Abstract
The distal tibiofibular syndesmosis is essential for the stability of the ankle mortise. Injury to the distal tibiofibular syndesmosis can lead to mortise instability and should be treated with syndesmotic stabilization to prevent long-term complications and degenerative osteoarthritis. Syndesmotic injuries can occur in isolation but are often accompanied by a fracture and are most commonly due to external rotation trauma of the foot. Diagnosing syndesmotic injury can be challenging and should include a complete anamnesis and physical examination. Radiological evaluation can be of assistance but cannot be completely relied on. Treatment intends to restore the tibiofibular stability. A number of treatment options have been described of which the syndesmotic screw is the most widely used. There is no consensus on the number and diameter of screws, the number of cortices, the location of placement, and the after treatment.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Introduction
The distal tibiofibular syndesmosis plays an essential role in the stability of the ankle mortise and is therefore important for weight transmission and walking (Close 1956; Rasmussen et al. 1982; Hermans et al. 2010).
In general there are three types of syndesmotic injury: Often, a syndesmotic injury is accompanied with a fracture, it can also be an isolated syndesmotic injury without a fracture, and the last one is an isolated injury of the anterior inferior tibiofibular ligament. In approximately 10 % of all patients with ankle fractures, syndesmosis injuries occur (Jensen et al. 1998) and approximately 20 % of these patients require internal fixation (Seitz et al. 1991; Thordarson et al. 1997). The incidence of syndesmosis injuries is approximately 15 per 100,000 in the general population (Jensen et al. 1998).
In ankle sprains the incidence of syndesmotic injury is 1–18 % of all ankle sprains (Hopkinson et al. 1990; Boytim et al. 1991; Pijnenburg 2006). Isolated injury of the anterior inferior tibiofibular ligament occurs in 3 % of inversion trauma of the ankle (Pijnenburg 2006). In the literature, with a sprained ankle usually a lateral ankle sprain is intended. This is because it is the most common and there will be injury of the lateral collateral ligaments. A high ankle sprain is defined as an isolated injury of the syndesmotic ligaments. Because clinical examination is generally not specific, the diagnosis is often missed, causing the wide spread in incidence. There is a difference between an injury of one or all syndesmotic ligaments and real instability of the distal tibiofibular joint and the ankle mortise.
Anatomy and Biomechanics
The distal tibiofibular syndesmosis is a syndesmotic joint formed by two bones and four ligaments. The distal tibia and fibula form the osseous part of the syndesmosis, and the lateral aspect of the distal fibula is convex and fits into the concave tibial incisure (Hermans et al. 2010). In 75 % of cases, there are contact facets covered with 0.5–1.0 mm thick cartilage joining the distal tibia and fibula, thus forming a true synovial joint (Bartonicek 2003).
The four ligaments are the anterior inferior tibiofibular ligament (AITFL), the posterior inferior tibiofibular ligament (PITFL), the inferior transverse ligament (ITL), and the interosseous ligament (IOL) (Hermans et al. 2010; Fig. 1). The syndesmotic ligaments resist lateral and anterior-posterior diastasis of the fibula from the tibia. Beumer et al. (2003c) reported that, in an intact syndesmosis, application of a 75 Nm external rotation moment on the foot caused external rotation of the fibula between 2° and 5° and posterior displacement of the fibula between 1.0 and 3.1 mm. This force can be compared to the force during the stance phase of gait. It has been shown that 1 mm movement of the talus to lateral causes 42 % decrease of contact area of the tibiotalar articulation. The individual syndesmotic stability is 35 % for the AITFL, 33 % for the ITL, 22 % for the IOL, and 9 % for the PITFL (Ramsey and Hamilton 1976). The IOL proximal continues into the interosseous membrane (IOM). The IOM provides lateral translation of the fibula, and it has been shown that it is an important stabilizer of the ankle mortise in the absence of the syndesmosis and the deltoid ligament (Close 1956).
In the literature, the term syndesmotic injury is used to describe an injury of the syndesmotic ligaments. This is misleading because the syndesmosis is a true joint.
Mechanism of Injury
External rotation of the foot, eversion of the talus, and hyperdorsiflexion (Hopkinson et al. 1990; Boytim et al. 1991; Scranton 2002) are the most common causes of syndesmotic injuries. These injuries are most prevalent in contact sports, such as hockey, football, and rugby. External rotation injures the structures of the syndesmosis by widening the mortise (Turco 1997; Taylor and Bassett 1993).
