Abstract
Background
The use of extravascular femoral closure devices in patients undergoing coronary angiography/intervention has not been sufficiently evaluated. We sought to define the impact of an extravascular polyglycolic acid (PGA) plug for the closure of a femoral access site in patients undergoing coronary angiography and/or percutaneous coronary intervention.
Methods
In this prospective, single-blind, multicenter trial we randomly assigned 319 patients to vessel closure with Angio-Seal® or Exo-Seal®. We hypothesized that the use of an extravascular closure device is not inferior to an anchor/plug-mediated device regarding the occurrence of the composite primary endpoint: hematoma > 5 cm, significant groin bleeding (TIMI major bleed), false aneurysm, and device failure.
Results
There was no significant difference in patient baseline characteristics or procedural results. After 24 h the primary endpoint occurred in nine patients (5.6 %) in the Angio-Seal® group and in 13 patients (8.2 %) inthe Exo-Seal® group (p = 0.38). Hematoma > 5 cm was noted in three patients (1.9 %) receiving Angio-Seal® vs. two patients (1.3 %) receiving Exo-Seal® (p = 0.99). In one patient (0.6 %) of the Exo-Seal® group, TIMI major bleeding occurred, requiring transfusion (p = 0.49). There were four (2.5 %) false aneurysms found in patients treated with Angio-Seal® and two (1.3 %) in patients treated with Exo-Seal® (p = 0.68). There was a trend for a higher incidence of device failure in the Exo-Seal® group (1.2 vs. 5.2 %, p = 0.06). At telephone interview after 30 days, there was no significant difference found regarding the events readmission with surgery of puncture site, infection, bleeding, hematoma, or pain.
Conclusion
In the present study, there were no significant differences found regarding the occurrence of hematoma > 5 cm, major bleeding, false aneurysm, and device failure between Angio-Seal® and Exo-Seal® 24 h after device implantation.
Zusammenfassung
Hintergrund
Die Verwendung extravaskulärer Verschlusssysteme für die Femoralarterie bei Patienten mit Koronarangiographie/perkutaner Intervention wurde bisher nicht ausreichend untersucht. Ziel der Autoren war, den Einfluss eines extravaskulären Polyglykolsäure (PGA) Anker basierten Verfahrens auf den Verschluss des Zugangs in der Leiste bei Patienten zu ermitteln, bei denen eine Koronarangiographie und/oder eine perkutane Koronarintervention erfolgte.
Methoden
In der vorliegenden prospektiven, einfach verblindeten Multizenterstudie wurden 319 Patienten randomisiert dem Gefäßverschluss mit Angio-Seal™ oder Exo-Seal® zugeteilt. Die Hypothese der Autoren bestand darin, dass der Einsatz eines extravaskulären Verschlusssystems einem System auf PGA/Ankerbasis im Hinblick auf das Auftreten des kombinierten primären Endpunkts aus Hämatom > 5 cm, erheblicher Blutung in der Leistenregion (schwere Blutung nach TIMI-Kriterien), Aneurysma spurium und „device“-Versagen nicht unterlegen sei.
Ergebnisse
Es fand sich kein signifikanter Unterschied bei den Ausgangsmerkmalen der Patienten oder den Ergebnissen der Prozedur. Nach 24 h trat der primäre Endpunkt bei 9 Patienten (5,6 %) in der Angio-Seal™- und bei 13 Patienten (8,2 %) der Exo-Seal®-Gruppe auf (p = 0,38). Ein Hämatom > 5 cm wurde bei 3 Patienten (1,9 %) unter Verwendung von Angio-Seal™ vs. 2 Patienten (1,3 %) unter Verwendung von Exo-Seal® (p = 0,99) festgestellt. Bei einem Patienten (0,6 %) der Exo-Seal®-Gruppe trat eine schwere Blutung nach TIMI-Kriterien auf, die eine Transfusion notwendig machte (p = 0,49). Es wurden 4 (2,5 %) falsche Aneurysmen bei den mit Angio-Seal™ behandelten Patienten und 2 (1,3 %) bei den mit Exo-Seal® behandelten Patienten (p = 0,68) diagnostiziert. Eine Tendenz zu einer höheren Inzidenz von „device“-Versagen bestand in der Exo-Seal®-Gruppe mit 1,2 vs. 5,2 % (p = 0,06). Bei einer telefonischen Befragung nach 30 Tagen war kein signifikanter Unterschied hinsichtlich der Ereignisse Wiederaufnahme mit chirurgischem Eingriff an der Punktionsstelle, Infektion, Blutung, Hämatom oder Schmerzen festzustellen.
