“The results show that the effect of multiple dose fractions, even a very small one, is in no respect different, in terms of macroscopic (skin) damages, from that of a single dose” Reisner, “Skin erythema and roentgen therapy”, 1933
Abstract
The toxicity of stereotactic body radiation therapy in the central chest remains an unsettled issue. The collected data concerning the observed complications are poorly understood and are limited in their quantity and quality, thus hampering a precise delineation of treatment-specific toxicity. The majority of complications scored as toxicity grade 5, namely respiratory failure and fatal hemoptysis, are most likely related to multiple competing risks and occurred at different dose fractionation schemas, e. g., 10–12 fractions of 4–5 Gy, 5 fractions of 10 Gy, 3 fractions of 20–22 Gy, and 1 fraction of 15–30 Gy. Further investigations with longer follow-up and more details of patients’ pretreatment and tumor characteristics are required. Furthermore, satisfactory documentation of complications and details of dosimetric parameters, as well as limitation of the wide range of possible fractionation schemes is also warranted for a better understanding of the risk factors relevant for macroscopic damage to the serially organized anatomic structure within the central chest.
Zusammenfassung
Das Risiko für schwere Nebenwirkungen der stereotaktischen Strahlentherapie bei zentralen Lungentumoren ist bisher schlecht definiert. Nicht nur die begrenzte Zahl der dokumentierten Ereignisse, sondern auch die Vielzahl der verwendeten Fraktionierungsschemata erschwert das Herausarbeiten valider prognostischer Faktoren. Auf Basis dieser Datenlage lässt sich das Risiko für Grad-5-Toxizitäten, insbesondere Atemversagen und tödliche Blutungen, kaum einem bestimmten Dosis- oder Fraktionierungsschema, wie z. B. 10–12 Fraktionen mit 4–5 Gy, 5 Fraktionen mit 10 Gy, 3 Fraktionen mit 20–22 Gy und 1 Fraktion mit 15–30 Gy zuordnen, da multiple patientenspezifische, konkurrierende Risiken dabei einen wesentlichen Einfluss zu haben scheinen. Es wird zukünftig erforderlich sein, prätherapeutische Patienten- und Tumorcharakteristika genauer zu erfassen, dosimetrische Parameter besser zu dokumentieren und die Vielfalt der Fraktionierungsschemata zu begrenzen, um die relevanten Risikofaktoren für schwere Nebenwirkungen an den seriell organisierten anatomischen Strukturen des zentralen Brustkorbs besser definieren zu können.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is little doubt that stereotactic body radiation therapy (SBRT) is safe for the treatment of peripheral lung lesions and it is used routinely. However, the primary controversy regarding the safety of SBRT involves its utility for centrally located lung tumors. During the past decades, the central chest has been widely acknowledged as a “no-fly zone” for SBRT, even in the National Comprehensive Cancer Network (NCCN) guidelines for the treatment of non-small cell lung cancer (NSCLC) in 2010 and 2011.
Nevertheless, the Radiation Therapy Oncology Group (RTOG) dose-escalation phase I study for centrally located lung cancer (RTOG 0813; [1]) has recently published its primary endpoint analysis. Except for one case of cardiac toxicity grade 3 (G3), all other toxicities G3–G5 occurred in the parallel arranged lung parenchyma (hypoxia and pneumonitis). Severe toxicities in the tracheobronchial tree and the esophagus were not reported. In the German metacentric analysis [2], one of 90 patients with central lung cancer died from pneumonitis G5 without evidence of bronchial stenosis or bleeding.
Indeed, reviews including comprehensive data concerning SBRT-specific morbidity and mortality when treating central lung tumors are sparse [3]. The aim of this paper is to provide a discursive prose, rather than a data summerizing review on the specific toxicity of SBRT to anatomic structures within the central chest.