The forces which arise in this type of injury cause the talus to rotate externally, thereby pushing the fibula externally away from the tibia, tearing one or more of the syndesmotic ligaments (Lauge-Hansen 1950; Wuest 1997). Widening of the ankle mortise that causes syndesmotic injury can also be the result of hyperdorsiflexion. The anterior aspect of the talar dome of the talus is wider than the posterior aspect causing the widening of the ankle mortise during dorsiflexion. With hyperdorsiflexion the forces become too high and the talus pushes the malleoli apart (Pankovich 1976) causing a sprain or rupture of the AITFL and PITFL (Turco and Gallant 1995). Syndesmotic injury is mostly combined with a fibular fracture such as Danis-Weber C/pronation-external rotation or pronation abduction (Riegels-Nielsen et al. 1983) and less frequently Danis-Weber B/supination-external rotation injuries (Heim et al. 2002). Some authors assume that the IOM is disrupted to the level of the fibular fracture and the higher the fibular fracture, the higher the changes of syndesmotic instability (Boden et al. 1989; Kennedy et al. 2000). Nielson et al. (2004) showed that the level of the fibular fracture does not correlate reliably with the level of interosseous membrane injury.
In American football and skiing, isolated ruptures of the syndesmosis caused by external rotation are reported but are rare (Fritschy 1989; Veltri et al. 1995; Pijnenburg 2006). The trauma mechanism of isolated AITFL rupture is an inversion/supination trauma of the ankle (Broström 1965; Fritschy 1989; Hopkinson et al. 1990; Uys and Rijke 2002).
Not all syndesmotic injuries lead to syndesmotic instability. When an unstable syndesmotic injury is not recognized and therefore untreated, it can cause degenerative changes leading to osteoarthritis and chronic pain.
Diagnoses
Symptoms
There are no specific symptoms that indicate syndesmotic injury, but pain in the anterolateral part of the ankle, swelling, inability to weight bear, pain during the push off phase of gait, and a feeling of giving way may be suggestive of an injury of the syndesmotic ligaments (Hopkinson et al. 1990). When there is a combination of syndesmotic injury with lateral ligament injury or an ankle fracture, the symptoms are not reliable.
Physical Examination
There are a number of special tests described to diagnose a syndesmotic injury in the absence of a fracture. The most common are the external rotation test when an external force is applied to the foot with stabilization of the leg (Boytim et al. 1991); the squeeze test, a compression of the fibula to the tibia above the midpoint of the calf (Hopkinson et al. 1990); the fibular translation test to move the fibula from anterior to posterior compared to the tibia (Ogilvie-Harris et al. 1994); and the Cotton test, where one translates the talus in the ankle mortise from medial to lateral with stabilization of the distal leg (Cotton 1910). The tests are positive if they provoke pain in the syndesmosis region, rather than increased displacement (Beumer et al. 2003).
The external rotation test has the lowest interobserver disagreement and the highest sensitivity (Alonso et al. 1998; Beumer et al. 2003; Sman et al. 2013). A functional stabilization test can also be subscribed (Harper and Keller 1989): A stabilizing tape bound the tibia and fibula tightly together. The patient is asked to stand, walk, and perform a toe raise and jump. When the pain is reduced after taping, the test is considered positive, suggesting a syndesmotic injury. The clinical tests may raise the suspicion of a syndesmotic injury, but they are not accurate in predicting syndesmotic instability (Beumer et al. 2003; Sman et al. 2012). Additional diagnostics may be necessary in almost all cases.
When syndesmotic injury is associated with an ankle fracture, clinical tests are not reliable. This is because of the pain, swelling, and dislocation that are associated with the fracture.
Imaging
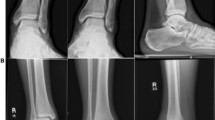
When there is a suspicion of syndesmotic injury, a standard mortise and lateral ankle radiography are the first type of imaging. Fractures can be ruled out or diagnosed. In case of an ankle fracture that requires surgery, further diagnostic is not necessary because the syndesmotic stability will be tested intraoperatively. The radiographs consist of a weight-bearing anterior to posterior (AP), a lateral view, and a mortise view. For evaluating diastasis of the fibula from the tibia, the radiographic parameters established by Harper et al. can be used (Harper and Keller 1989). These radiographic parameters are tibiofibular clear space, tibiofibular overlap, and medial tibiotalar clear space. A tibiofibular clear space of more than 6 mm or a tibiofibular overlap less than 6 mm on an AP view is suggestive for syndesmotic injury. This also applies for a tibiofibular overlap less than 1 mm or a medial tibiotalar clear space of more than 4 mm on a mortise view (Harper and Keller 1989; Evans and Schucany 2006; Fig. 2). All three parameters are affected by rotation of the tibia. The tibiofibular clear space on an AP view is the least unreliable of the three parameters because it is not significantly influenced by rotation of the tibia (Pneumaticos et al. 2002). Standard radiography will identify more severe injury but may not reveal mild instabilities (Beumer et al. 2003), and by a high rate of false negatives (Takao et al. 2003), normal radiographs cannot rule out syndesmotic instability.
