Abstract
Purpose
The purpose of our study was to determine the biomechanical properties of three different implants utilized for internal fixation of a supracondylar femur fracture. The retrograde supracondylar nail (SCN), the less invasive stabilization system plate (LISS) and the distal femoral nail (DFN) were tested and their biomechanical properties compared.
Methods
Twenty pairs of fresh-frozen human femura were used. Each femur was osteotomised to simulate a comminuted supracondylar fracture (AO/OTA 33.A3) and then randomized to fracture fixation with either SCN (n=9) or LISS (n=9). Each contralateral femur was stabilized with DFN as a control (n=18). Two femur pairs were spent on pretesting. All femura were subjected to axial (10–500 N) and torsional (0.1–14 Nm) loading.
Results
Eighteen matched femur pairs were analyzed. The post-loading median residual values were 49.78, 41.25 and 33.51% of the axial stiffness of the intact femur and 59.04, 62.37 and 46.72% of the torsional stiffness of the intact femur in the SCN, LISS and DFN groups. There were no significant differences between the three implants concerning axial and torsional stiffness.
Conclusions
All implants had sufficient biomechanical stability under physiological torsional and axial loading. All three implants have different mechanisms for distal locking. The SCN nail with the four-screw distal interlocking had the best combined axial and torsional stiffness whereas the LISS plate had the highest torsional stiffness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Between four and seven percent of femur fractures have a supracondylar localization [1, 6, 13]. Fractures in the distal third of the femur are around ten times less frequent than in the proximal [18]. Even if the prevalence of distal femur fractures is low, therapy is often difficult [6, 13, 19]. The trauma leading to distal femur fractures is different for young and older patients. Distal femur fractures in younger and adults are the result of high-energy impact and have complex fracture configurations [18, 25]. Eighty-five percent of the supracondylar fractures occurring in patients over 50 years of age are the result of low-energy trauma and have simple fracture forms [5, 24, 25]. Especially in elderly patients with poor bone stock, it may be difficult to achieve an adequately stable bone-implant construct [2, 6, 16].
The goal of treatment of distal femur fractures is to restore axial and rotational alignment and to create sufficient stability for early mobilization, all with minimal soft-tissue disruption [9]. Tension forces of the muscles around the knee joint and the joint movement itself tend to dislocate fracture fragments and therefore require strong fixation.
A number of devices and fixation techniques are available for distal femur fracture fixation [5, 6, 19, 30]. Actually, closed reduction with intramedullary retrograde nails and less invasive plate osteosynthesis are preferred methods of fixation [6, 8, 17, 19, 22, 24]. Intramedullary nailing has shown to be a successful fracture fixation with a favorable decrease of intraoperative blood loss, operating time, and hospital stay when compared with plate osteosynthesis [7, 11, 29]. A disadvantage of intramedullary nails is the poor stability of the distal interlocking screws or spiral blades in osteoporotic bone with the risk of nail protrusion into the articular space of the knee, resulting in knee damage or secondary malalignment as well as decreased knee motion [9–11].
There are different nails for intramedullary fixation of distal femur fractures available. In this study the distal femur nail (DFN) and the supracondylar nail (SCN) were tested. The main differences between both nails are the distal interlocking modalities. Using the DFN, stabilization of the condylar block is achieved by double interlocking in one plane. Spiral blade stabilization provides a broad bone-metal interface. Using the SCN fracture, stabilization is achieved with two condylar screws with nuts in the frontal plane. The lowermost screw is fixed in the interlocking hole using an end cap. Two additional interlocking screws, one placed in the anteromedial to posterolateral, the other in the anterolateral to posteromedial direction, enable additional fixation. When all four screws are used, interlocking is achieved in three directions. A variety of distal femur fractures, ranging from extra-articular metaphyseal (AO/OTA type A), to simple intra-articular (AO/OTAtype C1), can be stabilized with these nails. The LISS plate relies on extramedullary internal fixation by means of an anatomically pre-shaped plate that works like an internal splint. The surgical technique is referred to as minimally invasive plate osteosynthesis (MIPO): soft tissue dissection at the fracture site is minimized and the knee joint can remain closed [12, 15, 28]. Fixed-angle stabilization is achieved by using angular stable screws inserted into bone at a fixed angle [14]. No or minimal pressure is applied to the bone-nutrifying periosteum. The LISS fixation is an alternative to classic open reduction and internal fixation with compression plates. Delayed union, non-union as well as failure of fixation can occur when very rigid plates are used in distal femoral fractures with a simple fracture pattern [3, 23, 27].