Methods
The initial literature search was also based on studies identified by Kang et al. [3], and extended to a wide range of literature offered by citation analysis and manual as well as electronic reference chaining. Lung tumors located within 2 cm around the proximal tracheobronchial tree, or at a maximum distance of 1 cm from the heart and pericardium, and the esophagus were considered as central. To synthesize the literature data in the form of a comprehensive review, an approach incorporating qualitative research synthesis methodology was used. The key process involved in this review is illustrated in Table 1.
Results
Literature search
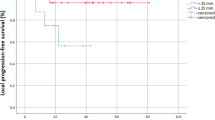
The search strategy identified 68 studies including 2457 patients treated with SBRT for central lesions. After repeated re-reading of each individual paper, 20 (30 %) studies with 608 (25 %) patients and 7 (10 %) studies with 207 (8 %) patients reporting ex negativo no specific and no long-term toxicity, respectively, were excluded. As a result, 41 (60 %) studies with 1642 patients (67 %) were considered to be highly relevant to the initial inquiry and included (see Fig. 1 and electronic supplementary material).
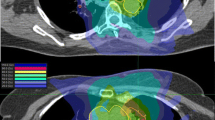
Individual data of 115 (7 %) patients (4.6 % of all patients treated in studies including central lesions) were extracted, reviewed, and characterized. Tracheobronchial toxicity was the most frequently reported (6.7 %). Other endpoints, including cardiac toxicity, respiratory failure, fatal hemoptysis, and esophageal toxicity ≥ G3, were equally reported, with rates of 2.8 %, 2.2 %, 2.3 %, 2.4 %, and 2.4 %, respectively. Overall, specific late toxicity occurred with a median total dose of 50 Gy (range 40–54 Gy) and a median biologically effective dose with α/β = 3 Gy (BED3) of 216 Gy3 (210–277 Gy3) in the hottest/shortest regimes compared with a median total dose of 45 Gy (range 30–50 Gy) and a median BED3 of 176 Gy3 (90–237 Gy3) in the coldest/longest regimes. A summary of toxicity data is shown in Table 2.
Cardiac toxicity
The beating heart can neither be categorized as a parallel nor as a serially arranged organ at risk (OAR). Tumor and normal tissue motion induced by the beating heart and in combination with respiratory-induced motion are poorly understood. The motion artifacts are more severe in the left lung adjacent to the beating heart. Compensation of heart motion seems to be impossible as yet, and the true maximal dose tolerated by the heart or its partial volume remains unknown, even in the conventional setting.
In a recently published study on 39 lung tumors that were close to the heart, increased cardiac uptake of 18-flurodeoxyglucose (18-FDG) was observed in positron-emission tomography (PET) in 9 patients in whom more than 5 cc of the heart was covered by the 20 Gy isodose line, but without meaningful correlation between this observation and cardiac toxicity [4]. Without describing the perfusion–metabolism patterns (normal, subendocardial match, transmural match, and mismatch), PET alone is obviously meaningless for post-SBRT cardiac toxicity assessment.
Cardiac toxicity in SBRT studies included radiation-induced damage to the pericardium, the impulse conductive tissue, and the myocardium. Fourteen cases were identified from eight studies. The largest data set on cardiac toxicity comes from experiences at Indiana University. However, SBRT-related pericardial effusion seems to be a rare entity (Table 3). This may be related to significant improvements in treatment planning techniques or to the use of less ablative doses than those applied by Indiana University or even to the reluctance of radiation oncologists to treat central tumors that are adjacent to the beating heart. After a median follow-up of 6.3 months (range 3–29 months), Bonomo and colleges from Florence University [14], who treated 16 paracardiac lesions with 3 fractions of 12 Gy, reported no long-term cardiac toxicity.
In the aforementioned phase II study [8], one patient died from complications of pericardial effusion without further information.
