenhart C, Pfeifer KJ, Reiser MF, Linsenmaier U. Current role of emergency US in patients with major trauma. Radiographics. 2008;28(1):225–42.
Nandipati KC1, Allamaneni S, Kakarla R, Wong A, Richards N, Satterfield J, Turner JW, Sung KJ. Extended focused assessment with sonography for trauma (EFAST) in the diagnosis of pneumothorax: experience at a community based level I trauma center. Injury. 2011;42(5):511-4. doi:10.1016/j.injury.2010.01.105.
Brooks A, Davies B, Smethhurst M, Connolly J. Emergency ultrasound in the acute assessment of haemothorax. Emerg Med J. 2004;21(1):44–6.
Soldati GSSCR. If you see the contusion, there is no pneumothorax. Am J Emerg Med. 2010;28(1):106–7.
Chiu WC, Cushing BM, Rodriguez A, Ho SM, Mirvis SE, Shanmuganathan K, et al. Abdominal injuries without hemoperitoneum: a potential limitation of focused abdominal sonography for trauma (FAST). J Trauma. 1997;42(4):617–23.
Shackford SR, Rogers FB, Osler TM, Trabulsy ME, Clauss DW, Vane DW. Focused abdominal sonogram for trauma: the learning curve of nonradiologist clinicians in detecting hemoperitoneum. J Trauma. 1999;46(4):553–62.
Boulanger BR, Rozycki GS, Rodriguez A. Sonographic assessment of traumatic injury. Future developments. Surg Clin N Am. 1999;79(6):1297–316.
Coley BD, Mutabagani KH, Martin LC, Zumberge N, Cooney DR, Caniano DA, et al. Focused abdominal sonography for trauma (FAST) in children with blunt abdominal trauma. J Trauma. 2000;48(5):902–6.
Dolich MO, McKenney MG, Varela JE, Compton RP, McKenney KL, Cohn SM. 2,576 ultrasounds for blunt abdominal trauma. J Trauma. 2001;50(1):108–12.
Gaarder C, Kroepelien CF, Loekke R, Hestnes M, Dormage JB, Naess PA. Ultrasound performed by radiologists-confirming the truth about FAST in trauma. J Trauma. 2009;67(2):323–7.
Labovitz AJ. Focused cardiac ultrasound in the emergent setting: a consensus statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr. 2010;23(12):30–1225.
Leibowitz D, Perlman G, Planer D, Gilon D, Berman P, Bogot N. Quantification of pericardial effusions by echocardiography and computed tomography. Am J Cardiol. 2011;107(2):331–5.
Carrié C, Biais M, Lafitte S, Grenier N, Revel P, Janvier G. Goal-directed ultrasound in emergency medicine: evaluation of a specific training program using an ultrasonic stethoscope. Eur J Emerg Med. 2015;22(6):419–25.
Ma OJ, Gaddis G, Norvell JG, Subramanian S. How fast is the focused assessment with sonography for trauma examination learning curve ? Emerg Med Australas. 2008;20:32–7.
Blaivas M, Lyon M, Duggal S. A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad Emerg Med. 2005;12(9):844–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Maurizio Zanobetti, Coppa Alessandro, Nazerian Peiman, Grifoni Stefano, Scorpiniti Margherita, Innocenti Francesca, Conti Alberto, Bigiarini Sofia, Gualtieri Simona, Casula Claudia, Ticali Piero Francesco and Pini Riccardo declare that they have no conflict of interest.
Ethical standard
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Zanobetti, M., Coppa, A., Nazerian, P. et al. Chest Abdominal-Focused Assessment Sonography for Trauma during the primary survey in the Emergency Department: the CA-FAST protocol. Eur J Trauma Emerg Surg 44, 805–810 (2018). https://doi.org/10.1007/s00068-015-0620-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-015-0620-y