The objective of our study was to determine the axial and rotational stiffness of distal femur fixation with three implants, differing in the mechanism of fixation and distal locking. The distal femoral nail (DFN) was chosen as reference and was compared to the retrograde supracondylar nail (SCN) and the less invasive stabilization system (LISS). This objective is of great importance because all three implants are in daily clinical use. With this biomechanical study, we examined if these implants achieve adequate fixation of a simulated comminuted supracondylar distal femur fracture, and, when they show any differences in stiffness, if they have any clinical relevance.
Materials and methods
Specimens
Twenty matched-pairs of fresh human cadaveric femura were used. The average age of the donors (8 male, 12 female) at the time of death were 78.2 years (range 66–93 years). Permission was obtained from the ethics commission. To detect osseous lesions, X-rays were taken from each specimen in two planes. The presence of a previous femoral fracture, a hip replacement or another implant and any kind of bone diseases were exclusion criteria. Additionally, all femura were evaluated for bone quality, similarity and mineral density using a dual-energy X-ray absorptiometry scan (DEXA, Hologic, Bedford, MA, USA).
Preparation
Specimens were stored at −20 °C up to −24 °C until preparation for biomechanical testing. All specimens were thawed at room temperature overnight, preventing dehydration by using moist cloths soaked in saline. After completely dissecting the soft tissues, the femura were proximally shortened to a complete length of 30 cm. The proximal and distal ends (condyle tips) of each femur were mounted in custom-built polymethylacrylat (PMMA) molds parallel to the condyles. A visual inspection for exact symmetrical positioning of both femura in the molds was performed.
Osteosynthesis and testing procedure
The femura were positioned with the PMMA potting in a servo-pneumatic testing machine with tension–torsion–actuators. The femoral shaft axis was tilted 6° to the vertical testing axis of the tension actuator (Fig. 1) [21]. The distal end (condyles) of the specimens was gimbal-mounted in the testing axis with 5 degrees of freedom of movement.
This setup tested compression, bending and torque resembling physiological axes (partial weight bearing of app. 50 kg). Prior to osteotomy and osteosynthesis, the solid embedded specimens were loaded with a maxima of axial compression of 500 N and 14 Nm in torsion, simulating a sinusoidal function [20]. Testing was completed after four cycles. These tests were done to obtain the baseline axial and torsional stiffness for each intact femur. With a sampling rate of 25 Hz the mean stiffness was calculated. Force versus elongation (alternation in length) in the test axis was defined as axial (= tension) stiffness in Newton per meter (N/m). Torque versus rotation was defined as torsion stiffness in Newton meter per degree (Nm/°).
A complete segmental defect of 1 cm was created by double transverse osteotomy in the distal metaphysis of each femur to reproduce the loss of structural continuity typical of fracture comminution prior to callus formation and thereby simulate an AO/OTA 33.A3 type fracture. The 1 cm transverse bone disc was cut out 6 cm proximal of the notch, perpendicular to the axis of the femoral shaft, according to the fracture model of Zlowodzki et al. [30].
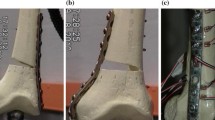
Subsequently, a randomized protocol predefined the side of the femoral pair for the Distal Femoral Nail, DFN (Synthes GmbH, Oberdorf, Switzerland) (n = 18) and the contralateral side for either the Supracondylar Nail, SCN (Stryker Trauma GmbH, Kiel, Germany) (n = 9) or the Less Invasive Stabilisation Sytem, LISS (Synthes, Paoli, PA, USA) (n = 9) (Fig. 2). All constructs were implanted by the same surgeon in accordance with the manufacturer’s instructions. Before the second series of tests, all specimens were again X-rayed in the anterior-posterior and lateral-medial planes.
