Abstract
Purpose
To assess the efficacy and safety of the Exoseal vascular closure device for antegrade puncture of the femoral artery.
Methods
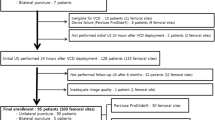
In a prospective study from February 2011 to January 2012, a total of 93 consecutive patients received a total of 100 interventional procedures via an antegrade puncture of the femoral artery. An Exoseal vascular closure device (6F) was used for closure in all cases. Puncture technique, duration of manual compression, and use of compression bandages were documented. All patients were monitored by vascular ultrasound and color-coded duplex sonography of their respective femoral artery puncture site within 12 to 36 h after angiography to check for vascular complications.
Results
In 100 antegrade interventional procedures, the Exoseal vascular closure device was applied successfully for closure of the femoral artery puncture site in 96 cases (96 of 100, 96.0 %). The vascular closure device could not be deployed in one case as a result of kinking of the vascular sheath introducer and in three cases because the bioabsorbable plug was not properly delivered to the extravascular space adjacent to the arterial puncture site, but instead fully removed with the delivery system (4.0 %). Twelve to 36 h after the procedure, vascular ultrasound revealed no complications at the femoral artery puncture site in 93 cases (93.0 %). Minor vascular complications were found in seven cases (7.0 %), with four cases (4.0 %) of pseudoaneurysm and three cases (3.0 %) of significant late bleeding, none of which required surgery.
Conclusion
The Exoseal vascular closure device was safely used for antegrade puncture of the femoral artery, with a high rate of procedural success (96.0 %), a low rate of minor vascular complications (7.0 %), and no major adverse events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last two decades, a variety of vascular closure devices have become available for arterial puncture site closure in patients undergoing percutaneous transfemoral diagnostic or interventional; coronary or peripheral procedures. Vascular closure devices have been developed to achieve quick hemostasis and early ambulation in patients after sheath removal and conclusion of diagnostic or interventional procedures without compromising safety compared to traditional manual compression. The goal is to limit patient discomfort compared to manual compression [1, 2].
In June 2010, a novel vascular closure device, Exoseal (Cordis Europe, Waterloo, Belgium), was introduced that achieves hemostasis by means of a visually guided deployment mechanism that delivers a bioabsorbable polyglycolic acid plug atop the femoral artery, anchored by the neurovascular bundle sheath [3, 4]. The device is designed for the closure of femoral artery puncture sites in patients who have undergone diagnostic or interventional procedures. The vascular closure device is available in three sizes (5F, 6F, 7F), and it may be combined with standard introducer sheaths. The Exoseal device delivers a synthetic bioabsorbable polyglycolic acid plug to the extravascular space adjacent to the arterial puncture site using visual guidance for vascular closure. The plug, which is entirely extravascular, is subsequently hydrolyzed into CO2 and H2O via the Krebs cycle over a 3 month period [3, 4].
The safety and efficacy of the of Exoseal vascular closure device were evaluated in a prospective multicenter randomized clinical trial in the United States; this study, the ECLIPSE trial, compared the Exoseal vascular closure device (6F) to manual compression. A total of 401 patients and 87 “roll-in” patients underwent a diagnostic or interventional coronary or peripheral procedure via common femoral artery puncture. Femoral artery closure in antegrade peripheral diagnostic or interventional procedures was not specifically evaluated [4].
Cordis states in the Exoseal vascular closure device use instructions, “The safety and effectiveness of the Exoseal vascular closure device has not been established for patients with antegrade puncture.” Even though antegrade puncture is not a contraindication for use, the precautions for the device indicate that “with antegrade puncture, the ability to accurately assess vessel size or extraluminal device position may be limited” [3].
The current study was designed to assess the efficacy and safety of the Exoseal vascular closure device, especially for antegrade puncture closure of the femoral artery in interventional procedures.
Patients and Methods
Patients
From February 2011 to January 2012, a total of 93 patients who underwent 100 consecutive interventional procedures via antegrade puncture of the femoral artery were included in a prospective study. Five patients received two consecutive interventional procedures; one patient was treated three times. The average age of treated patients was 76 ± 9 years. Of the 93 total patients, 42 were female and 51 were male (54.8 %; M:F 1.2:1.0). Data of body height and weight were documented in 87 cases; the average body mass index (BMI) of patients was 27.5 ± 3.8 kg/m2 (male 27.8 ± 3.5 kg/m2; female 27.1 ± 4.0 kg/m2). BMI ranged 18.7 to 35.9 kg/m2.