Respiratory failure
Fakiris et al. [15] stated that the abovementioned complications resulted from pericardial effusion as “respiratory failure.” Either the signs of cardiac tamponade resulting from delayed chronic pericardial effusion had been interpreted as “respiratory failure” because dyspnea is the most common presenting symptom, or this “respiratory failure” was possibly related to the preexisting pulmonary dysfunction or even to pneumonia. The immediate cause of respiratory failure remains unclear.
Indeed, respiratory failure is a general and ill-specified endpoint, and reflects a final condition resulting in death, regardless of the underlying cause initiating the events leading to death. The majority of deaths could be perceived as resulting from “respiratory failure,” as it would usually be documented in death certification. Thus, this clinical endpoint seems to be inappropriate for assessment of treatment-specific toxicity. Unfortunately, respiratory failure was used as a safety endpoint in six SBRT series (Table 4). This reflects the fact that the authors were unsure of the immediate cause of death, or unable to accurately ascertain the underlying or contributing causes of death.
Bronchial stenosis and atelectasis
The pathophysiological mechanisms underlying radiation-induced bronchial stenosis and subsequent collapse of the lung tissue remain poorly understood. Radiation injury to the bronchi might begin simply with erythema, edema in the mucosa, and transmural inflammatory infiltration that manifests in some degree of wall thickening of major airways without clinical evidence of airflow restriction [20]. At this stage, some radiological signs may begin to appear, including discrete hypoventilation of downstream lung tissue without changing tissue density or signs of atelectasis [21].
Over time, multiple superficial ulcers may become apparent. These occur mostly in “maximum dose” areas and are surrounded by endobronchitis [22]. Chronic endobronchitis might progress into ulceration and fibrosis. While ulceration may result in necrosis and fistula formation in the main/lobar bronchi [16, 17], the progression of fibrosis may ultimately narrow the segmental airways, resulting in the collapse of downstream lung tissue [22].
Tumor necrosis and the sloughing off of endobronchial mucosa after SBRT may also obstruct the airway lumen. This remains a potential problem even for endoscopic treatments, which are considered to be the safest intervention modality. Stauder et al. [18] reported on a patient who died from respiratory failure “secondary to tumor necrosis causing progressive bronchial obstruction.” In addition, increased production of mucus has been observed after re-irradiation with SBRT [23].
Furthermore, bronchial stenosis might not appear to be the only causal factor for atelectasis. There is more lung tissue around segmental bronchi compared to main/lobar bronchi, and thus also a higher risk of radiation-induced pneumonitis. The alveoli surrounding the lesions might be compressed by parenchyma fibrosis, tumor progression, or bacterial infection, resulting in cicatrization atelectasis. Thus, the collapse of lung tissue might not necessarily result from upstream airway stenosis.
Eleven cases of bronchial stenosis without secondary atelectasis and five cases of stenosis with secondary atelectasis were identified. By contrast, 28 cases of atelectasis without documented upstream bronchial stenosis were found (Table 5).
The most important attempt to estimate the dose–response relationship for atelectasis comes from the Karolinska University experience reported by Karlsson et al. [33]. However, the analysis was confused by several uncertainties addressed by the investigators themselves, thus rendering these constraints unsuitable for generalization across the literature. Furthermore, the authors did not distinguish patients who developed bronchial stenosis with secondary atelectasis from those with bronchial stenosis without atelectasis, or from those with atelectasis but without bronchial stenosis.
The study was also biased by bad resolution for the delineation of OAR, which resulted from a CT slice thickness of 1 cm and 0.5 cm before and after 1996, respectively. On such slices, subvolumes of the bronchial tree might not be visible and hotspots on the circumferential bronchial discs might be overlooked. By contrast, in a previously unpublished student thesis on the same cohort of patients, Karlsson [35] showed a dose–response relationship only for right-sided lung tumors.
