Abstract
Introduction
The initial evaluation of patients with thoracic trauma remains a diagnostic challenge for surgery and emergency physicians. Chest sonography plays a key role in the approach for this group of patients, through extended and focused evaluation with trauma sonography (E-FAST).
Objectives
To establish the diagnostic performance of the extension of the thoracic spine sign using chest sonography in trauma to diagnose hemothorax and compare it with the gold standard test chest computed tomography (CT).
Methods
This prospective observational study was conducted over 1 year. Patients who attended the emergency room with closed or penetrating thoracic or thoraco-abdominal trauma, an indication for a chest CT as part of a diagnostic evaluation according to institutional protocols, and who previously underwent a chest sonogram to determine the extent of the thoracic spine sign to diagnose hemothorax. Sonographic results were compared to a radiologist’s interpretation of the chest CT. The radiologists were blinded to the initial sonogram interpretation.
Results
Seventy-six patients were enrolled with an average age of 32 years. They mainly had closed trauma, which accounted for 77.6% of samples, and 222 chest images were taken. The sensitivity and specificity for this study were 78.7% and 92.6%, respectively, with a positive predictive value and negative predictive value of 65% and 97.8%, respectively.
Conclusions
Extension of the thoracic spine sign allows rapid identification of the presence, and more precisely, the absence of pleural effusion. This, therefore, allows an appropriate diagnosis and approach in the emergency room in patients with chest trauma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The initial evaluation of patients with thoracic trauma remains a diagnostic challenge for surgery and emergency physicians. The low reliability of clinical history and physical examination in the context of trauma has led physicians to depend on diagnostic images for decision-making. Computed tomography (CT) is a widely used diagnostic tool, but it requires some radiation exposure, and it is also not a good option for unstable or potentially unstable patients [1]. However, the frequency of sonographic evaluation has increased over the last decade, and it is an essential complementary modality in the initial approach for trauma patients in the emergency department [2].
In 1996 was describe a systematic evaluation of patients using ultrasound [3, 4]. The Focused Assessment with Sonography in Trauma (FAST) is a diagnostic tool used in the trauma service for evaluation of the hypotensive trauma patient [5]. FAST allows rapid determination of fluid within the peritoneal cavity or pericardial sac. In the mid-2000s, the performance of complementary evaluation with chest ultrasound to detect pneumothorax was demonstrated and its addition to the traditional FAST examination resulted in an extended FAST (E-FAST) [6, 7], playing since then, a complementary role to the clinical examination and Thorax radiography in the trauma patient, especially with hemodynamic instability [8,9,10,11,12].
The initial approach for a patient with chest trauma in the emergency room is focused on identifying possible life-threatening intra-thoracic lesions that will require immediate treatment. Examples of these lesions are flail chest, tension pneumothorax, open pneumothorax, massive pneumothorax, and cardiac tamponade. In 90% of chest trauma cases, patients do not require urgent surgery management, and thus, they can be managed with less morbid and invasive procedures such as closed thoracostomy. Based on this data, ultrasound plays an important role in the diagnostic approach using E-FAST, which is a fundamental complement of prompt patient evaluation. It allows fast and accurate decision-making, mainly for classification of unstable or potentially unstable patients [13,14,15].
In trauma, the extension of the thoracic spine sign on a chest ultrasound can be an indirect sign of hemothorax. This sign is the image that is transmitted by the sonographic waves for visualization of the vertebral bodies in the chest cavity near the superior part of the diaphragm in the presence of pleural liquid. This sign is not normally seen because of wave reflection that is caused by air that is present in healthy lungs [16]. In patients with lung occupation, the vertebral bodies are visualized from the abdomen to the chest cavity because the transmission of sonographic waves is better in the presence of liquid, which, in this case, allows us to rapidly identify the presence of liquid or blood in the pleural space. Therefore, the extension of the thoracic spine sign allows a prompt and accurate diagnostic approach and clinical decision-making in the trauma scenario.
