Abstract
Purpose
Socioeconomic aspects play an important role in health care. Patients with locally advanced head and neck cancer (LAHNC) experience detrimental effects on their quality of life (QoL). This prospective study examines QoL differences between patients with different socioeconomic status (SES) after intensity-modulated radiation therapy (IMRT).
Patients and methods
In all, 161 patients were questioned at the end of IMRT and at 12 and 24 months follow-up using the questionnaires of the European Organization for Research and Treatment of Cancer (EORTC) QLQ-30 and QLQ-HN35. Patients’ QoL 2 years after IMRT was compared to a population reference sample and QoL of patients from lower, middle, and higher social class 2 years after IMRT was analyzed by ANCOVA using baseline QoL (end of radiation treatment) as a covariate.
Results
Patients with high SES report worse QoL at the end of IMRT in the domains global health status (−15.2; p = 0.005), role function (−23.8; p = 0.002), and social function (−19.4; p = 0.023) compared to patients with middle and low SES. QoL improved during the first 12 and 24 months. However, 2 years after IMRT, middle and low SES patients report lower QoL in the domains global health status, physical function, and role function, and report a higher general (fatigue, pain, dyspnea) and head and neck cancer-specific symptom burden (pain, swallowing, senses, speech, social eating, opening mouth, and felt ill) than patients with high SES.
Conclusion
After IMRT for LAHNC, patients with high SES report worse QoL compared to patients with middle or low SES. There is a marked improvement within the first 24 months in many domains. However, the magnitude of improvement in patients with middle or low SES is significantly smaller compared to patients with high SES.
Zusammenfassung
Zielsetzung
Sozioökonomische Aspekte spielen bei vielen Erkrankungen und deren Therapie eine nicht zu unterschätzende Rolle, so auch bei Patienten mit lokal fortgeschrittenen Kopf-Hals-Tumoren (LFKHT). Diese Patienten erfahren durch Erkrankung und Therapie Einbußen in ihrer Lebensqualität (QoL). Diese prospektive Studie untersucht den Zusammenhang zwischen QoL und sozioökonomischem Status (SES) bei LFKHT-Patienten nach intensitätsmodulierter Strahlentherapie (IMRT).
Patienten und Methoden
Am Ende der Bestrahlung, nach 6–8 Wochen sowie 6, 12, 18 und 24 Monate nach Abschluss der IMRT haben 161 Patienten die standardisierten Fragebögen der EORTC (European Organization for Research and Treatment of Cancer) QLQ-C30 und QLQ-HN35 ausgefüllt. Nach 2 Jahren wurde die QoL der Gesamtpopulation mit der einer Referenzpopulation verglichen und der Zusammenhang zwischen QoL am Ende der IMRT und SES analysiert (ANCOVA).
Ergebnisse
Patienten der Gruppe mit hohem SES hatten eine deutlich schlechtere QoL in den Domänen globaler Gesundheitsstaus (−15,2; p = 0,005), Rollenfunktion (−23,8; p = 0,002) und soziale Funktion (−19,4; p = 0,023) verglichen mit Patienten der mittleren und niedrigen SES-Gruppen. Nach 12 und 24 Monaten verbesserte sich die QoL in vielen Domänen. Patienten mit mittlerem und niedrigem SES berichten 2 Jahre nach IMRT eine schlechtere QoL in den Domänen globaler Gesundheitszustand, körperliche Funktion und Rollenfunktion und eine höhere Symptomlast (Fatigue, Schmerzen, Dyspnoe). Im spezifischen Kopf-Hals-Tumor-Modul berichteten Patienten mit hohem SES signifikant weniger häufig Symptome im Vergleich zu Patienten mit mittlerem oder niedrigem SES (Schmerzen, Schlucken, Sinne, Sprechen, Essen in Gesellschaft, Mundöffnung und Krankheitsgefühl).