Each femur-implant construct was subjected to 200 load cycles. Axial load with an amplitude of 10–500 N and torsional load with an amplitude of 0.1–14 Nm were used similar to the load application in the tests of the intact femora. Each cycle lasts 10 s; 5 s of torque load starting at 0.5 Nm up to 14 Nm peak load synchronous with axial load starting at 10 N up to 500 N peak load followed by 5 s of unloading back to preload. The loads mentioned above were derived from the results of the pretesting of the two additional intact femora.
The software setting of the testing machine, the mounting of the samples and the stiffness-calculation program remained unchanged during all testing procedures. The results of the test of all bone-implant constructs were put in relation (percentage of stiffness) to the results of testing of the intact femora. The results of testing of the intact femora were called baseline values and put as 100 %.
Closure of the osteotomy gap or failure of osteosynthesis during testing was defined as complete loss of resistance of the bone implant constructs.
Statistical evaluation was performed using the Wilcoxon test in 2 × 9 pair comparisons: DFN–SCN and DFN–LISS. The nine differences between SCN–LISS as unconnected comparison were evaluated statistically with the rank sum test. Statistical analysis was performed using SPSS for Windows (version 17.0). To detect significant differences between implant groups, the Wilcoxon signed rank test was used. A value of P < 0.05 was considered statistically significant.
Results
The biomechanical data on a total of 36 femura (18 matched pairs) were analyzed. Two femura were used for pre-testing. The mean bone mineral density was 1.38 (0.98–1.68) g/cm².
The mean baseline-values of the intact femura for tension stiffness were 333.5 N/mm and for torsion stiffness 2.24 Nm/° (Figs. 3, 4).
DFN versus SCN
Under axial compression, the reconstructed tension stiffness was 44.6 % of the baseline-value of the intact femura (±25.1) for DFN and 52.8 % (±12.9) for SCN. After 200 cycles the stiffness under axial compression was 32.7 % (±25.7) for DFN and 37.9 % (±13.8) for SCN. The reconstructed torsional stiffness was 48.7 % (±14.9) for DFN and 55.3 % (±9.3) for SCN. After 200 cycles the stiffness under torque was 19.2 % (±15.1) for DFN and 26.6 % (±7.9) for SCN (Figs. 5, 6).
Reconstruction tension stiffness: Medians and interquartile ranges are marked as the black lines in the box plots; the bras represent the 25th to 75th percentile; outliners represent the minimum and maximum in the testing in the first four cycles and after 200 cycles. The mean results of the different implants are subtracted as shown: Values below zero in the plots show more stiffness in the DFN-specimens. Values above zero indicate more stiffness of the SCN and the LISS
Reconstruction torsion stiffness: Medians and interquartile ranges are marked as the black lines in the box plots; the bars represent the 25th to 75th percentile; outliners represent the minimum and maximum in the testing in the first four cycles and after 200 cycles. The mean results of the different implants are subtracted as shown: Values below zero in the plots show more stiffness in the DFN-specimens. Values above zero indicate more stiffness of the SCN and the LISS
DFN versus LISS
The reconstructed tension stiffness was 36.4 % (±25.1) for DFN and 36.7 % (±17.7) for LISS. After 200 cycles the stiffness under axial compression was 18.2 % (±19.2) for DFN and 20.8 % (±21.7) for LISS. The reconstructed torsional stiffness was 53.3 % (±10.6) for DFN and 63.7 % (±9.3) for LISS. After 200 cycles the torsional stiffness was 17.1 % (±15) for DFN and 27.1 % (±25) for LISS (Figs. 5, 6).