All patients were part of the daily routine in the department. Every patient who was going to receive an antegrade interventional procedure was considered for inclusion in the study. Patients who were not available for a follow-up visit 12 to 36 h after the conclusion of the interventional procedure were excluded from the study. The decision to use the Exoseal vascular closure device in a specific case was up to the interventional radiologist.
In 100 antegrade interventional procedures, 58 patients (58.0 %) had grade 4 peripheral vascular disease according to the Fontaine classification. Six cases (6.0 %) were considered to be grade 3 and 36 cases (36.0 %) grade 2b.
The procedures were performed in accordance with institutional guidelines. All subjects provided written informed consent. Approval of the local ethics committee was not required.
Interventional Procedure
A total of 96 of 100 antegrade interventional procedures were carried out by a single person with extensive experience in diagnostic and interventional procedures and use of vascular closure devices. In four cases, interventional procedures were performed by two further consultants, also skilled angiographers.
Safe access to the common femoral artery and the superficial femoral artery was obtained by the Seldinger technique with an 18-gauge needle and a 0.035 in. J wire (Terumo Europe, Leuven, Belgium). Scandicain (mepivacaine hydrochloride) was used for subcutaneous and perivascular local anesthesia. In all cases, the vascular sheath introducer (6F) with a Terumo dilatator was used. An Exoseal vascular closure device (6F) was used for closure in all cases. Angiographic fluoroscopy was performed and x-ray images were taken by Siemens Multistar Top fluoroscope (Siemens AG, Munich, Germany).
After the catheterization procedure, manual compression of the respective femoral artery access site was applied for at least 2 min. Patients were confined to bed for 6 h after the interventional procedure.
Follow-up
All patients were monitored by vascular ultrasound of their respective femoral artery puncture site within 12 to 36 h after the interventional procedure. Vascular ultrasound was used for display of the femoral artery puncture site and to check for minor and major vascular complications. Ultrasound examinations were carried out with Z.one Ultra Convertible Ultrasound system (Zonare Medical Systems, Mountain View, CA). An 18–3 linear array was used for two-dimensional and color-coded duplex ultrasonography of the femoral artery puncture site.
Vascular ultrasound was carried out to check for any vascular complication, but the primary focus was on pseudoaneurysm, arteriovenous fistula, retroperitoneal bleeding, stenosis, and thrombosis with resulting vascular insufficiency or embolization of the punctured femoral artery. Patients were also examined for recurrent and significant late bleeding, local infection, and nerve injury.
Before physical examination and color-coded duplex ultrasonography of the respective artery puncture site, patients were asked whether they still felt any pain at the puncture site and to define the level of pain on a scale from 1 (minimal pain) to 10 (maximum pain).
Study End Points
The primary efficacy end point was defined as successful closure of the respective femoral artery puncture site achieved by use of Exoseal vascular closure device after an antegrade interventional procedure.
The secondary efficacy end point was quick hemostasis within 2 min of manual compression after removal of the introducer sheath and conclusion of the interventional procedure.
Procedural success was defined as hemostasis achieved by the use of Exoseal vascular closure device without occurrence of closure-related major vascular complications in 12 to 36 h after the interventional percutaneous vascular procedure.
The primary safety end point was the rate of major vascular complications and major adverse events related to the femoral artery puncture site 12 to 36 h after the antegrade interventional procedure. In accordance with the ECLIPSE trial, major vascular complications were defined as follows: (1) need for vascular repair by surgical or nonsurgical techniques; (2) bleeding requiring a blood transfusion; (3) infection requiring antibiotics; (4) new-onset ischemia of the ipsilateral lower extremity; (5) need for surgical repair of access-site-related nerve injury; or (6) permanent access-site-related nerve injury [4].
The secondary safety end point was the rate of arterial closure-related minor vascular complications. Minor vascular complications were defined as follows: (1) recurrent local bleeding requiring a hemostatic intervention, or a ≥6 cm hematoma or ecchymosis; (2) development of pseudoaneurysm, arteriovenous fistula, vascular laceration, or retroperitoneal bleeding; (3) ipsilateral manifestations of vascular insufficiency or embolization, including loss of distal pulse, total arterial occlusion, or deep vein thrombosis; (4) infection; and (5) nerve injury [4].