Zusammenfassung
Am Ende der Radio(chemo)therapie für LFKHT schätzen Patienten mit höherem SES ihre QoL schlechter ein als Patienten mit mittlerem oder niedrigem SES. Nach 24 Monaten zeigt sich eine Verbesserung der QoL in vielen Domänen, wobei diese bei niedrigem SES deutlich weniger ausgeprägt ist als bei hohem SES.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past decade, quality of life (QoL) has become increasingly important in cancer care. In patients with locally advanced head and neck cancer, the tumor itself as well as the treatment can have a profound impact on QoL [1,2,3]. Therefore, long-term QoL has become an important endpoint alongside the classical survival endpoints [4, 5]. Patients with a low socioeconomic status (SES) have an increased risk of not only developing head and neck cancer, but also to be diagnosed in a more advanced stage of the disease and to have a worse survival compared to patients with a high SES [6,7,8]. The SES index includes education, income, occupation, and cost of living [9].
It is an ethical challenge to balance the consequences of societal and social deprivation on one side and to manage the economic burden caused by malignant diseases on the other [10]. Mackenbach et al. found that economic deprivation and it is consequential health-related impact causes 700,000 deaths per year and 33 million newly diagnosed diseases per year in the European Union [11]. This impact on disease incidence accounts for approximately 20% of overall health care costs and reduced national productivity. However, it is not appropriate to consider QoL only in economic terms [11].
Head and neck cancer is the sixth most common cancer worldwide, including in Germany [12]. It is prudent to consider and understand sociodemographic variables as well as health aspects, including QoL, in this patient population. Knowledge and understanding of the imbalances in health care in Germany is of utmost importance and societal relevance, and has become an important research field in Germany during recent years [10].
Data on QoL and SES in patients with locally advanced head and neck cancer are scarce. Short and Mallonee et al. looked in the US at QoL and differences in household income for various malignancies using the Functional Assessment of Cancer Therapy-General (FACT-G) and the SF-12 questionnaires and found that cancer patients with higher income not only have a better survival but also have a better QoL [13].
It has been reported that individuals with high SES are most likely more conscious about health and preventive measures. This is of importance in populations of low SES, in which the incidence of head and neck cancer is not only higher but people are much less conscious about this disease [8, 14, 15].
The aim of the present study was to analyze QoL in patients with locally advanced head and neck cancer (LAHNC) as a function of their SES, and to see if it differs up to 24 months after completion of intensity-modulated radiation therapy (IMRT) for LAHNC.
Patients and methods
Study design and sampling
Before adjuvant radio(chemo)therapy (R(C)T), eligible patients were enrolled into a prospective study by the radiation oncologist. Eligible patients with LAHNC had to have M0 disease, squamous cell histology, no contraindication to R(C)T, and be able to complete the QoL questionnaires and be compliant to follow-up appointments. QoL was measured at the end of IMRT and at 12 and 24 months follow-up. Questionnaires were self-completed in the physician’s office at the time of the visit.
The IMRT dose prescription followed the recommendations of the ICRU (International Commission on Radiation Units and Measurement) report, 83 [16]. In the adjuvant setting, patients received a total dose of 60–66 Gy at 2 Gy per fraction. If indicated, risk-adapted concurrent RCT was applied with cisplatin weekly with 30–40 mg/m2 or 100 mg/m2 every 3 weeks. In the primary setting, a total dose of 70 Gy was given with 5 fractions per week at 2 Gy per fraction.
Approval was obtained from the local ethics committee. All patients provided written informed consent.
Sociodemographic variables
At the beginning of RT, patients reported on age, marital status, education level, occupation, and monthly household net income. An adapted version of a composite social class indicator based on primary and secondary education, type of occupation and monthly household net income was calculated to assess social class [17]. Based on this index, patients can be classified into upper, middle, or lower social class.
Disease- and treatment-related variables
Disease- and treatment-related variables such as tumor diagnosis, tumor stage, and type of treatment were assessed and documented by the treating physicians.
Quality of life
Cancer-related quality of life was measured by applying the German version of the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30 (EORTC) QLQ-C30 [18]. The core module consists of 30 items from which a global quality of life score can be calculated as well as five functioning scales (emotional, physical, cognitive, social, and role functioning), three multi-item scales for cancer-related symptoms (fatigue, nausea and vomiting, pain) and six single-item scales for cancer-related symptoms (dyspnea, insomnia, appetite loss, constipation, diarrhea, financial difficulties).
