Abstract
Purpose
Primary radiation therapy is a curative treatment option for prostate cancer. The aim of this study was to evaluate the detection of the dominant intraprostatic lesion (DIL) with magnetic resonance imaging (MRI) for radiotherapy treatment planning, the comparison with transrectal ultrasound (TRUS)-guided biopsies and the examination of the dose distribution in relation to the DIL location.
Materials and methods
In all, 54 patients with treatment planning MRI for primary radiotherapy of prostate cancer from 03/2015 to 03/2017 at the Universitätsklinikum Würzburg were identified. The localization of the DIL was based on MRI with T2- and diffusion-weighted imaging. After registration of the MR image sets within Pinnacle3 (Philips Radiation Oncology Systems, Fitchburg, WI, USA), the dose distribution was analyzed. The location of the DIL was compared to the pathology reports in a side-based manner.
Results
The DIL mean dose (Dmean) was 77.51 ± 0.77 Gy and in 50/51 cases within the tolerance range or exceeded the prescribed dose. There was a significant difference in Dmean between ventral (n = 21) and dorsal (n = 30) DIL (77.87 ± 0.67 vs. 77.26 ± 0.77 Gy; p = 0.005). MRI-guided localization showed an accuracy and sensitivity of up to 78.8% and 82.1% for inclusion of secondary lesions, respectively.
Conclusion
Up to 82.1% of histologically verified intraprostatic lesions were identified in the context of MRI-guided radiotherapy treatment planning. As expected, dorsal DIL tend to be minimally underdosed in comparison to ventral DIL. Adequate dose coverage was achieved in over 98% of patients.
Zusammenfassung
Einleitung
Die primäre perkutane Radiotherapie ist eine kurative Therapieoption für das Prostatakarzinom. Das Ziel dieser Studie war die Evaluation der Detektion der dominanten intraprostatischen Läsion (DIL) mithilfe einer Magnetresonanztomographie (MRT) zur Radiotherapieplanung, der Vergleich mit der TRUS(transrektaler Ultraschall)-gestützten Stanzbiopsie und die Untersuchung der Dosisdistribution in Abhängigkeit von der anatomischen Lage der DIL.
Material und Methoden
Ausgewertet wurden 54 Patienten mit von März 2015 bis März 2017 im Rahmen der primären Radiotherapie des Prostatakarzinoms am Universitätsklinikum Würzburg durchgeführten Bestrahlungsplanungs-MRT. Die Lokalisation der DIL erfolgte anhand der MRT mit T2- und diffusionsgewichteten Sequenzen. Nach Registrierung der MR-Bilderserien innerhalb des Pinnacle3 (Philips Radiation Oncology Systems, Fitchburg, WI, USA) Planungssystems wurde die Dosisdistribution analysiert. Die Lage der DIL wurde mit den pathologischen Stanzbiopsiebefunden seitengetrennt verglichen.
Ergebnisse
Die mittlere Dosis (Dmean) der DIL betrug 77,51 ± 0.77 Gy, wobei in 50/51 Fällen der vorgegebene Toleranzbereich eingehalten oder überschritten wurde. Im Vergleich zwischen ventraler (n = 21) und dorsaler (n = 30) Lage der DIL zeigte sich ein signifikanter Unterschied der Dmean (77,87 ± 0,67 vs. 77,26 ± 0,77 Gy; p = 0,005). Die MRT-gestützte Lokalisierung erreichte eine Genauigkeit und eine Sensitivität von bis zu 78,8 bzw. 82,1% für die Inklusion von sekundären Läsionen.
Schlussfolgerung
Bis zu 82,1% histologisch verifizierter intraprostatischer Läsionen konnten im Kontext der MRT-gestützten Radiotherapieplanung identifiziert werden. Erwartungsgemäß tendieren dorsal gelegene DIL im Vergleich mit ventral gelegenen Läsionen zu einer minimalen Unterdosierung. Eine adäquate Dosisabdeckung konnte bei mehr als 98% der Patienten erreicht werden.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer is one of the most common cancer types in Europe [1] and primary radiotherapy is an established curative therapy option [2, 3]. Intensity-modulated radiation therapy and volumetric modulated arc therapy (VMAT) based techniques allow precise and high conformal radiation of the prostate with a favorable toxicity profile [4, 5]. While whole-gland radiotherapy and resection of the prostate are standard treatment modalities for prostate cancer, focal therapy trials are justified by recent findings that a dominant intraprostatic lesion, also called index lesion, determines prognosis and disease progression [6,7,8]. Local recurrence occurs at the site of the primary tumor [9, 10] which provides the rationale for focal therapy trials in a high proportion of patients [11]. Focal therapy of the prostate has been addressed recently by a position paper of the European Association of Urology wherein prospective recording of outcomes for this form of less radical treatment is encouraged [12]. In a recent radiotherapy-specific review the authors concluded that focal brachytherapy can be applied reasonably with decreased toxicity compared to whole-gland radiotherapy especially for low-risk prostate cancer patients [13]. Furthermore, contemporary efforts are underway to escalate the radiotherapy treatment to improve tumor control and limit toxicity to neighboring organs at risk (OAR) by applying a focal radiotherapy boost to the dominant intraprostatic lesion by MRI-guided brachytherapy or MRI-guided external beam radiation [14,15,16,17]. As MRI is increasingly becoming an integral part of diagnosis and treatment of prostate cancer, the aim of this retrospective single-institution trial was to study the possibility to detect and localize the index lesion with radiotherapy treatment planning MRI, to compare the results with pretreatment prostate punch biopsies and to analyze the dose distribution based on the anatomic location of the index lesion.