Results
Access, Device Deployment, and Time to Hemostasis
In 100 interventional procedures, the left common femoral artery was punctured 41 times (41.0 %). Vascular access was established via the right common femoral artery in 58 cases (58.0 %). In one instance (1.0 %), the left superficial femoral artery was intentionally punctured instead. Successful access to the common femoral artery and the superficial femoral artery could be obtained by single-wall vessel puncture in 82 cases (82.0 %); in 18 cases (18.0 %), vascular access was achieved by puncture of the opposing vessel walls. In 14 cases (14.0 %), more than a single puncture of the artery was needed for vascular access. More than one vascular access point was used during the angiographic procedure in three cases (3.0 %).
Five patients underwent two consecutive interventional procedures during this study. In two cases, the angiographic procedure was performed on each leg once. Three patients were treated a second time on the same side. One patient was treated three times; in this case, interventional procedures were performed two times on the same leg and once on the opposite leg. In patients who underwent a second interventional procedure on the same leg, the time between consecutive procedures ranged 52–209 days.
In 100 interventional angiographic procedures, angioplasty was performed in each case. Vascular stenting was necessary in 17 cases (17.0 %).
In 100 antegrade interventional angiographic procedures, the Exoseal vascular closure device was applied successfully for closure of the femoral artery puncture site in 96 cases (96.0 %). In five cases, a minor problem of kinking occurred, but successful vascular closure was still achieved.
In one case (1.0 %), the Exoseal device could not be properly used because of kinking of the vascular sheath introducer. In three cases (3.0 %), the resorbent plug of the Exoseal device could not be deployed at the femoral artery puncture site because the vascular closure device itself malfunctioned. In these three cases, the bioabsorbable plug was not properly delivered to the extravascular space adjacent to the arterial puncture site but was instead fully removed with the delivery system.
Quick hemostasis within 2 min of manual compression after removal of the introducer sheath was achieved in 86 cases (86.0 %). After the catheterization procedure was completed, the femoral access sites of 14 patients (14.0 %) were still bleeding after 2 min of manual compression. Prolonged bleeding occurred in 12 cases in which the Exoseal vascular closure device was deployed properly; in two cases, the Exoseal device could not be deployed, either as a result of problems with the vascular sheath introducer or as a result of device malfunction. Time to hemostasis was documented in eight of 14 cases if not achieved within 2 min of manual compression; in six cases, prolonged time to hemostasis was not recorded. In eight cases, the mean time to hemostasis with prolonged manual compression after not achieving hemostasis within 2 min was 7.9 ± 4.5 min.
Patients were treated with compression bandages on their puncture sites after angiographic intervention in 32 (32.0 %) of 100 cases. Compression bandages were used in 24 cases where quick hemostasis was obtained within 2 min of manual compression because of patient obesity. In 8 of 14 cases of prolonged time to hemostasis (>2 min with manual compression), compression bandages were applied.
Complications
The average age of patients with minor problems of kinking (although the antegrade interventional procedure was successfully finalized) was 76 ± 6 years. In comparison, the average age of all treated patients was 76 ± 9 years. The age of the single patient with vascular closure device failure that resulted from kinking of the flexible sheath introducer was 80 years. The average age of patients whose vascular closure devices malfunctioned—specifically, the bioabsorbable plug was removed with the delivery system—was 72 ± 6 years.
All patients with minor problems of kinking were male, as was the patient with device malfunction due to kinking of the sheath introducer. Two of three patients with vascular closure device malfunction because of plug removal were female.
Data of body height and weight were available for the single patient with vascular closure device failure due to kinking of the flexible sheath introducer; in this patient, BMI was 29.1 kg/m2, and an overhanging “apron” was evident. The average BMI of patients with minor kinking problems was 26.8 ± 2.8 kg/m2. In three cases, the Exoseal vascular closure device malfunctioned because the plug was removed with the delivery system; the average BMI for these patients was 29.8 ± 4.9 kg/m2.
Calcification of the common femoral artery and the superficial femoral artery was not documented. According to the interventional radiologists, arterial calcification did not affect the vascular closure procedure because of the entirely extravascular design of the closure device and the bioabsorbable polyglycolic acid plug.
Minor and Major Complications
Twelve to 36 h after the antegrade interventional procedure, there was no evidence of major vascular complications or major adverse events, as demonstrated by physical examination and vascular ultrasound of the femoral artery puncture site (Table 1). No patient required surgical intervention or blood transfusion.