On CT scans, the degree of deviations from normal tibiofibular clear space, tibiofibular overlap, and medial tibiotalar clear space is more precise than at radiography (Ebraheim et al. 1997). MRI can effectively image the structures of the syndesmosis with high interobserver agreement (Muhle et al. 1998). In acute injuries MRI has 93 % specificity and 100 % sensitivity for injury of the AITFL and 100 % specificity and sensitivity for injury of the PITFL compared to arthroscopy (Takao et al. 2003). In chronic syndesmosis injury sensitivity and specificity of MRI are 90 % and 95 %, respectively (Han et al. 2007). These studies are based on MRI in axial plane. Hermans et al. showed that a 45° oblique MRI plane has additional value in detecting an injury of the AITFL and the PITFL of their anatomical oblique course (Hermans et al. 2012).
It is important to determine or rule out if there is diastase of the fibula from the tibia, because it has consequences if it is left untreated. Isolated injury of the AITFL will not cause diastasis of the fibula from the tibia and therefore imaging is less important in the acute phase. If symptoms persist, imaging is indicated.
Arthroscopy
During arthroscopy, a stress test can be performed or a probe can be introduced in the distal tibiofibular joint to evaluate the stability of the syndesmosis. The intraoperative fluoroscopic external rotation stress tests are one of the test most often used (Jenkinson et al. 2005); the other is the Cotton test (Cotton 1910). An abnormal course or discontinuity of the ligament, a decrease in its tension, and a positive arthroscopic stress test are diagnostic criteria for syndesmotic instability. Takao et al. (2003) described that arthroscopy provides 100 % accuracy in detecting syndesmotic injuries (Fig. 3).
Intraoperative Assessment in Surgical Fixation of Ankle Fractures
It is difficult to predict syndesmotic instability preoperatively; therefore, intraoperative assessment is essential. The external rotation stress tests (Jenkinson et al. 2005) and Cotton or hook test (Cotton 1910; van den Bekerom 2011; Fig. 4) are the most widely used. These tests should always be performed after fixation of lateral (and medial or even posterior) malleolar fractures because syndesmotic injury combined with stable or stabilized medial and lateral malleoli does not always result in syndesmotic instability. Due the potential severe osteoarthritis of the mal-reduced ankle, whenever surgeons are in doubt about syndesmotic instability, fixation of the distal tibiofibular joint should be performed.
Treatment of Syndesmotic Instability
Operative Treatment of Syndesmotic Instability
There is an abundance of literature concerning the operative treatment of syndesmotic instability. A variety of syndesmotic fixation techniques have been described such as bioabsorbable screws, staples, cerclage wires, ank nails, bolts, and the syndesmotic hook; however, these are only sparsely noticed in literature and are not widely used (Burns 1942; Farhan and Smith 1985; Grady et al. 1995; Kara et al. 1999; Kabukcuoglu et al. 2000). Recently the use of a flexible implant has shown to be a safe and secure method, at least at the short term (den Daas et al. 2012). Most surgeons use the syndesmotic stabilization screw because of the wide experience, simple use, and good results. However, also the different technique options with the screw have been subject to debate.
Diameter of Screw
Both 3.5 and 4.5 mm screws for syndesmotic fixation are widely used, although in recent years there seems to be a tendency of favoring 3.5 mm screws (Monga et al. 2008; Bava et al. 2010; Schepers et al. 2012). In a study in which both screw diameters were biomechanically compared, no advantage was found for a 4.5 mm screw over a 3.5 mm screw (Thompson and Gesink 2000). Suggestions to adjust the diameter of the screw to the size of the fibula and tibia (as well as the length of the screw) have been made and seem, based on the literature available, justified (van den Bekerom et al. 2008). In a more recent biomechanical study, screw size and the number of engaged tibial cortices had no significant effect on mechanical stability of the distal fibula (Markolf et al. 2013).
Number of Screws
In a biomechanical study, two screw fixations were found to be superior to single screw fixation when applying external rotation to the ankle (Xenos et al. 1995). This was based on the higher external rotation force needed to induce failure of the fixation method. The value of this outcome for clinical practice is however doubtful. Hoiness and Stromsoe hypothesize that there were no functional differences in outcome, comparing one 4.5 mm quadricortical screw with two 3.5 mm tricortical screws, because of the same number of tibial cortices engaged in these two treatment options (Hoiness and Stromsoe 2004). In a randomized trial, the double tricortical screw fixation had higher functional scores after 3 months compared to a single quadricortical fixation. After 1 year, no significant differences were found and long-term results showed no significant difference (Wikerøy et al. 2010). Suggestions on the use of two screw fixation in certain cases have been made. Duchesneau and Fallat suggest the use of a quadricortical screw or two tricortical screws in mild to moderate diastasis and two quadricortical screws in complete instability in Maisonneuve fractures (Duchesneau and Fallat 1995). Thordarson (2004) recommends multiple quadricortical screw fixation in diabetics even in stable syndesmosis, in case of high risk for developing charcot arthropathy. The use of two screw fixation in obese or noncompliant patients has been made (van der Griend et al. 1997).