While reporting of atelectasis is more frequent, high rates of bronchial stenosis have been reported in only one study [26]. Of 9 patients, 3 of 6 patients who had tumors adjacent to the main/lobar bronchus and 2 of 3 patients with tumors adjacent to the segmental bronchus experienced partial bronchial stenosis, and 3 of the former 6 patients had complete stenosis. One patient developed bleeding, aspiration, and pneumonia. A pneumonectomy, which was performed to control the bleeding, then became the immediate cause of death.
In a similar vein, Bral et al. [29] reported on a case of fatal hemoptysis after stent placement for grade 3 bronchial stenosis, which was defined as the only treatment-related death. This patient most likely died of fatal hemoptysis from bronchovascular fistula formation resulting from the stent insertion procedure itself (see “fatal hemoptysis” below). From these observations, an erroneous “concern over the safety of stenting previously irradiated airways” was also drawn [29].
However, bleeding as an iatrogenic complication after stent implantation in nonirradiated airways is not rare. It remains unclear whether radiation therapy may increase the risk of iatrogenic bronchovascular fistula formation after stent implantation and also the risk of fatal hemoptysis.
Fatal hemoptysis
Fatal hemoptysis is one of the most serious reported complications after SBRT and was reported in 16 studies (Table 6). The clinical and pathological mechanism of fatal pulmonary hemorrhage in patients with lung cancer is poorly understood. The theory of cavitation with subsequent fistula formation between airways and bronchial circulation, rather than pulmonary circulation or a non-bronchial circulation system, e. g., aortobronchial fistula, seems to be the most plausible mechanism to explain the occurrence of hemoptysis of necrotizing tumors, local recurrence, necrotizing pneumonia, and of radiation induced-necrosis or of antineoplastic agents with a cavitation response.
Fatal hemoptysis is also commonly related to the high-pressure bronchial arterial system and rarely to the low-pressure pulmonary arterial system. Thus, the volume of the pulmonary artery exposed to high-dose radiation therapy might not be adequate at all for dosimetric analysis of radiation-related hemoptysis. In a recently published study by Han et al. [36], the widely believed dogma that fatal hemoptysis might result from high-dose radiation-induced damage to the pulmonary artery could not be confirmed, and only 2 of 100 patients with lung tumors adjacent to or invading the pulmonary artery experienced massive hemoptysis. In three SBRT studies, attempts were made to correlate the dose to the pulmonary artery with the occurrence of fatal hemoptysis. In two studies [23, 37], no correlation was found and the patient in the third study [38] was excluded from the final analysis [12].
In a chemoradiation setting, the presence of baseline major tumor cavitation and squamous cell histology [39], and central location and local recurrence and squamous cell histology [40] were associated with a high risk for hemoptysis.
The highest incidence of fatal hemoptysis was reported in a brachytherapy setting, although the discussion on postprocedural complications here remains controversial. A consensus report from a panel of experts addressing the problem of fatal hemoptysis in patients with lung cancer treated with bevacizumab demonstrated squamous cell histology and pretreatment sentinel bleeding to be prior risk factors, but not cavitation, tumor location, and invasion into blood vessels [41]. However, the panel of experts was confused by lacking standardized radiological criteria for assessing the centrality, vascular invasion, and grade of cavitation. In an SBRT study on tumors abutting the tracheobronchial tree, 2 of 4 patients died of pulmonary hemorrhage after receiving anti-vascular endothelial growth factor (VEGF; [42]).
Nonetheless, squamous cell carcinomas of the lung are usually centrally located, are more likely to invade the large blood vessels, and have a high tendency to cavitate; thus representing all of the abovementioned independent risk factors for fatal hemoptysis.
Bronchial necrosis and fistula formation
However, there is only one report with direct endoscopic evidence of the source of fatal bleeding from radiation-induced bronchial necrosis [49]. Overall, there are only three cases of endoscopic evidence of bronchial necrosis, and these resulted in different clinical scenarios, i. e., fatal hemoptysis [49], atelectasis [16], and bronchial fistula formation [17] after treating lung cancer, metastatic malignant melanoma, and malignant mesothelioma, respectively. Additionally, the Indiana University group reported one case of bronchitis and one case of tracheal necrosis in their series with doses of 3 fractions of 20 Gy and 3 fractions of 24 Gy, respectively (no information about location is available [5]).