Specific cancer-related QoL was measured with the EORTC Head and Neck Module H&N35 [19]. From the 35 items of the module, seven head and neck-specific multi-item scales can be derived (pain, swallowing, senses, speech, social eating, social contact, and sexuality) as well as six single-item scales (problems with teeth, problems opening mouth, dry mouth, sticky saliva, coughing, felt ill). In addition, the questionnaire comprises five yes/no items (use of painkillers, nutritional supplements, feeding tube, weight loss, and weight gain).
The EORTC QLQ-C30 and H&N35 questionnaires were scored according to the EORTC scoring manual [20]. Scores on each scale range from 0–100. Higher scores in functioning scales indicate higher health-related QoL; higher scores in symptom scales indicate more severe symptoms and thus lower QoL. Score differences of 10 points or more between patient subgroups are considered to be clinically relevant [21]. It has been demonstrated that EORTC QLQ-C30 and H&N35 are valid and reliable instruments for the measurement of QoL in head and neck cancer patients [22,23,24,25].
A score of 100 indicates perfect QoL on the functional scales, whereas for the symptom scales a score of 100 indicates a heavy burden. Score differences of 10 points or more between patient subgroups are considered to be clinically relevant [21]. The reliability and validity of the C30 and HN35 scales are considered acceptable [24, 25].
Data analysis
Descriptive analyses were carried out to examine sociodemographic and medical characteristics of the sample. Group differences based on patients’ socioeconomic status were analyzed by univariate analysis of variance for metric variables or chi-square tests for categorical variables.
To compare the sample’s quality of life to the norm population, we created an age- and gender-adjusted comparison sample from the German norm population sample by matching each patient with the norm sample’s value from the same age category and gender, and performed two-sample t‑tests [22].
Regarding cancer-related QoL and head and neck-specific QoL 2 years after the end of RT, we compared functioning scale scores and symptom scale scores of the EORTC QLQ-C30 and H&N35 of patients from lower, middle, and higher social classes by analyses of covariance using baseline QoL (end of RT) as a covariate.
For comparisons of means between groups we calculated effect sizes Cohen’s d and partial eta-squared. As suggested by Cohen (1988), effect sizes are categorized as small (d = 0.2, partial eta2 = 0.01), medium (d = 0.5, partial eta2 = 0.06), and large (d = 0.8, partial eta2 = 0.14; [26]).
All data analyses were performed using SPSS (Windows) version 18.0 (IBM Corporation, Armonk, New York, USA).
Results
Patients
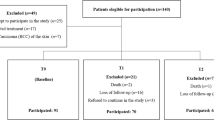
Between March 2009 and May 2014, 242 patients were enrolled into the study. 163 (67.4%) of those patients were alive 24 months after completion of radio(chemo)therapy, 62 (25.6%) had died, and 17 (7.0%) patients were lost to follow-up. Due to missing data on socioeconomic status, 2 patients had to be excluded from further analyses. Out of 161 patients included in the final analyses, 111 (68%) were male and 117 (72%) were married. The median age of the entire patient population was 60.9 years (range 22.7–82.9) and 71% of the sample presented with stage IV non-metastatic disease. Tumors of the oropharynx (38%) and the oral cavity (29%) were most prevalent. Patients with low socioeconomic status (SES) had significantly lower physical functioning scores and were more frequently diagnosed with a lower Karnofsky Performance Status (KPS) than patients with medium or high SES. They were also significantly more often widowed or divorced, more frequently retired, and denied more frequently current alcohol consumption (Table 1).
Treatment
114 patients (70%) had surgery initially and were referred for adjuvant treatment with curative intent. Of the patients receiving definitive RCT, 17 (15%) had prior chemotherapy. In total, 50% of patients had concurrent RCT.
SES as predictor for changes in QoL
At the end of radiation therapy (RT), patients with high SES reported significantly lower mean scores in their quality of life (EORTC QLQ-C30) than patients with low SES in regard to global health status (minus 15.2, p =0.005), role function (minus 23.8, p =0.002), and social function (minus 19.4, p =0.023). Mean scores reported for physical, emotional, and cognitive function and symptom burden did not differ significantly between SES groups (univariate analysis data not shown). Nearly all patients (97%) reported fatigue symptoms at the end of R(C)T and a substantial part of the sample reported symptoms such as pain (86%), insomnia (76%), appetite loss (76%) and nausea/vomiting (69%), dyspnea (58%), constipation (53%), and financial problems (58%). Frequencies of reported symptoms did not differ by SES (Table 2).