Materials and methods
The planning MRI, treatment plans and charts of 54 patients treated from March 2015 until March 2017 for low to high risk prostate cancer at the Radiation Oncology Department of the Universitätsklinikum Würzburg were reviewed. Radiotherapy was delivered according to institutional standard with volumetric modulated arc therapy in 33 fractions with simultaneous integrated boost and two dose levels of 1.82 and 2.31 Gy per fraction, resulting in a prescribed PTVBoost mean dose of 76.23 Gy and in a PTV dose of 60.06 Gy (prescribed to D95). In case of pelvic lymphatic radiation the prescribed dose was 45.5 Gy (D95) with 1.82 Gy per fraction. CTVP-SV consisted of the prostate without the seminal vesicles. PTVBoost was defined by a 5 mm margin around the CTVP-SV with avoidance of the rectum. The PTV was created by a 10 mm margin around the prostate including the seminal vesicles (CTVP+SV) in all but the dorsal direction, where a 7 mm margin was used.
All patients received pretherapeutic treatment planning MRI using a Siemens MAGNETOM Prisma with 3 T without an endorectal coil. MRI consisted of a native T2-weighted sequence, diffusion-weighted imaging (DWI; b‑value 800) with apparent diffusion coefficient (ADC) mapping and a contrast-enhanced T1-weighted sequence. Both T2-weighted sequence and ADC map were fused onto the radiotherapy treatment computed tomography (CT) within the Pinnacle3 (Philips Radiation Oncology Systems, Fitchburg, WI, USA) planning system which allowed the contouring of the DIL by one radiation oncologist trained in multiparametric MRI (mpMRI) of the prostate and the analysis of the dose distribution (Fig. 1).
The index lesion was defined as the lesion with the highest risk features based on the Prostate Imaging Reporting and Data System (PI-RADS) version 2 criteria [18]. If two similar lesions were present, the largest lesion was chosen. All patients had pathologic confirmed prostate cancer with diagnosis by TRUS-guided biopsy and in some patients additionally by transurethral prostate resection. The location of the DIL was documented by means of a sector map of the prostate (Fig. 2) and correlated with the pathology reports of the punch biopsies which provided the corresponding side of the cores and in 33 cases detailed location data. Statistical analysis was conducted with IBM SPSS v. 24.0 (IBM Corp., Armonk, NY, USA). An unpaired t‑test was used for the dose difference analysis between ventral and dorsal index lesions. Changes in accuracy were analyzed by applying a McNemar test. Differences were considered statistically significant in case of p < 0.05. For the mean dose analysis a 95% confidence interval (CI) of the difference in mean dose was calculated. Mean dose values are reported with standard deviation.
Sector map of the prostate, modified after Weinreb JC et al. [18]. AFS/AS anterior fibromuscular stroma, CZ central zone, PZ peripheral zone, TZ transition zone, US urethral sphincter. a: anterior, p: posterior, m: medial, l: lateral
Results
Clinical characteristics
The reviewed 54 men had a median age of 74 years (range 54–81 years). The PSA value at first diagnosis (iPSA) was in 39 patients below 10 ng/ml, in 8 patients between 10–20 ng/ml and in 7 patients >20 ng/ml. Regarding the Gleason score, 11 patients had a score of 6, 23 patients a score of 7 and 20 patients had a score of 8 to 10. According to the D’Amico risk classification 10 patients had low-risk prostate cancer, 20 patients an intermediate-risk prostate cancer and 24 patients high-risk prostate cancer. All patients were diagnosed by pretreatment TRUS-guided biopsy. A total of 11 patients had prior transurethral prostate resection. Clinical characteristics are summarized in Table 1.