Schlussfolgerung
In der vorliegenden Studie wurden keine signifikanten Unterschiede in Bezug auf das Auftreten eines Hämatoms > 5 cm, einer schweren Blutung, eines falschen Aneurysmas und eines „device“-Versagens zwischen Angio-Seal™ und Exo-Seal® 24 h nach Implantation des Systems festgestellt.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Vascular closure devices (VCDs) were developed to reduce access site bleeding, to improve patient comfort, and to accelerate ambulation after percutaneous coronary interventions (PCI) [1]. Despite higher complications rates in earlier studies [2], recent data suggest similar complication rates or even better outcomes after the use of VCDs as compared with manual compression [3, 4, 5]. Exo-Seal® (Cordis, Warren, N.J.) is an extravascular closure device that uses a polyglycolic acid (PGA) plug to occlude the puncture channel without affecting the inner lumen of the vessel. Whether the use of this extravascular closure device is as effective as the more widely used plug/anchor-mediated devices has not been evaluated to date.
We performed a randomized, multicenter, single-blind trial to prove the efficacy of the extravascular closure device Exo-Seal® in comparison with the collagen-based plug/anchor-mediated Angio-Seal® system.
Methods
Patient population
Between December 2011 and December 2012, patients who underwent either coronary angiography and/or PCI were recruited in three centers in Germany into the ACCESS study. Inclusion criteria were: age > 18 years, femoral access with a 6-Fr sheath, and ability to provide written informed consent. Patients with contraindications for any VCD – including (1) severe calcification of the vessel site, (2) severe peripheral artery disease, (3) puncture in the origin of the femoral profunda artery, (4) nonfemoral sheath insertion, (5) marked tortuosity of the femoral or iliac artery, and (6) marked obesity (BMI > 40) or cachexia (BMI < 20) – were excluded from the study [6, 7]. Patients with puncture in the common femoral artery as well as patients with puncture in the superficial femoral artery were included. A clinical exclusion criterion was continuous medication with oral anticoagulants. Whenever possible, recommendations of the CONSORT statement were applied [8]. The protocol was approved by the ethics committee and all patients gave written informed consent.
Study design and procedures
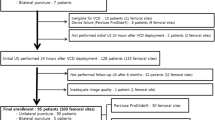
Patients were randomly assigned to treatment with Angio-Seal® or Exo-Seal® after they had undergone angiography/intervention according to standard protocols [9] and exclusion criteria were assessed (Fig. 1). Patients who underwent PCI were loaded with either 300 mg or 600 mg of clopidogrel or 60 mg of prasugrel or 180 mg of ticagrelor, followed by a maintenance dose of 75 mg of clopidogrel or 5 mg or 10 mg of prasugrel, or 90 mg of ticagrelor prior to the intervention. After insertion of a 6-Fr sheath, all patients received 3,000 IU of unfractionated heparin (UF). When PCI was performed after a diagnostic angiography or when an elective PCI was performed, heparin was given until an activated clotting time-level (ACT) of 250 s. Before using the VCD, angiography of the accessed femoral artery was performed to rule out major risk factors for malfunction of the system. Angio-Seal® or Exo-Seal® was implanted when ACT was < 300 s. The use of protamine was allowed. Placement of the device was performed according to the manufacturerʼs recommended technique. The operator had to have used the device at least 50 times. After insertion of the VCD, a circular groin dressing was applied and patients were immobilized for 4 h. After 4 h, the arterial puncture site was examined, and auscultation was performed. If there was no relevant complication, ambulation was initiated.
Anticoagulation either with unfractionated heparin or low-molecular-weight heparin was restarted 6 h after removal of the dressing. On the next day, clinical examination, ultrasound, and Doppler spectral analysis of the puncture site were performed on all patients.