The aim of this study is to evaluate the diagnostic performance of extension of the thoracic spine sign in chest trauma in identifying hemothorax by comparing it to the chest CT (which is the gold standard diagnostic tool).
Materials and methods
This prospective observational study was performed from June 1, 2018 to April 4, 2019 at the emergency department of University Hospital Fundación Valle del Lili, Cali, Colombia. The service has a total capacity for 103 patients who are distributed in different sections, as follows: observation, hospitalization, advanced monitoring, and minor observation. This also includes a triage system that comprises nursing professionals, general physicians, emergency physicians, and internal medicine physicians.
Patients
Eligible patients included those over 17-years-old with thoracic or thoraco-abdominal trauma, either closed or penetrating, with an indication for a chest CT according to institutional protocols. Patients with previous pulmonary surgery or pleurodesis, closed thoracostomy in the initial evaluation before images, previous pneumonia diagnosis in the past 15 days, unable to lie down or lie at less than 45°, or other trauma other than chest trauma were excluded from the study. Each patient had two different records: one for each hemithorax.
Among the 139 records, 111 where included, and they belonged to 76 patients. Twenty-eight records were excluded for different reasons (Fig. 1). Each image had a duplicate record, and the date and time that the image was taken and the ultrasound operator’s name were checked.
An ultrasound image was made for each patient for each hemithorax. A comparison of the ultrasound image and chest CT corresponding to each hemithorax was performed. In addition, the result of both images (left and right hemithorax) as a single report and the chest CT were compared in a global way. For this last point, we take as present the sign of the spine if any of the two images of a patient’s hemithorax was evidenced on ultrasound.
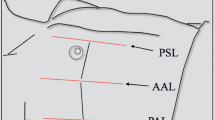
Chest sonography
Chest sonography was taken using Ultrasound Equipment Fujifilm Sonosite Edge II® (FUJIFILM Medical Systems Sonosite, Inc. Bothell, WA, 98021, USA), equipment with a Phased Array low frequency (1–5 MHz) transducer in the abdominal mode and a conventional bidimensional image. Images were taken with the patient in the supine decubitus position or laying at an incline of less than 45°. The transducer was placed in the cephalic direction. Pulmonary zones three and four and the hepatorenal and splenorenal views were evaluated in all patients. Once the diaphragm was located, the presence of pleural effusion was evaluated according to the presence of the extension of the thoracic spine sign (visualization of the thoracic spine vertebral bodies over the diaphragm) (Fig. 2).
Chest computed tomography
Patients who had an indication for chest CT as part of the initial evaluation based on the institutional protocol were included. Volumetric images were taken from the cranial base to the diaphragm, including the superior abdomen, and in some cases, if it was indicated, the pubic symphysis was included. If a contrast medium was needed, we used iodized media (iopromide) that was infused at a rate of 45 mL/s twice, with angiographic reconstruction using post-process MIP and VRT algorithms, which acquired only arterial and venous data. Images were interpreted in real time by an experimented radiologist who was blinded to the initial ultrasound results.
Data collection
Those who performed the ultrasounds were classified into two groups according to their formation degree, as follows: the team of specialists included emergency physicians and internists. This group had over 1 year of training in critical patient ultrasound. The other team was made up of internal medicine or emergency medicine residents who had less than 6 months of experience in the ultrasound technique. We called ecographists to take the images.
A physician was assigned as an investigation assistant to evaluate which patients in the emergency room fulfilled the inclusion criteria, and the ecographist was then asked to take the image without divulging information about the patient’s diagnosis, clinical history, or laboratory test. The images were interpreted in real time by ecographists, who also included the study variables in the database. All ultrasounds were taken before the CT scan.
The sonographic finding for the extension of the thoracic spine sign were quantified. These patients all had one chest CT, which is the gold standard, to evaluate the presence of pleural effusion, according to the institutional protocol. The findings were then compared to the sonogram images. Pleural effusion was defined as the presence of hemothorax or free liquid in the pleural space.