Location data and pathology analysis
In 10 out of 54 patients the location of the DIL was on the left side, in 34 patients on the right side and in 10 patients on both sides of the prostate. In 32 out of 54 patients the location of the DIL involved the peripheral zone, in 18 patients the transition zone, in 5 patients the anterior fibromuscular stroma, in 6 patients the central zone and in 3 patients the seminal vesicles. In 44 out of 54 patients the middle layer, in 32 patients the basis and in 23 patients the apex of the prostate was involved. Location data are summarized in Table 2.
Overall 82 intraprostatic lesions could be identified: 54 index lesions and 28 secondary lesions. The median volume of the index lesion was 1.66 cm3 (range 0.5–26.1 cm3). MRI-guided localization of the index lesion reached an accuracy of 68.3%, sensitivity of 66.7% and specificity of 75.0% in a side-based comparison with the TRUS-guided biopsy reports (n = 52; two patients not eligible because of lacking data). By inclusion of secondary lesions the accuracy could be significantly improved to 78.8% (McNemar test, p = 0.007, two-sided) with a sensitivity of 82.1% and a specificity of 65.0%. In a subgroup of 33 patients the pathology reports of the punch biopsy offered sextant location data which were compared to the prostate sector map (Fig. 2). In this subgroup accuracy was 66.2%, sensitivity 51.4% and specificity 82.8% for the index lesion. Including secondary lesions sextant comparison reached an accuracy of 67.2%, a sensitivity of 59.0% and a specificity of 76.3%.
Dose distribution analysis
In all, 41 out of 54 patients received VMAT-based radiotherapy of the prostate only and 13 patients received additional treatment of the pelvic lymph nodes. In case of low-risk prostate cancer reduction of delivered fractions from 33 to 32 was optional, resulting in 2 patients receiving a PTVBoost dose of 73.92 Gy (Dmean). One patient with lymph node metastasis received 30 fractions, resulting in a PTVBoost dose of 69.3 Gy (Dmean) in addition to antiandrogen treatment.
These three above described patients with an alternative fractionation were excluded from the subsequent analysis of the index lesion dose values because our aim was to detect deviances from the planned PTVBoost Dmean of 76.23 Gy in institutional standard fractionation. The mean Dmean of the DIL was 77.51 ± 0.77 Gy. Mean minimum dose was 74.55 ± 2.67 Gy and mean maximum dose was 79.12 ± 0.81 Gy. In 50 out of 51 patients Dmean DIL was within tolerance range of ±1% or above the prescribed dose. In most patients (39 out of 51) Dmean DIL was in the range of +1 to +3%. In 2 patients Dmean DIL was in the range of +3 to +5% and in 1 patient Dmean DIL was in the range of −1 to −2% (−1.4%).
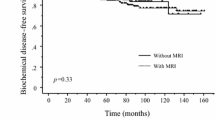
There was a significant difference in mean Dmean between index lesions located in the ventral part of the prostate (peripheral zone anterior, transition zone anterior/posterior, anterior fibromuscular stroma; n = 21) and in the dorsal part (peripheral zone posterior lateral/medial, central zone, seminal vesicles; n = 30) with 77.87 ± 0.67 Gy versus 77.26 ± 0.77 Gy respectively (unpaired t‑test; df = 49, p = 0.005, two-sided; 95% confidence interval [CI] of difference = 0.2–1.03 Gy; Fig. 3).
Discussion
MRI offers superior tissue contrast compared to CT which has led to an increasing use of mpMRI in the management of prostate cancer and in radiation oncology [19,20,21,22]. The localization and detection of intraprostatic lesions by MRI allows advanced treatment techniques with focal dose escalation and simultaneous OAR protection which was shown recently by the FLAME trial [14, 23]. As whole-gland radiotherapy is still the current standard of care, we studied the possibility to localize the index lesion with treatment planning MRI and to evaluate the dose coverage of the index lesion as clinically important target for avoidance of cancer progression [6].