Device description
Angio-Seal® (St. Jude Medical, St. Paul, Minn.) is a collagen-based plug system with a flat, absorbable rectangular anchor, an absorbable collagen plug, and an absorbable suture. Exo-Seal® (Cordis, Warren, N.J.) is a closure device with a bioabsorbable polyglycolic acid (PGA) plug, which is administered to the extravascular space above the arteriotomy using visual guidance (Fig. 2).
Vascular closure devices. a Angio-SealTM (St. Jude Medical, St. Paul, MN, USA). The device is made of three absorbable components: a small anchor, collagen and a suture. The anchor is placed in the artery via a sheath and then drawn against the wall of the artery, while the suture allows the collagen to compact to create a seal over the entry point in the artery. b Exo-Seal® (Cordis Corporation, Warren, N.J.). The Exo-Seal device consists of a Plug Applier and an absorbable Plug. The Plug Applier positions and deploys the absorbable Plug to the extravascular surface of the femoral artery access site. Hemostasis is achieved by a visually guided deployment mechanism, that delivers a bioabsorbable polyglycolic acid “plug” outside the femoral artery. The plug is completely extravascular and is hydrolyzed into CO2 and HO2 within 3 months
Data management and study endpoints
Demographic and procedural data were prospectively collected using a standardized procedural data sheet. This included date and type of intervention, sheath size, procedure-related drug doses, and number of previous interventions. Major or minor complications, as well as the time of events, were recorded.
The primary endpoint was the incidence of vascular complications after 24 h. Vascular complications were defined as hematoma > 5 cm, major bleeding, false aneurysm, and device failure.
Secondary endpoints were hematoma > 5 cm immediately after closure and pain while applying the closure device according to the Borg Scale, as well as after 30 days the presence of hematoma > 5 cm, infection, new bleeding events, any pain at the puncture site, or the necessity for surgical revision.
Bleeding was identified according to the thrombolysis in myocardial infarction (TIMI) criteria [10], and major bleeding was defined as “clinically overt signs of haemorrhage associated with a drop in haemoglobin of ≥ 5 g/dl or fatal bleeding that directly results in death within 7 days.”
Pain during closure procedure was categorized according to the Borg Scale, with minor pain defined as Borg < 5 and major pain as Borg ≥ 5 [11].
Device failure was defined as unsuccessful deployment of the device, either due to technical failure or operator dependent with the consequence of manual compression.
Acute coronary syndrome (ACS) was defined as elevation of creatine kinase (CK) > 140 U/l or elevation of troponin I > 0.5 ng/ml.
Statistical analysis
A noninferiority test was applied for the primary endpoint. The primary endpoint was defined as a composite of bleeding (requiring transfusion), hematoma > 5 cm, false aneurysm, and device failure. To estimate the number of patients per group based on a 1:1 randomization, we tested whether the odds ratio was close to 1.00. Hypotheses are depicted in the odds ratio model as follows:
H0: ln(OR) ≥ δ; H1:ln(OR) < δ.
Assuming an incidence of 5 % for the primary endpoint and a delta of 1.30, the calculated number of patients was 154 patients in each group to achieve 80 % power. This margin was chosen on clinical judgment and subject domain knowledge. Categorical variables were compared using Pearsonʼs χ² test or Fisherʼs exact test, when appropriate. All continuous variables are described as means ± SD. Differences between proportions and t tests were computed with SPSS version 21.0.
Results
A total of 328 patients were randomized, after exclusion of nine patients after peripheral angiography – 161 patients to treatment with Angio-Seal® and 158 to treatment with Exo-Seal®. Of these subjects, 101 patients (62.7 %) of the Angio-Seal® group and 95 (60.1 %) of the Exo-Seal® group underwent diagnostic angiography only. Table 1 shows the baseline characteristics of all patients.
An intervention was performed for treatment of ACS in 39 patients (24.2 %) of the Angio-Seal® group and in 45 patients (28.5 %) of the Exo-Seal® group. There was no patient with ST-elevation myocardial infarction included. Morphological and procedural characteristics are depicted in Table 2.