Number of Cortices
Four-cortical fixation provides more rigid stability, compared with tricortical fixation in syndesmotic instability. This method leads to less physiological movement in the ankle mortise. It is unclear if this will influence clinical outcome. In biomechanical research, no difference was found in strength of fixation of the syndesmosis through three or four cortices (Beumer et al. 2005; Nousiainen et al. 2008; Markolf et al. 2013). In a prospective randomized study, Moore et al. stabilized 127 people with syndesmotic disruptions with 3.5 mm cortical screws placed through three or four cortices. No differences were found in loss of reduction, screw breakage, or need for hardware removal (Moore et al. 2006). The prior mentioned statement of Duchesneau and Fallat to place a quadricortical screw or two tricortical screws in mild to moderate diastasis and two quadricortical screws in complete instability in Maisonneuve fractures could also be useful in this case. Also the removal of broken screws may be easier in quadricortical fixation compared to tricortical fixation.
Position of the Screw
The anatomical position of the fibula is posterior in respect to the tibia; therefore, a 30° anterior placement is advised to restore the fibula in the fibular notch (Hahn and Colton 2000). To prevent a proximal shift of the fibula, it has been recommended to place the screw parallel to the tibiotalar joint (Whittle 1998). Literature regarding the position of the screw in respect to the tibial plafond is not conclusive. McBryde et al. advised placement 2 cm above the tibiotalar joint because they found less syndesmotic widening in external rotation compared to screws placed at 3.5 cm proximal to the tibial plafond (Mcbryde et al. 1997). Kukreti, Faraj, and Miles evaluated the clinical and radiological outcomes in patients who had a transsyndesmotic screw placed and those who had a suprasyndesmotic syndesmotic screw placed. They reported no significant difference in terms of clinical and radiological outcomes (Kukreti et al. 2005).
Position of the Foot
Olerud reported in their cadaver study a decreased dorsal flexion of 0.1° for every degree of plantar flexion at implantation and therefore advised to place the syndesmotic screw with the foot in dorsiflexion (Olerud 1985). This could be explained by the anatomical properties of the talus. The wider anterior part of the talus could widen the mortise in dorsal flexion, placing the screw in neutral, or plantar flexion could impair this widening and therefore impair dorsal flexion. Tornetta et al. (2001) concluded that dorsal flexion of the ankle was not required during syndesmotic fixation to avoid loss of dorsal flexion after stabilization. In a randomized clinical trial by Rao, Muzammil, and Khan, no difference on the postoperative range of motion was seen when placing the syndesmotic screw with the ankle in neutral or 20° dorsiflexion (Rao et al. 2009).
Arthroscopy
Beside the previously mentioned diagnostic value of ankle arthroscopy in syndesmotic injury, arthroscopy can also contribute to the management of syndesmotic instability. When reducing the fibula in the fibular notch, ankle arthroscopy can monitor the anatomical reduction (Sri-Ram and Robinson 2005). Especially in Maisonneuve fractures, this can be a useful tool. Concomitant intra-articular injury such as chondral lesions can be monitored and treated when possible (Bekkers and Pijnenburg 2007).
Postoperative Management
It has been advised to start weight-bearing after screw removal because of the risk of abnormal ankle function or screw breakage (Needleman et al. 1989; Bell and Wong 2006). Beumer et al. (2005) advised to wait for weight-bearing after screw removal based on their findings that the syndesmotic screw cannot prevent excessive syndesmotic widening when loaded with a load comparable to body weight. Several clinical studies however found no difference in functional scores, pain, and range of motion between retained and removed screws. In a study by Manjoo et al., removed, broken, and loose screws had even better functional outcome than those with intact screws in situ. Hoiness compared outcome in patients with syndesmotic instability treated with one quadricortical screw or two tricortical screws. The quadricortical screw was routinely removed, whereas the two tricortical screws were retained. The authors did not find significant differences in functional scores, pain scores, and maximal dorsal flexion after 1 year (Hoiness and Stromsoe 2004).
Schepers reviewed clinical studies on the need for removal of the syndesmotic screw and concluded that the fear of less favorable outcome in retained screws seems unfounded. The author reported that screw removal could be considered if the positioning screw causes physical complaints, which is rare in tricortical placement (Schepers et al. 2011). In addition, the removal of the syndesmotic screw is accompanied by a complication rate of over 20 % (Schepers 2011; Hsu et al. 2011).
Complications
Complications due to fixation of the disrupted distal tibiofibular syndesmosis can occur. Inadequate reduction, even minimal, can result in tibiotalar joint incongruences which can lead to degenerative changes and poor clinical outcome (Klossner 1962; Ramsey and Hamilton 1976; de Souza et al. 1985). The rigid screw fixation of a joint, where normally physiological motion occurs, can result in syndesmotic screws breakage or loosening. However, the clinical consequences of this phenomenon seem minimal.