There are many studies which show the feasibility and sensitivity of diagnostic mpMRI-based detection of prostate cancer lesions with reference to whole-mount pathology [24,25,26]. In patients with primary radiotherapy treatment whole-mount pathology is not routinely available. Therefore, we correlated the treatment MRI with TRUS-guided biopsy reports as ground truth although TRUS-guided biopsy itself may miss significant proportions of high-grade prostate cancer foci [27] with a sensitivity level of around 50% [28]. On the other hand, mpMRI seems to outperform TRUS-guided biopsy for high-risk prostate cancer detection but may miss lower grade foci [28,29,30]: The PROMIS trial reported significant better sensitivity of mpMRI versus TRUS-guided biopsy (93% vs. 48%, p < 0.0001) for clinically significant cancer which was defined as Gleason score ≥ 4 + 3 or ≥6 mm of any cancer [28]. Furthermore, the recently published results of the PRECISION trial suggest the superiority of MRI-targeted biopsy over TRUS-guided biopsy [31]. Pal et al. confirmed the high sensitivity of mpMRI, but also reported that the sensitivity is lowered to 72% if International Society of Urological Pathology (ISUP) grade 2 cancer is included in the analysis [30]. Pal et al. concluded that reliance on mpMRI could deny patients with ISUP grade ≤ 3 potentially beneficial treatment [30].
In our study MRI and TRUS-biopsy derived location of the index lesion was matched in 68.3% (side-based assessment, n = 52) with an increase in accuracy by inclusion of secondary lesions to 78.8% which could be possibly explained by an overdetection of clinically insignificant cancer by TRUS-guided biopsy [28]. In the subgroup with sextant biopsy-based location data accuracy was only 67.2% with inclusion of secondary lesions, but the patient number was low (n = 33) and correlation and registration of MRI and pathology proves to be challenging, even in whole-mount pathology studies [32] and even by usage of the PI-RADS version 2 sector map for location description [33]. Sensitivity was decreased from 82.1 to 59.0% for the detection of the index lesion inclusive secondary lesions due to the fact that the sextant biopsy data are based on triple the amount of prostate segments.
There was a significant, but small difference in planned mean dose for dorsally located lesions compared to ventral locations with a mean Dmean of 77.26 ± 0.77 Gy versus 77.87 ± 0.67 Gy (p = 0.005). An explanation for this dose difference is the observance of OAR constraints especially for the rectum with the aim of dose reduction for the dorsal half respectively third of the rectum. In the definition of PTVBoost the rectum was routinely excluded which led to a dorsal dose gradient. Nevertheless, mean planned Dmean exceeded the prescribed dose of 76.23 Gy even for dorsal index lesions and each plan was critically reviewed before application for target volume coverage and simultaneous OAR protection. In our study only one out of 54 cases showed a slight underdosage of more than 1% in DIL mean dose, due to the location of the index lesion adjacent to the rectal wall. Thus, in more than 98% of all patients the planned dose coverage of the index lesion was adequate.
There are limitations to this study: We conducted a retrospective review of the histologic biopsy reports, as such no prospective confirming biopsy or whole-mount pathology were available. Implementation of automated segmentation [34,35,36] and deformable image registration [37] could improve accuracy of the MRI-histology comparison and minimize uncertainty arising from rigid image registration and from observer dependent variability in delineation [38, 39]. Our treatment planning MRI did not utilize dynamic contrast-enhanced imaging but a T1-weighted post contrast sequence for radiotherapy treatment planning with emphasis on the T2-weighted and DWI sequences for cancer delineation. A meta-analysis by Chen et al. concludes that dynamic contrast-enhanced imaging plays a supplementary, but still only confirmatory role in prostate cancer detection [40]. Although high diagnostic performance is desirable, we adopted a more practical, time and cost effective approach. Recently, DWI-sequences with higher b‑values have been proposed for lesion detection to increase sensitivity [41], but have not been implemented yet in this study collective. Additionally, we showed the planned radiotherapy dose, but for applied dose intra- [42,43,44] and interfraction [45,46,47] organ movement has to be considered. Adaptive radiotherapy techniques with compensation for movement errors as well as high-quality treatment planning as shown in this study form the basis of precision radiotherapy for prostate cancer [44].
Conclusion
Our data show that contemporary VMAT-based radiotherapy treatment planning allowed adequate dose coverage of the index lesion in more than 98% of all patients. Special attention must be given to index lesions located adjacent to the rectal wall where OAR constraints require careful treatment planning and contemporary image-guidance systems are of paramount importance. Integration of MRI in radiation oncology allows the detection of these lesions and may guide treatment planning concerning dose coverage. In the future it may form the basis for further trials of mpMRI-based focal radiotherapy. A diagnostic accuracy in the range of only 70% however challenges the concept of focal treatment only.