Implant failure
Comparing DFN against SCN, two instrumented specimens failed in the DFN group before testing was completed. There was no failure in the SCN group. Comparing DFN against LISS, three instrumented specimens of the DFN group failed and four instrumented LISS cases failed prior to test completion. The reasons for failure were a complete loss of resistance of the bone implant constructs due to breakage of the shaft or dislocation of the femur condyle out of the PMMA- block.
Statistic analysis
There were no statistically significant differences comparing DFN versus SCN, DFN versus LISS and SCN versus LISS using the Wilcoxon test (Table 1).
Discussion
This study investigated the biomechanical characteristics of three fixation devices in a distal gap osteotomy model of cadaveric matched-pair femura. In contrast to previous studies, a test set-up that allows freedom of a specimen’s movement in the mounting of the testing device was used in our study. While all of the implants used in this study offered an angular-stable interlocking with at least one screw or spiral blade, the major differences in design are found in the number and in the directions and planes of the distal interlocking devices. Using the DFN, stabilization of the distal fragment is achieved by one fully threaded non angle-stable interlocking screw and an angle-stable lateral-to-medial spiral blade. Using the SCN the distal fragment is stabilized with four interlocking screws, of which three are non angle-stable and the lowermost angle-stable. All screws of the LISS plate are angle-stable fixed.
All three interlocking modalities, which were tested in this biomechanical study achieved adequate fixation of simulated comminuted supracondylar distal femur fractures. No statistically significant differences were found in axial and rotational stiffness between the intramedullary retrograde supracondylar nail (SCN), the less invasive stabilization system (LISS) and the distal femoral nail (DFN). The stability achieved with the SCN under torsional and axial loads was slightly, albeit not significantly higher than the other two fixation modalities. Wähnert et al. [27] investigated the biomechanical characteristics of four fixation devices using a comminuted intra-articular distal femur fracture model. In their study the DFN and SCN as well as the T2 femoral nail (Stryker) and the angular stable plate AxSOS (Stryker) were tested under torsional and axial loading. The angular stable plate had significantly higher torsional stiffness than the three intramedullary nails. Comparing the intramedullary nails, the SCN and the T2 femoral nail were stiffer than the DFN nail. The SCN achieved the greatest axial stiffness, followed by the DFN and the T2 femoral nail and at least the AxSOS plate. All constructs were tested in a synthetic sawbone model and two nail constructs were also compared in fresh-frozen human cadaveric femura. While the fracture model differed from that used in our study, the implants and distal interlocking mechanisms were the same. The results are comparable although we did not find any statistically differences in our biomechanical investigation. The angular stable plate tested in the study of Wähnert et al. [27] had significantly higher torsional stiffness than the three nails. In our study the angular stable LISS plate was also advantageous in torsional stiffness under the mentioned biomechanical conditions. A lot of biomechanical studies found that plating has greater torsional stiffness, whereas intramedullary implants have greater axial stiffness [4, 8, 19, 27, 31].
The axial loads applied in our study are comparable with other published studies. In their study, Zlowodski et al. [31] performed loading tests with specimens, which were proximally and distally locked in the testing machine. Fragment movement was only seen in a varus direction due to the locked position of the fragments. Marti et al. [17] used cyclic load application up to 2,200 N in a constraint proximal and distal embedded femur implant construct mounted on a uniaxial compression testing machine with a lever arm. The line of tension force in the distal femur was physiologically simulated in our study. Also the freedom of movement in the distal fragment of the specimens potted and positioned in the machine was not restricted. An ideal setting should also allow tension and torsional load application without resetting the specimens in the testing machine when changing the load mode. Gimbal mounting of the specimens and upside down positioning of the samples in the testing machine fulfilled physiological setting requirements in our study. Additionally individual differences to the intact femora were tested. In our opinion this is a biomechanical model, which refers closer to the real situation. The distal interlocking of the SCN in three directions showed in this biomechanical study to be advantageous compared to the double interlocking in one plane of the DFN. Differences, which were not significant, were especially seen in the torsional stiffness between both bone-implant constructs. Clinical relevance of torsional stiffness differences were considered less important by Michel as well as Taylor et al. [20, 26] who measured moments in one weight loaded leg using a telemetric nail. Maximal rotational moments did not exceed 7–10 Nm.