Twelve and 24 months after radio(chemo) therapy, mean scores reported for function and symptom scales for general quality of life (EORTC QLQ-C30) recovered remarkably. Patients with low SES reported less advantageous changes in quality of life scores over time in many function and symptom scales than patients with medium or high SES (Table 2).
Similarly, regarding specific quality of life issues (EORTC head and neck module HN35), patients report substantial symptom burden in all symptom scales at the end of treatment and less impairments at 12 and 24 months after the completion of R(C)T (Table 3). Univariate analyses show that mean symptom scores at the end of R(C)T do not significantly differ by SES (data not shown).
ANCOVA analyses show that at 24 months after treatment, patients with high SES report significantly higher quality of life scores than patients with medium or low SES for their global health status and physical and role function. They also report significantly lower symptom burden regarding fatigue, pain, and dyspnea. Effect sizes of these group differences were medium (partial eta2 between 0.040 and 0.090; Table 4).
Considering specific quality of life scores (EORTC head and neck module), patients with high SES report significantly lower symptom burden than patients with medium or low SES for the items: pain, swallowing, senses, speech, social eating, opening mouth, and feeling ill. Effect sizes of these group differences were medium (partial eta2 between 0.040 and 0.085; Table 5).
All patients reported significantly impaired functioning scores as well as significantly increased symptom burden in all functioning and symptom scales of the EORTC QLQ-C30 24 months after the end of R(C)T compared to a population reference group. Effect sizes of these differences were mainly medium to large (d between 0.229 and 0.824; Table 6).
Discussion
Our study demonstrated that patients with a high SES undergoing IMRT for the treatment of head and neck cancer report significantly worse global and cancer-specific QoL compared to patients with a low SES at the end of R(C)T. Our data suggest that during the first 24 months after treatment, the recovery in patients with high SES is of a significantly larger magnitude compared to patients with low SES (panel 1 and 2, Supplementary Material). Patients with low SES report less significant changes in their role function and symptom burden at 12 and 24 months after treatment. This is in line with previous reports on SES as predictor for QoL and outcome in head and neck cancer patients as well as in cancer patients in general [7, 27,28,29,30].
To the best of our knowledge, this is the first study evaluating SES as a predictor for QoL using the EORTC questionnaires in head and neck cancer patients after R(C)T with curative intent in a patient population with LAHNC. A study looking at the impact of monthly income on QoL in cancer patients using the Functional Assessment of Cancer Therapy-General (FACT-G) and the SF-12 module as QoL measures found that patients with an affluent background had a significantly better QoL after surviving cancer [13].
It is worth noting that most studies on SES and cancer care outcome in general, as well as in head and neck cancer patients, define SES solely by a single item: income as the determinant of SES [6, 8, 14, 29, 31,32,33]. Using income alone as SES indicator has several limitations; it doesn’t account for employment status (retired versus employed/unemployed), comorbidities, wealth, living situation/support system, and is less stable than education [34]. In our study, we used the adapted version of a composite social class indicator based on primary and secondary education, type of occupation, and monthly household net income [17].
Contrary to other reports, the distribution of UICC stage in our study did not significantly differ between SES groups: Chu et al. showed that patients with low SES present significantly more often with more advanced disease at first diagnosis [29]. A US American study published by Naghavi et al. in 2016 reported that in Afro-Americans with head and neck cancer, there is an association between SE, employment status, and marital status on one side and delayed diagnosis and begin of therapy on the other [35].
In contrast to countries where socioeconomic imbalances are accompanied by limited or no access to healthcare, in Germany, every individual has access to health care coverage through the solidarity system. A Canadian study stating that Canadian citizens have access to universal healthcare [8] reported that low SES was associated with more advanced disease stage at diagnosis. Patients with low SES were more likely to consume alcohol and tobacco and were more likely to have cancer of the oral cavity and greater comorbidity [28]. This also partially applied to our patient population, which had more patients with oral cancers in the low and middle SES groups. In our patient population, more than two thirds of patients were grouped into low and middle SES groups and 22% into the high SES group. It was shown that the incidence of head and neck cancer is higher in deprived populations [6].