References
Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, Forman D, Bray F (2013) Dosimetric implications of inter- and intrafractional prostate positioning errors during tomotherapy: comparison of gold marker-based registrations with native MVCT. Eur J Cancer 49(6):1374–1403. https://doi.org/10.1016/j.ejca.2012.12.027
Hamdy FC, Donovan JL, Lane JA, Mason M, Metcalfe C, Holding P, Davis M, Peters TJ, Turner EL, Martin RM, Oxley J, Robinson M, Staffurth J, Walsh E, Bollina P, Catto J, Doble A, Doherty A, Gillatt D, Kockelbergh R, Kynaston H, Paul A, Powell P, Prescott S, Rosario DJ, Rowe E, Neal DE (2016) 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med 375(15):1415–1424. https://doi.org/10.1056/NEJMoa1606220
Kishan AU, Cook RR, Ciezki JP, Ross AE, Pomerantz MM, Nguyen PL, Shaikh T, Tran PT, Sandler KA, Stock RG, Merrick GS, Demanes DJ, Spratt DE, Abu-Isa EI, Wedde TB, Lilleby W, Krauss DJ, Shaw GK, Alam R, Reddy CA, Stephenson AJ, Klein EA, Song DY, Tosoian JJ, Hegde JV, Yoo SM, Fiano R, D’Amico AV, Nickols NG, Aronson WJ, Sadeghi A, Greco S, Deville C, McNutt T, DeWeese TL, Reiter RE, Said JW, Steinberg ML, Horwitz EM, Kupelian PA, King CR (2018) Radical prostatectomy, external beam radiotherapy, or external beam radiotherapy with Brachytherapy boost and disease progression and mortality in patients with Gleason score 9–10 prostate cancer. JAMA 319(9):896–905. https://doi.org/10.1001/jama.2018.0587
Delobel JB, Gnep K, Ospina JD, Beckendorf V, Chira C, Zhu J, Bossi A, Messai T, Acosta O, Castelli J, de Crevoisier R (2017) Nomogram to predict rectal toxicity following prostate cancer radiotherapy. PLoS ONE 12(6):e179845. https://doi.org/10.1371/journal.pone.0179845
Guckenberger M, Lawrenz I, Flentje M (2014) Moderately hypofractionated radiotherapy for localized prostate cancer: long-term outcome using IMRT and volumetric IGRT. Strahlenther Onkol 190(1):48–53. https://doi.org/10.1007/s00066-013-0443-x
Ahmed HU (2009) The index lesion and the origin of prostate cancer. N Engl J Med 361(17):1704–1706. https://doi.org/10.1056/NEJMcibr0905562
Wise AM, Stamey TA, McNeal JE, Clayton JL (2002) Morphologic and clinical significance of multifocal prostate cancers in radical prostatectomy specimens. Urology 60(2):264–269
Noguchi M, Stamey TA, McNeal JE, Nolley R (2003) Prognostic factors for multifocal prostate cancer in radical prostatectomy specimens: lack of significance of secondary cancers. J Urol 170(2 Pt 1):459–463. https://doi.org/10.1097/01.ju.0000070928.49986.04
Pucar D, Hricak H, Shukla-Dave A, Kuroiwa K, Drobnjak M, Eastham J, Scardino PT, Zelefsky MJ (2007) Clinically significant prostate cancer local recurrence after radiation therapy occurs at the site of primary tumor: magnetic resonance imaging and step-section pathology evidence. Int J Radiat Oncol Biol Phys 69(1):62–69. https://doi.org/10.1016/j.ijrobp.2007.03.065
Cellini N, Morganti AG, Mattiucci GC, Valentini V, Leone M, Luzi S, Manfredi R, Dinapoli N, Digesu C, Smaniotto D (2002) Analysis of intraprostatic failures in patients treated with hormonal therapy and radiotherapy: implications for conformal therapy planning. Int J Radiat Oncol Biol Phys 53(3):595–599
Karavitakis M, Winkler M, Abel P, Livni N, Beckley I, Ahmed HU (2011) Histological characteristics of the index lesion in whole-mount radical prostatectomy specimens: implications for focal therapy. Prostate Cancer Prostatic Dis 14(1):46–52. https://doi.org/10.1038/pcan.2010.16
van der Poel HG, van den Bergh RCN, Briers E, Cornford P, Govorov A, Henry AM, Lam TB, Mason MD, Rouviere O, De Santis M, Willemse PM, van Poppel H, Mottet N (2018) Focal therapy in primary localised prostate cancer: the European Association of Urology position in 2018. Eur Urol. https://doi.org/10.1016/j.eururo.2018.01.001