There are some limitations in the current study. The biomechanical protocol simplifies the in vivo conditions. Although not only axial compression but also torsion was tested, in vivo loading is more complex. Another limitation is the interaction of the results between torsion and tension within one sample. The reason for using this testing set-up was to mimic the in vivo conditions as well as possible. Another limitation of this matched-pair comparative study might be the small number of specimens. Due to the varying results especially in the LISS and DFN cases and due to the small number of specimens, the median values were chosen as the more reliable ones instead of the mean values. The use of sawbones would offer a more consistent biomechanical model, but this would correlate even less with the in vivo conditions than using fresh bones with variation in the bone mineral density values.
In this biomechanical study we could not find significant differences under torsional and axial loading comparing three different implants for fixation of distal femur fractures. Nevertheless, the three fixation devices differ in the mechanism of distal locking. For clinical use it is important knowing the particular qualities of each implant for choosing the most suitable one in each specific situation. For each fracture type he has to treat, the surgeon has to known the advantages and disadvantages of each implant. In case of a very distal fracture there is only a small condylar fragment left, so the use of the LISS plate may be one preferable possibility due to its several locking options still available for the small fragment. The same is true for the SCN, which offers four different locking patterns in a three-plane configuration. The DFN nail may be disadvantageous in such a very distal fracture because the locking screw may lie within the fracture gap and the only locking mechanism left would be the spiral blade.
Conclusion
All three tested interlocking modalities achieved adequate fixation of a simulated unstable supracondylar fracture of the distal femur. The interlocking modality of the SCN with three directions of distal interlocking seemed advantageous without the evidence of statistical significance.
References
Arneson TJ, Melton LJ 3rd, Lewallen DG, et al. Epidemiology of diaphyseal and distal femoral fractures in Rochester, Minnesota, 1965–1984. Clin Orthop Relat Res. 1988;234:188–94.
Bell KM, Johnstone AJ, Court-Brown CM, et al. Primary knee arthroplasty for distal femoral fractures in elderly patients. J Bone Jt Surg Br. 1992;74:400–2.
Dávid A. Distale Femurfrakturen. Orthopädie und Unfallchirurgie up2date. 2006;1:9–32.
David SM, Harrow ME, Peindl RD, et al. Comparative biomechanical analysis of supracondylar femur fracture fixation: locked intramedullary nail versus 95-degree angled plate. J Orthop Trauma. 1997;11:344–50.
Dunlop DG, Brenkel IJ. The supracondylar intramedullary nail in elderly patients with distal femoral fractures. Injury. 1999;30:475–84.
El-Kawy S, Ansara S, Moftah A, et al. Retrograde femoral nailing in elderly patients with supracondylar fracture femur; is it the answer for a clinical problem? Int Orthop. 2007;31:83–6.
Gellman RE, Paiement GD, Green HD, et al. Treatment of supracondylar femoral fractures with a retrograde intramedullary nail. Clin Orthop Relat Res. 1996;332:90–7.
Grass R, Biewener A, Rammelt S, et al. Retrograde locking nail osteosynthesis of distal femoral fractures with the distal femoral nail (DFN). Der Unfallchirurg. 2002;105:298–314.
Heiney JP, Barnett MD, Vrabec GA, et al. Distal femoral fixation: a biomechanical comparison of trigen retrograde intramedullary (i.m.) nail, dynamic condylar screw (DCS), and locking compression plate (LCP) condylar plate. J Trauma. 2009;66:443–9.
Ito K, Hungerbuhler R, Wahl D, et al. Improved intramedullary nail interlocking in osteoporotic bone. J Orthop Trauma. 2001;15:192–6.
Janzing HM, Stockman B, Van Damme G, et al. The retrograde intramedullary nail: prospective experience in patients older than sixty-five years. J Orthop Trauma. 1998;12:330–3.
Kanabar P, Kumar V, Owen PJ, et al. Less invasive stabilisation system plating for distal femoral fractures. J Orthop Surg (Hong Kong). 2007;15:299–302.