Statistical analysis
The sample size was calculated for diagnostic studies using paired groups [17], which estimated that 76 patients were needed to obtain a power of 80% with a significance level of 95%.
The discrete curative variables were expressed as the median and interquartile range (IR), and qualitative variables were expressed as the frequency and percentage. The precision and/or performance of each sonographic sign was obtained by comparing it to the chest CT results as the gold standard, including results for sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (LR +), and negative LR (LR −). This study was approved by the biomedical investigation ethics committee at the institution at which the study was performed. According to resolution 8430 of 1993 of the Colombian Ministry of Health, the descriptive studies are of lower risk than the minimum, taking into account that no interventions or modification of biological or physiological variables will be carried out. Therefore, the ethics committee was not asked to exempt informed consent.
Results
One hundred eleven records were included in the final analysis, which corresponds to 222 chest images. The age range was between 18 and 82 years, with a mean age of 32 years (IR, 25.50). Closed chest injury was the most common type of trauma (77%) (Table 1).
There were 13 patients with hemothorax in the right lung and 20 with hemothorax in the left lung who were diagnosed with chest CT; of these patients, 11 patients with hemothorax in the right lung and 15 with hemothorax in the left lung were diagnosed via sonographic study. The combined sensitivity and specificity for extension the thoracic spine sign were 78.7% [95% confidence interval (CI) 62.25–89.32] and 92.6% (95% CI 87, 95–95.54), respectively. The predictive values and the LRs were as follows: PPV, 65% (95% CI 49.51, 77.87); NPV, 97.8% (95% CI 92.27–98.12); LR +, 10.6 (95% CI 9.061–12.49); and LR −, 0.2 (95% CI 0.173–0.3034) (Tables 2, 3 and 4). Additionally, 89 of the 98 negative cases were correctly diagnosed in the right lung and 86 of the 91 true negatives were diagnosed in the left lung, based on the absence of the extension of the thoracic spine sign on chest ultrasound.
Discussion
Based on the results mentioned above, the diagnostic performance of the extension of the thoracic spine sign as a marker of hemothorax in a trauma context was high enough to be considered an accurate approach and sufficient for decision-making for managing trauma patients, highlighting a LR + of 10.6 (95% CI 9.061–12.49) and a NPV of 96.15% (95% CI 92.27–98.12).
In the emergency room, hemothorax is usually diagnosed by physical examination and chest x-ray. Although physical examination in the context of trauma in the emergency room has limited sensitivity and specificity [18]. Physical findings, such as hemodynamic instability, chest wall instability, hematoma, subcutaneous emphysema, and reduced respiratory sounds are easily detectable in initial care, which will allow prompt decision making (closed thoracotomy) even before a chest X-ray or E-FAST. The chest X-ray plays an irreplaceable role together with the clinical examination in the initial evaluation and management for the early detection of a series of life-threatening conditions (tension pneumothorax, pulmonary contusion, massive hemothorax, thoracic aortic rupture, among others). However, it can detect a relatively large effusion requiring at least 175 ml of fluid to show obliteration of the costophrenic angles on a vertical X-ray image [18]. Therefore, other diagnostic methods that are more accurate and reliable and that cost less are required to treat patients with chest trauma, in these cases E-FAST has a complementary function and the extension of the thoracic spine sign as a diagnostic marker can be a complement within the initial approach ultrasound protocol.
Normally the thoracic spine cannot be visualized above the diaphragm because lung air scatters ultrasound waves. In patients who have pleural occupation with liquid (blood), the spine can be visualized from the abdomen through the thoracic cavity. In the emergency room, patients with thoracic or thoraco-abdominal trauma (either closed or open) require a fast and reliable diagnostic method, which allows quick and accurate decisions to be made. Thus, evaluation of the extension of the thoracic spine sign will help to determine the presence of pleural effusion and, therefore, hemothorax in these patients, creating a practical and quick diagnostic protocol for the emergency room.