Being single, poorly educated, with low income (annual household income of less than 20,000 US$) were found to be the main determinants of SES [36]. Low SES was not shown to be predictive for malignant diseases in general but specific for head and neck cancer [36]. An increased incidence of head and neck cancer in low-income populations was also described in other Canadian studies [6, 8, 14, 32]. It was also shown that patients with high SES have a better chance of surviving cancer independent of tumor stage and consumption of nicotine or alcohol [8, 28]. Differences between ethnicity, SES, and survival could not be explained simply with demographic data, comorbidity, or differences in treatment strategies [37].
The incidence of oropharyngeal cancer is increasing, independent of SES. However, the greatest increase is seen in the patient population with high SES [6, 8]. A US American study reported that Afro-Americans with high SES are more likely to have HPV-associated oropharyngeal cancers than Afro-Americans with low SES [38]. In our population, HPV assessment was not routinely implemented until a few years ago. Therefore, we are unable to provide any reliable data for our sample. However, 38% (61 patients) of our population are patients with an oropharyngeal primary cancer. According to available epidemiological data, the prevalence of HPV (human papilloma virus) in northern Germany [39] is about 20–30% in oropharyngeal cancer, thus probably affecting less than 20 patients of our study population only and is therefore likely to be of negligible impact.
Critical comments
First, contrary to other reports, in our patient population there were less alcohol consumers and more smokers in the low SES group. This phenomenon might be underreporting of alcohol consumption. In addition, contrary to the United States, where nicotine consumption has dramatically reduced, smoking habits have remained practically unchanged in Europe [40]. In a study from Canada by Chu et al., smoking and heavy alcohol consumption were associated with more comorbidities and low SES [28]. Each risk factor is associated with a worse prognosis in general. Guo et al. showed that increased nicotine consumption is a significant negative predictor for cancer-specific survival. Particularly a high number of pack-years is associated with worse survival in low SES groups [41].
Second, in our patient population, 91% of patients were diagnosed with locally advanced cancers (UICC III/IV), and thus, by definition, were treated with R(C)T in the primary or adjuvant setting. Therefore, we cannot draw any conclusions about SES and stage of disease at diagnosis. Chu et al. looked at more than 4700 head and neck cancer patients and analyzed Asian-Pacific Islanders—the fastest growing population in California [29]. Low SES patients were diagnosed with more advanced disease and had a 24% increased risk of dying from head and neck cancer. In this population-based study, the potential survival benefit of adding chemotherapy to radiotherapy was superseded by low SES. QoL was not examined in this study. However, since QoL is a major predictor for cancer survival, it can be assumed that QoL in this patient population is likely to be poor [37, 38].
Finally, only native German speakers were included in the study, which might be a selection bias and results might not apply to other patient populations.
One of the strengths of this study is that few patients were lost to follow-up, strengthening the conclusions drawn from the data. Observational studies, while less rigorously controlled than randomized clinical trials, have the advantage of more accurately reflecting the real-life clinical situation because they suffer less frequently from selection bias that can result from excluding patients based on factors such as comorbidity and age.
Conclusion
Most head and neck cancer patients experience a negative impact on their quality of life after R(C)T and report scores below the reference population as long as 24 months after treatment. This prospective study shows that socioeconomic factors have a strong influence on quality of life in this patient group, especially in patients with low SES who show the strongest impairment [42, 43]. The potential association between SES and QoL as well as possible interventions such as counseling at the start of therapy and offering programs to support patients with lower SES should be investigated in future studies.