Kolmert L, Wulff K. Epidemiology and treatment of distal femoral fractures in adults. Acta Orthop Scand. 1982;53:957–62.
Kregor PJ, Perren SM. Evolution of fracture care of distal femoral fractures. Injury. 2001;32(Suppl 3):SC1–2.
Krettek C, Schandelmaier P, Tscherne H. New developments in stabilization of dia- and metaphyseal fractures of long tubular bones. Der Orthopade. 1997;26:408–21.
Kumar A, Jasani V, Butt MS. Management of distal femoral fractures in elderly patients using retrograde titanium supracondylar nails. Injury. 2000;31:169–73.
Marti A, Fankhauser C, Frenk A, et al. Biomechanical evaluation of the less invasive stabilization system for the internal fixation of distal femur fractures. J Orthop Trauma. 2001;15:482–7.
Martinet O, Cordey J, Harder Y, et al. The epidemiology of fractures of the distal femur. Injury. 2000;31(Suppl 3):C62–3.
Meyer RW, Plaxton NA, Postak PD, et al. Mechanical comparison of a distal femoral side plate and a retrograde intramedullary nail. J Orthop Trauma. 2000;14:398–404.
Michel M (1993) In vivo load on a locked intramedullary nail in the human femur. MD Thesis, University of Bern.
Pfeil J, Hasch E. Transposition osteotomy on the knee joint. Z Orthop Ihre Grenzgeb. 2005;143:R43–64.
Schandelmaier P, Partenheimer A, Koenemann B, et al. Distal femoral fractures and LISS stabilization. Injury. 2001;32(Suppl 3):SC55–63.
Schutz M, Muller M, Regazzoni P, et al. Use of the less invasive stabilization system (LISS) in patients with distal femoral (AO33) fractures: a prospective multicenter study. Arch Orthop Trauma Surg. 2005;125:102–8.
Sears BR, Ostrum RF, Litsky AS. A mechanical study of gap motion in cadaveric femurs using short and long supracondylar nails. J Orthop Trauma. 2004;18:354–60.
Seifert J, Stengel D, Matthes G, et al. Retrograde fixation of distal femoral fractures: results using a new nail system. J Orthop Trauma. 2003;17:488–95.
Taylor SJ, Walker PS. Forces and moments telemetered from two distal femoral replacements during various activities. J Biomech. 2001;34:839–48.
Wahnert D, Hoffmeier KL, Von Oldenburg G, et al. Internal fixation of type-C distal femoral fractures in osteoporotic bone. J Bone Jt Surg Am. 2010;92:1442–52.
Wick M, Muller EJ, Kutscha-Lissberg F, et al. Periprosthetic supracondylar femoral fractures: LISS or retrograde intramedullary nailing? Problems with the use of minimally invasive technique. Der Unfallchirurg. 2004;107:181–8.
Wild M, Thelen S, Spoor V, et al. Do locked compression intramedullary nails improve the biomechanical stability of distal femoral fractures? J Trauma. 2011;70:832–7.
Zlowodzki M, Bhandari M, Marek DJ, et al. Operative treatment of acute distal femur fractures: systematic review of 2 comparative studies and 45 case series (1989 to 2005). J Orthop Trauma. 2006;20:366–71.
Zlowodzki M, Williamson S, Cole PA, et al. Biomechanical evaluation of the less invasive stabilization system, angled blade plate, and retrograde intramedullary nail for the internal fixation of distal femur fractures. J Orthop Trauma. 2004;18:494–502.
Acknowledgments
Supported in part by Stryker Trauma GmbH, Kiel, Germany. The devices used in this study are approved by the FDA, International and German Medical Devices Authority.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mehling, I., Hoehle, P., Sternstein, W. et al. Nailing versus plating for comminuted fractures of the distal femur: a comparative biomechanical in vitro study of three implants. Eur J Trauma Emerg Surg 39, 139–146 (2013). https://doi.org/10.1007/s00068-012-0247-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-012-0247-1