Procedural results
In patients undergoing PCI, the procedural success rate was 100 % in both groups. Inspection immediately after intervention (secondary endpoint) showed that: hematoma > 5 cm was detected in three patients in each group (1.9 % vs. 1.9 %; p = 0.98), no patient had major bleeding in both groups, pain levels were significantly higher in patients treated with Angio-Seal® (Table 3). In two of 161 patients (1.2 %) who were treated with Angio-Seal® and in eight of 158 patients (5.1 %) who were treated with Exo-Seal®, the device could not be successfully deployed and manual compression was performed (p = 0.06). In patients who had device failure, time to hemostasis was not significantly different between the groups (288 s vs. 234 s; p = 0.61).
Inspection after 24 h (including primary endpoint)
After 24 h, three patients (1.9 %) in the Angio-Seal® group and two patients (1.3 %) in the Exo-Seal group® experienced hematoma > 5 cm (Table 4). One patient (0.6 %) in the Exo-Seal® group had TIMI major bleeding, which required transfusion. After 24 h, ultrasound of the puncture site was performed on all patients. False aneurysms were detected in four patients (2.5 %) treated with Angio-Seal® and in two patients (1.3 %) treated with Exo-Seal®. Of the four false aneurysms found in patients treated with Angio-Seal®, three were treated with thrombin injection and one with manual compression. Of the two patients with false aneurysm in the Exo-Seal® group, one was treated with thrombin injection and one with manual compression. None of the false aneurysms had to be treated with surgery.
Nine patients (5.6 %) in the Angio-Seal® group complained of severe pain vs. four (2.5 %) in the Exo-Seal® group (Borg ≥ 5; (p = 0.26). Arteriovenous fistula was detected via sonography in two patients of the Exo-Seal® group (1.3 %) vs. none in the Angio-Seal® group.
Follow-up after 30 days
During telephone interview after 36.1 ± 35.5 vs. 34.5 ± 30.8 days (follow-up rate, 92.6 %) patients were asked to report the appearance of one or more of the following: surgical revision of the access site, bleeding, new hematoma, infection, pain, or any other problem with the puncture site. One patient in the Exo-Seal® group was readmitted for surgical revision of the access site. No infection of the access site was reported in both groups (Table 5). Of note, 27 patients (19.4 %; Angio-Seal®) vs. 32 (23.5 %, Exo-Seal®; p = 0.46) indicated minor problems such as nervous sensations or problems with hip movement.
Discussion
The present study was conducted to compare the efficacy of the extrafemoral vascular closure device Exo-Seal® with the well-validated plug–anchor system Angio-Seal® for vessel closure after coronary angiography and PCI.
The major finding of our study was that the use of Exo-Seal® was not inferior to treatment with Angio-Seal® with regard to bleeding, hematoma, false aneurysm, and device failure. The use of Exo-Seal® was linked to a higher albeit not significant rate of device failure, and with significantly less pain as measured with the Borg Scale [11].
The occurrence of vascular complications is an independent predictor of nonfatal myocardial infarction or death within 1 year after intervention, and has been associated with a significant increase in mortality [7, 12, 13]. Although early ambulation and even exercise is feasible [14], nearly 20 years after their introduction, it is not definitely clear whetherVCDs are safer than manual compression, since the results of the existing devices are inconsistent. Some authors report lower complications rates [15–18], while others found no differences between VCDs and manual compression [19–24]. On the other hand, unintended consequences, specific for VCDs, such as infections and closure of the accessed artery are reported [25–26]. The most recent meta-analyses still remain conflicting. Smilowitz and coworkers found closure devices to be associated with significantly lower rates of vascular complications compared with primary hemostasis with manual compression [27], while Byrne et al. found that the data do not demonstrate consistent reductions in access-site complications [4]. Biancari et al. reported equal or higher rates of complications [28]. Nevertheless, VCDs are widely and increasingly used in interventional cardiology [29]. Since there is no class effect for closure devices, new devices need careful evaluation and comparison with existing devices.
Over the years, with decreasing sheath sizes, complication rates have dropped from 6 % to less than 1 % in some studies. Depending on the definitions, which vary widely, complications range between 0.9 and 10 %. Chevalier et al. observed a complication rate of 5.9 % in 306 high-risk patients [30]. In a meta-analysis of 12,937 patients undergoing either manual compression or vascular closure, Arora et al. reported complication rates of 2.4 % after PCI and vascular closure with different devices [15]. In the meta-analysis of Smilowitz et al., the complication rate was 0.87 % with a PCI rate of 34.8 % [27]. Overall, complications are reported to be between 0.5 and 1.8 % after angiography and 0.6 and 9 % after PCI [15, 31].