Minor vascular complications after antegrade puncture of the femoral artery were found in 7 (7.0 %) of 100 cases, with four cases (4.0 %) of pseudoaneurysms and three cases (3.0 %) of recurrent bleeding.
The average maximum diameter of the four pseudoaneurysms was 2.1 ± 0.6 cm.
Patients with vascular complications were reviewed by a second ultrasonographer, and the diagnosis was confirmed in all cases.
Arteriovenous fistula, vascular laceration, retroperitoneal bleeding, stenosis, and thrombosis of the femoral artery with resulting vascular insufficiency or embolization were not encountered. No patient had an infection or nerve injury within 12 to 36 h after conclusion of the antegrade interventional procedure.
Hematomas were observed in 10 (10.0 %) of 100 cases, with an average maximum diameter of 2.8 ± 1.2 cm. There was no patient with a hematoma or ecchymosis ≥6 cm. In all patients with hematomas, the vascular closure devices had been successfully deployed. One patient with significant late bleeding and one patient with pseudoaneurysm developed also hematomas at their femoral artery access sites.
In 99 interventional procedures, only 7 (7.1 %) patients reported persistent pain at their respective artery puncture site 12 to 36 h after femoral artery puncture. (In one case, the patient could not respond properly to the question because of dementia.) None of these patients experienced a minor or major complication after the antegrade interventional procedure. A malfunction of the vascular closure device occurred in only one patient with persistent arterial puncture site–related pain. The mean pain level on a scale from 1 (minimal pain) to 10 (maximum pain) was 5.4 ± 1.6 for these seven patients.
Three cases of pseudoaneurysm were treated successfully by ultrasound-guided thrombin injection. One case of pseudoaneurysm and all cases of significant later bleeding were treated with compression bandages. No surgical intervention was needed.
Analysis of Patients with Minor Complications
For significant late bleeding, the mean age of patients was 73 ± 17 years; the average age of patients with pseudoaneurysm was 79 ± 4 years, compared to 76 ± 9 years for the total cohort.
Two (50.0 %) of 4 patients with pseudoaneurysm as a vascular complication were male; 2 (66.7 %) of 3 patients with significant late bleeding were male. There was no obvious difference in preference of the left common femoral artery, right common femoral artery, or left superficial femoral artery for vascular complications.
In two of three cases of recurrent bleeding data of body height and weight were documented; the average BMI of these two patients was 25.1 ± 6.1 kg/m2 compared to an average BMI of all patients of 27.5 ± 3.8 kg/m2 (n = 87). BMI of patients with pseudoaneurysm was available in three of four cases and was 26.1 ± 3.6 kg/m2.
For all patients with minor vascular complications, femoral arterial puncture was straightforward, with only a single attempt for single-wall puncture. No patient with vascular complications needed more than one arterial access site during interventional procedure.
Angioplasty was performed in every patient with significant late bleeding. One patient with significant late bleeding was considered to have high-grade peripheral vascular disease (grade 4). All patients with pseudoaneurysm after the interventional procedure were considered to have grade 4 peripheral vascular disease and were treated with angioplasty. The Exoseal vascular closure device was successfully deployed in all patients with significant late bleeding; a minor kinking of the vascular introducer sheath occurred in one of these patients. There were two patients with significant late bleeding whose femoral artery access sites were still bleeding after the conclusion of the catheterization procedure and 2 min of manual compression, including the one patient with minor kinking of the sheath introducer during deployment of the vascular closure device. Both patients received compression bandages on their femoral arterial access sites.
All pseudoaneurysms occurred in patients with successful deployment of the Exoseal vascular closure device finalizing the interventional procedure. Bleeding of the vascular access site after 2 min of manual compression was evident in a single patient with late pseudoaneurysm. Manual compression was continued in that case until the bleeding stopped, and no compression bandage was applied. Another patient who developed a pseudoaneurysm later on was treated with a compression bandage although bleeding at the vascular access site had stopped within 2 min of manual compression. Out of six patients with two or three consecutive interventional procedures, only one experienced a vascular-site-related complication, and the specific vascular complication—pseudoaneurysm—occurred at the first of two consecutive interventions on the same side.
Coagulation
All three patients with significant late bleeding showed derangements of their coagulation parameters before the interventional procedure, including derangements of prothrombin time (PT, Quick), activated partial thromboplastin time (aPTT), and international normalized ratio (INR). Of four cases with pseudoaneurysm after antegrade arterial puncture closure, there were two patients with deranged coagulation parameters before the interventional procedure.