Synostosis formed after syndesmotic ligaments injury and syndesmotic screw placement have been reported (Albers et al. 1996). It is unclear if this is the result of the syndesmotic injury and subsequent hematoma which ossificates, the use of a syndesmotic screw, or both (Kaye 1989). Synostosis does not require treatment, especially if the ankle has good range of motion (Lindsjö 1981). Removal of the synostosis is advised only in active patients after maturation of the synostosis (van den Bekerom et al. 2013). Young and sportive patients might benefit from excision of the symptomatic ossification (Kottmeier et al. 1992; Veltri et al. 1995). Removal, breaking, or loosening of the screw before the ligaments have completely healed may induce recurrent diastasis (Donatto 2011) leading to chronic syndesmotic instability which is a difficult clinical problem (Roberts 1983; Whittle 1998).
Chronic Syndesmotic Instability
Syndesmotic injury can result in chronic syndesmotic instability. This is a challenging problem. In the literature, both mechanical and functional chronic instabilities are described (Freeman 1965). In mechanical instability clinical and radiographic criteria can be objectively documented. Functional instability is based on clinical symptoms only. With clinical examination stiffness, limited dorsiflexion in the tibiotalar joint, persistent pain, and swelling in the anterolateral aspect of the syndesmosis can be found. Radiographic examination should include the Cotton and the fibula translation tests, in which the possible motion of the fibula in respect to the tibia is compared to the contralateral side (van Dijk 2005). The type of management of chronic syndesmotic instability depends on the time elapsed after the initial trauma. In patients with subacute (6 weeks to 6 months) syndesmotic instability, the ruptured ligament is repaired and protected with placement of a syndesmotic screw. In chronic syndesmotic instability the ankle mortise should be restored with the creation of a distal tibiofibular synostosis (van den Bekerom et al. 2009). Although good results with late repair of syndesmotic instability have been described, treatment in the acute phase should always be pursued.
Conclusion
The distal tibiofibular syndesmosis is essential for the stability of the ankle mortise. Injury to the distal tibiofibular syndesmosis can lead to mortise instability and should be treated with syndesmotic stabilization to prevent long-term complications and degenerative osteoarthritis.
External rotation of the foot, eversion of the talus, and hyperdorsiflexion are the most common causes of syndesmotic injuries.
There are a number of special tests described to raise the suspicion of a syndesmotic injury, but they are not accurate in predicting syndesmotic instability. Additional diagnostics may be necessary in almost all cases. To make the diagnosis radiography, CT and MRI are used. MRI is the more specific and sensitive compared with arthroscopy which has an accuracy of 100 %.
It is difficult to predict syndesmotic instability preoperatively; therefore, intraoperative assessment is essential.
There is no evidence favoring a 4.5 mm screw over a 3.5 mm screw or vice versa. Screw diameter might therefore be adjusted to the preference of the surgeon. No benefit of placing two screws has been reported. Multiple screw placements could be considered in instability in Maisonneuve fractures, diabetic, and/or obese patients. The most widely used methods of syndesmotic stabilization are the conventional syndesmotic screw and the flexible implant. Other methods of fixation are only sparsely mentioned in literature. In biomechanical studies minimal anatomical and functional changes of the stabilized ankle have been described. In clinical studies no functional limitations of the syndesmotic screw were found, not even with broken or loosened screws. Retainment of the syndesmotic screw might therefore be considered in asymptomatic ankles. Weight-bearing in a plaster should be allowed postoperatively if an adequate osteosynthesis has been obtained. The consequences of not or late recognizing syndesmotic instability are serious. Complications of syndesmotic stabilization however are rare.
References
Albers GH, de Kort AF, Middendorf PR et al (1996) Distal tibiofibular synostosis after ankle fracture. A 14-year follow-up study. J Bone Joint Surg Br 78:250–252
Alonso A, Khoury L, Adams R (1998) Clinical tests for ankle syndesmosis injury: reliability and return of function. J Orthop Sports Phys Ther 27:276–284