The CLOSE-UP study comparing FemoSeal® with manual compression found a lower rate of large hematomas using FemoSeal®. The primary endpoint was the incidence of hematomas > 5 cm, which was reduced by an absolute 4.5 %, from 6.7 to 2.2 % [3].
Although not significantly different in the two groups, complication rates in our study were higher. Of note, more than 60 % of patients in both groups had more than one intervention through the same vessel, and more than 30 % of the patients presented with elevated troponin levels, a risk factor of adverse outcome regarding the access site itself. Furthermore, no ultrasound of the accessed vessel was performed prior to the intervention, so the exclusion of patients according to the aforementioned criteria was done on the basis of the angiogram alone, which was performed at the end of the procedure and before the use of the VCD.
The high rate of device failure of 5.1 % in the Exo-Seal® group has to be highlighted. In the meta-analysis of Smilowitz et al., failure of device implantation was reported to be in the range of 1.23 % [27]. Implantation failure in the Angio-Seal® group was 1.2 %, being exactly in the range of this analysis. This is a concern, since vascular complication rates in cases of device failure are reported to be up to 10 %. In the present study, all cases of device failure could be solved with manual compression and no further complications were reported. Albeit not significant, since operator experience with each of the two devices was required, this remains a concern for the use of Exo-Seal®.
With decreasing levels of local anesthesia, depending on the complexity of the intervention and therefore the length of the procedure, increasing pain levels with the use of closure devices are reported, since in a minority of procedures the local anesthesia is administered twice [32]. In a subgroup analysis of the CLOSE-UP I Study, reported pain levels, being only detected during the procedure, were significantly higher in patients treated with FemoSeal® compared with manual compression. In our study, pain levels were significantly lower with the use of the extravascular closure device compared with the anchor–plug system.
The existing evidence for the use of Exo-Seal® is poor. Wong and coworkers found a significantly shorter time to hemostasis in 401 patients receiving Exo-Seal® vs. manual compression [33]. The complication rate (minor complications defined as rebleeding, hematoma > 6 cm, access site rebleeding) was 8.5 %. Schmelter et al. demonstrated in 93 patients with an antegrade puncture that the use of the Exo-Seal® system was safe [34].
In a recent analysis by Wiemer et al., the use of a 7-Fr Exo-Seal® system was associated with a shorter time to hemostasis and time to ambulation as compared with manual compression [35]. In a retrospective analysis, Boschewitz and coworkers reported the safety and effectiveness of the Exo-Seal® system citing a very low complication rate of 1.17 % [36].
The ISAR-CLOSURE trial, which was presented recently at the Transcatheter Cardiovascular Therapeutics (TCT) meeting in 2014, compared outcomes after arteriotomy closure with manual compression, FemoSeal®, or Exo-Seal®. After 30 days, the VCD group reported access site complications in 6.9 % compared with 7.9 % in the manual compression group, establishing the noninferiority of VCD.
Based on our data, assuming extrafemoral devices to be as efficient as others, there are some implications and potential advantages of these devices that have to be addressed: First it seems conceivable that there is a possible application opportunity for the use of these devices in patients with contraindications for conventional VCDs, since there is no contact with the inner lumen of the diseased and/or calcified vessel. Second, it seems likely, that with improved operator experience the rates of device failure will drop. Unaddressed issues are the use in patients who are on oral anticoagulants and, as mentioned, in those patients with contraindications for conventional systems. Further studies are necessary to prove the indication of extravascular devices in these patients.