In 91 of 100 cases, anticoagulant therapy after interventional procedure was documented. In most cases (41 of 91, 45.1 %), patients were treated with a combination of acetylsalicylic acid p.o., clopidogrel p.o., and heparin i.v.; in 30 cases (33.0 %), patients only received heparin i.v. for anticoagulation; in seven cases (7.7 %), anticoagulant therapy consisted of acetylsalicylic acid p.o. and heparin i.v.; three patients (3.3 %) were treated solely with heparin s.c.; in two cases each (2.2 %), patients received either acetylsalicylic acid p.o. and clopidogrel p.o. or acetylsaliclic acid p.o. and heparin s.c. or a combination of acetylsalicylic acid p.o., clopidogrel p.o., and heparin s.c.; one patient (1.1 %) was treated with clopidogrel p.o. and heparin i.v., and another patient (1.1 %) received heparin i.v. and s.c. Two patients (2.2 %) did not receive any anticoagulation therapy after interventional procedure.
Discussion
A variety of vascular closure devices have been developed over the last two decades to achieve fast hemostasis, shorten time to ambulation, and improve comfort for patients undergoing percutaneous diagnostic or interventional vascular procedures. The safety of these devices should not be compromised compared to manual compression [1, 2]. Although most of these vascular closure devices have been tested for retrograde vascular procedures (e.g., cardiac catheterization), vascular closure devices are also used in diagnostic or interventional antegrade procedures (e.g., percutaneous transluminal angioplasty in patients with peripheral vascular disease).
Compared to the scientific literature available describing the use of vascular closure devices in retrograde percutaneous vascular procedures, the data for the use of vascular closure devices for closure of antegrade puncture sites are limited.
Exoseal
The 2009 ECLIPSE trial by Wong et al. remains the only available scientific article that evaluated the novel Exoseal vascular closure device (6F) in terms of procedural success and device safety [4]. In this study, 401 patients and 87 “roll-in” patients underwent diagnostic or interventional coronary or peripheral procedure, but there was no differentiation into use of Exoseal vascular closure device for antegrade or retrograde puncture closure. It is important to note that 49.9 % of procedures in the ECLIPSE trial were diagnostic in nature, compared to 100.0 % of interventional procedures in the current study.
Procedural success, defined as hemostasis achieved by the use of Exoseal vascular closure device without occurrence of closure-related major vascular complications, was 91.8 % (245 of 267) in the ECLIPSE trial, compared to 96.0 % (96 of 100) in the current study (Table 2) [4].
Device success, defined as uncomplicated deployment of the plug, removal of an intact delivery system, and hemostasis achieved in ≤5 min, was 89.1 % (238 of 267) in the ECLIPSE trial. Comparison between device success rates of the ECLIPSE trial and the current study is limited as a result of the definition of quick hemostasis of ≤2 min in the current study (86 of 100, 86.0 %) [4].
No major vascular complications or major adverse events related to the arterial closure were observed in the current study or in the ECLIPSE trial.
The combined event rate of secondary adverse events or minor vascular complications was 9.0 % (24 of 267) in the ECLIPSE trial. The minor complication rate was 15.0 % (20 of 133) in interventional patients only, compared to a minor complication rate of 7.0 % (7 of 100) in the current study [3, 4].
Compared to the ECLIPSE trial evaluating the Exoseal vascular closure device for diagnostic or interventional coronary or peripheral procedures, the current study shows similar results in terms of efficacy and safety for use in antegrade punctures only [4].
Other Vascular Closure Devices
The use of vascular closure devices other than Exoseal for closure of antegrade puncture sites in diagnostic and interventional procedures was evaluated in a small number of publications. Compared to the procedural success rates and major and minor complication rates of other vascular closure devices, the Exoseal vascular closure device is noninferior in terms of efficacy and safety compared to the Angio-Seal, Perclose, and StarClose devices (Table 2).
Angio-Seal
The efficacy and safety of the Angio-Seal vascular closure device (St. Jude Medical, St. Paul, MN) after antegrade puncture was evaluated in a prospective study with 120 obese patients by Minko et al. [5]. Hemostasis was achieved in 97 (80.8 %) of 120 cases with the Angio-Seal vascular closure device (6F and 8F). In 12 (10.0 %) of 120 cases, additional manual compression was required. In nine patients, the vascular closure device could not be deployed properly because of kinking of the sheath, and in two patients, the anchor of the Angio-Seal device dislodged out of the vessel.