Peach MS, Trifiletti DM, Libby B (2016) Systematic review of focal prostate brachytherapy and the future implementation of image-guided prostate HDR brachytherapy using MR-ultrasound fusion. Prostate Cancer. https://doi.org/10.1155/2016/4754031
Monninkhof EM, van Loon JWL, van Vulpen M, Kerkmeijer LGW, Pos FJ, Haustermans K, van den Bergh L, Isebaert S, McColl GM, Smeenk JR, Noteboom J, Walraven I, Peeters PHM, van der Heide UA (2018) Standard whole prostate gland radiotherapy with and without lesion boost in prostate cancer: toxicity in the FLAME randomized controlled trial. Radiother Oncol. https://doi.org/10.1016/j.radonc.2017.12.022
von Eyben FE, Kiljunen T, Kangasmaki A, Kairemo K, von Eyben R, Joensuu T (2016) Radiotherapy boost for the dominant intraprostatic cancer lesion-a systematic review and meta-analysis. Clin Genitourin Cancer 14(3):189–197. https://doi.org/10.1016/j.clgc.2015.12.005
Sundahl N, De Meerleer G, Villeirs G, Ost P, De Neve W, Lumen N, De Visschere P, Van Eijkeren M, Fonteyne V (2016) Combining high dose external beam radiotherapy with a simultaneous integrated boost to the dominant intraprostatic lesion: analysis of genito-urinary and rectal toxicity. Radiother Oncol 119(3):398–404. https://doi.org/10.1016/j.radonc.2016.04.031
Timon G, Ciardo D, Bazani A, Garioni M, Maestri D, De Lorenzo D, Pansini F, Cambria R, Rondi E, Cattani F, Marvaso G, Zerini D, Vischioni B, Ciocca M, Russo S, Molinelli S, Golino F, Scroffi V, Rojas DP, Fodor C, Petralia G, Santoro L, De Cobelli O, Orecchia R, Jereczek-Fossa BA (2016) Rationale and protocol of AIRC IG-13218, short-term radiotherapy for early prostate cancer with concomitant boost to the dominant lesion. Tumori 102(5):536–540. https://doi.org/10.5301/tj.5000547
Weinreb JC, Barentsz JO, Choyke PL, Cornud F, Haider MA, Macura KJ, Margolis D, Schnall MD, Shtern F, Tempany CM, Thoeny HC, Verma S (2016) PI-RADS prostate imaging—reporting and data system: 2015, version 2. Eur Urol 69(1):16–40. https://doi.org/10.1016/j.eururo.2015.08.052
Oberlin DT, Casalino DD, Miller FH, Meeks JJ (2017) Dramatic increase in the utilization of multiparametric magnetic resonance imaging for detection and management of prostate cancer. Abdom Radiol (NY) 42(4):1255–1258. https://doi.org/10.1007/s00261-016-0975-5
McPartlin AJ, Li XA, Kershaw LE, Heide U, Kerkmeijer L, Lawton C, Mahmood U, Pos F, van As N, van Herk M, Vesprini D, van der Voort van Zyp J, Tree A, Choudhury A (2016) MRI-guided prostate adaptive radiotherapy—a systematic review. Radiother Oncol 119(3):371–380. https://doi.org/10.1016/j.radonc.2016.04.014
Combs SE, Nusslin F, Wilkens JJ (2016) Individualized radiotherapy by combining high-end irradiation and magnetic resonance imaging. Strahlenther Onkol 192(4):209–215. https://doi.org/10.1007/s00066-016-0944-5
Bostel T, Pfaffenberger A, Delorme S, Dreher C, Echner G, Haering P, Lang C, Splinter M, Laun F, Muller M, Jakel O, Debus J, Huber PE, Sterzing F, Nicolay NH (2018) Prospective feasibility analysis of a novel off-line approach for MR-guided radiotherapy. Strahlenther Onkol 194(5):425–434. https://doi.org/10.1007/s00066-017-1258-y
Lips IM, van der Heide UA, Haustermans K, van Lin EN, Pos F, Franken SP, Kotte AN, van Gils CH, van Vulpen M (2011) Single blind randomized phase III trial to investigate the benefit of a focal lesion ablative microboost in prostate cancer (FLAME-trial): study protocol for a randomized controlled trial. Trials 12:255. https://doi.org/10.1186/1745-6215-12-255
Isebaert S, Van den Bergh L, Haustermans K, Joniau S, Lerut E, De Wever L, De Keyzer F, Budiharto T, Slagmolen P, Van Poppel H, Oyen R (2013) Multiparametric MRI for prostate cancer localization in correlation to whole-mount histopathology. J Magn Reson Imaging 37(6):1392–1401. https://doi.org/10.1002/jmri.23938
Chabanova E, Balslev I, Logager V, Hansen A, Jakobsen H, Kromann-Andersen B, Norgaard N, Horn T, Thomsen HS (2011) Prostate cancer: 1.5 T endo-coil dynamic contrast-enhanced MRI and MR spectroscopy—correlation with prostate biopsy and prostatectomy histopathological data. Eur J Radiol 80(2):292–296. https://doi.org/10.1016/j.ejrad.2010.07.004