There may be other competing risks that interfere with the course of necrosis. While the roles of cisplatin and pemetrexed in the worsening of radiation necrosis in the abovementioned case of fatal hemoptysis [49] remains unclear, the contribution of gemcitabine-related radiation recall reactions to mediastinal toxicity is well established. Le et al. [45] reported on a patient treated with single-dose radiation therapy, who, after switching his adjuvant chemotherapy to gemcitabine, developed a tracheoesophageal fistula followed by fatal hemoptysis from a “tracheovascular fistula” that was confirmed by postmortem findings. In the same series, another patient with a central lesion died of lung embolisms and radiation recall pneumonitis after receiving gemcitabine, and all G2–G5-scored toxicity for central lesions was associated with chemotherapy. In an aforementioned study [40], gemcitabine was linked to the development of fatal hemoptysis in patients with lung cancer.
Tracheoesophageal fistula formation was also seen only in patients who received anti-VEGF [50].
Esophagitis and esophageal ulceration
Clinically relevant esophageal toxicity with or without endoscopic evidence of ulceration was identified in eight SBRT studies (Table 7).
Data on esophageal motion induced by respiration in patients with lung cancer are very limited and the majority of data are derived from studies that attempt to estimate respiratory-induced motion of distal esophageal cancer. Although the longitudinal and circular motion of the esophagus during the comparatively longer duration of SBRT treatment may alter the dose distribution in the esophageal mucosa and musculature, resulting in over- or underestimation of doses in the esophagus, no data on the esophagus’ inherent motility in humans are available. In an animal-based model [51], an excursion of 2–10 mm of the longitudinal esophageal axis was observed, which was synchronous with “chest wall, diaphragm movement and intraluminal pressure.” The magnitude and duration of oral and aboral excursion were significantly greater for the distal and proximal esophagus, respectively.
While dose–volume effects in the esophagus have been exhaustively reviewed in the conventional setting, no large body of data existed—up until December 2015—on SBRT-related esophagus toxicity. Onimaru et al. [52] reported on a patient with metastatic lung cancer who developed fatal hemorrhage from an esophageal ulcer 5 months after SBRT. A retrospective recontouring of the esophagus revealed a hotspot resulting from the large uncertainty in treatment planning given the primitive techniques for planning target volume (PTV) and OAR localization, delineation, and positional verification used in this study. Indeed, the data are very limited, making it very difficult to draw a meaningful conclusion.
Conclusion
The similar rates of frightening complications reported in heterogeneous studies and their occurrence associated with all possible dose fractionation schedules suggest that there may be independent pretreatment patient and tumor risk factors surrounding these complications rather than the treatment per se. However, the data remain inconclusive regarding whether protracted fractionation is indeed necessary to reduce the rate of complications. The current utilization of mostly inadequate endpoints for toxicity assessment may create an outward appearance of validity under which multiple competing risks that significantly contributed to the occurrence and severity of observed toxicity are hidden. Further investigations with longer follow-up and more details on patients’ pretreatment and tumor characteristics are required. Moreover, satisfactory documentation of complications and details of dosimetric parameters and dose fractionation are warranted. If this does not occur, the biased reporting of toxicity will continue to challenge the future utility of high-dose ablative radiation therapy.