Limitations
The following limitations of the study need to be addressed. According to the study protocol, patients with peripheral vascular disease, calcifications, and insertion of the sheath in the origin of the profunda femoral artery were excluded. Peripheral artery disease was ruled out on the basis of the patient's history, available charts, and the results of the physical examination. A Doppler ultrasound was performed 24 h after the intervention and not before. This information could have had an impact on the results and are thus a limitation. Secondly, we did not compare Exo-Seal® with manual compression. Third, in order to provide comparable conditions for all patients, it was decided to keep a 4-h bedrest after implantation of the device. This may not be similar to real-world practice. Fourth, patients undergoing diagnostic angiography and patients treated with PCI were included in the study. Further, in all patients with diagnostic angiography, heparin was administered at a dose of 3,000 IE. Although the rate of device failure was higher in the Exo-Seal® group, we were not able to identify predictors of device failure in our study. A further limitation is the small sample size, which was calculated only to prove the noninferiority criteria of the primary endpoint.
Conclusion
Our results show that the extravascular closure device Exo-Seal® is not inferior to the well-validated anchor–plug device Angio-Seal®. With a nonsignificant higher rate of device failures, the overall complication rate of Exo-Seal® was similar to that of Angio-Seal®. The role of extravascular VCDs in the treatment of patients with contraindications for a VCD has to be further evaluated.
Abbreviations
- ACS:
-
Acute coronary syndrome
- PCI:
-
Percutaneous coronary intervention
- PGA:
-
Polyglycolic acid
- VCD:
-
Vascular closure device
References
Piper WD, Malenka DJ, Ryan TJ Jr, Shubrooks SJ Jr, OʼConnor GT, Robb JF, Farrel KL, Corliss MS, Hearne MJ, Kellett MA Jr, Watkins MW, Bradley WA, Hettleman BD, Silver TM, Mc Grath PD, OʼMears JR, Wennberg DE (2003) Northern New England cardiovascular disease study group. Predicting vascular complications in percutaneous coronary interventions. Am Heart J 145:1022–1029
Duffin DC, Muhlestein JB, Allison SB, Horne BD, Fowles RE, Sorensen SG, Revenaugh JR, Bair TL, Lappe DL (2001) Femoral arterial puncture management after percutaneous coronary procedures: a comparison of clinical outcomes and patient satisfaction between manual compression and two different vascular closure devices. J Invasive Cardiol 13:354–362
Holm NR, Sindberg B, Schou M, Maeng M, Kaltoft A, Bottcher M, Krusell L, Hjort J, Thuesen L, Terkelsen C, Christiansen E, Botker HE, Kristensen SD, Lassen JF; For the CLOSE-UP study group (2014) Randomised comparison of manual compression and FemoSealTM vascular closure device for closure after femoral artery access coronary angiography: the CLOSure dEvices Used in everyday Practice (CLOSE-UP) study. Eurointervention 9:183–190
Byrne RA, Cassese S, Linhardt M, Kastrati A (2013) Vascular access and closure in coronary angiography and percutaneous intervention. Nat Rev Cardiol 10:27–40
Dauerman LH (2014) Rewriting the history of vascular closure devices. Eurointervention 10:175–177
Applegate R, Sacrinty M, Little W, Gandhi S, Kutcher M, Santos R (2009) Prognostic implications of vascular complications following PCI. Catheter Cardiovasc Interv 74:74–75
Yatskar L, Selzer F, Feit F, Cohen HA, Jacobs AK, Williams DO, Slater J (2007) Access site hematoma requiring blood transfusion predicts mortality in patients undergoing percutaneous coronary intervention: data from the National Heart, Lung, and blood Institute Dynamic Registry. Catheter Cardiovasc Interv 69:961–966
Moher D, Schulz KF, Altman D; for the CONSORT group (2001) The CONSORT statement revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA 285:1987–1991