In 2004, Brooks et al. [19] evaluated chest ultrasonography as an extension of the FAST protocol compared to other diagnostic methods that were established at the time (chest X-ray, CT scan, thoracostomy, thoracotomy) in patients with chest trauma. They found a sensitivity and specificity for ultrasound of 92% and 100%, respectively, and a PPV and NPV of 100% and 92%, respectively for detecting hemothorax after trauma. They concluded that chest ultrasonography in the emergency context allows prompt and precise diagnosis of hemothorax and is, thus, a valuable key to increase the precision of clinical evaluation in these patients. These findings relate to our study, although the values we obtained were lower; this difference may be explained because in our study, images were taken by different observers with different degrees of experience.
The presence of an extension of the thoracic spine sign depends on how much liquid is present in the chest cavity and the angle at which the ultrasound study is performed. Therefore, the sign is less sensitive than the presence of free liquid in the cavity, but it is a finding that has diagnostic and therapeutic value in the emergency room [20].
Our findings using only one sonographic sign are consistent with those of historical records, demonstrating the strong diagnostic performance in detecting hemothorax, and having a high probability that hemothorax is not present when the sign is absent (96.15%). Although our sensitivity was slightly less than that of previous studies, it still shows that the sonographic sign has a strong diagnostic performance for diagnosing pleural effusion [16, 19, 21,22,23,24]. We also showed the diagnostic performance by determining the probability of having positive or negative results in patients with or without hemothorax, and we obtaining an LR + of 10.6 (95% CI 9.061–12.49) and an LR − of 0.22 (95% CI 0.173–0.3034), thus confirming a high precision and diagnostic performance.
The proportion of false negatives in our study ranged around 21.2%, this can be explained by carrying out the examination at a very early stage after the injury, where not enough free pleural fluid has accumulated yet. However, we consider that it was the result of a low hemothorax volume at the time of the examination and therefore a false negative “not relevant” or hemodynamically not significant, with no effect on the modification of patient care priorities and/or the taking additional medical behaviors. In addition, limitations in the quality of ultrasound images in subcutaneous emphysema, hematoma, and rib fractures should be considered.
Although a chest CT is the gold standard for diagnosing hemothorax, the time that is required to move the patient to the radiology unit and the time that is required to complete the CT limit its use in diagnosing and determining the prognosis of critical or potentially critical patients. The diagnostic performance of ultrasound allows a fast and precise approach, and it can even detect a small amount of pleural effusion, facilitating an accurate approach and management in the emergency department where time plays a major role, especially in unstable patients. This is relevant in initial trauma management, allowing characterization and stratification of the surgical intervention as urgent or emergent [25].
Future studies should evaluate the inter-observer agreement in observers with different degrees of experience in identifying the extension of the thoracic spine sign using a chest ultrasound in trauma patients. We considered the idea that the extension of the thoracic spine sign would be able to be clearly identified by observers without sufficient training and experience.
This study had some limitations. It took place at only one institution with thoraco-abdominal trauma rate was higher than other local institutions, which could limit comparison with other institutions with a lower trauma rate. It also was not possible to measure the reliability of the study independent of the ecographists’ experience. Measuring the ecographists’ experience was not possible because we could not guarantee that the ultrasound was performed for each patient by the two same physicians.
Another limitation was the small sample size and, therefore, the confidence intervals are wide. Another limitation relates to the number of ultrasounds that were performed by physicians within the past 6 months compared to ultrasounds that were performed by those with more than 1 year of experience. This could have affected the sensitivity.
In the statistical analysis, the agreement between residents and specialists was not assessed for the following reasons: first, only 24 patients were evaluated by two different ecographists, which is a small sample size to show a significant result. Second, in each group, the same ecographists were not involved, and this could generate variability when the findings were interpreted because in some cases. The second group of ecographists only had 2 weeks of training in performing an ultrasound examination on critical patients.