Rud E, Klotz D, Rennesund K, Baco E, Berge V, Lien D, Svindland A, Lundeby E, Berg RE, Eri LM, Eggesbo HB (2014) Detection of the index tumour and tumour volume in prostate cancer using T2-weighted and diffusion-weighted magnetic resonance imaging (MRI) alone. BJU Int 114(6b):E32–E42. https://doi.org/10.1111/bju.12637
Seisen T, Roudot-Thoraval F, Bosset PO, Beaugerie A, Allory Y, Vordos D, Abbou CC, De La Taille A, Salomon L (2015) Predicting the risk of harboring high-grade disease for patients diagnosed with prostate cancer scored as Gleason ≤6 on biopsy cores. World J Urol 33(6):787–792. https://doi.org/10.1007/s00345-014-1348-8
Ahmed HU, El-Shater Bosaily A, Brown LC, Gabe R, Kaplan R, Parmar MK, Collaco-Moraes Y, Ward K, Hindley RG, Freeman A, Kirkham AP, Oldroyd R, Parker C, Emberton M (2017) Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 389(10071):815–822. https://doi.org/10.1016/s0140-6736(16)32401-1
Pokorny MR, de Rooij M, Duncan E, Schroder FH, Parkinson R, Barentsz JO, Thompson LC (2014) Prospective study of diagnostic accuracy comparing prostate cancer detection by transrectal ultrasound-guided biopsy versus magnetic resonance (MR) imaging with subsequent MR-guided biopsy in men without previous prostate biopsies. Eur Urol 66(1):22–29. https://doi.org/10.1016/j.eururo.2014.03.002
Pal RP, Ahmad R, Trecartan S, Voss J, Ahmed S, Bazo A, Lloyd J, Walton TJ (2018) A single-centre evaluation of the diagnostic accuracy of multiparametric MRI against transperineal prostate mapping biopsy: an analysis of men with bengin histology and insignificant cancer following TRUS biopsy. J Urol. https://doi.org/10.1016/j.juro.2018.02.072
Kasivisvanathan V, Rannikko AS, Borghi M, Panebianco V, Mynderse LA, Vaarala MH, Briganti A, Budaus L, Hellawell G, Hindley RG, Roobol MJ, Eggener S, Ghei M, Villers A, Bladou F, Villeirs GM, Virdi J, Boxler S, Robert G, Singh PB, Venderink W, Hadaschik BA, Ruffion A, Hu JC, Margolis D, Crouzet S, Klotz L, Taneja SS, Pinto P, Gill I, Allen C, Giganti F, Freeman A, Morris S, Punwani S, Williams NR, Brew-Graves C, Deeks J, Takwoingi Y, Emberton M, Moore CM (2018) MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med. https://doi.org/10.1056/NEJMoa1801993
Park H, Piert MR, Khan A, Shah R, Hussain H, Siddiqui J, Chenevert TL, Meyer CR (2008) Registration methodology for histological sections and in vivo imaging of human prostate. Acad Radiol 15(8):1027–1039. https://doi.org/10.1016/j.acra.2008.01.022
Greer MD, Shih JH, Barrett T, Bednarova S, Kabakus I, Law YM, Shebel H, Merino MJ, Wood BJ, Pinto PA, Choyke PL, Turkbey B (2018) All over the map: an interobserver agreement study of tumor location based on the PI-RADSv2 sector map. J Magn Reson Imaging. https://doi.org/10.1002/jmri.25948
Shiradkar R, Podder TK, Algohary A, Viswanath S, Ellis RJ, Madabhushi A (2016) Radiomics based targeted radiotherapy planning (Rad-TRaP): a computational framework for prostate cancer treatment planning with MRI. Radiat Oncol 11(1):148. https://doi.org/10.1186/s13014-016-0718-3
Parra NA, Pollack A, Chinea FM, Abramowitz MC, Marples B, Munera F, Castillo R, Kryvenko ON, Punnen S, Stoyanova R (2017) Automatic detection and quantitative DCE-MRI scoring of prostate cancer aggressiveness. Front Oncol 7:259. https://doi.org/10.3389/fonc.2017.00259
Peeken JC, Nusslin F, Combs SE (2017) “Radio-oncomics”: the potential of radiomics in radiation oncology. Strahlenther Onkol 193(10):767–779. https://doi.org/10.1007/s00066-017-1175-0
Ciardo D, Jereczek-Fossa BA, Petralia G, Timon G, Zerini D, Cambria R, Rondi E, Cattani F, Bazani A, Ricotti R, Garioni M, Maestri D, Marvaso G, Romanelli P, Riboldi M, Baroni G, Orecchia R (2017) Multimodal image registration for the identification of dominant intraprostatic lesion in high-precision radiotherapy treatments. Br J Radiol 90(1079):20170021. https://doi.org/10.1259/bjr.20170021