References
Rogers SN, Ahad SA, Murphy AP (2007) A structured review and theme analysis of papers published on “quality of life” in head and neck cancer: 2000–2005. Oral Oncol 43:843–868
Infante-Cossio P, Torres-Carranza E, Cayuela A, Hens-Aumente E, Pastor-Gaitan P, Gutierrez-Perez JL (2009) Impact of treatment on quality of life for oral and oropharyngeal carcinoma. Int J Oral Maxillofac Surg 38:1052–1058
Tribius S, Raguse M, Voigt C, Münscher A, Gröbe A, Petersen C et al (2015) Residual deficits in quality of life one year after intensity-modulated radiotherapy for patients with locally advanced head and neck cancer. Strahlenther Onkol 191:501–510
Leung WS, Lee TF, Chien CY, Chao PJ, Tsai WL, Fang FM (2011) Health-related Quality of life in 640 head and neck cancer survivors after radiotherapy using EORTC QLQ-C30 and QLQ-H&N35 questionnaires. BMC Cancer 11:128
Maurer J, Hipp M, Schäfer C, Kölbl O (2011) Dysphagia. Impact on quality of life after radio(chemo)therapy of head and neck cancer. Strahlenther Onkol 187:744–749
Hwang E, Johnson-Obaseki S, McDonald JT, Connell C, Corsten M (2013) Incidence of head and neck cancer and socioeconomic status in Canada from 1992 to 2007. Oral Oncol 49:1072–1076
Singer S, Bartels M, Briest S, Einenkel J, Niederwieser D, Papsdorf K et al (2016) Socio-economic disparities in long-term cancer survival-10 year follow-up with individual patient data. Support Care Cancer. https://doi.org/10.1007/s00520-016-3528-0
McDonald JT, Johnson-Obaseki S, Hwang E, Connell C, Corsten M (2014) The relationship between survival and socio-economic status for head and neck cancer in Canada. J Otolaryngol Head Neck Surg 43:2
Yost K, Perkins C, Cohen R, Morris C, Wright W (2001) Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control 12:703–711
Lampert T, Koch-Gromus U (2016) Soziale Ungleichheit und Gesundheit. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 59:151–152
Mackenbach JP, Meerding WJ, Kunst AE (2011) Economic costs of health inequalities in the European Union. J Epidemiol Community Health 65:412–419
Robert-Koch-Institut (2016) Bericht zum Krebsgeschehen in Deutschland 2016. Robert-Koch-Institut, Berlin
Short PF, Mallonee E (2006) Income disparities in the quality of life of cancer survivors. Med Care 441:16–23
Johnson S, McDonald JT, Corsten M (2012) Oral cancer screening and socioeconomic status. J Otolaryngol Head Neck Surg 41:102–107
Johnson S, Corsten MJ, McDonald JT, Gupta M (2010) Cancer prevalence and education by cancer site: logistic regression analysis. J Otolaryngol Head Neck Surg 39:555–560
Hodapp N (2012) Der ICRU-Report 83: Verordnung, Dokumentation und Kommunikation der fluenzmodulierten Photonenstrahlentherapie (IMRT). Strahlenther Onkol 188:97–100
Winkler J, Stolzenberg H (1999) Social class index in the Federal Health Survey. Gesundheitswesen 61(Spec No):S178–S183
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85:365–376
Bjordal K, Ahlner-Elmqvist M, Tollesson E, Jensen AB, Razavi D, Maher EJ et al (1994) Development of a European Organization for Research and Treatment of Cancer (EORTC) questionnaire module to be used in quality of life assessments in head and neck cancer patients. EORTC Quality of Life Study Group. Acta Oncol 33:879–885
Fayers PM, Aaronson NK, Bjordal K et al (2001) On behalf of the EORTC Quality of Life Study Group. The EORTC QLQ-C30 Scoring Manual, 3rd edn. European Organisation for Research and Treatment of Cancer, Brussels
King MT (1996) The interpretation of scores from the EORTC quality of life questionnaire QLQ-C30. Qual Life Res 5:555–567
Schwarz R, Hinz A (2001) Reference data for the quality of life questionnaire EORTC QLQ-C30 in the general German population. Eur J Cancer 37:1345–1135
Arraras JI, Arias F, Tejedor M, Pruja E, Marcos M, Martínez E et al (2002) The EORTC QLQ-C30 (version 3.0) Quality of Life questionnaire: validation study for Spain with head and neck cancer patients. Psychooncology 11:249–256
Singer S, Wollbrück D, Wulke C, Dietz A, Klemm E, Oeken J et al (2009) Validation of the EORTC QLQ-C30 and EORTC QLQ-H&N35 in patients with laryngeal cancer after surgery. Head Neck 31:64–76