In conclusion, the extension of the thoracic spine sign allows prompt identification of the presence, and more specifically, the absence of occupying liquid in the pleural space. This allows an appropriate diagnostic approach and prompt and accurate decision-making in the emergency room in patients with thoracic or thoraco-abdominal trauma. Therefore, the possibility of adding the extension of the thoracic spine sign to the E-FAST protocol within the initial approach should be considered as a complementary diagnostic marker.
Code availability
Stata 15.
References
Heetveld MJ, Harris I, Schlaphoff G, Sugrue M. Guidelines for the management of haemodynamically unstable pelvic fracture patients. ANZ J Surg. 2004;74(7):520–9. https://doi.org/10.1111/j.1445-2197.2004.03074.x.
Montoya J, Stawicki SP, Evans DC, Bahner DP, Sparks S, Sharpe RP, et al. From FAST to E-FAST: an overview of the evolution of ultrasound-based traumatic injury assessment. Eur J Trauma Emerg Surg. 2016;42(2):119–26. https://doi.org/10.1007/s00068-015-0512-1.
Ali J, Rozycki GS, Campbell JP, Boulanger BR, Waddell JP, Gana TJ. Trauma ultrasound workshop improves physician detection of peritoneal and pericardial fluid. J Surg Res. 1996;63(1):275–9. https://doi.org/10.1006/jsre.1996.0260.
Boyes JH. Editor’s Comment. J Hand Surg Am. 1981;6(4):413. https://doi.org/10.1016/S0363-5023(81)80062-7.
Scalea TM, Rodriguez A, Chiu WC, Brenneman FD, Fallon WF, Kato K, et al. Focused assessment with sonography for trauma (FAST): results from an International Consensus Conference. J Trauma Int Infect Crit Care. 1999;46(3):466–72. https://doi.org/10.1097/00005373-199903000-00022.
Rowan KR, Kirkpatrick AW, Liu D, Forkheim KE, Mayo JR, Nicolaou S. Traumatic pneumothorax detection with thoracic US: correlation with chest radiography and CT–initial experience. Radiology. 2002;225(1):210–4.
Kirkpatrick AW, Sirois M, Laupland KB, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the extended focused assessment with sonography for trauma (EFAST). J Trauma. 2004;57(2):288–95.
Netherton S, Milenkovic V, Taylor M, Davis PJ. Diagnostic accuracy of eFAST in the trauma patient: a systematic review and meta-analysis. CJEM. 2019;21(6):727–38. https://doi.org/10.1017/cem.2019.381.
Montoya J, Stawicki SP, Evans DC, et al. From FAST to E-FAST: an overview of the evolution of ultrasound-based traumatic injury assessment. Eur J Trauma Emerg Surg. 2016;42(2):119–26. https://doi.org/10.1007/s00068-015-0512-1.
Akoglu H, Celik OF, Celik A, Ergelen R, Onur O, Denizbasi A. Diagnostic accuracy of the extended focused abdominal sonography for trauma (E-FAST) performed by emergency physicians compared to CT. Am J Emerg Med. 2018;36(6):1014–7. https://doi.org/10.1016/j.ajem.2017.11.019.
Bloom BA, Gibbons RC. Focused assessment with sonography for trauma (FAST). In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 5, 2020. PMID: 29261902. Bookshelf ID: NBK470479.
Pumarejo Gomez L, Tran VH. Hemothorax. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020 Jun 29. PMID: 30855807. Bookshelf ID: NBK538219.
Richards JR, McGahan JP. Focused assessment with sonography in trauma (FAST) in 2017: what radiologists can learn. Radiology [Internet]. 2017;283(1):30–48. https://doi.org/10.1148/radiol.2017160107.
McGahan J, Richards J. The focused abdominal sonography for trauma scan. J Ultrasound Med [Internet]. 2002. https://doi.org/10.7863/jum.2002.21.7.789.