Reekers et al. [6] evaluated a vascular closure device with anchor and plug (Angio-Seal) regarding safety and effectiveness in a multicenter study including 1107 patients. Antegrade access was performed in 15.3 % of all interventions. Deployment failure was 8.8 % for antegrade access. Before discharge, the access site complication rate was 4.0 % for antegrade access, and serious complications were reported in 1.2 % for antegrade and retrograde access, including two false aneurysms, six hematomas >5.9 cm, one case of significant bleeding, two vessel occlusions, and two vessel dissections. Furthermore, serious complications during follow-up were reported separately with a rate of 1.3 % for antegrade and retrograde access (including false aneurysms, hematoma >5.9 cm, vessel occlusion, partial occlusion of the vessel, and severe pain at the access site). It should be noted that only patients who returned spontaneously with a puncture site-related problem were assessed.
Lupattelli et al. [7] evaluated the Angio-Seal vascular closure device (6F) in antegrade common femoral artery punctures during endovascular procedures in a large study with 1889 diabetic patients with critical limb ischemia. The success rate for achieving hemostasis after antegrade puncture and device deployment was 97.9 %. Major vascular complications after antegrade puncture were encountered in 1.1 % (20 of 1,889), and the overall complication rate (major and minor complications combined) was 2.5 %.
In a retrospective study of 60 consecutive patients by Looby et al. [8], the Angio-Seal vascular closure device was evaluated for closure after antegrade common femoral artery puncture. Deployment of the Angio-Seal device failed in 4 (8.0 %) of 50 cases. There were no major complications recorded for the Angio-Seal device.
Use of the Angio-Seal STS and VIP vascular closure devices was retrospectively evaluated for antegrade puncture via the common femoral artery by Kapoor et al. [9]. The technical success rate (6F and 8F) in 55 patients was 98.2 % (55 of 56 procedures). No major vascular complications were encountered. There was no minor vascular complication as defined by the current study. Two patients developed small hematomas <6 cm.
Biondi-Zoccai et al. [10] performed a study with a small number of patients (n = 5) for evaluation of the efficacy and safety of the Angio-Seal vascular closure device after antegrade femoral arteriotomy. Hemostasis was achieved immediately by use of the Angio-Seal device in all cases; no major complications were observed.
Mukhopadhyay et al. [11] encountered one instance each of hematoma and worsening ischemia (4.8 %) in a series of 21 cases with the Angio-Seal device in antegrade puncture.
Malpositioning the Angio-Seal vascular closure device in antegrade or retrograde femoral artery closure attempts may result in traumatic dissection or occlusion of the femoral artery as a result of the intravascular position of the device’s anchor [12].
Perclose
In 2008, Chiu et al. [13] retrospectively compared the Angio-Seal vascular closure device (6F and 8F) to the Perclose ProGlide suture-mediated closure device (6F; Abbott Vascular, Redwood City, CA) in terms of efficacy and safety for closure in antegrade and retrograde common femoral artery punctures during peripheral angioplasty procedures. The failure rate for antegrade puncture closure was 11.1 % (2 of 18) with Angio-Seal and 38.7 % (12 of 31) with the Perclose vascular closure device. Minor complications were encountered in 27.8 % (5 of 18) with Angio-Seal and in 35.5 % (11 of 31) with Perclose ProGlide after closure of the antegrade puncture site.
A prospective study with 80 consecutive patients by Duda et al. in 1999 [14] investigated the efficacy and safety of the Perclose Techstar (6F and 7F) and ProStar Plus (8F) vascular closure devices. Mean time to hemostasis was 5.2 ± 3.8 min (n = 78). The procedural success rate was 96.3 % (77 of 88), with two cases of device deployment failure and one case of retroperitoneal bleeding. The successful device deployment rate was 97.5 % (78 of 80). The rate of major complications was 1.3 % (1 of 80), with a case of retroperitoneal hematoma requiring blood transfusion and surgical repair. Minor complications were encountered in 5 (6.3 %) of 80 patients, with one case of pseudoaneurysm, one case of lymphatic fistula, and three cases of hematomas (3–5 cm in diameter).