Singer S, Arraras JI, Chie WC et al (2013) Performance of the EORTC questionnaire for the assessment of quality of life in head and neck cancer patients EORTC QLQ-H&N35: a methodological review. Qual Life Res 22:1927–1941
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Routledge Academic, Erlbaum, New York, Hillsdale
Wells M, Swartzman S, Lang H, Cunningham M, Taylor L, Thomson J et al (2016) Predictors of quality of life in head and neck cancer survivors up to 5 years after end of treatment: a cross-sectional survey. Support Care Cancer 24:2463–2472
Chu KP, Habbous S, Kuang Q et al (2016) Socioeconomic status, human papillomavirus, and overall survival in head and neck squamous cell carcinomas in Toronto, Canada. Cancer Epidemiol 40:102–112
Chu K, Shema S, Wu S, Gomez S, Chang E, Le Q (2011) Head and neck cancer specific survival based on socioeconomic status in Asians and Pacific Islanders. Cancer 117:1935–1945
Booth CM, Li G, Zhang-Salomons J, Mackillop WJ (2010) The impact of socioeconomic status on stage of cancer at diagnosis and survival: a population-based study in Ontario, Canada. Cancer 116:4160–4167
Mackillop WJ, Zhang-Salomons J, Groome PA, Paszat L, Holowaty E (1997) Socioeconomic status and cancer survival in Ontario. J Clin Oncol 15:1680–1689
Boyd C, Zhang-Salomons JY, Groome PA, Mackillop WJ (1999) Associations between community income and cancer survival in Ontario, Canada, and the United States. J Clin Oncol 17:2244–2255
Johnson S, McDonald JT, Corsten M, Rourke R (2010) Socio-economic status and head and neck cancer incidence in Canada: a case-control study. Oral Oncol 46:200–203
Shavers VL (2007) Measurement of socioeconomic status in health disparities research. J Natl Med Assoc 99:1013–1023
Naghavi AO, Echevarria MI, Strom TJ et al (2016) Treatment delays, race, and outcomes in head and neck cancer. Cancer Epidemiol 45:18–25
Johnson S et al (2008) Socioeconomic factors in head and neck cancer. J Otolaryngol Head Neck Surg 37:597–601
Molina MA, Cheung MC, Perez EA, Byrne MM, Franceschi D, Moffat FL et al (2008) African American and poor patients have a dramatically worse prognosis for head and neck cancer. Cancer 113:2797–2806
Liederbach E, Kyrillos A, Wang C‑H, Liu JC, Sturgis EM, Bhayani MK (2017) The national landscape of human papillomavirus-associated oropharynx squamous cell carcinoma. Int J Cancer 140:504–512
Quabius ES, Haag J, Kühnel A et al (2015) Geographical and anatomical influences on human papillomavirus prevalence diversity in head and neck squamous cell carcinoma in Germany. Int J Oncol 46:414–422
World Health Organization Regional Office for Europe (2014) European tobacco control status report 2014. WHO, Copenhagen
Guo Y, Logan HL, Marks JG, Shenkman EA (2015) The relationships among individual and regional smoking, socioeconomic status, and oral and pharyngeal cancer survival: a mediation analysis. Cancer Med 4:1612–1619
van Nieuwenhuizen AJ, Buffart LM, Brug J, Leemans CR, Verdonck-de Leeuw IM (2015) The association between health related quality of life and survival in patients with head and neck cancer: a systematic review. Oral Oncol 51:1–11
Kypriotakis G, Vidrine DJ, Francis LE, Rose JH (2016) The longitudinal relationship between quality of life and survival in advanced stage cancer. Psychooncology 25:225–231
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S. Tribius, M.S. Meyer, C. Pflug, H. Hanken, C.‑J. Busch, A. Krüll, C. Petersen, and C. Bergelt declare that they have no competing interests.
Caption Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Tribius, S., Meyer, M.S., Pflug, C. et al. Socioeconomic status and quality of life in patients with locally advanced head and neck cancer. Strahlenther Onkol 194, 737–749 (2018). https://doi.org/10.1007/s00066-018-1305-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-018-1305-3
Keywords
- Quality of life
- Head and neck cancer
- Intensity-modulated radiotherapy
- Rehabilitation
- Socioeconomic status