References
Bezjak A, Paulus R, Gaspar LE et al (2016) Primary study endpoint analysis for NRG Oncology/RTOG 0813 trial of stereotactic body radiation therapy (SBRT) for centrally located non-small cell lung cancer (NSCLC). Int J Radiat Oncol Biol Phys 94:4–5
Shanne DH, Nestle U, Allgäuer M et al (2015) Stereotactic body radiotherapy for centrally located stage I NSCLC: a multicenter analysis. Strahlenther Onkol 191:125–132
Kang KH, Okoze CC, Patel RB et al (2015) Complications from stereotactic body radiotherapy for lung cancer. Cancers (Basel) 7:981–1004
Evans DJ, Gomez DR, Chang JY et al (2013) Cardiac 18F-fluorodeoxyglucose uptake on positron emission tomography after thoracic stereotactic body radiation therapy. Radiother Oncol 109:82–88
Timmerman R, Papiez L, McGary R et al (2003) Extracranial stereotactic radioablation: results of phase I study in medically inoperable stage I non-small cell lung cancer. Chest 124:1946–1955
McGarry R, Papiez L, Williams M et al (2005) Stereotactic body radiation therapy of early stage lung non-small cell carcinoma: phase I study. J Radiat Oncol Biol Phys 63:1010–1015
Timmerman R, Lohr F (2005) Normal tissue dose constraints applied in lung stereotactic body radiation therapy. In: Kavanagh BD, Timmerman R (eds) Stereotactic body radiation therapy. Lippincott Williams & Wilkins, Philadelphia, pp 29–37
Timmerman R, McGarry R, Yiannoutsos C et al (2006) Excessive toxicity when treating central tumors in a phase II study of stereotactic body radiation therapy for medically inoperable early stage lung cancer. J Clin Oncol 24:4833–4839
Milano MT, Chen Y, Katz AW et al (2009) Central thoracic lesions treated with hypofractionated stereotactic body radiotherapy. Radiother Oncol 91:301–306
Baba F, Shibamoto Y, Ogino H et al (2010) Clinical outcomes of stereotactic body radiotherapy for stage I non-small cell lung cancer using different doses dependent on tumor size. Radiat Oncol 5:81
Shibamato Y, Hashizume C, Baba F et al (2012) Stereotactic body radiotherapy using a radiobiolgy-based regimen for stage I non-small cell lung cancer. Cancer 118:2078–2084
Chang JY, Li QQ, Xu QY et al (2014) Stereotactic ablative radiation therapy for centrally located early stage or isolated parenchymal recurrences of non-small cell lung cancer: how to fly in a “No Fly Zone”. Int J Radiat Oncol Biol Phys 88:1120–1128
Modh A, Rimmer A, Williams E et al (2014) Local control and toxicity in a large cohort of central lung tumors treated with stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys 90:1168–1176
Bonomo P, Livi L, Rampini A et al (2013) Stereotactic body radiotherapy for cardiac and paracardiac metastases: University of Florence experience. Radiol Med 118:1055–1065
Fakiris A, McGarry R, Yinnoutoss C et al (2009) Stereotactic body radiation therapy for early-stage non-small-cell lung carcinoma: four years results of a prospective phase II study. Int J Radiat Oncol Biol Phys 75:677–682
Rowe BP, Boffa DJ, Wilson LD et al (2010) Stereotactic body radiotherapy for central lung tumors. J Thorac Oncol 7:1349–1399
Unger K, Ju A, Oermann E et al (2010) CyberKnife for hilar lung tumors: report of clinical response and toxicity. J Hematol Oncol 3:39
Stauder MC, McDonald OK, Olivier KR et al (2011) Early pulmonary toicity following lung stereotactic body radiation therapy delivered in consecutive daily fractions. Radiother Oncol 99:166
Tekatli H, Senan S, Dahele M et al (2015) Stereotactic ablative radiotherapy (SABR) for central lung tumors: Plan quality and long-term clinical outcomes. Radiother Oncol 117:64–70
Joyner M, Salter JB, Papanikolaus N et al (2006) Stereotactic body radiation therpy for centrally located lung lesions. Acta Oncol 45:802–807