Silber S, Albertsson P, Aviles FF, Camici PG, Colombo A, Hamm C, Jorgensen E, Marco J, Nordrehaug JE, Ruzyllo W, Urban P, Stone GW, Wijns W; Task Force Members (2005) Guidelines for percutaneous coronary interventions: the task force for Percutaneous Coronary Interventions of the European Society of Cardiology. Eur Heart J 26:804–847
Bovill EG, Terrin ML, Stump DC, Berke AD, Frederick M, Collen D, Feit F, Gore JM, Hillis LD, Lambrew CT (1991) Hemorrhagic events during therapy with recombinant tissue-type plasminogen activator, heparin, and aspirin for acute myocardial infarction. Results of the Thrombolysis in Myocardial infarction (TIMI), Phase II Trial. Ann Intern Med 115:256–265
Borg G (2003) An index for relations between perceptual magnitudes based on level-anchored ratio scaling. In: Berglund B, Borg E (Eds) Fechner Day. International Society for Psychophysics, Stockholm
Omoifui NA, Califf RM, Pieper K, Keeler G, OʼHanesian MA, Berdan LG, Mark DB, Talley JD, Topol EJ (1995) Peripheral vascular complications in the Coronary Angioplasty versus Excisional Atherectomy Trial (CAVEAT-1). J Am Coll Cardiol 26:922–930
Ndrepepa G, Berger PB, Mehilli J, Seyfarth M, Neumann FJ, Schömig A, Kastrati A (2008) Periprocedural bleeding and 1-year outcome after percutaneous coronary interventions: appropriateness of including bleeding as a component of a quadruple end point. J Am Coll Cardio 51:690–697
Rittger H, Schmidt M, Breithardt OA, Mahnkopf C, Brachmann J, Sinha AM (2011) Cardio-respiratory exercise testing early after the use of the Angio-Seal system for arterial puncture site closure after coronary angioplasty. Eurointervention 7:242–247
Arora N, Matheny ME, Sepke C, Resnic FS (2007) A propensity analysis of the risk of vascular complications after cardiac catheterization procedures with the use of vascular closure devices. Am Heart J 153:606–611
Resnic FS, Blake GH, Ohno-Machado L, Swlwyn AP, Popma JJ, Rogers C (2001) Vascular closure devices and the risk of vascular complications after percutaneous coronary intervention in patietns receiving glycoprotein IIb-IIIa inhibitors. Am J Cardiol 88:493–496
Tavris DR, Gallauresi BA, Lin B, Rich SE, Shaw RE, Weintraub WS, Brindis RG, Hewitt K (2004) Risk of local adverse events following cardiac catheterization by hemostasis device use and gender. J Invasive Cardiol 16:459–464
Marco SP, Amin AP, House JA, Kennedy KF, Sperus JA, Rao SV, Cohen DJ, Messenger JC, Rumsfeld JS; National Cardiovascular Dtat Registry (2010) Association between use of bleeding avoidance strategies and rik of periprocedural bleeding among patients undergoing percutaneous coronary intervention. JAMA 303:2156–2164
Nikolsky E, Mehran R, Halkin A, Aymong ED, Mintz GS, Lasic Z, Negoita M, Fahy M, Krieger S, Moussa I, Moses JW, Stone GW, Leon MB, Pocock SJ, Dangas G (2004) Vascular complications associated with arteriotomy closure devices in patients undergoing percutaneous coronary procedures: a meta-analysis. J Am Coll Cardiol 44:1200–1209
Deuling JH, Vermeulen RP, Anthonio RA, van den Heuvel AF, Jaarsma T, Jessrung G, de Smet BJ, Tan ES, Zijlstra F (2008) Closure of the femoral artery afere cardiac catheterization: a comparison of Angio-Seal, StarClose, and manual compression. Catheter Cardiovasc Interv 71:518–523
Applegate RJ, Sacrinty MT, Kutcher MA, Baki TT, Gandhi SK, Santos RM, Little WC (2006) Propensity score analysis of vascular comolications after diagnostic cardiac catherziuation and percutaneous coronary intervention 1998–2003. Catheter Cardiovasc Interv 67:556–562
Exaire JE, Dauerman HL, Topol EJ, Blankenship JC, Wolski K, Raymond RE, Cohen EA, Moliterno DJ; TARGET Investigators (2004) Triple antiplatelet therapy does not increase femoral access bleeding with vascular closure devices. Am heart J 147:31–34
Tron C, Kning R, Eltchaninoff H, Douillet R, Chassaing S, Sanchez-Giron C, Cribier A (2003) An randomized comparison of a percutaneous suture device versus manual compression for femoral artery hemostais after PTCA. J Interv Cardiol 16:217–221