Bartonicek J (2003) Anatomy of the tibiofibular syndesmosis and its clinical relevance. Surg Radiol Anat 25:379–386
Bava E, Charlton T, Thordarson D (2010) Ankle fracture syndesmosis fixation and management: the current practice of orthopaedic surgeons. Am J Orthop (Belle Mead NJ) 39(5):242–246
Bekkers JEJ, Pijnenburg ACM (2007) Artroscopisch geleide behandeling van syndesmoseletsel. Ned Tijdschr Traumatol 15(1):11–14
Bell DP, Wong MK (2006) Syndesmotic screw fixation in Weber C ankle injuries-should the screw be removed before weigthbearing? Injury 37:891–898
Beumer A, van Hemert WL, Swierstra BA et al (2003a) A biomechanical evaluation of clinical stress tests for syndesmotic ankle instability. Foot Ankle Int 24:358–363
Beumer A, Valstar ER, Garling EH et al (2003b) External rotation stress imaging in syndesmotic injuries of the ankle: comparison of lateral radiography and radio-isometry in a cadaveric model. Acta Orthop Scand 74:201–205
Beumer A, Valstar ER, Garling EH et al (2003c) Kinematics of the distal tibiofibular syndesmosis: radiostereometry in 11 normal ankles. Acta Orthop Scand 74(3):337–343
Beumer A, Campo MM, Niesing R et al (2005) Screw fixation of the syndesmosis: a cadaver model comparing stainless steel and titanium screws and three and four cortical fixation. Injury 36:60–64
Boden SD, Panos LA, McCowin P et al (1989) Mechanical consideration for the syndesmotic screw. J Bone Joint Surg Am 71:1548–1555
Boytim MJ, Fischer DA, Neumann L (1991) Syndesmotic ankle sprains. Am J Sports Med 19:294–298
Broström L (1965) Sprained ankles. III. Clinical observations in recent ligament ruptures. Acta Chir Scand 130:560–569
Burns BH (1942–1943) Diastasis of the inferior tibiofibular joint. Proc R Soc Med 36:330–332
Close JR (1956) Some applications of the functional anatomy of the ankle joint. J Bone Joint Surg Am 38-A(4):761–781
Cotton FJ (1910) Fractures and joint dislocation. WB Saunders, Philadelphia, p 549
De Souza LJ, Gustilo RB, Meyer TJ (1985) Results of operative treatment of displaced external rotation-abduction fractures of the ankle. J Bone Joint Surg Am 67:1066–1074
den Daas A, van Zuuren WJ, Pelet S et al (2012) Flexible stabilization of the distal tibiofibular syndesmosis: clinical and biomechanical considerations: a review of the literature. Strateg Trauma Limb Reconstr 7(3):123–129
Donatto KC (2011) Ankle fractures and syndesmosis injuries. Orthop Clin North Am 32(1):79–90
Duchesneau S, Fallat LM (1995) The Maisonneuve fracture. J Foot Ankle Surg 34:422–428
Ebraheim NA, Lu J, Yang H et al (1997) Radiographic and CT evaluation of tibiofibular syndesmotic diastasis: a cadaver study. Foot Ankle Int 18:693–698
Evans JM, Schucany WG (2006) Radiological evaluation of a high ankle sprain. Proc (Baylor Univ Med Cent) 19(4):402–405
Farhan MJ, Smith TW (1985) Fixation of diastasis of the inferior tibiofibular joint using the syndesmosis hook. Injury 16:309–311
Freeman MAR (1965) Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br 47:669–677
Fritschy D (1989) An unusual ankle injury in top skiers. Am J Sports Med 17:282–285
Grady JF, Moore CJ, O’Connor KJ et al (1995) The use of a transsyndesmotic bolt in the treatment of tibiofibular diastasis: two case studies. J Foot Ankle Surg 34:571–576
Hahn DM, Colton CL (2000) Malleolar fractures. In: Ruedi TP, Murphy WL (eds) AO principles of fracture management, vol 2. Thieme, New York, pp 559–581
Han SH, Lee JW, Kim S et al (2007) Chronic tibiofibular syndesmosis injury: the diagnostic efficiency of magnetic resonance imaging and comparative analysis of operative treatment. Foot Ankle Int 28(3):336–342
Harper MC, Keller TS (1989) A radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle 10:156–160
Heim D, Schmidlin V, Ziviello O (2002) Do type B malleolar fractures need a positioning screw? Injury 33:729–734
Hermans JJ, Beumer A, de Jong TA et al (2010) Anatomy of the distal tibiofibular syndesmosis in adults: a pictorial essay with a multimodality approach. J Anat 217(6):633–645
Hermans JJ, Beumer A, Hop WCJ et al (2012) Tibiofibular syndesmosis in acute ankle fractures: additional value of an oblique MR image plan. Skeletal Radiol 41:193–202
Hoiness P, Stromsoe K (2004) Tricortical versus quadricortical syndesmosis fixation in ankle fractures: a prospective, randomized study comparing two methods of syndesmosis fixation. J Orthop Trauma 18:331–337
Hopkinson WJ, St Pierre P, Ryan JB et al (1990) Syndesmosis sprains of the ankle. Foot Ankle 10:325–330
Hsu YT, Wu CC, Lee WC et al (2011) Surgical treatment of syndesmotic diastasis: emphasis on effect of syndesmotic screw on ankle function. Int Orthop 35(3):359–364