Oskan F, Korhuber C, Krause G et al (2013) Simultaneous stereotactic body radiation therapy of a primary non-small cell lung cancer and synchronous carcinoma in situ in a medically inoperable patient: case report. Radiat Oncol 8:213
Onishi H, Araki T, Shirato H et al (2004) Stereotactic hypofractionated hig-dose irradiation for stage I non-small cell lung carcinoma: Clinical outcomes in 245 subjects in a Japanese multi-institutional study. Cancer 101:1623–1631
Peulen H, Karlsson K, Lindberg K et al (2011) Toxicity after reirradiation of pulmonary tumours with stereotactic body radiotherapy. Radiother Oncol 101:260–266
Song DY, Benedict SH, Cardinale RM et al (2005) Stereotactic body radiation therapy of lung tumors: preliminary experience using normal tissue complication probability-based dose limits. Am J Clin Oncol 28:591–596
Baumann P, Nyman J, Lax I et al (2006) Factors important for efficacy of stereotactic body radiotherapy of medically inoperable stage I lung cancer. A retrospective analysis of patients treated in the Nordic countries. Acta Oncol 45:787–795
Song SY, Choi W, Shin S et al (2009) Fractionated stereotactic body radiation therapy for medically inoperable stage I lung cancer adjacent to central large bronchus. Lung Cancer 66:89–93
Oshiro Y, Aruga T, Tsuboi K et al (2010) Stereotactic body radiotherapy for lung tumors at the pulmonary hilum. Strahlenther Onkol 186:274–279
Andratschke N, Zimmermann F, Boehm E et al (2011) Stereotactic radiotherapy for of histologically proven inoperable stage I non-small cell cancer: patterns of failure. Radiother Oncol 101:245–249
Bral S, Gevarte T, Linthout N et al (2011) Prospective, risk-adapted strategy of stereotactic body radiation therapy for early stage non-small-cell lung cancer: results of phase II study. Int J Radiat Oncol Biol Phys 80:1343–1349
Haasbeek CJ, Laagerwaard FJ, Soltman BJ et al (2011) Outcomes of stereotactic ablative radiotherapy for centrally located early-stage lung cancer. J Thorac Oncol 6:2036–2043
Feddock J, Arnold S, Shelton B et al (2013) Stereotactic body radiation therapy can be used safely to boost residual disease in locally advanced non-small cell lung cancer: a prospective study. Int J Radiat Oncol Biol Phys 85:1325–1331
Prendergast BM, Dobelbower MC, Bonner JA, Bonner JA et al (2013) Stereotactic body radiation therapy (SBRT) for lung malignancies: preliminary toxicity resuls using a flattening filter linear accelartor operating at 2400 monitor units per minute. Radiat Oncol 8:273
Karlsson K, Nyman J, Baumann P et al (2013) Retrospective cohort study of bronchial doses and radiation-induced atelectasis after stereotactic body radiation therapy of lung tumors located close to the bronchial tree. Int J Radiat Oncol Biol Phys 87:590–595
Nishimura S, Takeda A, Sanuki N et al (2014) Toxicities of organs at risk in the mediastinal and hilar regions following stereotactic body radiotherapy for centrally located lung tumors. J Thorac Oncol 9:1370–1376
Karlsson K (2006) Centrally located lung tumors treated with stereotactic body radiation therapy: student thesis. Stockholm University, Stockholm (http://www.diva-portal.org/smash/get/diva2:197881/FULLTEXT01.pdf)
Han CB, Wang WL, Quint L et al (2014) Pulmonary artery invasion, high-dose radiation, and overall survival in patients with non-small cell lung cancer. Int J Radiat Oncol Biol Phys 89:313–321
Feddock J, Cleary R, Arnold S et al (2013) Risk for fatal pulmonary hemorrhage does not appear to be increased following dose escalation using stereotactic body radiotherapy (SBRT) in locally advanced non-small cell lung cancer (NSCLC). J Radiosurg SBRT 2:235–242