Cura FA, Kapadia SR, LʼAllier PL, Schneider JP, Kreindel MS, Silver MJ, Yadav JS, Simpfendorfer CC, Raymond RR, Tuzcu EM, Franco I, Whitlow PL, Topol EJ, Ellis SG (2000) Safety of femoral closure devices after percutaneous coronary interventions in the era of glycoprotein IIb/IIIa platelet blockade. Am J Cardiol 86:780–782
Brueck M, Bandorski D, Rauber K, Boening A (2010) Percutaneous transluminal dilatation of inadvertent parital or complete occlusion of the femoral artery caused by Angio-Seal deployment for puncture site closure after cardiac catheterization. J Invasive Cardiol 303:2156–2164
Applegate RJ (2010) Unintended consequences of femoral artery closure devices. J Invasive Cardiol 22:353–357
Smilowitz N, Kirtane A, Guiry M, Gray W, Dolcimascolo P, Querijero M, Echeverry C, Kalcheva N, Flores B, Sing VP, rabbani LR, Kodali S, Collins M, Leon B, Mosis J, Weisz G (2012) Practices and complications of vascular closure devices and manual compression in patients undergoing elective transfemoral coronary procedures. Am J Cardiol 110:177–182
Biancari F, Andrea VD, Di Mario C, Savino G, Tiozzo V, Catania A (2010) Meta-analysis of randomized trials on the efficadcy of vascular closure devices afer diagnostic angiography and angioplasty. Am Heart J 159:518–531
Turi ZG (2008) An evidence-based approach to femoral arterial access and closure. Rev Cardiovasc Med 9:6–18
Chevalier B, Lancelin B, Koning R, Henry M, Gommeaux A, Pilliere R, Lefevre T, Boughalem K, Marco J, Dupouy P; Hemostase Trial Investigators (2003) Effect of a closure device on complication rates in high-local-risk patients: results of a randomized multicentre trial. Catheter Cardiovasc Interv 58:285–291
Eggebrecht H, Haude M, Woertgen U, Schmermund A, von Birgelen C, Naber C, Baumgart D, Kaiser C, Oldenburg O, Bartel T, Kroeger K, Erbel R (2002) Sysmtetic use of a collagen-based vascular closure device immediately after cardiac catheterization procedures in 1,317 conscutive patients. Catheter Cardiovac Interv 57:486–495
Sindberg B, Schou M, Hansen L, Christiansen KJ, Jǿrgensen KS, Sǿltoft M, Holm NR, Maeing M, Kristensen SD, Lassen JF (2013) Pain and discomfort in closure of femoral accesss coronary angiography. The CLOSuredEvices used in everyday practice (CLOSE-UP) pain sub study. Eur J Cardiovasc Nurs 13:221–226
Wong SC, Bachinsky W, Cambier P, Stoler R, Aji J, Roger J, Hermiller J, Nair R, Hutman H, Wang H (2009) A randomized comparison of a novel bioabsorbable vascular closure device versus manual compression in the achievement of hemostatis after percutaneous femoral procedures. J Am Coll Cardiol Intv 2:785–793
Schmelter C, Liebl A, Poullos N, Ruppert V, Vorwerk D (2013) Suitability of Exo-Seal closure device for antegrade femoral artery puncture site closure. Cardiovasc Intervent Radiol 36:659–668
Wiemer M, Langer C, Fichtlscherer S, Firschke C, Hofbauer F, Lins M, Haude M, Debéfve C, Stoll HP, Hanefeld C (2012) First-in-man experience with a new 7F vascular closure device (EXOSEALTM): the 7F ECLIPSE study. J Interv Cardiol 5:518–525
Boschewitz JM, Andersson M, Naehle CP, Schild HH, Wilhelm K, Meyer C (2013) Retrospective evaluation of safety and effectiveness of the Exo-Seal vascular closure device for single vascular closure and closure after repeat puncture in diagnostic and interventional radiology: single center experience. J Vasc Interv Radiol 24:698–702
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Ketterle, H. Rittger, I. Helmig, L. Klinghammer, S. Zimmermann, W.Hohenforst-Schmidt, J. Brachmann, H. Nef, S. Achenbach, C. Schlundt state that there are no conflicts of interest.
Additional information
J. Ketterle and H. Rittger contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Ketterle, J., Rittger, H., Helmig, I. et al. Comparison of Exo-Seal® and Angio-Seal® for arterial puncture site closure. Herz 40, 809–816 (2015). https://doi.org/10.1007/s00059-015-4306-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-015-4306-3