In 2001, Hahn et al. [15] evaluated the Perclose Closer suture-mediated closure device (6F and 7F; Abbott Vascular) and encountered three deployment failures (60.0 %) in five antegrade punctures; two were rescued by insertion of a second device.
StarClose
The StarClose vascular closure device (Abbott Vascular) was evaluated in a large study by Spiliopoulos et al. in 2011 [16] for achieving hemostasis after antegrade or retrograde femoral artery catheterization during peripheral angioplasty procedures (6F, 7F, 8F). The hemostasis success rate was 93.9 % (1,139 of 1,213), with 237 (20.8 %) of these 1,139 requiring additional manual compression for <5 min. In 1.1 %, the nitinol clip could not be delivered properly (13 of 1,213), resulting in a device success rate of 98.9 %. Overall major and minor complication rates were reported as 0.3 % (4 of 1,213) and 5.3 % (64 of 1,213), respectively.
Chiu et al., in a 2010 study [17], encountered a 10.0 % (4 of 40) failure rate of the StarClose vascular closure device deployment in antegrade puncture closures. There was no major complication observed after use of the StarClose device. The total minor complication rate was 22.5 % (9 of 40) after antegrade punctures.
Fantoni et al. in 2008 [18] reported a procedural success rate of 100.0 % and no major local vascular complications during a 30 day follow-up for use of a clip-based arterial closure device after ipsilateral antegrade common femoral artery puncture in 30 patients with critical limb ischemia.
Obesity, Kinking of the Flexible Sheath Introducer, and Arterial Calcification
In the current study, obesity could not be unambiguously determined as a predictor for procedural difficulties or vascular complications. On the one hand, vascular closure device malfunction due to kinking of the flexible sheath introducer was connected to a high BMI (29.1 vs. 27.5 kg/m2, n = 1 vs. n = 87), and on the other hand, the average BMI of patients with minor problems of kinking and successful antegrade puncture site closure was lower than the total cohorts’ BMI (26.8 vs. 27.5 kg/m2, n = 5 vs. n = 87). Patients with malfunction of the vascular closure device due to plug removal with the delivery system were heavier than the average BMI for all patients (29.8 vs. 27.5 kg/m2, n = 3 vs. n = 87). The BMI of patients with vascular complications was lower than the average BMI (significant late bleeding: 25.1 kg/m2, n = 2; pseudoaneurysm: 26.1 kg/m2, n = 3).
Minko et al. in 2012 [5] reported obesity as an independent risk factor for insufficient sealing of the antegrade femoral artery puncture site with the Angio-Seal vascular closure device (26.6 vs. 28.8 kg/m2). In contrast, obesity and local arterial calcification were not regarded as predictors for deployment failure in a study by Reekers et al. [6] utilizing the Angio-Seal vascular closure device for antegrade and retrograde access site closure.
Vascular closure device malfunction due to kinking of the flexible sheath introducer is a problem, not only in this study but in other studies as well. Nevertheless, although rarely reported, it is a common problem, especially in obese patients, and may lead to technical failure of vascular closure devices [5].
According to the performing interventional radiologists, the degree of (intravascular) arterial calcification at the antegrade puncture site did not affect the procedure’s difficulty in the current study as a result of the extravascular design of the vascular closure device, including the bioabsorbable polyglycolic acid plug, which is delivered atop the femoral artery, anchored by the neurovascular bundle sheath [4].
Success, Failure, and Complications
There is no unanimous definition of minor and major complications after diagnostic or interventional angiographic procedures. Although some authors consider hematoma >5 cm, pseudoaneurysm, and arteriovenous fistula to be major vascular complications, others regard them as minor (e.g., the ECLIPSE trial) as long as no surgical repair or blood transfusion is needed [4, 9]. Development of hematoma is generally considered to be a minor complication or not a complication at all.
It is arguable whether pseudoaneurysms treated by thrombin injection (in this study, three of four) ought to be regarded as major complications because vascular repair was performed by nonsurgical techniques. If considered as major, these complications produced a major closure-related complication rate of 3.0 % (3 of 100) in the current study.
The differences in definition of minor and major complications indicate the need for standardized definitions of closure-related complications with use of vascular closure devices so that they may be better compared. In addition, the definitions of hemostasis success, device success, and procedural success vary in the published literature, as does the interval to a follow-up visit.
Conclusion
We found the Exoseal vascular closure device to be safely applicable for antegrade puncture of the femoral artery, with a high rate of procedural success (96.0 %), a low rate of minor vascular complications (7.0 %), and no major adverse events. Malfunction due to kinking of the flexible vascular sheath introducer was rare (1.0 %).