Melniker LA, Leibner E, McKenney MG, Lopez P, Briggs WM, Mancuso CA. Randomized controlled clinical trial of point-of-care, limited ultrasonography for trauma in the emergency department: the first sonography outcomes assessment program trial. Ann Emerg Med. 2006;48(3):227–35. https://doi.org/10.1016/j.annemergmed.2006.01.008.
Dickman E, Terentiev V, Likourezos A, Derman A, Haines L. Extension of the thoracic spine sign: a new sonographic marker of pleural effusion. J Ultrasound Med. 2015;34(9):1555–611. https://doi.org/10.7863/ultra.15.14.06013.
Beam CA. Strategies for improving power in diagnostic Radiology research. AJR. 1992;159:631–7. https://doi.org/10.2214/ajr.159.3.1503041.
Atkinson P, Milne J, Loubani O, Verheul G. The V-line: a sonographic aid for the confirmation of pleural fluid. Crit Ultrasound J [Internet]. 2012;4(1):19. https://doi.org/10.1186/2036-7902-4-19.
Brooks A, Davies B, Smethhurst M, Connolly J. Emergency ultrasound in the acute assessment of haemothorax. Emerg Med J. 2004;21(1):44–6. https://doi.org/10.1136/emj.2003.005438.
Raheja R, Brahmavar M, Joshi D, Raman D. Application of lung ultrasound in critical care setting: a review. Cureus. 2019;11(7):1–15. https://doi.org/10.7759/cureus.5233.
Lau JSK, Yuen CK, Mok KL, Yan WW, Kan PG. Visualization of the inferoposterior thoracic wall (VIP) and boomerang signs-novel sonographic signs of right pleural effusion. Am J Emerg Med [Internet]. 2018;36(7):1134–8. https://doi.org/10.1016/j.ajem.2017.11.023.
Yousefifard M, Baikpour M, Ghelichkhani P, Asady H, Shahsavari Nia K, Moghadas Jafari A, et al. Screening performance characteristic of ultrasonography and radiography in detection of pleural effusion; a meta-analysis. Emerg (Tehran, Iran) [Internet]. 2016;4(1):1–10.
Ma J, Mateer JR. Trauma ultrasound examination versus chest radiography in the detection of hemothorax. Ann Emerg Med. 1997;1(2):312–6. https://doi.org/10.1016/S0196-0644(97)70341-X.
Eibenberger KL, Dock WI, Ammann ME, Dorffner R, Hörmann MF, Grabenwöger F. Quantification of pleural effusions: sonography versus radiography. Radiology [Internet]. 1994;191(3):681–4. https://doi.org/10.1148/radiology.191.3.8184046.
Melniker LA, Leibner E, McKenney MG, Lopez P, Briggs WM, Mancuso CA. Randomized controlled clinical trial of point-of-care, limited ultrasonography for trauma in the emergency department: the first sonography outcomes assessment program trial. Ann Emerg Med. 2006;48(3):227–35. https://doi.org/10.1016/j.annemergmed.2006.01.008.
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Fredy Watts, Carlos A. Vargas, Jaime A. Quintero, Roger Figueroa and Andres Castro declare that we have no conflict of interest.
Ethical approval
This study was approved by the biomedical investigation ethics committee at the institution at which the study was performed.
Consent to participate
This study was approved by the biomedical investigation ethics committee at the institution at which the study was performed. According to resolution 8430 of 1993 of the Colombian Ministry of Health, the descriptive studies are of lower risk than the minimum, taking into account that no interventions or modification of biological or physiological variables will be carried out. Therefore, the ethics committee was not asked to exempt informed consent.
Rights and permissions
About this article
Cite this article
Vargas, C.A., Quintero, J., Figueroa, R. et al. Extension of the thoracic spine sign as a diagnostic marker for thoracic trauma. Eur J Trauma Emerg Surg 47, 749–755 (2021). https://doi.org/10.1007/s00068-020-01459-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-020-01459-1