Harvey H, Orton MR, Morgan VA, Parker C, Dearnaley D, Fisher C, deSouza NM (2017) Volumetry of the dominant intraprostatic tumour lesion: intersequence and interobserver differences on multiparametric MRI. Br J Radiol 90(1071):20160416. https://doi.org/10.1259/bjr.20160416
Steenbergen P, Haustermans K, Lerut E, Oyen R, De Wever L, Van den Bergh L, Kerkmeijer LG, Pameijer FA, Veldhuis WB, van der Voort van Zyp JR, Pos FJ, Heijmink SW, Kalisvaart R, Teertstra HJ, Dinh CV, Ghobadi G, van der Heide UA (2015) Prostate tumor delineation using multiparametric magnetic resonance imaging: inter-observer variability and pathology validation. Radiother Oncol 115(2):186–190. https://doi.org/10.1016/j.radonc.2015.04.012
Chen Z, Zheng Y, Ji G, Liu X, Li P, Cai L, Guo Y, Yang J (2017) Accuracy of dynamic contrast-enhanced magnetic resonance imaging in the diagnosis of prostate cancer: systematic review and meta-analysis. Oncotarget 8(44):77975–77989. https://doi.org/10.18632/oncotarget.20316
Woo S, Suh CH, Kim SY, Cho JY, Kim SH (2018) Head-to-head comparison between high- and standard-b-value DWI for detecting prostate cancer: a systematic review and meta-analysis. AJR Am J Roentgenol 210(1):91–100. https://doi.org/10.2214/ajr.17.18480
Boda-Heggemann J, Kohler FM, Wertz H, Ehmann M, Hermann B, Riesenacker N, Kupper B, Lohr F, Wenz F (2008) Intrafraction motion of the prostate during an IMRT session: a fiducial-based 3D measurement with Cone-beam CT. Radiat Oncol 3:37. https://doi.org/10.1186/1748-717x-3-37
Badakhshi H, Wust P, Budach V, Graf R (2013) Image-guided radiotherapy with implanted markers and kilovoltage imaging and 6‑dimensional position corrections for intrafractional motion of the prostate. Anticancer Res 33(9):4117–4121
Wilbert J, Baier K, Hermann C, Flentje M, Guckenberger M (2013) Accuracy of real-time couch tracking during 3‑dimensional conformal radiation therapy, intensity modulated radiation therapy, and volumetric modulated arc therapy for prostate cancer. Int J Radiat Oncol Biol Phys 85(1):237–242. https://doi.org/10.1016/j.ijrobp.2012.01.095
Haekal M, Arimura H, Hirose TA, Shibayama Y, Ohga S, Fukunaga J, Umezu Y, Honda H, Sasaki T (2018) Computational analysis of interfractional anisotropic shape variations of the rectum in prostate cancer radiation therapy. Phys Med 46:168–179. https://doi.org/10.1016/j.ejmp.2017.12.019
Shibayama Y, Arimura H, Hirose TA, Nakamoto T, Sasaki T, Ohga S, Matsushita N, Umezu Y, Nakamura Y, Honda H (2017) Investigation of interfractional shape variations based on statistical point distribution model for prostate cancer radiation therapy. Med Phys 44(5):1837–1845. https://doi.org/10.1002/mp.12217
Wust P, Joswig M, Graf R, Bohmer D, Beck M, Barelkowski T, Budach V, Ghadjar P (2017) Dosimetric implications of inter- and intrafractional prostate positioning errors during tomotherapy: comparison of gold marker-based registrations with native MVCT. Strahlenther Onkol 193(9):700–706. https://doi.org/10.1007/s00066-017-1141-x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Tamihardja, M. Zenk and M. Flentje declare that they have no competing interests.
Ethical standards
This article does not contain any studies with animals performed by any of the authors. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all patients before treatment. An additional individual consent for this analysis was not needed.
Rights and permissions
About this article
Cite this article
Tamihardja, J., Zenk, M. & Flentje, M. MRI-guided localization of the dominant intraprostatic lesion and dose analysis of volumetric modulated arc therapy planning for prostate cancer. Strahlenther Onkol 195, 145–152 (2019). https://doi.org/10.1007/s00066-018-1364-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-018-1364-5