References
Katz SG, Abando A (2004) The use of closure devices. Surg Clin North Am 84:1267–1280
Schwartz BG, Burstein S, Economides C et al (2010) Review of vascular closure devices. J Invasive Cardiol 22:599–607
Cordis (2011) Instructions for use: Cordis Exoseal vascular closure device. Cordis Corporation, Miami Lakes
Wong CW, Bachinsky W, Cambier P; for the ECLIPSE Trial Investigators et al (2009) A randomized comparison of a novel bioabsorbable vascular closure device versus manual compression in the achievement of hemostasis after percutaneous femoral procedures: the ECLIPSE trial (Ensure’s Vascular Closure Device Speeds Hemostasis trial). JACC Cardiovasc Interv 2:785–793
Minko P, Katoh M, Gräber S, Buecker A (2012) Obesity: an independent risk factor for insufficient hemostasis using the AngioSeal vascular closure device after antegrade puncture. Cardiovasc Intervent Radiol 35:775–778
Reekers JA, Müller-Hülsbeck S, Libicher M et al (2011) CIRSE vascular closure device registry. Cardiovasc Intervent Radiol 34:50–53
Lupattelli T, Tannouri F, Garaci FG et al (2010) Efficacy and safety of antegrade common femoral artery access closure using the Angio-Seal device: experience with 1889 interventions for critical limb ischemia in diabetic patients. J Endovasc Ther 17:366–375
Looby S, Keeling AN, McErlean A et al (2008) Efficacy and safety of the AngioSeal vascular closure device post antegrade puncture. Cardiovasc Intervent Radiol 31:558–562
Kapoor B, Panu A, Berscheid B (2007) Angio-Seal in antegrade endovascular interventions: technical success and complications in a 55-patient series. J Endovasc Ther 14:382–386
Biondi-Zoccai GG, Fusaro M, Tashani A et al (2007) AngioSeal use after antegrade femoral arteriotomy in patients undergoing percutaneous revascularization for critical limb ischemia: a case series. Int J Cardiol 118:398–399
Mukhopadhyay K, Puckett MA, Roobottom CA (2005) Efficacy and complications of AngioSeal in antegrade puncture. Eur J Radiol 56:409–412
Wille J, Vos JA, Overtoom TT et al (2006) Acute leg ischemia: the dark side of percutaneous femoral artery closure device. Ann Vasc Surg 20:278–281
Chiu AH, Vander Wal R, Tee K et al (2008) Comparison of arterial closure devices in antegrade and retrograde punctures. J Endovasc Ther 15:315–321
Duda SH, Wiskirchen J, Erb M et al (1999) Suture-mediated percutaneous closure of antegrade femoral arterial access sites in patients who have received full anticoagulation therapy. Radiology 210:47–52
Hahn U, Betsch A, Wiskirchen J et al (2001) A new device for percutaneous suture-mediated closure of arterial puncture sites using exteriorized needles: initial experience. J Invasive Cardiol 3:456–459
Spiliopoulos S, Katsanos K, Karnabatidis D et al (2011) Safety and efficacy of the starclose vascular closure device in more than 1000 consecutive peripheral angioplasty procedures. J Endovasc Ther 18:435–443
Chiu AH, Coles SR, Tibballs J, Nadkarni S (2010) The StarClose vascular closure device in antegrade and retrograde punctures: a single-center experience. J Endovasc Ther 17:46–50
Fantoni C, Medda M, Mollichelli N et al (2008) Clip-based arterial haemostasis after antegrade common femoral artery puncture. Int J Cardiol 128:427–429
Conflict of interest
D. Vorwerk received payment for lectures from Cook Group Incorporated, ev3, W. L. Gore & Associates, Inc., C. R. Bard, Inc., and Cordis Corporation. He also received payment for development of educational presentations from Cook Group Incorporated, ev3, W. L. Gore & Associates, Inc., C. R. Bard, Inc., Cordis Corporation, and BSIC, Inc. The other authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schmelter, C., Liebl, A., Poullos, N. et al. Suitability of Exoseal Vascular Closure Device for Antegrade Femoral Artery Puncture Site Closure. Cardiovasc Intervent Radiol 36, 659–668 (2013). https://doi.org/10.1007/s00270-012-0501-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-012-0501-2