Jenkinson RJ, Sanders DW, Macleod MD et al (2005) Intraoperative diagnosis of syndesmosis injuries in external rotation ankle fractures. J Orthop Trauma 19(9):604–609
Jensen SL, Andresen BK, Mencke S et al (1998) Epidemiology of ankle fractures: a prospective population-based study of 212 cases in Aalborg, Denmark. Acta Orthop Scand 69:48–50
Kabukcuoglu Y, Kucukkaya M, Eren T et al (2000) The ANK device: a new approach in the treatment of the fractures of the lateral malleolus associated with the rupture of the syndesmosis. Foot Ankle Int 21:753–758
Kara AN, Esenyel CZ, Sener BT et al (1999) A different approach to the treatment of the lateral malleolar fractures with syndesmosis injury: the ANK nail. J Foot Ankle Surg 38:394–402
Kaye RA (1989) Stabilisation of ankle syndesmosis injuries with a syndesmotic screw. Foot Ankle 9:290–293
Kennedy JG, Soffe KE, Dalla Vedova P et al (2000) Evaluation of the syndesmotic screw in low Weber C ankle fractures. J Orthop Trauma 14:359–366
Klossner O (1962) Late results of operative and non-operative treatment of severe ankle fractures. Acta Chir Scand 293(Suppl) 1–93
Kottmeier SA, Hanks GA, Kalenak A (1992) Fibular stress fracture, associated with distal tibiofibular synostosis in an athlete: a case report and literature review. Clin Orthop 281:195–198
Kukreti S, Faraj A, Miles JN (2005) Does position of syndesmotic screw affect functional and radiological outcome in ankle fractures? Injury 36:1121–1124
Lauge-Hansen N (1950) Fractures of the ankle II. Combined experimental surgical and experimental-roentgenologic investigations. Arch Surg 60:957–985
Lindsjö U (1981) Operative treatment of ankle fractures. Acta Orthop Scand Suppl 52:1–131
McBryde A, Chiasson B, Wilhelm A et al (1997) Syndesmotic screw placement: a biomechanical analysis. Foot Ankle Int 18:262–266
Monga P, Kumar A, Simons A et al (2008) Management of distal tibio-fibular syndesmotic injuries: a snapshot of current practice. Acta Orthop Belg 74(3):365–369
Moore JA Jr, Shank JR, Morgan SJ et al (2006) Syndesmosis fixation: a comparison of three and four cortices of screw fixation without hardware removal. Foot Ankle Int 27:567–572
Morkolf KL, Yockson SR, MCSAllistee DR (2013) Syndesmosig fixation using dual 3.5 mm and 4.5 mm Screns with tricortical and quadricortical purchose: a biomechanical study. Foot Ankle Int 34:734–739
Muhle C, Frank LR, Rand T et al (1998) Tibiofibular syndesmosis: high-resolution MRI using a local gradient coil. J Comput Assist Tomogr 22(6):938–944
Needleman RL, Skrade DA, Stiehl JB (1989) Effect of the syndesmotic screw on ankle motion. Foot Ankle 10:17–24
Nielson JH, Sallis JG, Potter HG et al (2004) Correlation of interosseous membrane tears to the level of the fibular fracture. J Ortop Trauma 182:68–74
Nousiainen MT, McConnell AJ, Zdero R et al (2008) The influence of the number of cortices of screw purchase and ankle position in Weber C ankle fracture fixation. J Orthop Trauma 22:473–478
Ogilvie-Harris DJ, Reed SC, Hedman TP (1994) Disruption of the ankle syndesmosis: biomechanical study of the ligamentous restraints. Arthroscopy 10:558–560
Olerud C (1985) The effect of the syndesmotic screw on the extension capacity of the ankle joint. Arch Orthop Trauma Surg 104(5):299–302
Pankovich AM (1976) Maisonneuve fracture of the fibula. J Bone Joint Surg Am 58:337–342
Pijnenburg ACM (2006) Thesis: acute ankle injuries; diagnostic and therapeutic strategies on evidence-based grounds. ACM Pijnenburg, University of Amsterdam, The Netherlands
Pneumaticos SG, Noble PC, Chatziioannou SN et al (2002) The effects of rotation on radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle Int 23:107–111
Ramsey PL, Hamilton W (1976) Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg Am 58(3):356–357
Rao SE, Muzammil S, Khan AH (2009) Technique of syndesmotic screw insertion in weber C ankle fractures. J Surg Pak 14:58–62
Rasmussen O, Tovborg-Jensen I, Boe S (1982) Distal tibiofibular ligaments. Analysis of function. Acta Orthop Scand 53(4):681–686
Riegels-Nielsen P, Christensen J, Greiff J (1983) The stability of the tibio-fibular syndesmosis following rigid internal fixation for type C malleolar fractures: an experimental and clinical study. Injury 14:357–360
Roberts RS (1983) Surgical treatment of displaced ankle fractures. Clin Orthop Relat Res 172:164–170
Schepers T (2011) To retain or remove the syndesmotic screw: a review of literature. Arch Orthop Trauma Surg 131(7):879–883