Chang JY, Xu Q, Balter P et al (2013) Clinical outcome and toxicity in central located or isolated recurrent non-small cell lung cancer treated with stereotactic ablative radiation therapy. Int J Radiat Oncol Biol Phys 87:514–S515
Ito M, Niho S, Nihei K et al (2012) Risk factors associated with fatal pulmonary hemorrhage in locally advanced non-small cell lung cancer treated with chemoradiotherapy. BMC Cancer 12:27
Kim YH, Kim EY, Ban HY et al (2010) Risk of fatal hemoptysis after concurrent chemoradiation in patients with non-small cell cancer. Chonnam Med J 46:19–24
Reck M, Barlesi F, Crino L et al (2012) Predicting and managing the risk of pulmonary haemorrhage in patients with NSCLC in patients treated with bevacizumab: a consensus report from a panel of experts. Ann Oncol 23:1111–1120
Haseltine JM, Rimmner A, Gelblum DY et al (2015) Fatal complications after stereotactic body radiation therapy for central lung tumors abutting the proximal bronchial tree. Pract Radiat Oncol 6(2):e27–e33
Wulf J, Hadinger U, Oppitz U et al (2001) Stereotactic radiotherapy of targets in the lung and the liver. Strahlenther Onkol 177:645–655
Fink AS, Kim JA, McBride RD (2007) Toxicity and efficacy of treating mediastinal and hilar lesions. In: Urshel HJ (ed) Robotic radiosurgery: treating tumors that move with respiration. Springer, Heidelberg, pp 177–192
Le QT, Loo BW, Ho A et al (2006) Results of a phase I dose-escalation study using single-fraction stereotactic radiotherapy for lung tumors. J Thorac Oncol 1:802–809
Trovo M, Minatel E, Durofil E et al (2014) Stereotactic body radiation therapy for re-irradiation of persistent or recurrent non-small cell lung cancer. Int J Radiat Oncol Biol Phys 88:114–119
Kilburn JM, Kuremskz JG, Blackstock AW et al (2014) Thoracic re-irradiation using stereotactic body radiotherapy (SBRT) techniques as first or second course of treatment. Radiother Oncol 110:505–510
Park HS, Harder EM, Mancini BR (2015) Central versus peripheral tumor location: influence on survival, local control and toxicity following stereotactic body radiotherapy for primary non-small cell lung cancer. J Thorac Oncol 10:832–837
Corradetti MN, Haas AR, Rengan R (2012) Central-airway necrosis after stereotactic body radiation therapy. N Eng J Med 366:2327–2329
Stephans KL, Djemil T, Diaconu C et al (2014) Esophageal dose tolerance to hypofractionated stereotactic body radiation therapy: risk factors for late toxicity. Int J Radiat Oncol Biol Phys 90:197–102
Dodds WY, Stewart ET, Hodges D et al (1973) Movement of the feline esophagus associated with respiration and peristalsis: an evaluation using tantalum marker. J Clin Invest 52:1–13.
Onimaru R, Shirato H, Schimizu H et al (2003) Tolerance of organs at risk in small volume, hypofractionated, image-guided radiotherapy for primary and metastatic lung cancers. Int J Radiat Oncol Biol Phys 56:126–135
Guckenberger M, Wulf J, Mueller G et al (2009) Dose-response relationship for image-guided stereotactic body radiotherapy of pulmonary tumors: relevance of 4D dose calculation. Int J Radiat Oncol Biol Phys 74:47–54
Kelly P, Balter PA, Rebueno N et al (2010) Stereotactic body radiation therapy for patients with lung cancer previously treated with thoracic radiation. Int J Radiat Oncol Biol Phys 78:1387–1393
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
F. Oskan, G. Becker, and M. Bleif declare that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
Caption Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Oskan, F., Becker, G. & Bleif, M. Specific toxicity after stereotactic body radiation therapy to the central chest. Strahlenther Onkol 193, 173–184 (2017). https://doi.org/10.1007/s00066-016-1063-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-016-1063-z