Schepers T, Van Lieshout EM, de Vries MR et al (2011) Complications of syndesmotic screw removal. Foot Ankle Int 32(11):1040–1044
Schepers T, van Zuuren WJ, van den Bekerom MP et al (2012) The management of acute distal tibio-fibular syndesmotic injuries; Results of a nationwide survey. Injury 43(10):1718–1723
Scranton PE (2002) Isolated syndesmotic injuries: diastasis of the ankle in the athlete. Tech Foot Ankle Surg 1:88–93
Seitz WH Jr, Bachner EJ, Abram LJ et al (1991) Repair of the tibiofibular syndesmosis with a flexible implant. J Orthop Trauma 51:78–82
Sman AD, Hiller CE, Refshauge KM (2013) Diagnostic accuracy of clinical tests for diagnosis of ankle syndesmosis injury: a systematic review. Br J Sports Med 47(10):620–628
Sri-Ram K, Robinson AH (2005) Arthroscopic assessment of the syndesmosis following ankle fracture. Injury 36(5):675–678
Takao M, Ochi M, Oae K et al (2003) Diagnosis of a tear of the tibiofibular syndesmosis: the role of arthroscopy of the ankle. J Bone Joint Surg 85B:324–329
Taylor DC, Bassett FH (1993) Syndesmosis ankle sprains: diagnosing the injury and aiding recovery. Phys Sports Med 21(12):39–46
Thompson MC, Gesink DS (2000) Biomechanical comparison of syndesmosis fixation with 3.5- and 4.5-millimeter stainless steel screws. Foot Ankle Int 21:736–741
Thordarson DB (2004) Ankle fractures in diabetics. Tech Foot Ankle Surg 3(3):192–197
Thordarson DB, Hedman TP, Gross D et al (1997) Biomechanical evaluation of polylactide absorbable screws used for syndesmosis injury repair. Foot Ankle Int 18:622–627
Tornetta P 3rd, Spoo JE, Reynolds FA et al (2001) Overtightening of the ankle syndesmosis: is it really possible? J Bone Joint Surg Am 83-A(4):489–492
Turco VJ (1997) Injuries to the ankle and foot in athletics. Orthop Clinics North Am 8:669–682
Turco VJ, Gallant GG (1995) Occult trauma and unusual injuries in the foot and ankle. In: Nicholas JA, Hershman EB (eds) The lower extremity and spine in sports medicine, vol 1, 2nd edn. CV Mosby, St Louis, pp 475–493
Uys HD, Rijke AM (2002) Clinical association of acute lateral ankle sprain with syndesmotic involvement: a stress radiography and magnetic resonance imaging study. Am J Sports Med 30(6):816–822
van den Bekerom MPJ (2011) Diagnosing syndesmotic instability in ankle fractures. World J Orthop 2(7):51–56
van den Bekerom MPJ, Hogervorst M, Bolhuis HW et al (2008) Operative aspects of the syndesmotic screw: Review of current concepts. Inju Int J Care Inju 39:491–498
van den Bekerom MP, de Leeuw PA, van Dijk CN (2009) Delayed operative treatment of syndesmotic instability. Current concepts review. Injury 40(11):1137–1142
van den Bekerom MP, Kloen P, Luitse JS et al (2013) Complications of distal tibiofibular syndesmotic screw stabilization: analysis of 236 patients. J Foot Ankle Surg S1067–2516(13):00140–00143
van der Griend R, Michelson JD, Bone LB (1997) Fractures of the ankle and the distal part of the tibia. Instr Course Lect 46:311–321
van Dijk CN (2005) Acute syndesmotic injury. In: Chan KM, Karlsson J (eds) ISAKOS-FIMS world consensus conference on ankle instability. ISAKOS (International Society of Arthroscopy, Knee Surgery and Orthopaedic Spoets Medicine, San Ramon, USA
Veltri DM, Pagnani MJ, O’Brien SJ et al (1995) Symptomatic ossification of the tibiofibular syndesmosis in professional football players: a sequela of the syndesmotic ankle sprain. Foot Ankle Int 16:285–290
Whittle AP (1998) Fractures of the lower extremity. In: Canale ST (ed) Campbell’s operative orthopaedics, 39th edn. Mosby, St Louis, pp 2046–2048
Wikerøy AK, Høiness PR, Andreassen GS et al (2010) No difference in functional and radiographic results 8.4 years after quadricortical compared with tricortical syndesmosis fixation in ankle fractures. J Orthop Trauma 24(1):17–23
Wuest TK (1997) Injuries to the distal lower extremity syndesmosis. J Am Acad Orthop Surg 5:172–181
Xenos JS, Hopkinson WJ, Mulligan ME et al (1995) The tibiofibular syndesmosis. Evaluation of the ligamentous structures, methods of fixation, and radiographic assessment. J Bone Joint Surg Am 77:847–856
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Berlin Heidelberg
About this entry
Cite this entry
de Vaal, M.M., van Zuuren, W., van den Bekerom, M.P.J., Pijnenburg, B.A.C.M. (2015). Syndesmosis Injuries. In: Doral, M.N., Karlsson, J. (eds) Sports Injuries. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-36569-0_137
Download citation
DOI: https://doi.org/10.1007/978-3-642-36569-0_137
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-36568-3
Online ISBN: 978-3-642-36569-0
eBook Packages: MedicineReference Module Medicine